Abstract
BACKGROUND:
The curriculum of pathology is conventionally “taught” in a series of didactic lectures, which promotes learning by rote. In this study, case-based learning (CBL) was introduced to assess its effect on higher order cognition and problem-solving skills in undergraduate medical students.
SUBJECTS AND METHODS:
The prescribed syllabus of hepatobiliary system was delivered to the undergraduate medical students of the fourth semester by conventional didactic lectures. A pretest, which contained questions designed to test both analysis and recall, was administered, followed by CBL sessions, in the presence of a facilitator, encouraging active discussion among students. Students were then assessed using a similar posttest. The perceptions of the students and the faculty were gathered by means of feedback questionnaires. The scores obtained by the students in the pre- and post-test were compared by paired t-test.
RESULTS:
Eighty-one students participated in CBL sessions, with 95.06% expressing a desire for more such sessions, preferably in all the topics. The faculty members also felt that CBL would be beneficial for the students but opined that it should be restricted to some topics. CBL was found to cause a highly significant (P < 0.0001) improvement in the students’ higher levels of cognition, whereas the lower orders of cognition remained unaffected (P = 0.2048).
CONCLUSIONS:
CBL promotes active learning and helps in the development of critical thinking and analysis in undergraduate medical students. Although it is resource-intensive, an attempt should be made to incorporate it along with lectures in clinically important topics.
Keywords: Case-based learning, higher order cognition, pathology, undergraduate medical education
Introduction
In India, the curriculum of Pathology is conventionally delivered to the undergraduate student in the form of a series of didactic lectures sequentially dealing with different systems.[1] The present approach promotes learning by rote and lays less emphasis on the development of higher order of cognition like analysis and synthesis. Moreover, the exclusion of the end-user, that is, the patient, often causes the students to lose interest and does little to promote critical thinking and problem-solving skills, which are the essential attributes of a first contact physician.[2] As a result, students view Pathology as a hurdle to be crossed before being initiated into the clinical sciences, rather than the foundation stone on which the edifice of their clinical competence would be constructed.
Case-based learning (CBL) is a small group interactive teaching intervention, where cases are discussed under the guidance of a facilitator. The introduction of cases/scenarios helps the learners understand the practical application of theoretical knowledge. It uses a “guided-inquiry approach,” in which students are prompted to build upon their existing knowledge by sharing, questioning and discussion[3,4] but unlike the “open-inquiry approach” of problem-based learning (PBL) where students may digress from the topic, the presence of a facilitator ensures that the students attain the learning objectives in a time-efficient manner.[4]
CBL is promoted worldwide because it is learner-centric, interactive and patient-oriented, instead of being teacher-centric, monotonous, and content-driven.[3] Despite its proven advantages, only few studies have been undertaken in undergraduate medical students in the Asian subcontinent,[5,6,7,8,9,10] as CBL is resource-intensive.[6] However, early clinical exposure is the need of the hour, and it has been promoted by the Medical Council of India (MCI) in its Vision 2015 document.[11] Keeping this in view, this study was undertaken to promote interest, in-depth understanding and analytical thinking in undergraduate students in Pathology, using cases as triggers. The objectives of this study were 2-fold to assess the perceptions of the students and faculty to the introduction of CBL and to assess the impact, if any, of this intervention on the students’ performance.
Subjects and Methods
The study was conducted on the second professional undergraduate medical students after obtaining approval of the Institutional Ethics Committee. Informed written consent was obtained from the participating students.
A departmental faculty meeting was held in which the faculty was sensitized to the need for higher order cognitive thinking like critical thinking and analysis in the medical students. Four case scenarios dealing with hepatobiliary disorders were designed, keeping in view the educational requirements of a first contact physician. All the faculty members were shown the designed cases and their perceptions were gathered. The case scenarios were also shown to clinical specialty experts (pediatricians, physicians, and surgeons) who were given sufficient time to analyze them and provide feedback. The feedback provided was utilized to finalize the cases.
The prescribed curriculum of hepatobiliary system was delivered to the students by conventional didactic lectures. Thereafter, a pretest designed to test both analytical skills and recall, containing multiple-choice questions and structured essay questions, was administered. The pretest was taken by 82 students (the number of students presents out of the batch of 98 students).
The batch was divided into four groups for the CBL sessions. They were explained about the purpose and methodology of CBL and directed to come prepared for the same. The CBL sessions were commenced a week later and administered in place of tutorials. Eighty-one students attended these sessions and were considered the study group. At the beginning of each session, the same faculty member who had delivered the lectures, acting as a facilitator in CBL, gave a brief overview of the approach to a patient presenting with jaundice, as prescribed by standard textbooks of medicine. Then, the cases were introduced to the students and the learning objectives were laid out. The students were encouraged to build on their existing knowledge through active participation, questioning, reasoning, and group discussion. Other than the initial briefing, the facilitator's role was limited to encouraging group dynamics, ensuring the attainment of learning objectives and time management. Four cases were discussed over a time span of 2 h. At the end of each session, students’ feedback was collected.
A posttest containing questions of a similar pattern and a similar difficulty level as the pretest was designed and validated by the departmental faculty members. The posttest was scheduled a week after the conclusion of all CBL sessions and was taken by 79 students.
Although CBL sessions were held using paper cases, admitted patients with similar clinical profiles were sought for. The students were informed about such admissions and directed to visit the same, in an effort to reinforce the concepts learnt. The collaborating clinicians discussed the same cases during the clinical postings.
A cross-sectional survey was conducted to gather the perceptions of the 81 students attending the sessions and the 12 faculty members in the Department of Pathology regarding CBL. For this purpose, two different anonymous feedback questionnaires were used, both of which contained close- and open-ended questions. The close-ended questions were used to evaluate the perception of the students (Annexure 1 (147.2KB, pdf) ) and faculty (Annexure 2 (145.6KB, pdf) ) about the use of CBL as a teaching intervention, and to gather the students’ responses to the conduction of the sessions. They were graded on a 5-point Likert scale ranging from strongly agree (which was graded as 1) to strongly disagree (which was graded as 5). Open-ended questions were used to gather suggestions regarding the preferred use of CBL and the improvement of the sessions.
Feedback form for students (regarding case-based learning)
Feedback form for faculty members (regarding case-based learning)
Of the students who attended the CBL sessions, 59 students took both the pre- and post-tests. The effect of CBL on the academic performance was assessed in this subgroup of students.
Statistical analysis
The responses obtained in the student and faculty feedback questionnaires were analyzed using descriptive statistics. The scores obtained in the pretest were compared with those obtained in the posttest for both the analysis and recall-based questions by paired t-test. Statistical analysis was performed using SPSS v19.0 (IBM Co., Armonk, NY, USA).
Results
Students attending the CBL sessions gave an overwhelming positive response to this intervention [Table 1 and Figure 1]. All of them (100.0%) felt that CBL helped in better understanding of the disease process. Of the 81 students who provided feedback, 80 (98.77%) agreed that introduction of cases made the subject more interesting, and 78 (96.30%) felt that it made them more confident about dealing with clinical situations. They also agreed that this intervention motivated them to use additional learning resources, improved their learning abilities, enhanced their communication skills, and facilitated team learning, which was reported by 74 (91.36%), 76 (93.82%), 67 (82.72%), and 66 (69.14%) learners, respectively.
Table 1.
Feedback of students to case-based learning sessions
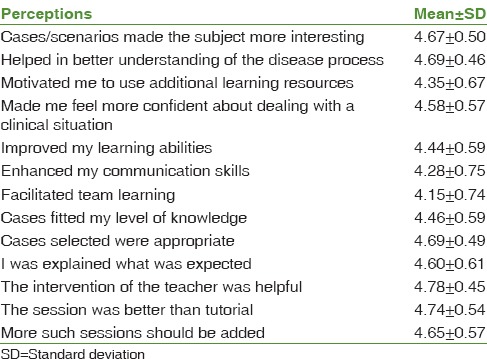
Figure 1.
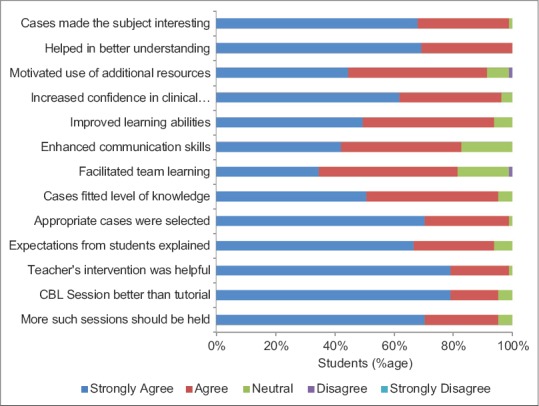
Pattern of student response to case-based learning sessions
Regarding the method by which these sessions were administered, 76 students (93.83%) felt that they were clearly explained what was expected from them. Majority of the students, that is, 80 (98.77%) and 77 (95.06%), respectively, also felt that the cases selected were appropriate and fitted their current level of knowledge, which was reiterated strongly by 57 (70.37%) and 41 (50.62%) students. The intervention of the teacher was found to be helpful by 80 students (98.77%), with 64 (79.01%) strongly agreeing to the same.
Summing up, an overwhelming majority of the learners (95.06% each) felt that CBL sessions were better than tutorials and expressed a desire for more such sessions, with only 4 (4.94%) remaining neutral and none dissenting.
The use of a case-based approach in all the topics was projected by 57 learners (70.37%), and 60 (74.07%) opined that CBL should preferably be used with lectures. However, 21 of the learners (25.93%) opted for the use of CBL as the primary teaching method.
When asked open-ended questions regarding suggestions for improvement, most students maintained that no improvement was required. Three students suggested that a patient may be visited in the hospital or brought during discussion. Two students emphasized that such sessions should only be conducted by “good” teachers. One student suggested that the basics be revisited by a PowerPoint presentation for 5–10 min at the beginning of the session. Other suggestions included reducing the number of cases, reducing the length of the session, and formation of smaller groups.
The response of the 12 faculty members to CBL as a teaching/learning intervention, though guarded, was also positive [Table 2 and Figure 2]. All of them felt that cases would make the subject more interesting for the learners, help in better understanding of the disease process, and also help identify gaps in their knowledge. Most of them also felt that CBL would improve the students’ learning abilities (91.67%) and lead to improved student-teacher interaction (75.%). However, one (8.33%) and three (25.0%) members, respectively, chose to remain neutral on this score.
Table 2.
Feedback of faculty to case-based learning sessions
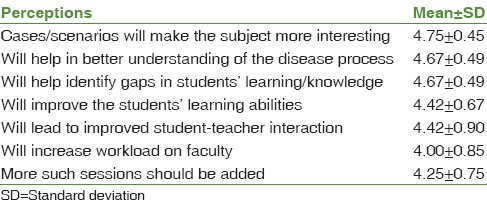
Figure 2.
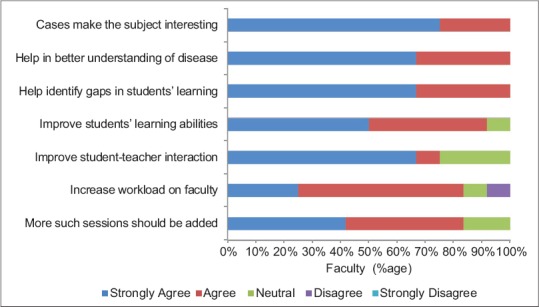
Pattern of faculty response to case-based learning sessions
Although all the faculty members perceived CBL as a beneficial tool for learners, 10 (83.33%) felt that it would increase the workload on faculty, one (8.33%) remained neutral, and one (8.33%) disagreed.
To summarize, ten out of 12 (83.33%) faculty members felt that more such sessions should be incorporated in the undergraduate Pathology curriculum.
Contrary to the students’ opinion, 11 faculty members (91.67%) felt that CBL should be used only in some, and not all, topics. However, like the students, all of them felt that it should be used along with lectures.
In response to the open-ended questions, the two main problems perceived by the faculty in the implementation of CBL, each expressed by three faculty members, were that it was time-consuming and would increase the workload on the already overburdened faculty. To be successful, CBL would require training of the faculty and prior clinical exposure on the part of the student. Other fears expressed were that it would require more faculty members and being time-consuming, might lead to difficulty in completing the prescribed syllabus.
The only way to optimize CBL, as suggested by six faculty members (50%), was to introduce it along with integration, preferably vertical. Similar to students, faculty also suggested that the basic concepts be introduced first and smaller groups be formed. Other suggestions for improvement included presentation of cases by students to improve interaction and involvement. It was also suggested that a case-based approach be limited to bedside teaching, but with emphasis on pathology.
In response to the open-ended question regarding areas where a case-based approach may be used, three thrust areas emerged. These were hematology, clinically common domains of systemic pathology (like renal, respiratory, and gastrointestinal pathology) and in conjunction with practical experiments (such as those in hematology and urine examination).
Using a paired t-test, [Figure 3] a highly significant difference (P = 4.69 ×/105) was found between the students’ scores in the analytical questions in the pretest (mean 8.44 ± 8.82) and the posttest (mean 14.24 ± 7.95). However, no significant difference (P = 0.2048) was found between the scores in the recall-based questions in the pretest (mean 16.56 ± 5.86) and the posttest (mean 17.53 ± 5.74). Thus, in this study, CBL was found to contribute significantly to the development of higher order cognition in students, including critical thinking and analysis but made no difference to the lower order cognition like recall.
Figure 3.
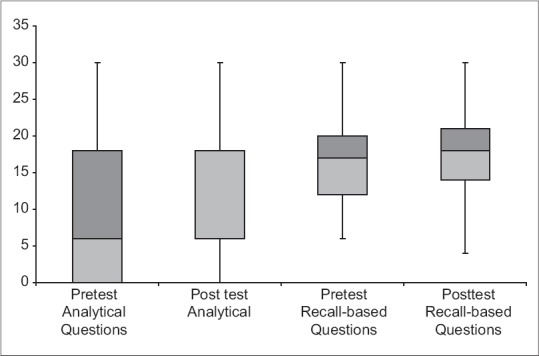
Box-plot and whisker chart of scores obtained in pre- and post-test
Discussion
The Accreditation Council for Graduate Medical Education of the United States enumerates six core competencies for every physician, which includes practice-based learning and patient care, apart from medical knowledge.[12] In India, the undergraduate medical education is primarily lecture-based, though many regulatory and advisory bodies like the MCI are ushering in innovative teaching interventions. In its Vision 2015 document, the MCI has promoted early clinical exposure and emphasized that a doctor should be able to fulfill five roles, including those of a clinician, a lifelong learner, and a leader and member of the health care team. Thus, a fresh medical graduate should be able to demonstrate effective clinical problem-solving skills, be an active, self-directed learner and a good collaborator.[3] To address these needs, CBL was selected as a suitable pedagogical tool. This study was initially planned as a case-control study of lecture versus CBL format with crossover but resistance to change by the administration dictated that teaching through lectures was nonnegotiable, and experiments with other innovations like CBL were permitted as adjuncts.
CBL evolved as an alternative to PBL[4] wherein students come with some advance preparation, and facilitators have an important role as they guide the discussions back to the learning objectives when students explore tangents.[5] CBL has traditionally been found to provide intrinsic motivation,[4,5,6,7,9] promote deep learning,[4,5,6,7,8,9,10] stimulate scientific enquiry,[4,9,13] integrate knowledge, and practice[4,5,6,7,8,9,10,11,13] and help students develop a collaborative approach to learning.[4,6,7] Evaluation of the feedback questionnaires of students showed that the CBL sessions conducted achieved all these targets. Faculty noted that the introduction of cases generated enthusiasm and led to increased involvement and active participation by all the students. This was in stark contrast to routinely held tutorials where only few students come prepared and interact. Many students reported back with details about the admitted patients having similar profiles, seeking clarification on various points, which showed that increased interest in the subject and self-directed learning were additional outcomes.
A significant parameter, which was assessed numerically in this study, probably for the first time, was the differential impact that CBL made on the lower and higher levels of learning. Questions testing lower orders of cognition like recall showed a mild increase in scores in the posttest as compared to the pretest, possibly because of the positive effect of reinforcement. However, a highly significant increase in scores was noted in the questions testing higher orders of cognition. This showed that higher levels of cognition and in-depth understanding can be attained even by a 2nd year undergraduate student, by challenging his analytical skills with problems.
Although the study design had to be changed, feedback questionnaires later showed this to be beneficial, as both the students and the faculty favored the utilization of CBL along with lectures. Interestingly, some of the earlier studies from the Western world have also found that lectures help in better preparation for written examinations and promoted CBL as an effective adjunct to lectures.[13]
Despite its proven advantages, the major hurdle cited, especially in a resource-poor country like ours, is that it requires motivated and trained faculty, validated case scenarios, infrastructural and logistical support and perhaps, most important, the time for planning and preparation.[7] However, we need to look at the other side of the coin. It is time that we utilized the biggest resource that we have the large number of patients visiting our hospitals to further the education of our future doctors. CBL is a way of utilizing this untapped resource for generating interest and promoting better contextual understanding of the pre- and para-clinical individuals, which may otherwise seem dry and boring.
As this is a new teaching/learning intervention, not currently practised in most Indian medical schools, there is a need for sensitization and training of faculty members, including those of other departments, to facilitate integration and proper administration. In this study, the faculty could not be motivated to undertake CBL sessions, and all the sessions were conducted by a single faculty member. However, it is worth mentioning that though initially sceptical, some faculty members expressed a desire to administer CBL in some clinically important topics on witnessing the students’ response and the rise in their grades. Another limitation was the size of the groups, which varied from 15 to 23. Multiple sessions with fewer cases and smaller groups could have led to better group dynamics and enhanced communication. The long-term outcomes of CBL also need to be evaluated.
Conclusions
The introduction of cases generates interest, promotes active learning, and helps in the development of critical thinking and analysis in undergraduate medical students. Although CBL is resource-intensive, an attempt should be made to incorporate it along with lectures in clinically important topics, especially in the early phases of undergraduate medical education, which deal solely with pre- and para-clinical specialties.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
I would like to acknowledge the motivation, guidance and support provided by Dr. Shailendra Handu, Associate Professor (Pharmacology), SMS and R, Greater Noida, Uttar Pradesh, India.
References
- 1.Medical Council of India Regulations on Graduate Medical Education. 1997. [Last accessed on 2016 May 30]. Available from: http://www.mciindia.org/Rules-and-Regulation/GME_REGULATIONS.pdf .
- 2.Klemenc-Ketis Z, Kersnik J. Deficiency areas in decision making in undergraduate medical students. Adv Med Educ Pract. 2014;5:223–7. doi: 10.2147/AMEP.S64920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Williams B. Case based learning – A review of the literature: is there scope for this educational paradigm in prehospital education? Emerg Med J. 2005;22:577–81. doi: 10.1136/emj.2004.022707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Srinivasan M, Wilkes M, Stevenson F, Nguyen T, Slavin S. Comparing problem-based learning with case-based learning: Effects of a major curricular shift at two institutions. Acad Med. 2007;82:74–82. doi: 10.1097/01.ACM.0000249963.93776.aa. [DOI] [PubMed] [Google Scholar]
- 5.Ciraj AM, Vinod P, Ramnarayan K. Enhancing active learning in microbiology through case based learning: Experiences from an Indian medical school. Indian J Pathol Microbiol. 2010;53:729–33. doi: 10.4103/0377-4929.72058. [DOI] [PubMed] [Google Scholar]
- 6.Jamkar AV, Burdick W, Morahan P, Yemul VY, Sarmukadum AV, Singh G. Proposed model of case based learning for training undergraduate medical student in surgery. Indian J Surg. 2007;69:176–83. doi: 10.1007/s12262-007-0016-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nair SP, Shah T, Seth S, Pandit N, Shah GV. Case based learning: A method for better understanding of biochemistry in medical students. J Clin Diagn Res. 2013;7:1576–8. doi: 10.7860/JCDR/2013/5795.3212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gupta K, Arora S, Kaushal S. Modified case based learning: Our experience with a new module for pharmacology undergraduate teaching. Int J Appl Basic Med Res. 2014;4:90–4. doi: 10.4103/2229-516X.136786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ghosh S, Pandya HV. Implementation of Integrated Learning Program in neurosciences during first year of traditional medical course: Perception of students and faculty. BMC Med Educ. 2008;8:44. doi: 10.1186/1472-6920-8-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Srinivas V, Kotwal A, Tekian A. Effect of Case Based Learning on Undergraduate Medical Students in Pathology. [Last accessed on 2016 May 30]. Available from: http://www.faimer.org/education/fellows/abstracts/10Srinivas.pdf .
- 11.MCI-Vision. 2015. [Last accessed on 2016 May 30]. Available from: http://www.mciindia.org/tools/announcement/MCI_booklet.pdf .
- 12.ten Cate O, Scheele F. Competency-based postgraduate training: Can we bridge the gap between theory and clinical practice? Acad Med. 2007;82:542–7. doi: 10.1097/ACM.0b013e31805559c7. [DOI] [PubMed] [Google Scholar]
- 13.Kassebaum DK, Averbach RE, Fryer GE., Jr Student preference for a case-based vs. lecture instructional format. J Dent Educ. 1991;55:781–4. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Feedback form for students (regarding case-based learning)
Feedback form for faculty members (regarding case-based learning)


