Abstract
The purpose of this study was to evaluate the long-term clinical and radiographic outcomes of posterolateral lumbar fusion for lumbar stenosis cases requiring bilateral facetectomy in conjunction with a laminectomy. The authors evaluated 34 consecutive patients who had undergone a lumbar laminectomy, bilateral partial facetectomy, and posterolateral fusion at a single institution between 1981 and 1996. They included 25 men and 9 women with a mean age of 42 years (range, 27–57 years). Twenty-three cases were instrumented and 11 were noninstrumented. Mean follow-up was 21 years (range, 15–29 years). Outcomes evaluated included reoperation rate, clinical outcomes evaluated by the Oswestry Disability Index (ODI) score, radiographic evaluations of adjacent segmental degeneration (ASD) and lumbar lordosis, and contributing demographic factors to disease progression. At final follow-up, 17 of the 34 patients had undergone reoperation (43% of the instrumented group and 64% of the noninstrumented group). There were no differences in the reoperation rate or ODI improvement between the instrumented and noninstrumented groups (P>.05). Female patients required more revisions, had less ODI improvement, had greater postoperative ASD, and had less maintenance of their postoperative lumbar lordosis. There was no difference in maintenance of postoperative lumbar lordosis or ASD between the instrumented and noninstrumented groups. Instrumentation did not improve revision rates, clinical outcomes, or radiographic outcomes in laminectomies requiring contemporaneous facetectomies.
The surgical treatment of low back pain and sciatica has undergone marked changes as the etiology of this disease has been better evaluated. An emphasis on surgery for nerve root compression by disk sequestration popularized by Mixter and Barr in 1934 has introduced a broader concept of pain generation encompassing treatment of associated spinal abnormalities that contribute to chronic lower back and leg pain.1–3 Although direct or indirect decompression of the neural elements remains the mainstay of treatment, a wide facetectomy is often needed in cases where lumbar stenosis is a result of significant facet hypertrophy.1–3 In these scenarios, what is the method of choice for an arthrodesis?
With iatrogenic instability from a wide decompression, is instrumentation cost-effective, and who is the ideal candidate for it?4–6 There is limited literature on this topic.1–3,7,8 Instrumented lumbar fusions have become popular; however, they come with their own complications.1–3,7,8 The current authors’ purpose was to evaluate the surgical procedures commonly used in the past decades to achieve lumbar fusion in cases requiring a wide laminectomy and bilateral partial facetectomy. Specifically, they assessed (1) reoperation rate; (2) clinical outcomes evaluated by the Oswestry Disability Index (ODI) score; (3) radiographic evaluations of adjacent segmental degeneration (ASD) and contributing demographic factors to disease progression; and (4) radiographic evaluations of lumbar lordosis.
Materials and Methods
The authors evaluated all patients who had undergone a wide lumbar laminectomy, bilateral partial facetectomy (more than 50%), and posterolateral arthrodesis for degenerative lumbar stenosis between 1981 and 1996 with a minimum 15-year follow-up. The only indication for surgery was symptomatic degenerative lumbar stenosis. All procedures were performed at a single institution by the senior author (C.B.), who is an experienced spine surgeon. Exclusion criteria were spondylolisthesis, scoliosis, moderate or severe flat-back (less than 30° of preoperative lumbar lordosis), fractures, tumors, cases with a concomitant anterior procedure, or less than a minimum 15-year follow-up. The reason for the chosen minimum follow-up inclusion criteria was two-fold. Evaluation of long-term outcomes was a goal of the study; furthermore, noninstrumented fusions were an older surgical technique, and the authors had attempted to control for the length of follow-up between the instrumented and noninstrumented cohorts and to minimize biases. Appropriate institutional review board approval was obtained for the study.
The patients included 25 men and 9 women with a mean age of 42 years (range, 27–57 years) at the time of the surgery. They were followed for a mean of 21 years (range, 15–27 years). Non-instrumented cases had a longer mean follow-up period of 25 years, compared with 19 years in the instrumented cohort. Noninstrumented cases were performed from 1981 to 1989, compared with the instrumented cases, which were performed from 1988 to 1996. No patient was lost to follow-up. Only 2 patients had a previous spine fusion. All patients had neurogenic claudication with varying degrees of back pain. In most cases, the neurogenic claudication and leg pain were more symptomatic than the back pain. Hospital records, radiographs, and office charts were reviewed. Specifically, postoperative lumbar lordosis and ASD were examined. Furthermore, the effects of demographic factors such as age and sex were included in the analysis of results.
All fusions involved decortication of the transverse processes and autograft use (local and iliac crest). All cases used only local autograft bone from the laminectomy and facetectomy. No allograft bone was used. Eleven patients were fused without the addition of instrumentation. Twenty-three patients had an arthrodesis that was instrumented. The instrumentation constructs included pedicle screws with AO plates. All fusions except one were over 2 or more levels, and all except 3 extended to the first sacral vertebra. The postoperative regimen was the same for all patients, which included the use of a lumbar chair back brace for a total of 3 days.
All radiographic evaluations were anteroposterior (AP) and lateral standing radiographs by the senior author (C.B.). Lordosis was measured from the superior endplates of L1 to S1.9,10 The initial postoperative follow-up images were evaluated for lordosis and compared with the most recent follow-up radiographs.
An analysis of ASD was performed at the most recent follow-up. A scoring system was devised that incorporated the main features of ASD by classifying them into degrees of severity ranging from grade 1 through grade 3. Grade 1 represented slight or no ASD and was qualified by the absence of spondylolisthesis greater than 4 mm, no angulation greater than 10°, no additional surgeries at that level, and less than 50% loss of disk height as compared with the earlier radiographs. Grade 2 was characterized by between 50% and 75% loss of disk height and absence of the factors mentioned above. Grade 3 represented severe ASD and was characterized by the presence of any of the following: greater than 75% loss of disk height, spondylolisthesis greater than 4 mm, or angulation greater than 10°. The presence of a subsequent surgery extending the fusion to that affected level was also considered to be grade 3 ASD. The first cranial segment (first adjacent segment) and the second cranial segment (second adjacent segment) were scored separately.
In all patients, radiographic outcomes were also correlated to ASD by grouping them into 1 of 4 categories as follows: patients with grade 1 (mild or none) ASD at both adjacent segments were characterized as having an excellent radiographic result. Those with a maximum grade of 2 (mild) at either or both of the adjacent segments were classified as having a good result. Patients who had 1 adjacent segment with severe grade 3 involvements were considered to have a fair result, and patients with severe ASD at both levels were classified as having a poor result.
All data were recorded using an Excel spreadsheet (Microsoft Corporation, Redmond, Washington). Statistical data analysis was performed using Fisher’s exact test, paired Student’s t test, and odds ratios (ORs) to evaluate reoperation rates, ODI scores, and radiographic outcomes between instrumented and noninstrumented groups. A P value less than .05 was used as a threshold for significance.
Results
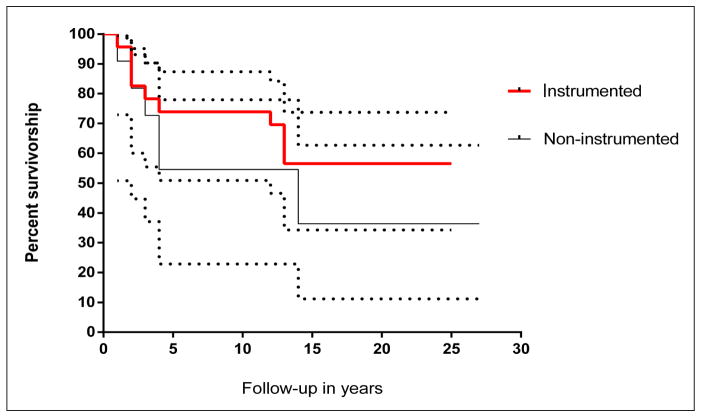
At final follow-up, 17 (50%) of the 34 patients had undergone either a revision or an extension of their fusion with an overall mean of 1 reoperation (range, 1–3) after the index procedure. This included 7 (64%) reoperations in the noninstrumented group and 10 (43%) reoperations in the instrumented group (P=.46). To further evaluate the follow-up adjusted outcomes, the authors performed a Kaplan-Meier analysis, which showed no significant differences in failures defined by reoperations between the 2 groups (P=.32) (Figure); however, with larger sample sizes, this difference may trend toward or become different. The underlying reasons for reoperation in the noninstrumented group were symptomatic pseudoarthrosis (n=5) and symptomatic ASD (n=2); in the instrumented group, 4 reoperations were due to symptomatic pseudoarthrosis and 6 were due to symptomatic ASD (Table 1). All reoperations occurred within 15 years of the index surgery. All patients were ambulatory at the most recent follow-up. When outcomes were stratified by sex, a greater number of women (7 of 9) required reoperation compared with men (10 of 25), and this trended toward significance (OR, 5.25; 95% confidence interval [CI], 0.9–30.6; P=.06).
Figure.
Kaplan-Meier survivorship analysis of instrumented vs noninstrumented patients. Dotted lines represent the 95% confidence interval.
Table 1.
Summary of Patients’ Demographics
| Demographic | No. |
|---|---|
| Noninstrumented | 11 |
| Instrumented | 23 |
| Reoperationa | 17 |
| No reoperationa | 17 |
| Male | 25 |
| Female | 9 |
| ASD | 8 |
| Pseudoarthrosis | 9 |
| Male reoperationa | 10 |
| Female reoperationa | 7 |
Abbreviation: ASD, adjacent segmental degeneration.
Revision of original surgery.
Overall, there were similar improvements in mean ODI scores at final follow-up in the instrumented and noninstrumented groups. In the instrumented group, mean ODI score improved from 83 points (range, 72–94 points) preoperatively to 43 points (range, 21–58 points) postoperatively. In the noninstrumented group, mean ODI score improved from 85 points (range, 70–92 points) preoperatively to 46 points (range, 61–84 points) postoperatively (Table 2). Therefore, there was no difference in mean ODI score improvement between the 2 groups (40 vs 39 points, respectively; P=.81).
Table 2.
Oswestry Disability Index Scores
| Parameter | Instrumented
|
Reoperation
|
Sex
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| No | Yes | P | Yesa | Noa | P | Male | Female | P | |
| Patients, No. | 11 | 23 | - | 17 | 17 | - | 25 | 9 | - |
| Preoperative ODI score, mean | 85 | 83 | .78 | 89 | 81 | .27 | 85 | 84 | .89 |
| Postoperative ODI score, mean | 46 | 43 | .75 | 80 | 34 | .001 | 28 | 79 | .001 |
| Score improvement, mean | 39 | 40 | .81 | 9 | 45 | .001 | 57 | 5 | .001 |
Abbreviation: ODI, Oswestry Disability Index.
Revision of original surgery.
Female patients and patients undergoing reoperation had less improvement in ODI scores. Male patients’ ODI scores improved by a mean of 57 points, whereas female patients’ ODI scores improved by a mean of only 5 points (P=.001). The reoperation group only improved 9 points, whereas the patients who did not require a second surgery improved 45 points (P=.001) (Table 2).
Overall, 24% (n=8) of patients had an excellent radiographic result, 29% (n=10) had a good result, 32% (n=11) had a fair result, and 15% (n=5) had a poor result (Table 3). When the outcomes were substratified between instrumented and noninstrumented patients, there was no significant difference in the number of patients who had achieved excellent or good results (52% vs 54%, respectively; P=.88). The incidence of severe ASD was the same for both the first and second adjacent cranial segments. Eleven (32%) patients showed evidence of severe ASD at the first adjacent cranial level and 11 showed evidence of severe ASD at the following level. The mean grade was 1.9 at the first level and 2 at the second level.
Table 3.
Radiographic Outcomes: ASD Grade on Final Follow-up of Cranial 2 Levels
| Parameter | Grade
|
|||
|---|---|---|---|---|
| Excellent | Good | Fair | Poor | |
| Overall | 24% | 29% | 32% | 15% |
| Noninstrumented | 27% | 27% | 27% | 18% |
| Instrumented | 22% | 30% | 35% | 13% |
| Male | 32% | 36% | 55% | 8% |
| Female | 0% | 11% | 56% | 33% |
Abbreviation: ASD, adjacent segmental degeneration.
There was a linear correlation between the mean length of follow-up and the presence of ASD. The mean follow-up period was 18 years for those with an excellent result, 21 years for those with a good result, 23 years for those with a fair result, and 25 years for those with a poor result. When outcomes were substratified based on patient demographics, mean age of patients at the time of surgery with fair or poor results was 44 years (range, 29–57 years), compared with 40 years (range, 27–55 years) for patients with good or excellent results (P=.09). Female patients had inferior results compared with males (P=.002). Of the 9 females in this study, 5 (56%) had a fair result, 3 (33%) had a poor result, 1 (11%) had a good result, and 0 had an excellent result (Table 4). Hence, there were no females without radiographic evidence of ASD.
Table 4.
Radiographic Outcomes: Lordosis (L1 to S1)
| Demographic | Lordosis
|
||||
|---|---|---|---|---|---|
| Preoperative | Immediate Postoperative | Final Follow-up | Overall Improvement | Loss of Lordosis at Final Follow-up | |
| Overall | 34° | 46° | 44° | 10° | 2° |
| Noninstrumented | 33° | 43° | 42° | 9° | 1° |
| Instrumented | 35° | 50° | 45° | 12° | 3° |
| Male | 33° | 45° | 44° | 11° | 1° |
| Female | 36° | 48° | 41° | 5° | 7° |
| Reoperationa | 32° | 41° | 38° | 6° | 3° |
| No reoperationa | 34° | 49° | 48° | 14° | 1° |
Revision of original surgery.
The instrumented and noninstrumented cohorts were well matched with regard to preoperative lumbar lordosis (35° vs 33°). However, there were no differences the improvement of preoperative lumbar lordosis or in the maintenance of postoperative lordosis in the instrumented and noninstrumented cohorts (P>.62). No correlation was seen between the immediate postoperative lordosis and the radiographic outcomes with respect to ASD. Patients with excellent or good radiographic outcomes had a mean immediate postoperative lordosis of 46.5°, with an average loss of 1.5° over time. For those with a fair or poor outcome, mean immediate postoperative lordosis was 45.5°, with an average loss of 2.3° over time. However, when examining sex, female patients had significant loss of postoperative lordosis over time compared with male patients (7° vs 1°; P=.01).
Discussion
Lumbar spine fusion techniques have evolved considerably over the past 20 years, with an approximately 500% increase in lumbar spine surgery expenditure since the year 1992 (from $75 to $482 million in 2003).11 Managing degenerative lumbar stenosis in a cost-effective way is a challenge. Therefore, for the particular scenario of degenerative lumbar stenosis that requires a laminectomy and facetectomy, is instrumentation necessary, and does it improve clinical and radiographic outcomes? In the current study, the authors sought to evaluate the clinical and radiographic outcomes and reoperation rate in patients who had undergone a wide lumbar laminectomy, facetectomy, and posterolateral arthrodesis in an attempt to identify potential contributing factors for the overall outcomes.
The study has several limitations, including a small sample size and an unequal number of males and females. The retrospective nature of the study could have introduced selection biases. For example, the noninstrumented cases were performed earlier in the study. Also, the authors used a nonvalidated grading system for ASD and correlation with clinical outcomes. In addition, the cohort was not sex-matched, which could have introduced biases. However, the authors believe the outcomes are valuable because no previous study has compared the long-term clinical and radiographic outcomes of instrumented and noninstrumented posterolateral lumbar fusions for laminectomy/facetectomy surgeries.
When the authors examined the improvement of lumbar lordosis and maintenance of postoperative lumbar lordosis, there was no difference between the noninstrumented and instrumented cases. Although one might expect that the use of instrumentation would enhance the maintenance of lordosis, there are 2 possible explanations for why this was not found. In this study, either Luque wire constructs, Texas Scottish Rite Hospital (TSRH) instrumentation, or AO plates were used (Table 5). These forms of instrumentation are inferior to modern-day pedicle screw/rod constructs. For example, Luque wires and TSRH hooks provide only posterior column fixation, whereas modern pedicle screws provide nearly 3-column support. Furthermore, global sagittal or coronal imbalance was an exclusion criterion of the study. Surgery was for lumbar stenosis requiring a wide decompression. In these cases with minor flatback deformity and lumbar stenosis, it is theorized that the flatback was largely postural in nature to alleviate the lumbar stenosis. Therefore, by removing the compressing pathology with a wide decompression, the postural flatback improves. So in this particular scenario, instrumentation may not be necessary to improve and maintain lumbar lordosis.
Table 5.
Instrumentation Design
| Parameter | No. (%) |
|---|---|
| Overall | 23 (100) |
| Pedicle screw/AO plate | 16 (70) |
| Luque wire construct | 5 (22) |
| Texas Scottish Rite Hospital System | 2 (9) |
The authors found no correlation between the original postoperative lordosis and the incidence of ASD. This is concordant with the findings of several authors.9,10,12–16 However, in a study addressing sagittal alignment and ASD in 83 patients, Kumar et al17 found the lowest incidence of ASD in patients with normal alignment and the highest in patients who had alterations in the C7 plumb line. Their study highlights the fact that the global sagittal balance of the spine may be a more important factor than the degree of lumbar lordosis itself.
The incidence of postoperative radiographic ASD after fusion has been reported to be variable, ranging from 5.2% to 100%.13 The current study showed that 50% of patients had moderate to severe ASD at one or both adjacent cephalad levels, which is consistent with the literature.13–15,17–19 The authors found that the mean ASD grade for each first or second cranial segment was similar (2.0 for the first and 1.9 for the second). In this study, longer follow-up was associated with a higher incidence of ASD. This finding may indicate that postoperative ASD is a progression of the preoperative spinal pathology and/or a consequence of altered biomechanics of a fusion.9,12–14,17,19,20
One of the most important findings of this study was the disproportionate number of fair and poor radiographic results in females. Female sex is considered to be a potential risk factor for ASD.13 Etebar and Cahill19 noted a large difference between males and females; out of a study population of 125 patients, a total of 18 developed symptomatic ASD. Fifteen of these cases were postmenopausal females.19 Theoretically, osteoporosis could have led to the inferior maintenance of lumbar lordosis and clinical outcomes seen in the female cohort of the study. However, dual-energy X-ray absorptiometry scans were not routinely ordered at latest follow-up.
Not only were the radiographic outcomes similar between the instrumented and noninstrumented cohorts, but the improvement in ODI scores was also similar. This is in agreement with Katz et al,21 whose retrospective review of 272 patients treated for lumbar degenerative stenosis showed that the noninstrumented fusion group had better relief of back pain at 6 months and 2 years compared with the instrumented fusion group. Despite the noninstrumented cases in the current study having a lengthier follow-up period, they maintained good clinical and radiographic outcomes.
Conclusion
A noninstrumented fusion is an effective surgical option for degenerative lumbar stenosis where a wide laminectomy and bilateral partial facetectomy are required. Postoperative lumbar lordosis was not found to be correlated with a long-term incidence of ASD. Longer follow-up appears to be a risk factor for development of ASD and may be a consequence of disease progression or altered biomechanics. Adjacent segmental degeneration is as likely as not to occur to a level requiring further surgery, whether instrumented or in situ.
Footnotes
Dr Pourtaheri, Dr Billings, Dr Bogatch, Dr Issa, Dr Haraszti, Mr Mangel, Dr Lord, Dr Park, Dr Ajiboye, and Dr Ashana have no relevant financial relationships to disclose. Dr Emami is a paid consultant for and is on the speaker’s bureau of DePuy.
References
- 1.Polly DW, Jr, Santos ER, Mehbod AA. Surgical treatment for the painful motion segment: matching technology with the indications. Posterior lumbar fusion. Spine (Phila Pa 1976) 2005;30(suppl 16):S44–S51. doi: 10.1097/01.brs.0000174529.07959.c0. [DOI] [PubMed] [Google Scholar]
- 2.Fischgrund JS. The argument for instrumented decompressive posterolateral fusion for patients with degenerative spondylolisthesis and spinal stenosis. Spine (Phila Pa 1976) 2004;29(2):173–174. doi: 10.1097/01.BRS.0000111142.76601.1A. [DOI] [PubMed] [Google Scholar]
- 3.Phillips FM. The argument for noninstrumented posterolateral fusion for patients with spinal stenosis and degenerative spondylolisthesis. Spine (Phila Pa 1976) 2004;29(2):170–172. doi: 10.1097/01.BRS.0000106318.98185.6E. [DOI] [PubMed] [Google Scholar]
- 4.Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am. 1991;73(6):802–808. [PubMed] [Google Scholar]
- 5.Fischgrund JS, Mackay M, Herkowitz HN, Brower R, Montgomery DM, Kurz LT. 1997 Volvo Award winner in clinical studies. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine (Phila Pa 1976) 1997;22(24):2807–2812. doi: 10.1097/00007632-199712150-00003. [DOI] [PubMed] [Google Scholar]
- 6.Kornblum MB, Fischgrund JS, Herkowitz HN, Abraham DA, Berkower DL, Ditkoff JS. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective long-term study comparing fusion and pseudarthrosis. Spine (Phila Pa 1976) 2004;29(7):726–733. doi: 10.1097/01.brs.0000119398.22620.92. [DOI] [PubMed] [Google Scholar]
- 7.Zdeblick TA. A prospective, randomized study of lumbar fusion: preliminary results. Spine (Phila Pa 1976) 1993;18(8):983–991. doi: 10.1097/00007632-199306150-00006. [DOI] [PubMed] [Google Scholar]
- 8.Bjarke Christensen F, Stender Hansen E, Laursen M, Thomsen K, Bünger CE. Long-term functional outcome of pedicle screw instrumentation as a support for posterolateral spinal fusion: randomized clinical study with a 5-year follow-up. Spine (Phila Pa 1976) 2002;27(12):1269–1277. doi: 10.1097/00007632-200206150-00006. [DOI] [PubMed] [Google Scholar]
- 9.Jackson RP, McManus AC. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size: a prospective controlled clinical study. Spine (Phila Pa 1976) 1994;19(14):1611–1618. doi: 10.1097/00007632-199407001-00010. [DOI] [PubMed] [Google Scholar]
- 10.Korsgaard M, Christensen FB, Thomsen K, Hansen ES, Bunger C. The influence of lumbar lordosis on spinal fusion and functional outcome after posterolateral spinal fusion with and without pedicle screw instrumentation. J Spinal Disord Tech. 2002;15(3):187–192. doi: 10.1097/00024720-200206000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Weinstein JN, Lurie JD, Olson PR, Bronner KK, Fisher ES. United States’ trends and regional variations in lumbar spine surgery: 1992–2003. Spine (Phila Pa 1976) 2006;31(23):2707–2714. doi: 10.1097/01.brs.0000248132.15231.fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rahm MD, Hall BB. Adjacent-segment degeneration after lumbar fusion with instrumentation: a retrospective study. J Spinal Disord. 1996;9(5):392–400. [PubMed] [Google Scholar]
- 13.Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976) 2004;29(17):1938–1944. doi: 10.1097/01.brs.0000137069.88904.03. [DOI] [PubMed] [Google Scholar]
- 14.Ghiselli G, Wang JC, Bhatia NN, Hsu WK, Dawson EG. Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am. 2004;86(7):1497–1503. doi: 10.2106/00004623-200407000-00020. [DOI] [PubMed] [Google Scholar]
- 15.Okuda S, Iwasaki M, Miyauchi A, Aono H, Morita M, Yamamoto T. Risk factors for adjacent segment degeneration after PLIF. Spine (Phila Pa 1976) 2004;29(14):1535–1540. doi: 10.1097/01.brs.0000131417.93637.9d. [DOI] [PubMed] [Google Scholar]
- 16.Inaoka M, Yamazaki Y, Hosono N, Tada K, Yonenobu K. Radiographic analysis of lumbar spine for low-back pain in the general population. Arch Orthop Trauma Surg. 2000;120(7–8):380–385. doi: 10.1007/pl00013766. [DOI] [PubMed] [Google Scholar]
- 17.Kumar MN, Baklanov A, Chopin D. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J. 2001;10(4):314–319. doi: 10.1007/s005860000239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Whitecloud TS, III, Davis JM, Olive PM. Operative treatment of the degenerated segment adjacent to a lumbar fusion. Spine (Phila Pa 1976) 1994;19(5):531–536. doi: 10.1097/00007632-199403000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Etebar S, Cahill DW. Risk factors for adjacent-segment failure following lumbar fixation with rigid instrumentation for degenerative instability. J Neurosurg. 1999;90(suppl 2):163–169. doi: 10.3171/spi.1999.90.2.0163. [DOI] [PubMed] [Google Scholar]
- 20.Chou WY, Hsu CJ, Chang WN, Wong CY. Adjacent segment degeneration after lumbar spinal posterolateral fusion with instrumentation in elderly patients. Arch Orthop Trauma Surg. 2002;122(1):39–43. doi: 10.1007/s004020100314. [DOI] [PubMed] [Google Scholar]
- 21.Katz JN, Lipson SJ, Lew RA, et al. Lumbar laminectomy alone or with instrumented or noninstrumented arthrodesis in degenerative lumbar spinal stenosis: patient selection, costs, and surgical outcomes. Spine (Phila Pa 1976) 1997;22(10):1123–1131. doi: 10.1097/00007632-199705150-00012. [DOI] [PubMed] [Google Scholar]