Abstract
Objective:
To conduct a systematic review with meta-analysis assessing the effectiveness of conservative rehabilitation programs for improving health-related quality of life (HRQL) in individuals with chronic ankle instability (CAI).
Data Sources:
PubMed, MEDLINE, CINAHL, and SPORTDiscus were searched from inception to January 2016.
Study Selection:
Studies were included if the researchers examined the effects of a conservative rehabilitation protocol in individuals with CAI, used validated patient-reported outcomes (PROs) to quantify participant-perceived HRQL, and provided adequate data to calculate the effect sizes (ESs) and 95% confidence intervals (CIs). Studies were excluded if the authors evaluated surgical interventions, prophylactic taping, or bracing applications or examined only the immediate effects of 1 treatment session.
Data Extraction:
Two investigators independently assessed methodologic quality using the Physiotherapy Evidence Database (PEDro) Scale. Studies were considered low quality if fewer than 60% of the criteria were met. Level of evidence was assessed using the Strength of Recommendation Taxonomy. Preintervention and postintervention sample sizes, means, and standard deviations of PROs were extracted.
Data Synthesis:
A total of 15 studies provided 24 participant groups that were included in the analysis. Seven high-quality studies with a median PEDro score of 50% (range = 10%−80%) and a median level of evidence of 2 (range = 1−2) were identified. The magnitudes of preintervention to postintervention PRO differences were examined using bias-corrected Hedges g ESs. Random-effects meta-analysis was performed to synthesize PRO changes across all participant groups. Positive ES values indicated better PRO scores at postintervention than at preintervention. The α level was set at .05. Meta-analysis revealed a strong ES with a nonoverlapping 95% CI (ES = 1.20, CI = 0.80, 1.60; P < .001), indicating HRQL improved after conservative rehabilitation.
Conclusions:
Based on the quality of the evidence and the results of the meta-analysis, grade A evidence showed that conservative rehabilitation produces large improvements in HRQL for people with CAI.
Key Words: patient-reported outcomes, conservative care, ankle sprains
Key Points
Balance training demonstrated a high level of evidence and the largest summary effect, indicating it may be the most appropriate rehabilitation strategy to improve health-related quality of life (HRQL) in individuals with chronic ankle instability (CAI).
Manual therapy may improve HRQL in people with CAI.
Future researchers should evaluate the effectiveness of impairment-based treatment paradigms for improving HRQL in individuals with CAI.
Chronic ankle instability (CAI) is a condition characterized by residual symptoms after 1 or more acute ankle sprains.1 These residual symptoms include episodes of “giving way,” a sensation of instability, recurrent ankle sprains, and functional deficits.1 Acute ankle sprains, which spur the development of CAI, are one of the most common orthopaedic injuries, with more than 600 000 occurring each year in the United States.2 Whereas ankle sprains are considered minor injuries, with about 50% resolving within 7 days,3 32% to 74% of patients will develop CAI.4,5 Given the frequency of ankle sprains, this scenario creates an enormous health care burden.2,6 This burden is further exacerbated by the association between CAI and decreased physical activity levels7 and the increased risk of posttraumatic ankle osteoarthritis.8 Therefore, evidence-based rehabilitation interventions capable of mitigating the effects of CAI are needed.
Conventionally, conservative rehabilitation for individuals with CAI has focused on addressing disease-oriented measures related to the mechanical and sensorimotor impairments that are the common clinical manifestations of this condition. However, the growing adoption of evidence-based practice (EBP) has emphasized the need to incorporate patient-oriented outcomes when evaluating the effectiveness of an intervention.9 Patient-oriented outcomes evaluate a patient's health status and the effectiveness of a treatment based on the patient's perspective.9 One essential aspect of patient-oriented outcomes is evaluating health-related quality of life (HRQL), a multidimensional concept that incorporates physical, psychological, and social domains and is often affected by individual experiences and perceptions.10
Patient-reported outcomes (PROs) are used to capture the perceptions that individuals have about their health status. Patient-reported outcome instruments that assess ankle-specific function, overall health, and fear of reinjury have identified HRQL impairments in those with CAI compared with individuals who do not have CAI.11 In many investigations, researchers have primarily used region-specific PROs to examine the effects of rehabilitation in individuals with CAI to gain a patient-oriented perspective of physical function. However, drawing conclusions about the patient-oriented effects of these interventions is difficult, as a wide variety of rehabilitation strategies and region-specific PRO instruments have been examined. To our knowledge, no authors have performed a comprehensive systematic review to examine the effects of conservative rehabilitation on PROs in individuals with CAI. Conducting a systematic review of the literature with a corresponding meta-analysis may offer a greater understanding of the effectiveness of the currently available CAI rehabilitation interventions to improve HRQL. Therefore, the purpose of our systematic review with meta-analysis was to collect, critically appraise, and provide a synthesis of the published evidence to assess the effects of CAI rehabilitation interventions on HRQL.
METHODS
Search Strategy
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines to perform a systematic search to locate studies in which investigators evaluated the effect of a conservative rehabilitation intervention on PROs in individuals with CAI.12 We searched PubMed and EBSCO Host (CINAHL, MEDLINE, SPORTDiscus) from their inception through January 27, 2016. Electronic databases were searched using combinations of key words related to the research question (Table 1). The Boolean operators OR, AND, and NOT were used to combine search terms, and the search was limited to human studies and manuscripts written in English. The reference lists of articles screened during the systematic search were hand searched for additional publications. The constructed Boolean phrase, systematic search, and hand search were completed by 2 investigators (C.J.P., M.C.H.).
Table 1. .
Search Strategy
| Step |
Search Terms |
Boolean Operator |
EBSCO Host |
PubMed |
| 1 | Chronic ankle instability | OR | 1933 | 733 |
| Functional ankle instability | ||||
| Ankle instability | ||||
| 2 | Rehabilitation | OR | 2 875 934 | 7 288 050 |
| Treatment | ||||
| Balance | ||||
| Postural control | ||||
| Mobilization | ||||
| Strength | ||||
| 3 | Surgery | OR | 1 885 167 | 2 404 068 |
| Surgical | ||||
| 4 | 1, 2 | AND | 624 | 577 |
| 5 | 3, 4 | NOT | 421 | 242 |
| Duplicates | 217a | |||
| Total identified | 446 |
Total number of duplicates between EBSCO and PubMed.
Selection Criteria
The eligibility of articles identified by the systematic search was determined by 2 authors (C.J.P., M.C.H.) using specific inclusion and exclusion criteria. Initially, the titles and abstracts of all articles were screened for eligibility. When eligibility could not be determined during the initial screen, the full text of the manuscript was examined.
Inclusion Criteria.
The following inclusion criteria were used to select and screen studies: (1) articles in which the primary aim of the investigation was to examine the effects of a conservative rehabilitation intervention for individuals with CAI; (2) articles involving human participants described as having a history of at least 1 ankle sprain and classified as having CAI, functional ankle instability, mechanical ankle instability, or recurrent ankle sprains; (3) articles including validated multi-item PROs used to quantify the patients' perceived changes due to treatment; and (4) peer-reviewed, full-text articles.
Exclusion Criteria.
The following exclusion criteria were used to screen studies: (1) articles that did not include validated PROs to assess self-perceived function before and after a conservative rehabilitation program; (2) articles in which sufficient data to calculate effect sizes (ESs; eg, mean, standard deviation) were not reported or provided; (3) articles in which evaluated treatments included only the application of tape, braces, orthotic devices, or therapeutic modalities; (4) articles that evaluated the effects of an intervention immediately after 1 application; (5) articles that were not published in English; or (6) articles that were case studies, case reviews, editorials, commentaries, guidelines, or reviews.
Methodologic Quality
The Physiotherapy Evidence Database (PEDro) scale13 was used to assess the methodologic quality of the included studies. This scale has demonstrated acceptable reliability (intraclass correlation coefficient = 0.68).13 The PEDro is a 10-item scale designed to determine the methodologic quality of randomized control trials by assessing their internal validity. Each item is scored as yes or no. Studies that scored equal to or greater than 60% of the PEDro items as yes were deemed high-quality evidence.14 Included studies were initially scored independently by 2 reviewers (C.J.P., M.C.H.). After independent scoring, the 2 reviewers met to resolve any disagreements. If a disagreement could not be resolved, a third reviewer (J.M.H.) was consulted. The percentage of agreement among the reviewers was calculated for each PEDro item.
Data Extraction
During the initial review of the included studies, 2 independent reviewers (C.J.P., M.C.H.) extracted data, including study aims, study designs, study quality, inclusion criteria, participant characteristics, clinician details, intervention procedures, outcome assessments, statistical techniques, conclusions, and relevant methodologic limitations. Discrepancies in interpretation were resolved by discussion until a consensus was achieved. If a consensus could not be achieved, a third reviewer (J.M.H.) was consulted.
The primary outcome of interest for this systematic review was PRO scores. Only preintervention and postintervention PRO scores were extracted for intervention groups. During the extraction of PRO scores, the Foot and Ankle Disability Index (FADI)–Sport subscale identified in the literature was reported as the Foot and Ankle Ability Measure (FAAM)–Sport in this review because the 2 instruments contained the same questions.
To further classify the included studies, we created a moderator variable to examine specific types of rehabilitation reported in the literature. The moderator variable rehabilitation type refers to the nature of interventions that were conducted. Four levels were coded for rehabilitation type: balance training, manual therapy, strength training, and combination. Balance-training rehabilitation was used to describe studies that included rehabilitation protocols involving tasks that challenged the participants' ability to maintain static or dynamic balance. Manual-therapy studies investigated interventions in which hands-on manual-therapy techniques (eg, mobilizations, massage) were applied to the lower extremity. Strength-training studies examined interventions primarily designed to strengthen the lower extremity. Finally, studies classified as combination used a mixture of rehabilitation approaches in which participants underwent conservative rehabilitation that consisted of 2 or more of the interventions. Studies included in this review may have incorporated multiple intervention groups within the study; therefore, the outcomes were categorized according to the different rehabilitation types.
Statistical Analysis
Separate meta-analyses were performed for the overall effect and each rehabilitation type. For each meta-analysis, we used a random-effects model in which individual study measures were pooled using bias-corrected Hedges g ESs and 95% confidence intervals (CIs) to determine the magnitude of change in patient-oriented outcomes in individuals with CAI from preintervention to postintervention. The Hedges g ES is a unitless measure that is corrected for sample size to represent an effect that exists on a parametric distribution.15 A positive ES indicated that PRO scores improved from preintervention to postintervention. In most studies, investigators used both the FAAM/FADI activities of daily living (ADL) subscale and the FAAM–Sport. The average FAAM/FADI–ADL ES (0.88) and the average FAAM–Sport ES (0.88) of the included studies were very similar; therefore, when both instruments were reported, the values were pooled for analysis to reduce sample-size inflation. For studies in which multiple rehabilitation types were examined, each group was treated independently in the analyses. All meta-analysis procedures were performed in Comprehensive Meta-Analysis software (version 2.0; BioStat, Englewood, NJ). Effect sizes were interpreted as weak (≤0.40), moderate (0.41−0.69), or strong (≥0.70).15 The α level was set a priori at .05. Further data analysis was performed via a qualitative assessment of ES estimates between rehabilitation types and determining if CIs crossed zero.
Assessment of Publication Bias
Assessment of the robustness of the observed overall effect on PRO change was completed using the Orwin fail-safe N test. This test determines the number of studies with trivial findings that would be needed to nullify the pooled ES of the included studies. A funnel plot of all included comparisons was generated to assess the likelihood of publication bias. To further assess publication bias, we also used the trim-and-fill method of imputing missing studies.
Sensitivity Analysis
To assess the sensitivity of the results to the influence of a single participant group, we completed a 1-study-removed analysis. This method repeats the meta-analysis multiple times, with 1 participant group removed each time to determine if the observed effect was affected. A 1-study-removed analysis was completed for the overall effect and each rehabilitation type.
Level of Evidence
We used the Strength-of-Recommendation Taxonomy (SORT) to assess the level of evidence and provide an overall grade of recommendation.16 Level 1 evidence was considered good-quality, patient-oriented evidence; level 2 evidence was considered limited-quality, patient-oriented evidence; and level 3 was considered other evidence.16 The SORT guidelines for strength of recommendation consider grade A to be consistent, good-quality, patient-oriented evidence; grade B, inconsistent or limited-quality, patient-oriented evidence; and grade C, consensus, disease-oriented evidence; and so on.16 For this systematic review, 3 or more high-quality studies were required to provide grade A evidence.
RESULTS
Literature Search
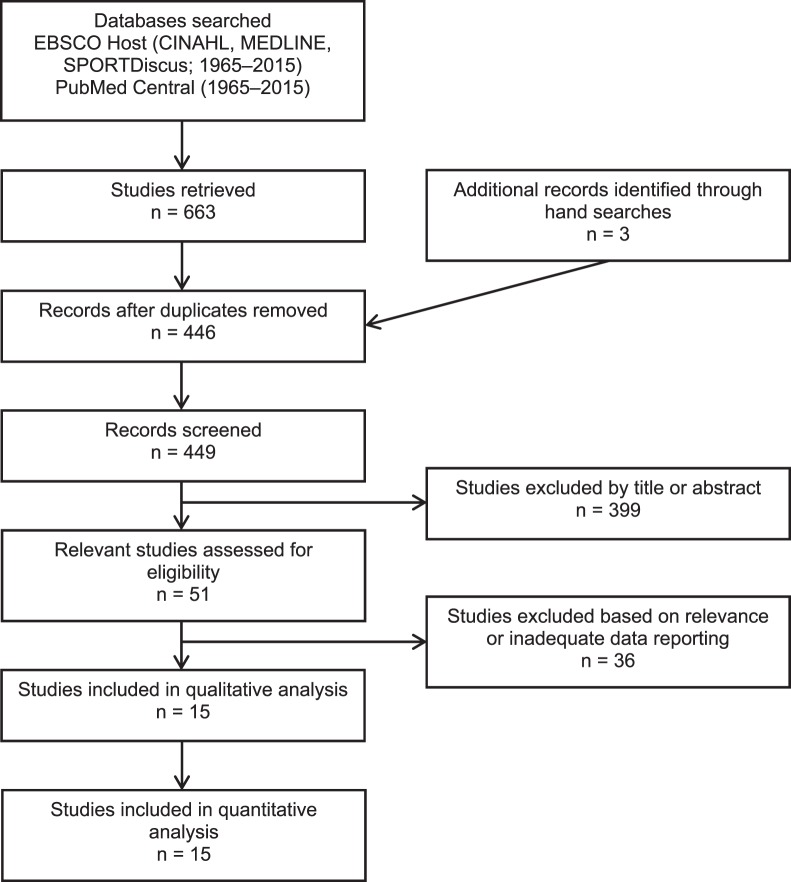
Using the initial search strategy, we identified 446 potential articles (Figure 1). A hand search of references identified an additional 3 potential articles. Of the 449 articles screened, 399 were excluded based on the title or abstract, and 36 were excluded based on relevance or inadequate data reporting. Fifteen articles met our inclusion criteria and provided 24 participant groups for analysis.17−31 One participant group23 was included after we hand measured the mean and standard deviation from a figure. The 15 articles were classified into the following categories based on rehabilitation type: balance training,20,21,23,25,28,30 manual therapy,17,19,22,26,31 and combination.18,24,25,27,29,30 Strength training was not included as a rehabilitation type because the authors of only 1 study27 investigated the isolated effects of a strength-training protocol. Several participant groups were included in the analysis for each moderator variable: balance training (n = 8), manual therapy (n = 7), and combination (n = 7). A methodologic summary of the included studies is presented in Table 2.
Figure 1. .
Flow chart of literature review.
Table 2. .
Methodologic Summary of the Included Studies Continued on Next Page
| Author and Design |
Sample Size/Group |
Participant Characteristics |
Intervention |
Intervention Frequency |
Outcome Measures |
Results |
| Hale et al24 (2007), randomized controlled trial | 29 CAI, 19 healthy CAI control = 12/13, CAI rehabilitation = 13/16, healthy = 17/19 | Unilateral CAI, history of ankle sprain, chronic weakness or pain, and episodes of giving way in last 6 mo | Home-exercise program and supervised rehabilitation: gastrocnemius and soleus stretching, ankle strengthening, single-limb balance training Supervised rehabilitation: box hops, carioca, figure of 8 | 4 wk, 6 supervised sessions, home-exercise program 5 per week Wks 1 and 2 = 2 sessions/wk, wks 3 and 4 = 1 session/wk | FADI (%) FADI–Sport (%) | Rehabilitation had greater FADI and FADI–Sport change scores compared with control and healthy groups. |
| McKeon et al28 (2008), randomized controlled trial | 31 CAI Balance training = 16/16 and control = 15/15 | History of more than 1 ankle sprain, giving way, and ≥4 yes responses on Ankle Instability Instrument | Progressive dynamic balance training: hop to stabilization, hop to stabilization and reach, unanticipated hop to stabilization, single-limb stance with eyes open and closed (20 min/session) | 4 wk, 12 supervised sessions (20 min) | FADI (%) FADI–Sport (%) | Balance training had greater postintervention scores compared with preintervention and control postintervention scores. |
| Beazell et al17 (2012), randomized controlled trial | 43 CAI Proximal tibiofibular joint manipulations = 15/15, distal tibiofibular joint manipulations = 14/15, and control = 13/13 | History of ankle sprain, episodes of giving way, <85% on FAAM–Sport or ≥3 yes responses on modified Ankle Instability Instrument, and 5° dorsiflexion deficit compared bilaterally | Proximal tibiofibular joint manipulations: 1–2 thrusts per session Distal tibiofibular joint manipulations: 1–2 thrusts per session | 3 wk, 4 supervised sessions | FAAM–Sport (%) | No changes in FAAM–Sport scores over time or compared with control participants in the proximal and distal tibiofibular joint manipulation groups. |
| Hilgendorf et al25 (2012), randomized controlled trial | 16 CAI Balance training = 8/8, vestibular-ocular reflex training = 8/8 | History of ≥2 ankle sprains and ≥1 episode of giving way in last 6 mo | Progressive dynamic balance training with and without vestibular-ocular reflex training | 4 wk, 12 supervised sessions | FAAM–ADL (%) FAAM–Sport (%) | FAAM–ADL and FAAM–Sport improved from preintervention to postintervention for both groups. No differences between groups were found. |
| Hoch et al26 (2012), prospective cohort study | 12 CAI | History of ankle sprain, ≥2 episodes of giving way in past 3 mo, ≥4 yes responses on Ankle Instability Instrument, ≤90% on the FAAM–ADL, and ≤80% on the FAAM–Sport | Maitland grade II talocrural joint traction (2 sets of 2 min) and Maitland grade III anterior-to-posterior talocrural joint traction (4 sets of 2 min) | 2 wk, 6 mobilization sessions | FAAM–ADL (%) FAAM–Sport (%) | FAAM–ADL and FAAM–Sport improved at postintervention and 1-wk follow-up compared with preintervention. |
| Schaefer and Sandrey30 (2012), randomized controlled trial | 36 CAI Balance training and Graston instrument-assisted soft tissue mobilization = 13/15, balance training and sham = 12/15, and balance training and control = 11/15 | History of inversion ankle sprain, repeated injury, and perception of giving way | Dynamic flex-band stretching warm-up (10 min), progressive dynamic balance training, and Graston instrument-assisted soft tissue mobilization | 4 wk, 8 supervised sessions (45 min) | FAAM–ADL (%) FAAM–Sport (%) | FAAM–ADL and FAAM–Sport improved from preintevention to postintevention for all groups. |
| Gilbreath et al22 (2014), prospective cohort study | 11 CAI | History of ankle sprain, ≥1 episode of giving way in past 3 mo, ≤25 on the CAIT, and participation in physical activity 20 min/d 3 times/wk | Weight-bearing talocrural mobilizations with movement (2 sets of 4 repetitions with 30-s holds) | 2 wk, 3 mobilization sessions | FAAM–ADL (%) FAAM–Sport (%) | FAAM–Sport improved. FAAM–ADL did not change. |
| Collins et al18 (2014), nonrandomized controlled trial | 36 CAI Strain-counterstrain = 13/13 and sham = 14/14 | History of ankle sprain at least 3 mo before study and ≥3 episodes of giving way in past year | Strain-counterstrain of tender points of the pelvis and lower extremity (90-s holds) and home-exercise program of strengthening and proprioceptive training | 4 wk, 4 strain-counterstrain or sham sessions and 12 d of home-exercise program | FAAM–ADL (%) FAAM–Sport (%) | Strain-counterstrain and sham groups both had greater FAAM–ADL and FAAM–Sport scores postintervention than preintervention. |
| Hale et al23 (2014), nonrandomized controlled trial | 34 CAI Balance training = 13/17 and control = 14/17 | History of >1 ankle sprain and reported feeling of giving way | Progressive balance- training program: dynamic and static single-limb stance activities; program completed on stable ankle only | 4 wk, 8 supervised sessions (30 min) | FADI–ADL (%) FADI–Sport (%) | Balance training improved scores from preintervention to postintervention on the FADI–Sport. FADI–ADL did not change. |
| Kim et al27 (2014), randomized controlled trial | 30 CAI Strength = 10/10, strength/proprioceptive exercises = 10/10, and control = 10/10 | Episodes of giving way due to previous ankle sprain and ≤24 on the CAIT | TheraBanda ankle- strengthening (10 min) and proprioceptive exercises involving single-limb balance and marching in place (10 min) | 4 wk, 12 supervised sessions | CAIT (score) | CAIT scores improved with strength and strength/proprioceptive exercises versus control. Strength/proprioceptive exercises improved scores compared with strength alone. |
| Cruz-Díaz et al20 (2015), randomized controlled trial | 70 CAI Balance training = 35/35 and control = 35/35 | History of ankle sprain ≥6 mo before study with subjective feeling of instability and <27 on the CAIT | Individually tailored balance training: static single-limb or double-limb stance tasks; control group completed general lower extremity strengthening program | 6 wk, 18 supervised sessions | CAIT (score) | Both groups improved CAIT scores. Balance training resulted in greater change score than control group. |
| Cruz-Díaz et al19 (2015), randomized controlled trial | 90 CAI Mobilizations with movement = 29/30, sham = 28/31, and control = 21/29 | History of ankle sprain, ≥2 sprains on same side in last 2 y, feeling of giving way, >2 cm weight-bearing–lunge test asymmetry, and no ankle sprain on contralateral side | Weight-bearing mobilizations with movement according to the Mulligan “no-pain rule” (2 sets of 10 repetitions); sham consisted of a fixed ankle while knee was flexed and extended (2 sets of 10 repetitions) | 3 wk, 6 supervised sessions | CAIT (score) | Differences in the CAIT were found for mobilizations with movement compared with control and sham after treatment and at 6-mo follow-up. |
| De Ridder et al21 (2015), case-control study | 39 CAI and 31 healthy Balance training = 33/39 and healthy = 31/31 | History of ≥2 ankle sprains, 1 ankle sprain associated with 3 wk of activity restriction, sensation of giving way, decreased functional participation, and physically active | Progressive balance- training program: single-limb and some double-limb tasks; tasks progressed by changing upper extremity position, visual status, and surface | 8 wk, 24 home balance sessions | FADI (%) FADI–Sport (%) | Individuals with CAIT had higher FADI and FADI–Sport scores after than before balance training. |
| Salom-Moreno et al29 (2015), randomized controlled trial | 27 CAI Balance training and strength = 13/13 and balance training, strength, and dry needling = 14/14 | History of ankle sprain, ≥1 episode of giving way in past 6 mo, pain >3 points on 11-point scale, and <26 on CAIT | Progressive TheraBanda ankle-strengthening and balance-training tasks; trigger-point dry needling to lateral peroneus muscle | 8 wk, 16 supervised sessions, with dry needling completed over first 4 wk (8 sessions) | FAAM–ADL (%) FAAM–Sport (%) | Both groups increased FAAM scores from baseline, with balance training, strength, and dry needling increasing scores more. |
| McKeon and Wikstrom31 (2016), randomized controlled trial | 80 CAI Mobilization = 19/20, massage = 19/20, stretching = 18/20, and control = 19/20 | History of ≥2 episodes of giving way in past 6 mo, ≥5 on the Ankle Instability Instrument, ≤90% FAAM, and ≤80% FAAM–Sport | Maitland grade III anterior-to-posterior talocrural joint mobilizations (2 sets of 2 min), petrissage and effleurage plantar massage (2 sets of 2 min), and heel cord stretching with knee slightly bent (3 sets of 30 s) | 2 wk, 6 supervised sessions | FAAM–ADL (%) FAAM–Sport (%) | FAAM–ADL improvements after massage and stretching. FAAM–Sport improvements after massage and mobilizations. |
Abbreviations: CAI, chronic ankle instability; CAIT, Cumberland Ankle Instability Tool; FAAM, Foot and Ankle Ability Measure; FADI, Foot and Ankle Disability Index; FADI–ADL, FADI activities of daily living subscale; FADI–Sport, FADI Sport subscale.
The Hygenic Corporation, Akron, OH.
Authors of the included articles had evaluated HRQL using only region-specific PROs that assessed the physical domain of HRQL. Specifically, 14 combined FAAM–ADL and FAAM–Sport, 3 FAAM–Sport, 3 combined FADI–ADL and FAAM–Sport, and 4 Cumberland Ankle Instability Tool (CAIT) participant groups were included in the analysis.
Methodologic Quality
The 2 reviewers initially agreed on 141 of 150 (94%) PEDro items. All but 1 disagreement was resolved through discussion between the reviewers. Overall, quality scores of the included studies ranged from 10% to 80%, with a median of 50%. A total of 7 studies17−20,25,29,31 were high quality, and 8 studies21−24,26−28,30 were low quality. Six studies were classified as level 1 evidence,17,19,20,25,29,31 and 9 as level 2 evidence.18,21–24,26–28,30 The individual items, quality scores, and levels of evidence can be found in Table 3.
Table 3. .
The Physiotherapy Evidence Database (PEDro) Individual Items and Quality Index Scores for the Included Articles
| Item |
Hale et al24 (2007) |
McKeon et al28 (2008) |
Beazell et al17 (2012) |
Hilgendorf et al25 (2012) |
Hoch et al26 (2012) |
Schaefer and Sandrey30 (2012) |
Gilbreath et al22 (2014) |
Collins et al18 (2014) |
Hale et al23 (2014) |
Kim et al27 (2014) |
Cruz-Díaz et al19 (2015) |
Cruz-Díaz et al20 (2015) |
De Ridder et al21 (2015) |
Salom-Moreno et al29 (2015) |
McKeon and Wikstrom31 (2016) |
| 1. Random allocation | Yes | Yes | Yes | Yes | No | Yes | No | No | No | Yes | Yes | Yes | No | Yes | Yes |
| 2. Allocation concealed | No | Yes | No | Yes | No | Yes | No | No | No | No | Yes | Yes | No | Yes | Yes |
| 3. Similar at baseline | Yes | Yes | Yes | No | No | No | No | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes |
| 4. Blinding of all subjects | No | No | No | No | No | No | No | Yes | No | No | No | No | No | No | No |
| 5. Blinding of all therapists | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No |
| 6. Blinding of all assessors | No | No | Yes | No | No | No | No | Yes | No | No | Yes | Yes | No | No | No |
| 7. More than 85% of follow-up | Yes | No | Yes | Yes | Yes | No | Yes | Yes | No | No | Yes | Yes | No | Yes | Yes |
| 8. Intention to treat | No | No | No | Yes | Yes | No | Yes | Yes | No | No | Yes | Yes | No | Yes | Yes |
| 9. Between-groups statistical comparison | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes |
| 10. Point measures and variability | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 11. Eligibility criteria indicated | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Yes, No. (%)a | 5 (50) | 5 (50) | 6 (60) | 6 (60) | 4 (40) | 4 (40) | 4 (40) | 7 (70) | 3 (30) | 4 (40) | 8 (80) | 8 (80) | 1 (10) | 7 (70) | 7 (70) |
| Level of evidence | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 1 | 1 |
Scores are based on items 1 through 10.
Data Synthesis
Overall Summary Effect.
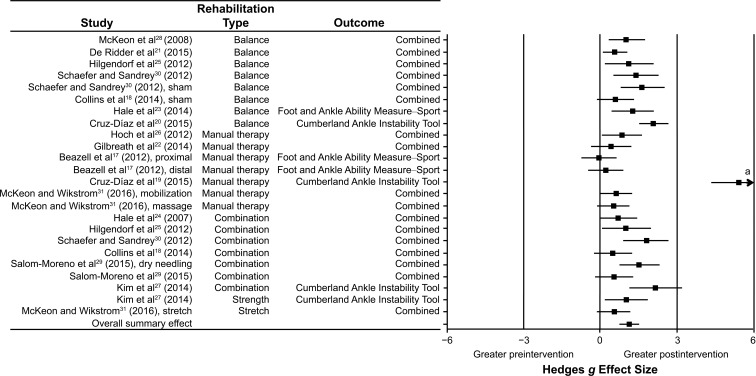
Across all the included studies and subgroups, the overall effect of the preintervention-to-postintervention comparisons was 1.11 (95% CI = 0.76, 1.46; P < .001), indicating that individuals with CAI demonstrated strong improvements in HRQL after rehabilitation. The individual ESs and the cumulative effects are shown in Figure 2 and Table 4, respectively.
Figure 2. .
Summary of Hedges g effect sizes and 95% confidence intervals for the included participant groups. a Confidence interval exceeded 6.
Table 4. .
Effect Size and 95% Confidence Intervals of Participant Groups
| Study and Summary Results |
Rehabilitation Type |
Outcome |
Hedges g |
95% Confidence Interval |
P Value |
| McKeon et al28 (2008) | Balance | Combined | 1.06 | 0.35, 1.77 | .004 |
| De Ridder et al21 (2015) | Balance | Combined | 0.59 | 0.11, 1.07 | .02 |
| Hilgendorf et al25 (2012) | Balance | Combined | 1.13 | 0.16, 2.09 | .02 |
| Schaefer and Sandrey30 (2012) | Balance | Combined | 1.44 | 0.56, 2.31 | .001 |
| Schaefer and Sandrey30 (2012), sham | Balance | Combined | 1.66 | 0.78, 2.54 | <.001 |
| Collins et al18 (2014), sham | Balance | Combined | 0.61 | −0.12, 1.33 | .10 |
| Hale et al23 (2014) | Balance | FAAM–Sport | 1.28 | 0.45, 2.11 | .003 |
| Cruz-Díaz et al20 (2015) | Balance | CAIT | 2.10 | 1.53, 2.67 | <.001 |
| Summary balance | 1.22 | 0.79, 1.65 | <.001 | ||
| Hoch et al26 (2012) | Manual therapy | Combined | 0.86 | 0.07, 1.65 | .03 |
| Gilbreath et al22 (2014) | Manual therapy | Combined | 0.45 | −0.35, 1.25 | .27 |
| Beazell et al17 (2012), proximal | Manual therapy | FAAM–Sport | −0.03 | −0.71, 0.65 | .93 |
| Beazel et al17 (2012), distal | Manual therapy | FAAM–Sport | 0.23 | −0.47, 0.93 | .52 |
| Cruz-Díaz et al19 (2015) | Manual therapy | CAIT | 5.41 | 4.32, 6.50 | <.001 |
| McKeon and Wikstrom31 (2016), mobilization | Manual therapy | Combined | 0.64 | 0.01, 1.27 | .048 |
| McKeon and Wikstrom31 (2016), massage | Manual therapy | Combined | 0.54 | −0.09, 1.16 | .10 |
| Summary manual therapy | 1.10 | 0.09, 2.11 | .03 | ||
| Hale et al24 (2007) | Combination | Combined | 0.73 | 0.01, 1.45 | .047 |
| Hilgendorf et al25 (2012) | Combination | Combined | 1.01 | 0.06, 1.96 | .04 |
| Schaefer and Sandrey30 (2012) | Combination | Combined | 1.81 | 0.94, 2.68 | <.001 |
| Collins et al18 (2014) | Combination | Combined | 0.51 | −0.23, 1.25 | .18 |
| Salom-Moreno et al29 (2015), dry-needling | Combination | Combined | 1.54 | 0.74, 2.34 | <.001 |
| Salom-Moreno et al29 (2015) | Combination | Combined | 0.56 | −0.19, 1.31 | .14 |
| Kim et al27 (2014) | Combination | CAIT | 2.17 | 1.14, 3.20 | <.001 |
| Summary combination | 1.14 | 0.67, 1.60 | <.001 | ||
| Kim et al27 (2014) | Strength | CAIT | 1.03 | 0.16, 1.90 | .02 |
| McKeon and Wikstrom31 (2016), stretch group | Stretch | Combined | 0.56 | −0.09, 1.20 | .09 |
| Overall summary | 1.11 | 0.76, 1.46 | <.001 |
Abbreviations: CAIT, Cumberland Ankle Instability Tool; FAAM, Foot and Ankle Ability Measure.
Summary Effects for Rehabilitation Type.
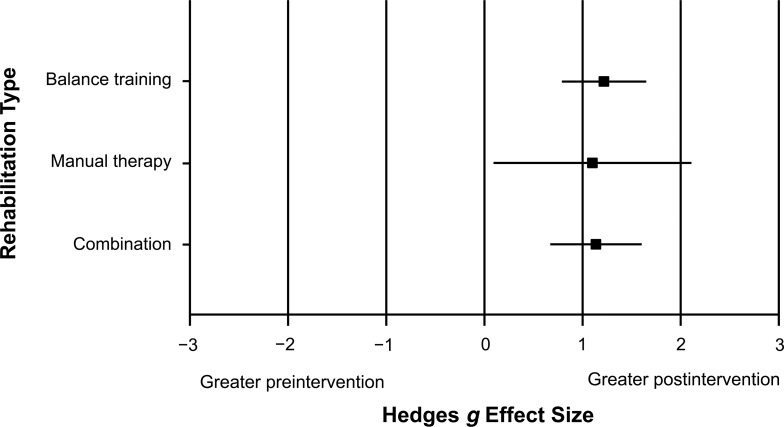
We observed no differences among the 3 levels of rehabilitation type (Q = 0.086, P = .96; Figure 3). Studies labeled as balance training demonstrated a strong effect with a CI that did not encompass zero (ES = 1.22; 95% CI = 0.79, 1.65; P < .001). Studies labeled as manual therapy demonstrated a strong effect (ES = 1.10; 95% CI = 0.09, 2.11; P = .03). Lastly, studies labeled as combined demonstrated a strong effect with a CI that did not encompass zero (ES = 1.14; 95% CI = 0.67, 1.60; P < .001).
Figure 3. .
Summary of Hedges g effect sizes and 95% confidence intervals for rehabilitation type.
Publication Bias
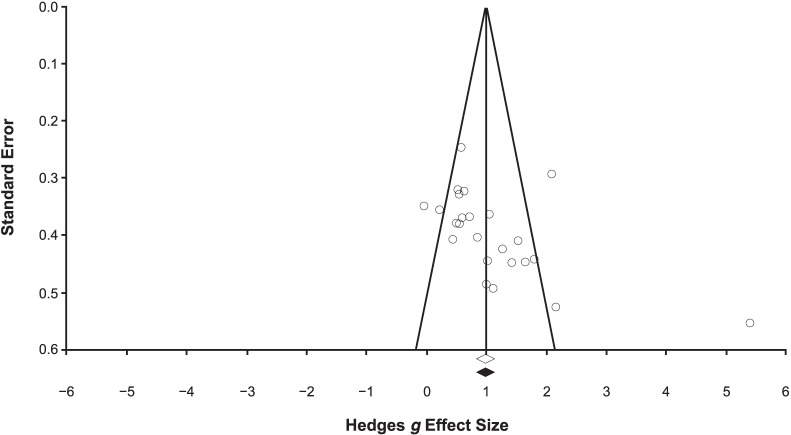
The likelihood of publication bias was assessed using a funnel plot (Figure 4). Based on the relative symmetry and even distribution of the studies within the funnel plot, it is unlikely that publication bias played a role in the results of the meta-analyses. This was further indicated via the trim-and-fill method, as no studies were inputted or removed. The results of the Orwin fail-safe N test indicated that a range of 214 to 451 additional studies, based on a trivial effect range of the Hedges g from 0.10 to 0.05, would be needed to nullify the overall summary effect. Based on the aforementioned results, publication bias was highly unlikely.
Figure 4. .
Funnel-plot analysis for publication bias.
Sensitivity Analysis
Overall Sensitivity Analysis.
The results of the 1-study-removed method indicated that the overall ES remained strong (range = 0.94–1.16; 95% CI = 0.70, 1.52). All P values were less than .001, which indicated no single participant group substantially influenced the overall summary effect.
Rehabilitation Type Sensitivity Analysis.
The 1-study-removed analysis for balance training (range = 1.01–1.35; 95% CI = 0.69, 1.77) and combination (range = 1.00–1.25; 95% CI = 0.55, 1.76) groups demonstrated that the ES remained strong. All P values were less than .001, which indicated no single ES substantially influenced the overall summary effect for these groups. However, the 1-study-removed analysis for manual-therapy rehabilitation type indicated that the ES ranged from 0.44 to 1.30 (95% CI = −0.03, 2.46) and P values ranged from .002 to .056, with 3 of the 7 P values indicating no difference (P > .053). This indicates that a single participant group substantially influenced the ES for this rehabilitation type. When we removed the Cruz-Díaz et al19 study, the pooled ES decreased from 1.10 to 0.44, and the 95% CI (0.16, 0.72) was narrow, signifying that this study influenced the pooled ES and subsequent recommendation.
Level of Evidence
Overall, grade A evidence supported region-specific, physical domain HRQL improvements in individuals with CAI after conservative rehabilitation. This recommendation was based on consistent findings from 6 level 117,19,20,25,29,31 and 9 level 218,21−24,26−28,30 studies. For balance training, grade B evidence indicated that this rehabilitation type improved HRQL based on consistent findings from 2 level 120,25 and 5 level 218,21,23,28,30 studies. For manual therapy, grade B evidence supported its effectiveness in improving HRQL based on inconsistent findings from 3 level 117,19,31 and 2 level 222,26 studies. For combination interventions, grade B evidence supported its use to improve HRQL based on consistent findings from 2 level 125,29 and 4 level 218,24,27,30 studies.
DISCUSSION
The purpose of our systematic review with meta-analysis was to determine the effects of different rehabilitation interventions on HRQL in individuals with CAI. Our findings indicated that published rehabilitation strategies effectively improved the physical domain of HRQL in individuals with CAI (overall ES = 1.11). Grade A evidence supported this result, as indicated by consistent findings from level 1 to level 2 evidence. Furthermore, the evidence suggested that balance training, manual therapy, and a combination of interventions can be used to improve patient-oriented outcomes. Therefore, any of these rehabilitation strategies could be used in clinical practice to improve HRQL in individuals with CAI.
Balance Training
We found grade B evidence that a balance-training rehabilitation protocol effectively improved HRQL, as measured by patient-oriented outcomes, in individuals with CAI. Moderate to strong ESs (pooled = 1.22; range = 0.59−2.10) indicated improvement when comparing preintervention and postintervention outcomes. Three25,28,30 of the 718,20,21,23,25,28,30 studies were based on a program developed by McKeon et al.28 These interventions were 4 weeks long and involved progressive single-limb balance and hopping tasks. The remaining balance interventions18,20,21,23 used progressive exercises for 4 to 8 weeks. The largest ES (2.10) was demonstrated by Cruz-Díaz et al,20 who also used one of the longest intervention durations (6 weeks). The lowest ESs (0.59 and 0.61) were reported in the only studies18,21 with home-based balance-training programs. These results may imply that supervised balance-training interventions more effectively improve HRQL, as measured by PROs, than unsupervised home-based programs.
Manual Therapy
Grade B evidence indicated that a manual-therapy–focused intervention program improved patient-oriented outcomes in individuals with CAI.17,19,22,26,31 This finding should be interpreted with caution, however, as a single participant group substantially influenced the summary ES for this intervention type. When the Cruz-Díaz et al19 study was removed (ES = 5.41), the summary ES was moderate (ES = 0.44). Therefore, it is more likely that PROs moderately improve after isolated manual-therapy interventions.
The manual-therapy techniques investigated included talocrural anterior-to-posterior Maitland grade III joint mobilizations,26,31 Mulligan talocrural mobilizations with movement,19,22 tibiofibular manipulations,17 and plantar massage.31 Tibiofibular manipulation demonstrated the weakest ESs (range = −0.03 to 0.23)17 compared with the 4 studies19,22,26,31 in which researchers investigated talocrural mobilizations (range = 0.45 to 5.41). Therefore, from the patient's perspective, manual-therapy techniques for improving talar mobility and positioning may be more effective than other manual-therapy techniques. The talocrural mobilization protocols included 322 (ES = 0.45) to 619,26,31 (ES = 0.64–5.41) mobilization sessions completed during periods ranging from 2 weeks22,26,31 (ES = 0.45–0.86) to 3 weeks19 (ES = 5.41). Mobilizations-with-movement protocols varied, with participants completing 2 sets of 10 repetitions in 1 study19 and 2 sets of 4 repetitions with 30-second holds at the end range of dorsiflexion in another.22 Anterior-to-posterior Maitland grade III joint-mobilization techniques were implemented using 231 and 426 sets of 2-minute applications. In addition, plantar cutaneous massage had a moderate effect on PROs (ES = 0.54).31 This finding, however, was accompanied by a 95% CI that crossed zero. Together, these results indicated a continued need to determine the patient characteristics, manual-therapy techniques, and treatment volume and dosage that optimize HRQL improvements in individuals with CAI.
Combined Interventions
We found grade B evidence that rehabilitation programs involving 2 or more targeted interventions improved PRO measures in individuals with CAI. The summary effect (ES = 1.14) indicated that combined interventions had a strong effect on PROs from preintervention to postintervention. The combined interventions consisted of stretching,24,30 strength training,18,24,27,29 balance training,18,24,25,27,29,30 vestibular-ocular reflex training,25 soft tissue mobilization,30 dry needling,29 and strain-counterstrain.18 All combined rehabilitation protocols included a balance-training component; 2 protocols25,30 required participants to complete a balance-training program based on McKeon et al.28 In 5 studies, researchers investigated the combined effect of 2 interventions18,25,27,29,30; in 2 studies, the combined effect of 3 interventions.24,29 Combined interventions demonstrated a slightly lower summary effect than isolated balance training, which may indicate that adding other interventions to balance training may not result in greater HRQL gains for individuals with CAI.
Practical Implications
This systematic review with meta-analysis demonstrated that the available rehabilitation strategies improve ankle-specific PROs for individuals with CAI. We observed a strong overall effect for improving scores on region-specific PROs, specifically the FAAM–ADL, FAAM–Sport, FADI, FADI–Sport, and CAIT. Whereas improvements were noted using each of the aforementioned PROs, the CAIT seemed to be sensitive to rehabilitation, as it displayed the largest ESs (1.03−5.41). Of the included PROs, the CAIT was the only instrument that was not designed to capture changes in self-reported disability because it is primarily used as a diagnostic tool to identify CAI.32 The high responsiveness of the CAIT may have resulted from the relevance of its items to the activity limitations of individuals with CAI, whereas the FAAM and FADI were designed for broader patient populations. In future research, investigators should evaluate this instrument as an outcome measure.
Despite variations in rehabilitation strategies, dosages, and rehabilitation lengths, region-specific improvements were consistently demonstrated. Of the available rehabilitation strategies, supervised balance-training programs demonstrated the greatest PRO improvements in individuals with CAI. This was true when balance training was used in isolation or in combination with other treatment modalities. In addition, balance training used in combination with other rehabilitation strategies demonstrated summary effects similar to those of isolated balance training. This indicates that supplementing balance training with other interventions may not further improve HRQL when compared with isolated balance training.
Limitations
Whereas we followed the PRISMA guidelines,12 our study had limitations. Our electronic search was conducted to find articles written in English in databases thought to be most relevant to journals that frequently publish articles related to CAI. However, we may not have identified and included all articles relevant to this review. In addition, evidence was limited regarding the isolated effects of strength-training interventions despite their common use in clinical practice. Therefore, we could not make recommendations about the effect of strength training on HRQL. Lastly, individuals with CAI have shown decreased HRQL as measured using region-specific, dimension-specific, and global outcome measures.11 Thus, a multidimensional profile of HRQL should be used to evaluate the effectiveness of CAI rehabilitation strategies. The evidence presented in this review included only studies in which the researchers used region-specific PROs due to a lack of evidence assessing other domains of HRQL. In future work, investigators should use a multidimensional HRQL profile to examine the effectiveness of common CAI rehabilitation strategies from the whole-person perspective.
Authors of the included studies all used similar inclusion (a history of ankle sprains and subsequent episodes of giving way) and exclusion criteria, but none implemented intervention protocols with designs based on clinician-oriented, measured impairments. For all included studies, the interventions were delivered using blanket procedures regardless of the presence of measureable deficits. This cookie-cutter approach to CAI rehabilitation is contradictory to developing CAI treatment protocols.33 In their rehabilitation paradigm, Donovan et al33 suggested that CAI rehabilitation should be conducted using an assess, treat, and reassess model. They theorized that, by treating individual-specific deficits, greater health improvements may be attained.33 By focusing on deficits specific to the individual, clinicians may create an environment most conducive to achieving HRQL improvements from the patient's perspective. To promote patient-centered care and to mimic a realistic model of clinical care, researchers studying CAI interventions should consider adopting impairment-based treatment protocols. Furthermore, to mimic true clinical care, investigators need to move from laboratory-based intervention studies to point-of-care research.
CONCLUSIONS
This synthesis of the available evidence suggested that several rehabilitation strategies effectively improve ankle-specific HRQL in individuals with CAI. Balance training demonstrated a high level of evidence and the largest summary effect, indicating that it may be the most appropriate rehabilitation strategy to improve HRQL in individuals with CAI. Furthermore, manual therapy may have a degree of clinical efficacy as an intervention to improve HRQL. More research is needed to examine the isolated effects of other common rehabilitation strategies (ie, strength training) to understand how these strategies contribute to the overall treatment effect. In addition, investigators should explore the effectiveness of impairment-based treatment models for improving HRQL in individuals with CAI.
REFERENCES
- 1. Hertel J. . Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002; 37 4: 364– 375. [PMC free article] [PubMed] [Google Scholar]
- 2. Waterman BR, Belmont PJ, Cameron KL, Deberardino TM, Owens BD. . Epidemiology of ankle sprain at the United States Military Academy. Am J Sports Med. 2010; 38 4: 797– 803. [DOI] [PubMed] [Google Scholar]
- 3. Swenson DM, Collins CL, Fields SK, Comstock RD. . Epidemiology of U.S. high school sports-related ligamentous ankle injuries, 2005/06−2010/11. Clin J Sport Med. 2013; 23 3: 190– 196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Anandacoomarasamy A, Barnsley L. . Long term outcomes of inversion ankle injuries. Br J Sports Med. 2005; 39 3: E14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Konradsen L, Bech L, Ehrenbjerg M, Nickelsen T. . Seven years follow-up after ankle inversion trauma. Scand J Med Sci Sports. 2002; 12 3: 129– 135. [DOI] [PubMed] [Google Scholar]
- 6. Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. . The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014; 44 1: 123– 140. [DOI] [PubMed] [Google Scholar]
- 7. Hubbard-Turner T, Turner MJ. . Physical activity levels in college students with chronic ankle instability. J Athl Train. 2015; 50 7: 742– 747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Valderrabano V, Hintermann B, Horisberger M, Fung TS. . Ligamentous posttraumatic ankle osteoarthritis. Am J Sports Med. 2006; 34 4: 612– 620. [DOI] [PubMed] [Google Scholar]
- 9. Snyder AR, Parsons JT, Valovich McLeod TC, Curtis Bay R, Michener LA, Sauers EL. . Using disablement models and clinical outcomes assessment to enable evidence-based athletic training practice, part I: disablement models. J Athl Train. 2008; 43 4: 428– 436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Parsons JT, Snyder AR. . Health-related quality of life as a primary clinical outcome in sport rehabilitation. J Sport Rehabil. 2011; 20 1: 17– 36. [DOI] [PubMed] [Google Scholar]
- 11. Houston MN, Hoch JM, Hoch MC. . Patient-reported outcome measures in individuals with chronic ankle instability: a systematic review. J Athl Train. 2015; 50 10: 1019– 1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Moher D, Liberati A, Tetzlaff J, Altman DG. . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009; 62 10: 1006– 1012. [DOI] [PubMed] [Google Scholar]
- 13. Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. . Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003; 83 8: 713– 721. [PubMed] [Google Scholar]
- 14. Munn J, Sullivan SJ, Schneiders AG. . Evidence of sensorimotor deficits in functional ankle instability: a systematic review with meta-analysis. J Sci Med Sport. 2010; 13 1: 2– 12. [DOI] [PubMed] [Google Scholar]
- 15. Cohen J. . Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 16. Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. J Am Board Fam Pract. 2004; 17 1: 59– 67. [DOI] [PubMed] [Google Scholar]
- 17. Beazell JR, Grindstaff TL, Sauer LD, Magrum EM, Ingersoll CD, Hertel J. . Effects of a proximal or distal tibiofibular joint manipulation on ankle range of motion and functional outcomes in individuals with chronic ankle instability. J Orthop Sports Phys Ther. 2012; 42 2: 125– 134. [DOI] [PubMed] [Google Scholar]
- 18. Collins CK, Masaracchio M, Cleland JA. . The effectiveness of strain counterstrain in the treatment of patients with chronic ankle instability: a randomized clinical trial. J Man Manip Ther. 2014; 22 3: 119– 128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cruz-Díaz D, Lomas Vega R, Osuna-Pérez MC, Hita-Contreras F, Martínez-Amat A. . Effects of joint mobilization on chronic ankle instability: a randomized controlled trial. Disabil Rehabil. 2015; 37 7: 601– 610. [DOI] [PubMed] [Google Scholar]
- 20. Cruz-Díaz D, Lomas-Vega R, Osuna-Pérez MC, Contreras FH, Martínez-Amat A. . Effects of 6 weeks of balance training on chronic ankle instability in athletes: a randomized controlled trial. Int J Sports Med. 2015; 36 9: 754– 760. [DOI] [PubMed] [Google Scholar]
- 21. De Ridder R, Willems TM, Vanrenterghem J, Roosen P. . Effect of a home-based balance training protocol on dynamic postural control in subjects with chronic ankle instability. Int J Sports Med. 2015; 36 7: 596– 602. [DOI] [PubMed] [Google Scholar]
- 22. Gilbreath JP, Gaven SL, Van Lunen B, Hoch MC. . The effects of mobilization with movement on dorsiflexion range of motion, dynamic balance, and self-reported function in individuals with chronic ankle instability. Man Ther. 2014; 19 2: 152– 157. [DOI] [PubMed] [Google Scholar]
- 23. Hale SA, Fergus A, Axmacher R, Kiser K. . Bilateral improvements in lower extremity function after unilateral balance training in individuals with chronic ankle instability. J Athl Train. 2014; 49 2: 181– 191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hale SA, Hertel J, Olmsted-Kramer LC. . The effect of a 4-week comprehensive rehabilitation program on postural control and lower extremity function in individuals with chronic ankle instability. J Orthop Sports Phys Ther. 2007; 37 6: 303– 311. [DOI] [PubMed] [Google Scholar]
- 25. Hilgendorf JR, Vela LI, Gobert DV, Harter RA. . Influence of vestibular-ocular reflex training on postural stability, dynamic visual acuity, and gaze stabilization in patients with chronic ankle instability. Athl Train Sports Health Care. 2012; 4 5: 220– 229. [Google Scholar]
- 26. Hoch MC, Andreatta RD, Mullineaux DR, et al. Two-week joint mobilization intervention improves self-reported function, range of motion, and dynamic balance in those with chronic ankle instability. J Orthop Res. 2012; 30 11: 1798– 1804. [DOI] [PubMed] [Google Scholar]
- 27. Kim KJ, Kim YE, Jun HJ, et al. Which treatment is more effective for functional ankle instability: strengthening or combined muscle strengthening and proprioceptive exercises? J Phys Ther Sci. 2014; 26 3: 385– 388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. McKeon PO, Ingersoll CD, Kerrigan DC, Saliba E, Bennett BC, Hertel J. . Balance training improves function and postural control in those with chronic ankle instability. Med Sci Sports Exerc. 2008; 40 10: 1810– 1819. [DOI] [PubMed] [Google Scholar]
- 29. Salom-Moreno J, Ayuso-Casado B, Tamaral-Costa B, Sánchez-Milá Z, Fernández-de-Las-Penas C, Alburquerque-Sendin F. . Trigger point dry needling and proprioceptive exercises for the management of chronic ankle instability: a randomized clinical trial. Evid Based Complement Alternat Med. 2015; 2015: 790209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Schaefer JL, Sandrey MA. . Effects of a 4-week dynamic-balance-training program supplemented with Graston instrument-assisted soft-tissue mobilization for chronic ankle instability. J Sport Rehabil. 2012; 21 4: 313– 326. [DOI] [PubMed] [Google Scholar]
- 31. McKeon PO, Wikstrom EA. . Sensory-targeted ankle rehabilitation strategies for chronic ankle instability. Med Sci Sports Exerc. 2016; 48 5: 776– 784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gribble PA, Delahunt E, Bleakley CM, et al. Selection criteria for patients with chronic ankle instability in controlled research: a position statement of the International Ankle Consortium. J Athl Train. 2014; 49 1: 121– 127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Donovan L, Hart JM, Saliba SA, et al. Rehabilitation for chronic ankle instability with or without destabilization devices: a randomized controlled trial. J Athl Train. 2016; 51 3: 233– 251. [DOI] [PMC free article] [PubMed] [Google Scholar]