Abstract
Background:
Keloids are abnormal wound responses characterised by excessive deposition of collagen and glycoprotein. They are both aesthetically and symptomatically distressing for most of the patients. There are reports of keloid management with pulsed dye laser (PDL), fractional carbon dioxide (CO2) laser and neodymium-doped yttrium aluminium garnet (Nd:YAG) laser individually and also in combination of CO2 with PDL and CO2 with Nd:YAG. Here, we discuss a combination of all the 3 lasers as a therapy for keloids.
Aim:
This study aims to assess the efficacy of fractional CO2 laser, long pulse Nd:YAG laser and PDL in the management of keloids.
Materials and Methods:
Fifteen patients with keloids were treated by fractional CO2 laser, followed by PDL and long pulse Nd:YAG laser at monthly intervals. Four patients discontinued the study and were lost for follow-up. Photographs were taken at the beginning of the treatment and at the end of five sessions. Clinical improvement was analysed based on a visual analogue scale graded by three blinded observers after assessing the clinical photographs for the improvement in size, colour and aesthetic impression.
Results:
Of the 11 patients, one patient had excellent improvement, one patient had good improvement, four patients had moderate improvement, two patients had mild improvement and three had no improvement.
Conclusion:
Lasers may have a synergistic effect when combined with other modalities of treatment but cannot be used as monotherapy in the treatment of keloids.
Keywords: Carbon dioxide laser, keloids, Nd:YAG laser, pulsed dye laser
INTRODUCTION
Keloids are aberrant responses to cutaneous insult characterised by hyperproliferation of dermal collagen.[1] They present as a cosmetic concern, often associated with pain and pruritus. Treatment of keloids includes surgical excision, dermabrasion, grafting, radiation, pressure therapy, silicone gel sheeting and intralesional corticosteroids.[2,3]
The application of lasers in cutaneous surgery has evolved to a great extent in the last three decades. 585-nm pulsed dye laser (PDL) has been effectively used to reduce scar erythema, size and associated symptoms.[4,5,6,7,8,9,10,11,12,13,14,15] The combinations of carbon dioxide laser (CO2) with PDL[11] and CO2 with yttrium aluminium garnet laser (YAG)[16] have also been tried for the treatment of keloids.
Apfelberg et al.[17] first reported the use of lasers on keloids by irradiation with CO2 and argon lasers in 13 patients out of whom, only one patient showed improvement.
Subsequently, neodymium-doped YAG laser (Nd:YAG) and PDL were evaluated for the treatment of keloids, with variable outcomes.[18] PDL showed promising results.[4,5,6,7,8,9,10,11,12,13,14,15] Several authors suggested that other therapeutic modalities such as intralesional steroids, silicone gel sheets or pressure therapy should be advocated in combination with lasers.[18]
We report the efficacy of fractional CO2 , PDL and long pulse Nd:YAG laser for the treatment of keloids.
MATERIALS AND METHODS
Fifteen patients above 14 years of age with keloids, all of whom were not treated before the beginning of the study were included in the study. Patients below 14 years, pregnant and lactating females, and patients with a history of isotretinoin use in the past 6 months were excluded. Written and informed consent (both in English and local language) was obtained from each patient before starting the treatment and for taking photographs. Photographs of every keloid included in the study were taken at baseline and before each session of the laser, using a DSLR Nikon D5100. Ethical clearance for the study was obtained from the Institutional Human Ethics Committee.
After taking photographs, patients were locally anaesthetised by a topical eutectic mixture of lidocaine and prilocaine under occlusion for 1 h. The cream was wiped off with a wet gauze and the area to be lased was cooled with ice packs to prevent unnecessary thermal injury and discomfort. Protective eyewear was provided to the patient, treating doctor and all the personnel assisting the procedure.
Fractional CO2 laser (Lumenis AcuPulse Carbon Dioxide Laser, Germany) was delivered at an initial energy of 10 mJ with increments of 5 mJ at each sitting. Five minutes after the delivery of fractional CO2 , a combination of PDL and long pulse Nd:YAG laser (Cynosure Cynergy Multiplex, Massachusetts, USA) was delivered at a PDL fluence of 4 J/cm2 in the 1st sitting with increments of 1 J/cm2 during each sitting, while keeping the fluence of Nd:YAG constant at 20 J/cm2. After the procedure, the treated area was again cooled; the patient was counselled about adequate photoprotection. Topical steroid was applied immediately post-procedure to reduce the inflammation. No other treatment for keloids was given to the patient.
All the patients underwent 5 sittings of the treatment with fractional CO2 , PDL and long pulse Nd:YAG lasers at intervals of 4 weeks. No complications such as hypo or hyperpigmentation, ulceration, or infection were observed during the study. All the patients were followed up for 6 months.
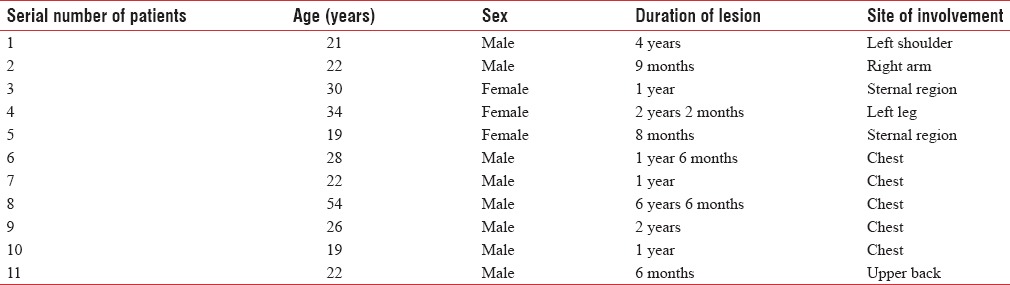
Of the 15 patients included in the study, 11 patients completed the study [Table 1]. Four patients discontinued the study and were lost for the follow-up. Clinical improvement was analysed based on a visual analogue scale graded by three blinded observers (qualified dermatologists who were not a part of our study) after assessing the clinical photographs for the improvement in size, colour and aesthetic impression.
Table 1.
Epidemiological profile of all the patients
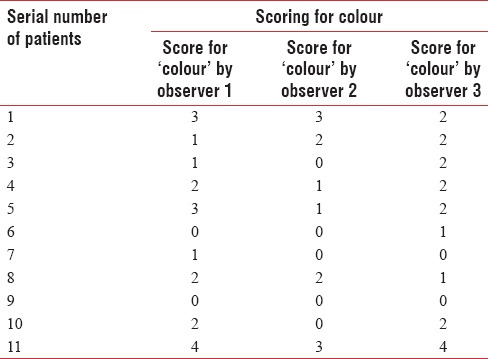
A score of 0 for 'no improvement, 1 for “mild improvement” (<25%), 2 for “moderate improvement” (26%–50%), 3 for “good improvement” (51%–75%) and 4 for “excellent improvement” (76%–100%) was accorded'.
RESULTS
The scores given for all the three parameters (size, colour and aesthetic impression) by each observer for each patient were recorded [Tables 2–4].
Table 2.
Scores accorded by 3 observers for size
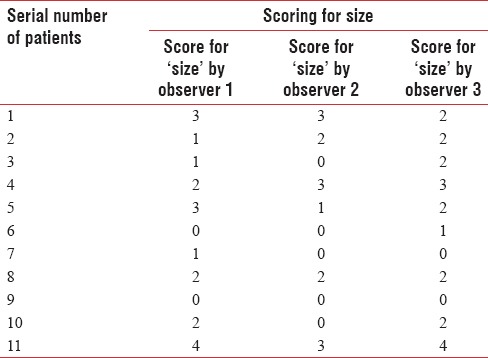
Table 4.
Scores accorded by 3 observers for aesthetic impression
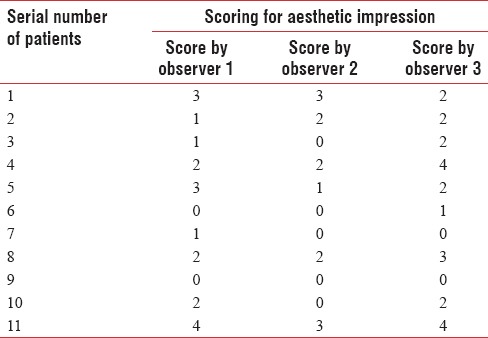
Table 3.
Scores accorded by 3 observers for colour
The mean score of all the three observers was calculated [Table 5].
Table 5.
Mean of scores accorded by 3 observers
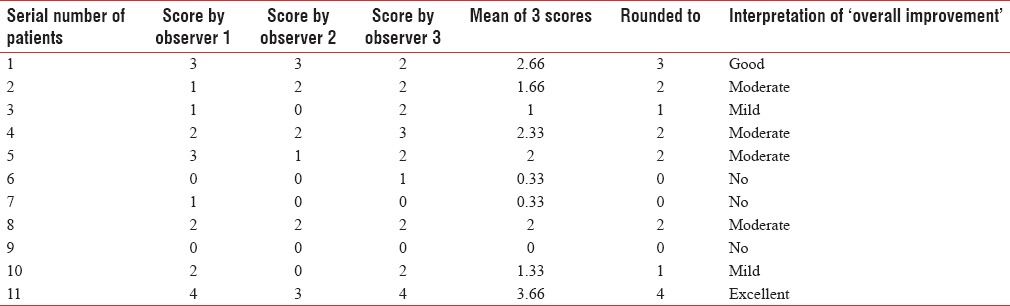
Of the 11 patients, 1 (9%) had excellent improvement i.e., complete flattening, 1 (9%) had good improvement, 4 (37%) had moderate improvement, 2 (18%) had mild improvement and 3 (27%) had no improvement (27%) [Graph 1]. During the follow-up of 6 months, only one patient had an increase in the size of the keloid.
Graph 1.

Overall improvement
Figures 1–4 show the pre- and post-treatment photographs of four patients with keloids.
Figure 1.
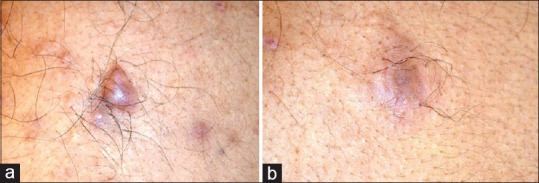
(a) Before starting the treatment, (b) after five sessions of laser treatment
Figure 4.
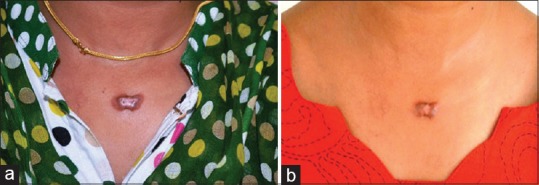
(a) Before starting the treatment, (b) after five sessions of laser treatment
Figure 2.

(a) Before starting the treatment, (b) after five sessions of laser treatment
Figure 3.

(a) Before starting the treatment, (b) after five sessions of laser treatment
DISCUSSION
There has been a significant advancement in the field of lasers in dermatology over the last three decades which has changed the face of aesthetics and dermato-medicine.
The fractional CO2 laser acts by the principle of fractional photothermolysis in which there is thermal ablation of tiny microscopic columns by microthermal zones. Following this, there is the induction of repair and re-epithelialisation by the columns of intact skin surrounding the affected skin by epidermal stem cell proliferation and fibroblast-derived neocollagenogenesis.[19]
The vascular lasers act by getting absorbed by haemoglobin which produces heat and causes coagulation necrosis resulting in hypoperfusion and tissue hypoxia. This leads to neocollagenesis, heating of collagen fibres with dissociation of disulphide bonds and subsequent realignment of collagen fibres.[9,20]
In addition, the PDL which has a less deeper wavelength than the Nd:YAG laser, gets absorbed by the haemoglobin and converts it into black methaemoglobin which acts as a chromophore for the Nd:YAG laser.
In a study conducted by Kono et al.,[21] 19 hypertrophic scars were irradiated with a PDL which demonstrated that 16 lesions (84%) showed a significant flattening of the scar and reduction in erythema. Therefore, he suggested that treatment of scars with PDL can help to reduce the erythema and size very effectively. In our study, it was found that, out of 11 lesions, 8 lesions (73%) showed improvement in size and erythema/colour which was in accordance with the study done by Kono et al.[21]
In 2004, Chan et al.[22] treated 36 scars in 27 patients with 585 nm – PDL and 66% reported clinical improvement which is slightly less than that of our study which showed improvement in 72% of patients.
Another study done by Nouri et al.[23] in 2003, revealed that all the 12 post-operative scars treated with three sessions of PDL (585 nm) showed significant overall improvement and enhanced cosmetic appearance. However, in our study, improvement in aesthetic impression was seen only in 8 (73%) out of 11 patients.
Several studies using CO2 laser were carried out to prove its efficacy in the treatment of keloids. Norris[24] in 1991, Apfelberg et al.[25] in 1989, Stern and Lucente[26] also in the year 1989 conducted studies to assess the efficacy of CO2 laser on keloids but failed to prove promising results. However, a study conducted by Alster et al.[11] in 20 patients with hypertrophic scars proved to be effective when the CO2 laser was used in combination with PDL.
Kumar et al.[27] treated 17 keloids with Nd:YAG laser and demonstrated that 10 lesions (58.8%) completely resolved and 7 lesions (41.2%) showed only partial resolution. However, our study demonstrated complete resolution only in 1 keloid (9.09%) and partial resolution in 7 keloids (63.64%).
Sherman and Rosenfeld,[28] in the year 1988 irradiated 17 keloids with Nd:YAG laser and found promising results with all the keloids. Similarly, Abergel et al.[29] conducted a study in 8 patients with keloids using Nd:YAG laser and demonstrated good results.
Several laser sessions are advised for obtaining a promising response, but lower fluences are suggested for the avoidance of adverse effects in patients with a higher melanin content in the skin, although, some authors have reported that higher fluences are associated with a better tissue response.[6,7,20]
In another review study by Bouzari et al., it was concluded that different lasers are effective in not only the treatment but also the prevention of hypertrophic scars and keloids.[30] Our study demonstrated complete resolution only in 1 keloid (9.09%) and partial resolution in 7 keloids (63.64%).
CONCLUSION
Lasers may have a synergistic effect when combined with other modalities of treatment but cannot be used as monotherapy in the treatment of keloids. The limitations of our study include a small sample size and the limited number of laser sessions. To assess the efficacy of lasers alone, other modalities of treatment were avoided which could have given better results.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kelly AP. Medical and surgical therapies for keloids. Dermatol Ther. 2004;17:212–8. doi: 10.1111/j.1396-0296.2004.04022.x. [DOI] [PubMed] [Google Scholar]
- 2.Alster TS, West TB. Treatment of scars: A review. Ann Plast Surg. 1997;39:418–32. doi: 10.1097/00000637-199710000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Ketchum LD, Cohen IK, Masters FW. Hypertrophic scars and keloids. A collective review. Plast Reconstr Surg. 1974;53:140–54. doi: 10.1097/00006534-197402000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Alster TS, Kurban AK, Grove GL, Grove MJ, Tan OT. Alteration of argon laser-induced scars by the pulsed dye laser. Lasers Surg Med. 1993;13:368–73. doi: 10.1002/lsm.1900130314. [DOI] [PubMed] [Google Scholar]
- 5.Alster TS. Improvement of erythematous and hypertrophic scars by the 585-nm flashlamp-pumped pulsed dye laser. Ann Plast Surg. 1994;32:186–90. doi: 10.1097/00000637-199402000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Dierickx C, Goldman MP, Fitzpatrick RE. Laser treatment of erythematous/hypertrophic and pigmented scars in 26 patients. Plast Reconstr Surg. 1995;95:84–90. [PubMed] [Google Scholar]
- 7.Goldman MP, Fitzpatrick RE. Laser treatment of scars. Dermatol Surg. 1995;21:685–7. doi: 10.1111/j.1524-4725.1995.tb00270.x. [DOI] [PubMed] [Google Scholar]
- 8.Alster TS, Williams CM. Improvement of keloid sternotomy scars by the 585 nm pulsed dye laser: A controlled study. Lancet. 1995;345:1198–200. doi: 10.1016/s0140-6736(95)91989-9. [DOI] [PubMed] [Google Scholar]
- 9.Alster TS, McMeekin TO. Improvement of facial acne scars by the 585 nm flashlamp-pumped pulsed dye laser. J Am Acad Dermatol. 1996;35:79–81. doi: 10.1016/S0190-9622(96)90501-0. [DOI] [PubMed] [Google Scholar]
- 10.Alster TS, Nanni CA. Pulsed dye laser treatment of hypertrophic burn scars. Plast Reconstr Surg. 1998;102:2190–5. doi: 10.1097/00006534-199811000-00060. [DOI] [PubMed] [Google Scholar]
- 11.Alster TS, Lewis AB, Rosenbach A. Laser scar revision: Comparison of CO2 laser vaporization with and without simultaneous pulsed dye laser treatment. Dermatol Surg. 1998;24:1299–302. doi: 10.1111/j.1524-4725.1998.tb00003.x. [DOI] [PubMed] [Google Scholar]
- 12.Lupton JR, Alster TS. Laser scar revision. Dermatol Clin. 2002;20:55–65. doi: 10.1016/s0733-8635(03)00045-7. [DOI] [PubMed] [Google Scholar]
- 13.Alster TS, Handrick C. Laser treatment of hypertrophic scars, keloids, and striae. Semin Cutan Med Surg. 2000;19:287–92. doi: 10.1053/sder.2000.18369. [DOI] [PubMed] [Google Scholar]
- 14.Wittenberg GP, Fabian BG, Bogomilsky JL, Schultz LR, Rudner EJ, Chaffins ML, et al. Prospective, single-blind, randomized, controlled study to assess the efficacy of the 585-nm flashlamp-pumped pulsed-dye laser and silicone gel sheeting in hypertrophic scar treatment. Arch Dermatol. 1999;135:1049–55. doi: 10.1001/archderm.135.9.1049. [DOI] [PubMed] [Google Scholar]
- 15.Groover IJ, Alster TS. Laser revision of scars and striae. Dermatol Ther. 2000;13:50–9. [Google Scholar]
- 16.Cheng ET, Nowak KC, Koch RJ. Effect of blended carbon dioxide and erbium:YAG laser energy on preauricular and ear lobule keloid fibroblast secretion of growth factors: A serum-free study. Arch Facial Plast Surg. 2001;3:252–7. doi: 10.1001/archfaci.3.4.252. [DOI] [PubMed] [Google Scholar]
- 17.Apfelberg DB, Maser MR, Lash H, White D, Weston J. Preliminary results of argon and carbon dioxide laser treatment of keloid scars. Lasers Surg Med. 1984;4:283–90. doi: 10.1002/lsm.1900040309. [DOI] [PubMed] [Google Scholar]
- 18.English RS, Shenefelt PD. Keloids and hypertrophic scars. Dermatol Surg. 1999;25:631–8. doi: 10.1046/j.1524-4725.1999.98257.x. [DOI] [PubMed] [Google Scholar]
- 19.Manstein D, Herron GS, Sink RK, Tanner H, Anderson RR. Fractional photothermolysis: A new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med. 2004;34:426–38. doi: 10.1002/lsm.20048. [DOI] [PubMed] [Google Scholar]
- 20.Reiken SR, Wolfort SF, Berthiaume F, Compton C, Tompkins RG, Yarmush ML. Control of hypertrophic scar growth using selective photothermolysis. Lasers Surg Med. 1997;21:7–12. doi: 10.1002/(sici)1096-9101(1997)21:1<7::aid-lsm2>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 21.Kono T, Erçöçen AR, Nakazawa H, Honda T, Hayashi N, Nozaki M. The flashlamp-pumped pulsed dye laser (585 nm) treatment of hypertrophic scars in Asians. Ann Plast Surg. 2003;51:366–71. doi: 10.1097/01.SAP.0000067722.07175.62. [DOI] [PubMed] [Google Scholar]
- 22.Chan HH, Wong DS, Ho WS, Lam LK, Wei W. The use of pulsed dye laser for the prevention and treatment of hypertrophic scars in chinese persons. Dermatol Surg. 2004;30:987–94. doi: 10.1111/j.1524-4725.2004.30303.x. [DOI] [PubMed] [Google Scholar]
- 23.Nouri K, Jimenez GP, Harrison-Balestra C, Elgart GW. 585-nm pulsed dye laser in the treatment of surgical scars starting on the suture removal day. Dermatol Surg. 2003;29:65–73. doi: 10.1046/j.1524-4725.2003.29014.x. [DOI] [PubMed] [Google Scholar]
- 24.Norris JE. The effect of carbon dioxide laser surgery on the recurrence of keloids. Plast Reconstr Surg. 1991;87:44–9. [PubMed] [Google Scholar]
- 25.Apfelberg DB, Maser MR, White DN, Lash H. Failure of carbon dioxide laser excision of keloids. Lasers Surg Med. 1989;9:382–8. doi: 10.1002/lsm.1900090411. [DOI] [PubMed] [Google Scholar]
- 26.Stern JC, Lucente FE. Carbon dioxide laser excision of earlobe keloids. A prospective study and critical analysis of existing data. Arch Otolaryngol Head Neck Surg. 1989;115:1107–11. doi: 10.1001/archotol.1989.01860330097026. [DOI] [PubMed] [Google Scholar]
- 27.Kumar K, Kapoor BS, Rai P, Shukla HS. In-situ irradiation of keloid scars with Nd:YAG laser. J Wound Care. 2000;9:213–5. doi: 10.12968/jowc.2000.9.5.25985. [DOI] [PubMed] [Google Scholar]
- 28.Sherman R, Rosenfeld H. Experience with the Nd:YAG laser in the treatment of keloid scars. Ann Plast Surg. 1988;21:231–5. doi: 10.1097/00000637-198809000-00007. [DOI] [PubMed] [Google Scholar]
- 29.Abergel RP, Dwyer RM, Meeker CA, Lask G, Kelly AP, Uitto J. Laser treatment of keloids: A clinical trial and an in vitro study with Nd:YAG laser. Lasers Surg Med. 1984;4:291–5. doi: 10.1002/lsm.1900040310. [DOI] [PubMed] [Google Scholar]
- 30.Bouzari N, Davis SC, Nouri K. Laser treatment of keloids and hypertrophic scars. Int J Dermatol. 2007;46:80–8. doi: 10.1111/j.1365-4632.2007.03104.x. [DOI] [PubMed] [Google Scholar]


