Abstract
Background:
Graft fixation is important for graft take. Fibrin glue has been proposed as an ideal material, because of its human origin and it provides firm adhesion in seconds or minutes.
Objective:
To evaluate the efficiency of fibrin glue, in increasing the take of skin graft. Assessment includes surgical time taken for graft fixation, haematoma/seroma formation, engraftment and wound closure by day 14.
Methods:
The study is an observational prospective study conducted in the Department of Plastic Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, from January 2016 to June 2016. Sixteen patients who underwent split skin grafting were assessed during the study period. Fibrin glue was used on the recipient bed before grafting.
Results:
Better haemostasis and graft adhesion, with a significant reduction of surgical time, were noted.
Conclusion:
The safety profile of fibrin glue was excellent as indicated by the lack of any related serious adverse experiences. These findings demonstrate that it is safe and effective for attachment of skin grafts, with outcomes at least as good as conventional methods.
Keywords: Fibrin glue, graft fixation, graft take, skin graft
INTRODUCTION
The first experiments in the use of fibrinogen as a tissue adhesive were carried out in 1940.[1] The concept of fibrin glue became realistic in the 1970s, with the advent of techniques for isolation and concentration of coagulation factors. In 1972, the success of fibrin glue in repairing a peripheral nerve was described. Since then, there have been many reports of successes, and the use of fibrin glue has been extended into several areas of medicine.[2,3,4,5,6]
Many surgeons have indicated fibrin glue as the ideal sealant material, and because of its human origin, it is not toxic towards tissue. Fibrin glue promotes firm adhesion in seconds or minutes; it is reabsorbed within a few days after application, contains tissue more rapidly and decreases the risks of hematomas and graft losses.[7,8]
METHODS
The study was an observational prospective study conducted in the Department of Plastic Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, from January 2016 to June 2016. Sixteen patients who underwent split skin grafting were assessed during the study period [Table 1]. Fibrin glue used in this study was EVICEL (R) Fibrin Sealant Human, ETHICON, Inc, Somerville, NJ, USA) [Figure 1]. It is supplied as one vial each of biological active component 2 (BAC2) (55–85 mg/ml fibrinogen) and thrombin (800–1200 IU/ml human thrombin) frozen solutions.
Table 1.
Selection of patients
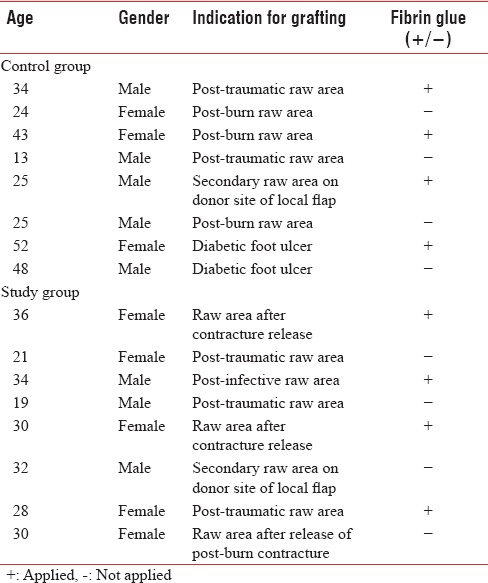
Figure 1.

Fibrin glue
The patients were divided into two groups by procedure:
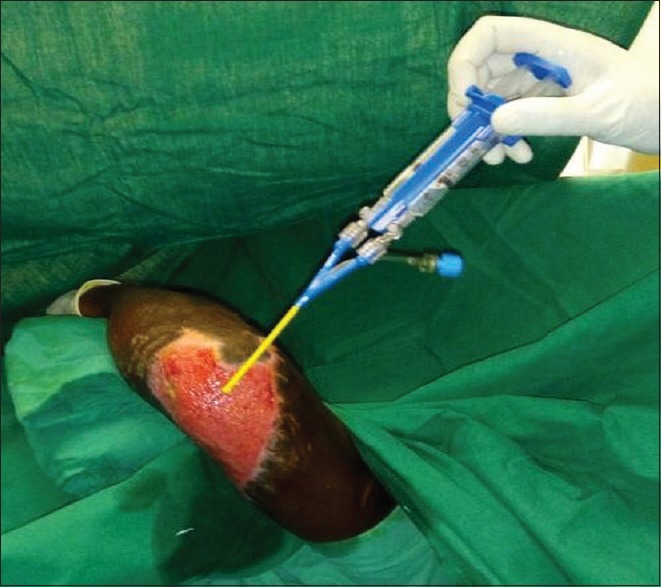
Reconstruction by graft, with the use of fibrin glue [Figure 2]
Reconstruction by graft, without the use of fibrin glue.
Figure 2.

Pre-operative photograph of post-traumatic raw area
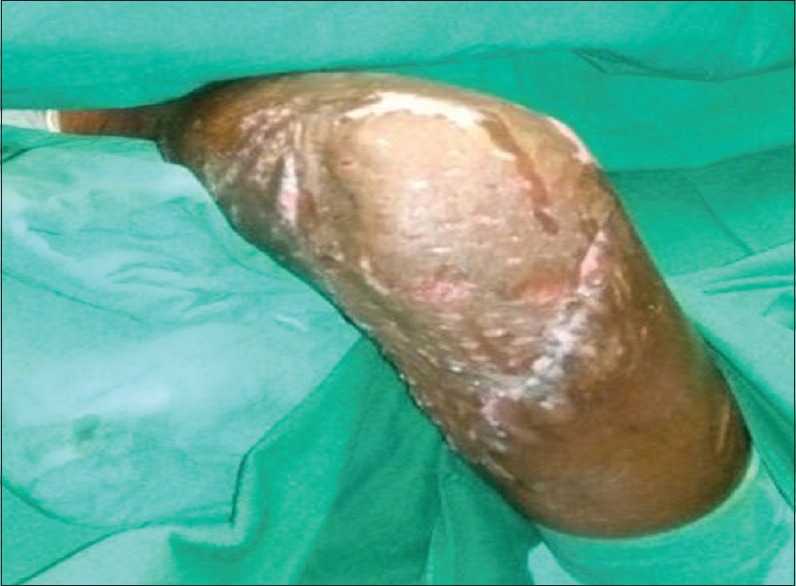
In the lesions of Category A patients, fibrin glue (EVICEL) was sprayed in short bursts (0.1–0.2 ml) onto the tissue to produce a thin, even layer, followed by grafting [Figures 3 and 4].
Figure 3.
Group 1 - Intraoperative photograph showing fibrin glue being sprayed on the wound bed
Figure 4.
Group 1 - Intraoperative photograph showing graft adherence with fibrin glue
After graft adhesion, dressing was applied, followed by occlusion using gauze and Micropore tape. In control wounds, grafting was placed in the usual manner with suture or with skin stapler followed by application of dressing.
RESULTS
Sixteen patients who underwent split skin grafting were assessed for the surgical time taken for graft fixation, haematoma/seroma formation and wound closure by day 14 [Table 2].
Table 2.
Parameters assessed
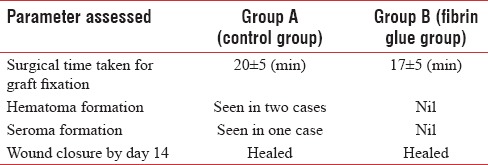
In the lesions submitted to cutaneous grafting and covered with fibrin glue, haemostasis was instantaneous and the adhesion of the graft was also firm and immediate. These benefits noticeably reduced surgical time to around 3 min. No reactions were noted to fibrin glue [Figure 5].
Figure 5.

Group 1 - Post-operative photograph showing complete wound healing on day 7
The 14th day evaluations showed no differences between the groups.
DISCUSSION
The use of fibrin glue has been described in many situations such as repair of the peripheral nerves and other viscera, fistula occlusion, surgery of cerebral tumours, skin grafting and application in burn patients.[2,3,5,7,8,9,10,11,12] The continuing evolution in the preparation and use of fibrin glue is emphasised in the literature.
Fibrin glue is commercially available and is produced from homologous plasma. However, contamination risks, potentially related to hepatitis C virus and HIV,[13] have discouraged its production in many countries. There are also reports of the production of fibrin glue by extraction of fibrinogen from animal serum although there is discussion about the possibility of hypersensitivity reactions from heterologous proteins.[14]
The fibrin glue product used in this study is EVICEL (R). EVICEL is manufactured from pooled human plasma. EVICEL is provided as a single use kit consisting of two packages: one package contains one vial of BAC2 and one vial of thrombin. The second package contains a sterile spray application device. The two components (BAC2 and thrombin) should be mixed and applied topically.
Autologous fibrin glue may be produced from one blood unit (500 ml). Fibrinogen is obtained from blood through centrifugation and cryoprecipitation techniques and is converted into fibrin glue by adding thrombin during surgery. Fibrinogen may be stored in a freezer at 20°C and can be used for 2 years.
Efficient haemostasis is reported in various studies, and as the principal advantage of fibrin glue in surgery on organs with non-suturable haemorrhage such as liver, spleen and retroperitoneal surfaces.[10,13] The firm adhesion that facilitates the joining of tissues is also reported in various studies involving surgery on internal organs.[5,7,10,15]
Skin graft take occurs in three phases. The first phase consists of plasmatic imbibition and lasts 24–48 h. This is followed by an inosculatory phase and a process of capillary ingrowth that occurs essentially simultaneously until generalised blood flow has been established by the 5th or 6th post-graft day.
Initially, a fine fibrin mesh links the graft to the bed, but over the first 4 days, this meshwork becomes lined with endothelial cells and links up with the vessels of the graft.
As it is proved by many studies that early skin graft survival depends on stabilisation of the graft by the fibrin network between the graft and the recipient bed. Fibrin glue provides an immediate, highly cross-linked fibrin network that will stabilise the graft and facilitate graft nutrition by serum imbibitions (plasmatic circulation) with subsequent ingrowth of vascular buds (neovascularisation).
In our study, it was seen that the use of fibrin glue in the intraoperative period greatly facilitated surgery because haemostasis was immediate. Due to the rapid and efficient haemostasis, it was observed during clinical evolution that there was no development of haematomas and if they showed up at all, they were small and did not affect graft take. The adhesion of the grafts was firm and suture was not necessary, thus reducing the surgical time when compared to control cases. A limiting factor for the use of fibrin glue is its cost because the products commercially available are very expensive.
The limiting factor of this preliminary study was a small sample size, and hence no statistical analysis was done.
CONCLUSION
Safety profile of fibrin glue was excellent and there were no adverse effects noted with it being effective in promoting the take of skin graft. Cost of fibrin glue and small sample size are the limiting factors.
Financial support and sponsorship
This study was financially supported by the Department of Plastic Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Dyson M, Young S, Pendle CL, Webster DF, Lang SM. Comparison of the effects of moist and dry conditions on dermal repair. J Invest Dermatol. 1988;91:434–9. doi: 10.1111/1523-1747.ep12476467. [DOI] [PubMed] [Google Scholar]
- 2.Chakravorty RC, Sosnowski KM. Autologous fibrin glue in full-thickness skin grafting. Ann Plast Surg. 1989;23:488–91. doi: 10.1097/00000637-198912000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Dahlstrøm KK, Weis-Fogh US, Medgyesi S, Rostgaard J, Sørensen H. The use of autologous fibrin adhesive in skin transplantation. Plast Reconstr Surg. 1992;89:968–72. [PubMed] [Google Scholar]
- 4.Eaglstein WH. Experiences with biosynthetic dressings. J Am Acad Dermatol. 1985;12(2 Pt 2):434–40. doi: 10.1016/s0190-9622(85)80006-2. [DOI] [PubMed] [Google Scholar]
- 5.Härting F, Koornneef L, Peeters HJ, Gillissen JP. Glued fixation of split-skin graft to the bony orbit following exenteration. Plast Reconstr Surg. 1985;76:633–5. doi: 10.1097/00006534-198510000-00030. [DOI] [PubMed] [Google Scholar]
- 6.Lilius P. Fibrin adhesive: Its use in selected skin grafting. Practical note. Scand J Plast Reconstr Surg Hand Surg. 1987;21:245–8. doi: 10.3109/02844318709086451. [DOI] [PubMed] [Google Scholar]
- 7.Kram HB, Shoemaker WC, Clark SR, Macabee JR, Yamaguchi MA. Spraying of aerosolized fibrin glue in the treatment of nonsuturable hemorrhage. Am Surg. 1991;57:381–4. [PubMed] [Google Scholar]
- 8.Jabs AD, Jr, Wider TM, DeBellis J, Hugo NE. The effect of fibrin glue on skin grafts in infected sites. Plast Reconstr Surg. 1992;89:268–71. doi: 10.1097/00006534-199202000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Kram HB, Reuben BI, Fleming AW, Shoemaker WC. Use of fibrin glue in hepatic trauma. J Trauma. 1988;28:1195–201. doi: 10.1097/00005373-198808000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Ormann W, Hopf G. Spontaneous splenic rupture in infectious mononucleosis organ preserving operation by means of fibrin tissue adhesive. Langenbecks Arch Chir. 1988;373:2402. doi: 10.1007/BF01261816. [DOI] [PubMed] [Google Scholar]
- 11.Saltz R, Dimick A, Harris C, Grotting JC, Psillakis J, Vasconez LO. Application of autologous fibrin glue in burn wounds. J Burn Care Rehabil. 1989;10:504–7. doi: 10.1097/00004630-198911000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Siedentop KH. Autologous fibrin tissue adhesive. Laryngoscope. 1985;95:10746. [PubMed] [Google Scholar]
- 13.Byrne DJ, Hardy J, Wood RA, McIntosh R, Cuschieri A. Effect of fibrin glues on the mechanical properties of healing wounds. Br J Surg. 1991;78:841–3. doi: 10.1002/bjs.1800780723. [DOI] [PubMed] [Google Scholar]
- 14.Brown DM, Barton BR, Young VL, Pruitt BA. Decreased wound contraction with fibrin glue – Treated skin grafts. Arch Surg. 1992;127:404–6. doi: 10.1001/archsurg.1992.01420040046007. [DOI] [PubMed] [Google Scholar]
- 15.Matras H, Dinges HP, Lassmann H, Mamoli B. Suture-free interfascicular nerve transplantation in animal experiments. Wien Med Wochenschr. 1972;122:517–23. [PubMed] [Google Scholar]


