Abstract
Objectives
To compare the incidence of visible strings after postplacental intracesarean insertion of Cu375 and CuT380A intrauterine contraceptive devices (IUD).
Methods
This was a prospective, randomized comparative study. A total of 100 women fulfilling the inclusion and exclusion criteria underwent postplacental intracesarean insertion of either Cu375 IUD or CuT380A IUD. Women were followed up at 1, 6 weeks and 3 months after IUD insertion and were questioned about IUD expulsion or removal at each visit. The cervix was inspected to visualize the IUD strings. Data were analyzed by Chi-square test.
Results
At 6-week follow-up, 97.9% women in group A versus 41.7% women in group B had strings visible at the cervical os and at 3 months 100% women in group A versus only 47.9% women in group B (p < 0.001) had visible strings of IUD.
Conclusion
Both Cu375 and CuT380A IUD are safe postpartum method of contraception but Cu375 if used for intracesarean IUD insertion increases the incidence of visible IUD strings. Hence, it avoids radiological investigations and invasive procedures at follow-up visits required to locate the IUD when strings are not visible.
CTRI No. CTRI/2015/09/006221.
Keywords: Postpartum contraception, CuT380A IUD, Cu375 IUD, String visibility, Intracesarean PPIUD
Introduction
The immediate postpartum intrauterine device (PPIUD) insertion is safe, effective, long acting, reversible method of postpartum contraception and does not interfere with breast feeding [1–3]. Pregnancy with short interconceptional period after cesarean section carries the increased risk of morbidity. Cesarean delivery gives opportunity to obstetrician to counsel woman for PPIUD usage [4, 5]. Intracesarean intrauterine device (IUD) insertion can be done under vision, thus obviating fear of perforation of uterus [5].
After removal of placenta, fundus of the uterus corresponds to 5-month pregnant uterine size. Therefore, in significant number of women, strings of CuT380A IUD are not visible, especially after intracesarean insertions [3, 6–9]. Involution of uterus makes IUD strings descend and become visible. Dewan et al. [9] reported the reason for non-visibility of PPIUD strings to be non-descent in all cases. Non-visibility of PPIUD strings is a source of apprehension as women are concerned about possible rare complication of perforation of IUD into abdominal cavity [6, 7, 9, 10]. This myth gets momentum when women are informed about non-visualization of IUD strings at follow-up visits leading to request for premature removal of otherwise well-placed IUD [11]. Dewan et al. [9] reported that 40% women with non-visible strings who requested the removal of well-placed IUD had intracesarean CuT380A IUD insertions. Despite the fact that IUD services are provided free of cost in India, non-visibility of PPIUD strings has limited its use [7].
During follow-up visit, visualization of PPIUD strings rules out expulsion and reassures both service provider and women about in utero presence of IUD [6]. Also the removal of IUD with visible strings is easy, requiring simply grasping the strings and pulling gently [6, 10].
Majority of IUD with missing strings can be retrieved in office setting. Invasive methods like hysteroscopy may be required which is stressful for woman and service provider. It also has financial impact due to loss of wages in multiple hospital visits [9, 10].
The length of strings of CuT380A IUD (HLL Lifecare Limited, India) is 11.5 cm, whereas Cu375 IUD has longer nylon thread of 19.4 cm (Pregna International Limited, India). Non-visualization of CuT380A IUD strings at follow-up visits is due to its short strings [5, 6, 8, 12, 13]. Therefore, postplacental insertion of Cu375 IUD following cesarean delivery may lead to string visibility at cervical os in more number of women. At present, there are few studies in the literature that deal with visibility of IUD strings in women undergoing intracesarean PPIUD insertion [5, 6, 8, 9, 12, 13]. Hence, the present study was planned to see whether intracesarean Cu375 IUD insertion solves the problem of missing IUD strings at follow-up visits. The objective was to compare the incidence of visible strings of Cu375 and CuT380A IUD after postplacental intracesarean insertions.
Materials and Methods
Study Design
This was a prospective, randomized comparative study conducted in Department of Obstetrics and Gynaecology at Safdarjang Hospital, Delhi, India, from June 2015 to November 2015 after getting approval from Institutional ethical board.
Assuming visibility of strings at 6-week follow-up visit of CuT380A IUD [6] to be 62% and Cu375 IUD [5] to be 92%, α to be 5%, power 90%, a sample of 40 per group was required for the study. Adding 25% to be lost to follow-up, a sample of 50 women per group was taken in the study.
Study Participants
Women were recruited in study when they were admitted to antenatal ward for cesarean delivery. Women were counseled about different postpartum family planning methods regarding advantages and side effects. Eligible women interested in getting PPIUD insertion were given a participant information sheet, and written informed consent was taken. First assessment was done during screening visit where a detailed history was undertaken to rule out women belonging to World Health Organization’s IUD Medical Eligibility Criteria category 3 or 4 [1].
Inclusion criteria were women over 18 years of age, scheduled for elective cesarean delivery, opting for PPIUD contraception for less than or up to 5 years and willing to come for follow-up.
Second assessment was undertaken during cesarean to check for the exclusion criteria. Participants with postpartum hemorrhage, fever in recent antepartum period and history of leaking per vaginum for more than 18 h were excluded.
Study participants were assigned randomly into Cu375 IUD group and CuT380A IUD group. The arm allocation was done using computer-generated table of random numbers. The randomization assignment was kept inside opaque, sealed envelope. The next envelope in sequence was opened by the obstetrician, and arm allocation was determined.
All cesarean deliveries were performed by a study investigator. In either group, intracesarean postplacental insertion of Cu375/CuT380A IUD was done manually through the uterine incision placing the IUD at the fundus and strings were guided by fingers through the cervical canal from inside the uterus. Strings were trimmed if visible at vulva during vaginal toileting.
High vaginal swab culture was sent at 48 h postoperative. Antibiotics were administered, and women were kept under observation for evidence of postpartum hemorrhage or sepsis for 72 h postcesarean as per the hospital protocol for cesarean section. Before discharge, postinsertion counseling was done. She was explained regarding IUD side effects and normal postpartum symptoms. Women were told to come back if she experiences foul smelling vaginal discharge, lower abdominal pain with fever and if IUD has fallen out.
Follow-Up Visits
Women were advised to return for scheduled follow-up visits at 1, 6 weeks and 3 months postpartum. At each follow-up visit, women were interviewed in a prestructured proforma about any complaints, menstrual history, and abdominal and speculum examination was done to verify the presence of IUD. Strings were cut short to 2 cm from external os if IUD strings were found to be long. If strings were not visible, ultrasound was done to confirm in utero presence of IUD. Women with IUD expulsion or any other complication were treated accordingly.
Data Analysis
The primary outcome variable included string visibility at each follow-up visit. Secondary outcome variables were number of women with complaints of pelvic pain, heavy menstrual bleeding, pelvic infection, expulsion, invasive procedure and complications like uterine perforation. Complete expulsion was defined as no IUD inside the uterus confirmed on ultrasound. Partial expulsion was defined as an IUD limb protruding through the cervical os. Complete/partial expulsions were not counted in visibility/non-visibility of strings and were excluded from the denominator. Pelvic infection was considered to be present if women had cervical, adnexal, or uterine tenderness, purulent discharge, with or without fever.
Statistical analysis was done by using Chi-square test to analyze the difference between the variables of two groups Cu375 IUD and CuT380A IUD. Significance level was set at p < 0.05. SPSS version 19 for Windows statistical software was used for all the computations.
Results
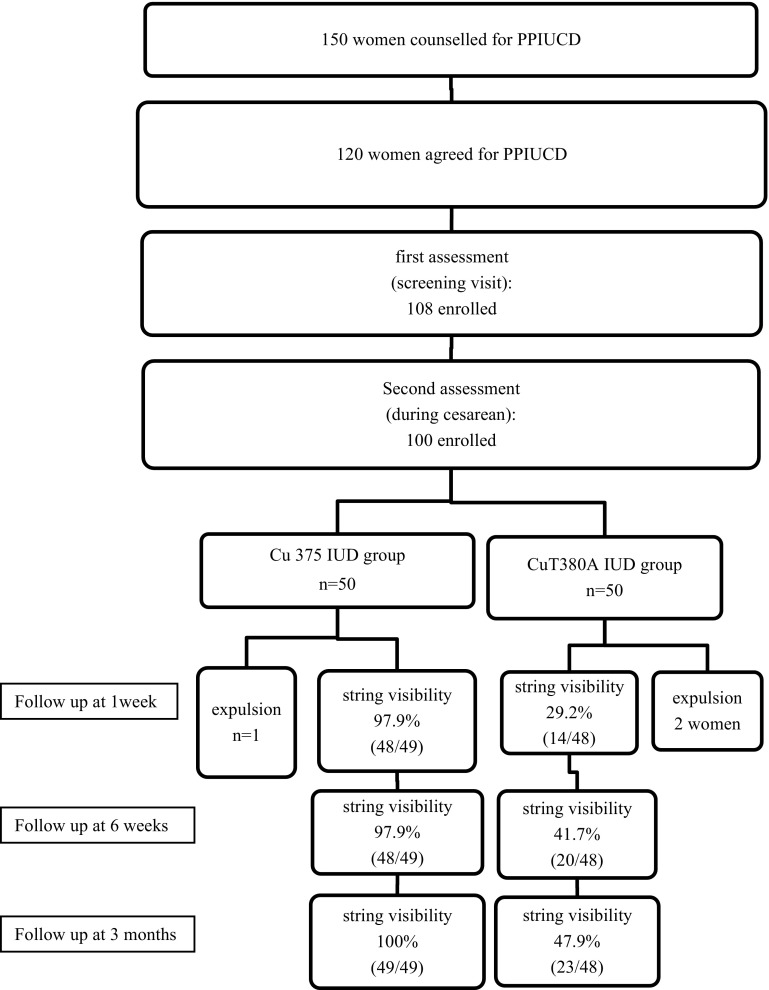
A total of 100 eligible women were recruited and randomly assigned into Cu375 IUD and CuT380A IUD group, each consisting of 50 women (Fig. 1). Mean age, literacy and socioeconomic status were comparable between the two groups (Table 1).
Fig. 1.
Flowchart
Table 1.
Demographic characteristics
| Characteristics | Cu 375 (n = 50) | CuT380A (n = 50) | p value |
|---|---|---|---|
| Age (years) | 22.85 ± 2.59 | 23.4 ± 2.26 | 0.051 |
| Education | |||
| Illiterate | 21 (42%) | 22 (44%) | 0.84 |
| Socioeconomic status | |||
| Low | 35 (70%) | 37 (74%) | 0.65 |
| Middle | 15 (30%) | 13 (26%) | 0.65 |
All 100 women attended the first follow-up visit at 1 week. Strings were visible in 97.9% (48/49) women in Cu375 IUD group and in only 29.2% (14/48) women in CuT380A IUD group at 1 week. The difference was statistically significant (p < 0.001). Visibility of IUD strings increased at successive follow-up visits. String visibility was 97.9% (48/49) in Cu375 IUD group and 41.7% (20/48) in CuT380A IUD group at 6 weeks (p < 0.001). At 3-month follow-up, string visibility of Cu375 IUD was 100% (49/49) compared to 47.9% (23/48) in CuT380A IUD group which was statistically significant (p < 0.001).
The presence of IUD in the uterus was confirmed by transvaginal sonography in cases of non-visibility of strings in both the groups. Non-visibility of IUD strings was due to complete expulsion in 2(4%) women in CuT380A IUD group at 1-week follow-up. These were noticed by women themselves. There was one case of partial expulsion detected on speculum examination in Cu375 IUD group. Woman had accidently pulled the protruding strings of Cu375 IUD. IUD was found in cervical canal which was removed. All 3 women who had expelled IUD were counseled for IUD reinsertion at 6 weeks which they accepted.
There was no case of expulsion in either group at 6-week and 3-month follow-ups. Non-visibility of IUD strings in all women at 6 weeks and 3 months was due to non-descent of strings. There was no case of removal, misplaced IUD or uterus perforation in either group.
There was no case of pelvic infection in either group (confirmed on clinical examination and high vaginal swab culture). Few women had heavy bleeding and pelvic pain at 1 week, got relieved by tranexamic acid and pain killers. None of the women had persistent heavy bleeding or pelvic pain at 6-week and 3-month follow-up visits (Table 2). The continuation rates at 3 months were 98 and 96% in Cu375 and CuT380A IUD group, respectively.
Table 2.
Findings of follow-up at 1 week
| Adverse events | Cu 375 (n = 50) | CuT380A (n = 50) | p value |
|---|---|---|---|
| Heavy bleeding | 5 (10%) | 6 (12%) | 0.75 |
| Pelvic pain | 7 (14%) | 6 (12%) | 0.77 |
| Pelvic infection | 0 | 0 | |
| Expulsion | 1 (2%) | 2 (4%) | 0.56 |
Discussion
The first follow-up visit was planned at 1 week as this coincided with postnatal visit for stitch removal in cesarean patients. Majority of women with Cu375 IUD insertion complained of strings protruding out of vulva which was cut short up to 2 cm from the level of external os. None of the women in CuT380A IUD insertions either complained of protruding strings or required shortening of strings. Present study had low expulsion rate of IUDs (4% in CuT380A and 2% in Cu375 IUD). Studies indicate that expulsion rates after intracesarean IUD insertion are much lower, probably because placement at the fundus is ensured and the cervical os is less likely to be fully dilated [5, 6].
Second postnatal visit was planned at 6 weeks with assumption that by 6 weeks, uterine involution, descent of strings and expulsions if any would have occurred. Present study showed string visibility to be significantly higher in Cu375 IUD insertions which increased at successive follow-up visits. Strings were visualized in all (100%) Cu375 IUD insertions and nearly half (47.9%) of CuT380A IUD insertions at 3-month follow-up visit.
Reason for non-visibility of strings was non-descent in all the women of both the groups as confirmed by pelvic sonography. Dewan et al. [9] also found the reason for non-visibility of strings to be non-descent of the strings and hypothesized that in many cases strings may become curled up and not be seen at the cervical os. There was no case of misplaced IUD or perforation observed in our study. Also, there are no reports of perforation with postpartum insertion of IUD in the literature [5, 6, 8, 13].
Studies have reported low visibility of strings following CuT380A IUD intracesarean insertions. Dewan et al. [9] reported 32.1 and 56.8% string visibility of CuT380A IUD at 3- and 6-month follow-up visits, respectively. They proposed that uterus involution and resumption of menstruation may be a contributing factor for increased string visibility with the passage of time. Lucksom et al. [12] observed tail visibility of 10% at 6 weeks which increased to 41% at 3-month follow-up visit. Lester et al. [8] found strings were visible in only 44% of women in follow-up visit at 6 months with CuT380A IUD inserted intracesarean. Singal et al. [6] found strings were visible in 62 and 71% women at 1- and 3-month follow-up visits, respectively, after CuT380A IUD intracesarean insertions. Higher string visibility reported by Singal et al. [6] may be due to inclusion of emergency cases, whereas our study included only elective cesarean cases.
In contrast to CuT380A IUD intracesarean studies, there are few studies in the literature which studied clinical outcome of Cu375 IUD intracesarean insertions. All of them reported higher string visibility at follow-up visits. Bhutta et al. [5] reported thread visibility in 92% women at 6-week follow-up visit after intracesarean Cu375 IUD insertions. Also, Farhat et al. [13] in his study on intracesarean Cu375 IUD insertions found 94.7 and 96.3% women had thread visibility at 6-week and 3-month follow-up visits. Similarly, present study showed string visibility in 97.9% women at 6 weeks and in 100% women at 3-month follow-up visit [5, 6, 8, 10, 12, 13]. Possible reason of higher string visibility in Cu375 IUD group may be longer string length of Cu375 IUD.
Dewan et al. [9] and Lester et al. [8] regarded non-visualization of CuT380A IUD strings to be a major deterrent in optimal utilization of this effective family planning method. Visibility of PPIUD strings at follow-up visits is likely to lead to increased acceptance and continuation rate in eligible woman. Result of Farhat et al., Bhutta et al. [5, 13] and present study also suggest Cu375 IUD insertion, with long strings at cesarean section, may improve string visibility.
None of the woman had persistent heavy bleeding or pelvic infection in present study after intracesarean insertion of Cu375 or CuT380A IUD. Studies of various non-hormonal IUDs have also shown no increased risk of infection or other adverse events with intracesarean inserted PPIUD compared to delayed insertion [6, 7, 10, 11].
The merits of the study are that it is the first randomized comparative study and has found solution to non-visibility of strings in intracesarean inserted PPIUD. The limitations of our study are small sample size with a follow-up of 3 months.
To conclude, both Cu375 IUD and CuT380A IUD are safe postpartum method of contraception, available free of cost in Government supply. Cu375 if used for intracesarean IUD insertion solves the problem of non-visibility of strings and avoids radiological investigations and invasive procedures at follow-up visits required to locate IUD in the case of non-visible strings, thus leading to the increased utilization of IUD in eligible women.
Therefore, we recommend intracesarean Cu375 IUD insertion as a highly effective, safe and convenient method of postpartum contraception to address the unmet need of family planning in developing countries like India where woman do not come for postnatal contraception.
Kavita Agarwal
She is working as Assistant Professor, Department of Obstetrics and Gynaecology, Safdarjung Hospital, Delhi. She was awarded first prize, FOGSI Dr. C.S. Dawn prize at AICOG, Agra. She won All Rounder YUVA trophy in North Zone Yuva FOGSI 2016, was awarded Dr. APJ Abdul Kalam’s appreciation award and received Certificate of Excellence award on Women’s day. She was given Certificate of Appreciation Award for valuable contribution in the Community Health Intervention Programme and has received many prizes in various national and international conferences. She has 19 publications in various reputed journals. Participated as speaker, chairperson and panelist in various conferences. Her field of interest is infertility and reproductive endocrinology.
Compliance with Ethical Standards
Conflict of interest
Dr. Kavita Agarwal, Dr. Rupali Dewan, Dr. Pratima Mittal and Dr. Abha Aggarwal declare that they have no conflict of interest.
Ethical Approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed Consent
Informed consent was obtained from all patients for being included in the study.
Footnotes
Dr. Kavita Agarwal is a Assistant Professor in Department of Obstetrics and Gynaecology, Safdarjung Hospital, New Delhi; Dr. Rupali Dewan is a Professor and Consultant in Department of Obstetrics and Gynaecology, Safdarjung Hospital, New Delhi; Dr. Pratima Mittal is a Professor and Head of Department in Department of Obstetrics and Gynaecology, Safdarjung Hospital, New Delhi; Dr. Abha Aggarwal is a Scientist F in NIMS, India.
References
- 1.World Health Organization . Medical eligibility criteria for contraceptive use. 5. Geneva: World Health Organization; 2015. [PubMed] [Google Scholar]
- 2.Goldstuck ND, Steyn PS. Intrauterine contraception after cesarean section and during lactation: a systematic review. Int J Women Health. 2013;5:811–818. doi: 10.2147/IJWH.S53845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Levi E, et al. Immediate postplacental IUD insertion at cesarean delivery: a prospective cohort study. Contraception. 2012;86:102. doi: 10.1016/j.contraception.2011.11.019. [DOI] [PubMed] [Google Scholar]
- 4.Fox MC, Oat-Judge J, Severson K, et al. Immediate placement of intraiuterine devices after first and second trimester pregnancy termination. Contraception. 2011;83:34–40. doi: 10.1016/j.contraception.2010.06.018. [DOI] [PubMed] [Google Scholar]
- 5.Bhutta SZ, Butt IJ, Bano K. Insertion of intrauterine contraceptive device at cesarean section. J Coll Phys Surg Pak. 2011;21(9):527–530. [PubMed] [Google Scholar]
- 6.Singal S, Bharti R, Dewan R, et al. Clinical outcome of post placental Copper T 380A insertion in women delivering by cesarean section. J Clin Diagn Res. 2014;8(9):OC01–OC04. doi: 10.7860/JCDR/2014/10274.4786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gutgutia I, et al. Comparative evaluation of Postpartum versus post MTP insertion of intrauterine contraceptive device. Int J Reprod Contracept Obstet Gynecol. 2015;4(1):23–29. [Google Scholar]
- 8.Lester F, Kakaire O, Byamugisha J. Intracesarean insertion of CuT380A versus 6 weeks postcesarean: a randomized clinical trial. Contraception. 2015;91:198–203. doi: 10.1016/j.contraception.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 9.Dewan R, Dewan A, Singal S, et al. Non-visualisation of strings after postplacental insertion of Copper- T 380A intrauterine device. J Fam Plan Reprod Health Care. 2016;0:1–9. doi: 10.1136/jfprhc-2015-101200. [DOI] [PubMed] [Google Scholar]
- 10.Prabhakaran S, Chuang A. In office retrieval of intrauterine contraceptive devices with missing strings. Contraception. 2011;83(2):102–106. doi: 10.1016/j.contraception.2010.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mishra S. Evaluation of safety, efficacy and expulsion of post-placental and Intra cesarean insertion of intrauterine contraceptive devices. J Obstet Gynecol India. 2014;64(5):337–343. doi: 10.1007/s13224-014-0550-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lucksom PG, Kanungo BK, Sebastian N, et al. Comparative study of interval versus postpartum Cu-T insertion in a central referral hospital of North East India. Int J Reprod Contracept Obstet Gynecol. 2015;4(1):47–51. [Google Scholar]
- 13.Arshad F, Ejaz L, Noreen H, et al. Trans cesarean insertion of intrauterine contraceptive device. JSOGP. 2014;4:73–78. [Google Scholar]