Introduction
Paragangliomas are rare neuroendocrine tumors associated with the sympathetic and parasympathetic system [1]. While they are known to occur anywhere in the body, they rarely affect the female genital tract. Here, we present a case of an 18-year-old female who presented to us with abnormal vaginal bleeding and was found to have a non-secretory vaginal paraganglioma.
Case History
An 18-year-old female presented with episodes of increased vaginal bleeding over a period of 2 months. She did not complain of bleeding from any other site and had no previous or family history of coagulopathy or bleeding disorders. On examination, her vitals were normal, but she was found to be pale. No mass was palpated. The patient was not sexually active and had an intact hymen, and so a complete pelvic examination could not be performed. Laboratory investigations revealed a hemoglobin level of 5.5 g/dL. Ultrasound (USG) of the pelvis and abdomen was performed and was unremarkable. The patient received blood transfusions. Magnetic resonance imaging (MRI) of the pelvis was ordered which showed a heterogenous polypoid lesion within the vaginal cavity measuring about 3 × 1.6 cm (Fig. 1). No extension into cervix or surrounding tissues was seen. A biopsy of the lesion was taken and revealed features suggestive of a well-differentiated neuroendocrine tumor, with sparse mitotic activity and mild ulceration of the overlying mucosa. Computed tomography (CT) imaging of the chest and abdomen was unremarkable, with no evidence of metastasis or a primary elsewhere. Urinary catecholamines and fractionated metanephrines were also normal. The patient was taken for surgery, and the mass was completely enucleated, en bloc. Histological sections of the mass showed tumor cells arranged in nests, separated by thin fibrous septa with granular cytoplasm and minimal nuclear pleomorphism (Fig. 2a, b). On immunohistochemistry (IHC), the tumor was positive for synaptophysin, chromogranin and negative for desmin, CD163 and AE1/AE3, an epithelial cell marker (Fig. 2c, d). A low Mib-1 score of 3–4% was reported. A diagnosis of non-functioning vaginal paraganglioma was made.
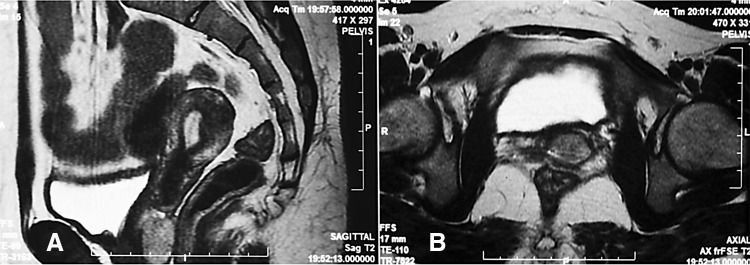
Fig. 1.
MRI pelvis showing a hyperintense mass on the posterior wall of vagina extending into corresponding fornix on T2-weighted images (a sagittal, b axial)
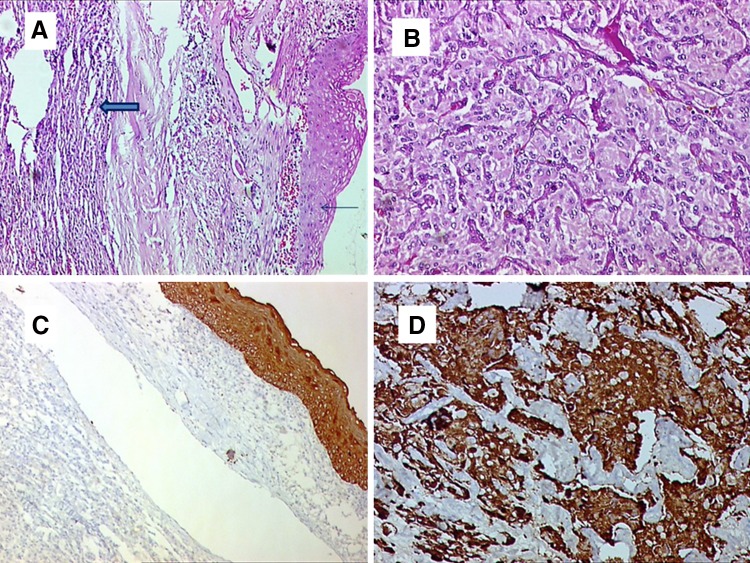
Fig. 2.
a Normal overlying squamous epithelial lining is seen (thin arrow) with lesion showing a nested tumor pattern (thick arrow) and stippled tumor nuclei (×40). b Increasing magnification showing nested pattern with nuclei that are relatively regular with minimal pleomorphism (×200). c Immunohistochemistry of the tumor shows AE1/AE3 marker (epithelial marker) negative in the tumor. The internal control of the overlying squamous epithelium is positive (×40). d Tumor staining positive for chromogranin (×200)
The patient was put on follow-up and has been asymptomatic for the last 5 months.
Discussion
Paragangliomas (PGL) are rare neuroendocrine tumors of the paraganglia and are associated with the sympathetic and parasympathetic system. They can be found in practically every site in which normal paraganglia are known to occur, with tumors arising from the adrenal medulla traditionally referred to as pheochromocytomas [1]. As such, they are rarely found in the female genital tract, with only 6 reported cases of vaginal paraganglioma in the literature [2].
Clinically, the presentation of paragangliomas varies depending upon the location and secretory nature of the tumor among others. PGL that secrete catecholamines often present with sympathetic symptoms such as headaches, hypertension and arrhythmias. Symptoms often worsen on manipulation of the lesion, a feature which has important implications in the preoperative care of these patients [3]. PGL occurring outside the adrenal gland are often associated with the parasympathetic system and do not secrete catecholamines [1].
Vaginal paragangliomas have certain unique features. Out of the 6 previously reported cases, half presented with abnormal vaginal bleeding and/or a vaginal mass (Table 1). Patients can also present with sympathetic symptoms during coitus or biopsy/surgery. In one previously reported case, during excision of what seemed to be a dormant mass, the patient suddenly landed in a hypertensive crisis, suggesting that even previously non-secretory lesions may release catecholamines during manipulation.
Table 1.
Vaginal paragangliomas reported in the literature
| References | Age | Secretory status | Presentation | Treatment |
|---|---|---|---|---|
| Cai et al. [2] | 17 | Secretory | Vaginal bleeding; HTN | Surgical excision |
| Mannelli et al. [3] | 65 | Non-secretory | Pelvic mass | Uterine artery embolization; surgical excision |
| Shen et al. | 38 | Secretory | Vaginal mass; HTN; palpitations | Surgical excision |
| Brustmann | 33 | Non-secretory | Vaginal bleeding | Surgical excision |
| Hassan et al. | 24 | Secretory | Vaginal mass, MI | Surgical excision |
| Parkes et al. | 11 | Non-secretory | Vaginal bleeding | Surgical excision |
| Akhtar et al. | 18 | Non-secretory | Vaginal bleeding | Surgical excision |
HTN hypertension, MI myocardial infarction
Establishing a diagnosis of a vaginal paraganglioma preoperatively can be challenging. Of 7 cases, 3 presented with symptoms of catecholamine excess. A blood or urine assay to determine metanephrines or noradrenaline may be helpful in such patients. Radiological features cannot distinguish a vaginal paraganglioma from other more common lesions in the vaginal wall such as a smooth muscle tumor [2]. Pelvic USG can be unremarkable, such as in our case. A CT scan or MRI can help demarcate the size and extent of the lesion. In addition, contrast-enhanced CT scan may show increased vascularity of the mass prompting less invasive strategies such as uterine artery embolization prior to biopsy or excision. An FDG-PET/CT scan can reveal increased uptake in the lesion and help identify metastatic lesions.
Histopathology is essential for a definitive diagnosis. Histologically, lesions resemble paragangliomas elsewhere with cells often arranged in a characteristic nesting pattern (zellballen) with prominent vascular slit like spaces in between nests [1]. On immunohistochemistry, positivity for chromogranin, synaptophysin, neuron-specific enolase and S-100 has been consistently observed. Ultrastructural examination may reveal neurosecretory granules.
Surgical excision is the definitive treatment for a vaginal paraganglioma. In one case, embolization of the uterine artery was performed prior to excision of a highly vascular mass. Preoperative alpha blockade therapy is practiced regularly [4].
A diagnosis of vaginal paraganglioma generally portends a good prognosis. All of the reported cases had an unremarkable follow-up period with no reports of metastasis or spread.
In conclusion, vaginal paragangliomas are rare tumors of the vaginal tract. A diagnosis may be considered in a patient with abnormal vaginal bleeding, symptoms of sympathetic overactivity during coitus or pelvic examination, with increased vascularity on CT scan. Adequate preoperative care can prevent complications such as hypertensive crisis or arrhythmias during surgery or biopsy.
Othman Salim Akhtar, M.D.
completed his training as a pathologist at SKIMS, Srinagar, before moving to Weill Cornell Medical Center in New York City where he joined the laboratory of Prof. Ari Melnick, carrying out research in lymphomas for 1 year. He returned to Hakim Sanaullah Cancer Center, a rural Cancer Center in North Kashmir, for a brief period to help establish diagnostic facilities there, before joining as a resident physician at the University at Buffalo, Buffalo, NY, USA.
Compliance with Ethical Standards
Conflict of interest
The authors report no conflict of interest.
Informed Consent
Informed consent was obtained from the patient to prepare this manuscript. No personal information is shared in the description of this case, and no experiments were carried out on the patient.
Footnotes
Othman Salim Akhtar is a Resident at University at Buffalo; Kedar K. Deodhar is a Professor, Department of Pathology at Tata Memorial Hospital; Anupurva Dutta is a Senior Resident, Department of Pathology at Tata Memorial Hospital; Farhat Jabeen is a Associate Professor, Department of Obstetrics and Gynecology at Government Medical College; Shad Salim Akhtar is a Professor of Medicine, Director at Hakim Sanaullah Cancer Centre.
References
- 1.Rosai J. Adrenal gland and other paraganglia. In: Rosai J, editor. Rosai and Ackerman’s surgical pathology. USA: Elsevier; 2011. p. 1082. [Google Scholar]
- 2.Cai T, Li Y, Jiang Q, et al. Paraganglioma of the vagina: a case report and review of the literature. Onco Targets Ther. 2014;7:965–968. doi: 10.2147/OTT.S62174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mannelli M, Dralle H, Lenders JW. Perioperative management of pheochromocytoma/paraganglioma: is there a state of the art? Horm Metab Res. 2012;44(5):373–378. doi: 10.1055/s-0032-1306275. [DOI] [PubMed] [Google Scholar]
- 4.Fishbein L, Orlowski R, Cohen D. Pheochromocytoma/paraganglioma: review of perioperative management of blood pressure and update on genetic mutations associated with pheochromocytoma. J Clin Hypertens (Greenwich) 2013;15(6):428–434. doi: 10.1111/jch.12084. [DOI] [PMC free article] [PubMed] [Google Scholar]