Abstract
Objective: To determine whether there is any difference between virtual reality game–based balance training and real-world task-specific balance training in improving sitting balance and functional performance in individuals with paraplegia. Methods: The study was a pre test–post test experimental design. There were 30 participants (28 males, 2 females) with traumatic spinal cord injury randomly assigned to 2 groups (group A and B). The levels of spinal injury of the participants were between T6 and T12. The virtual reality game–based balance training and real-world task-specific balance training were used as interventions in groups A and B, respectively. The total duration of the intervention was 4 weeks, with a frequency of 5 times a week; each training session lasted 45 minutes. The outcome measures were modified Functional Reach Test (mFRT), t-shirt test, and the self-care component of the Spinal Cord Independence Measure–III (SCIM-III). Results: There was a significant difference for time (p = .001) and Time × Group effect (p = .001) in mFRT scores, group effect (p = .05) in t-shirt test scores, and time effect (p = .001) in the self-care component of SCIM-III. Conclusions: Virtual reality game–based training is better in improving balance and functional performance in individuals with paraplegia than real-world task-specific balance training.
Keywords: balance, paraplegia, rehabilitation, self-care, virtual reality
Introduction
Spinal cord injury (SCI) can cause temporary or permanent changes in the spinal cord's normal sensory-motor or autonomic functions. These changes may adversely affect an individual's functional status and quality of life.1,2 Most of the functional activities, such as eating, dressing, and transfers, are performed in a sitting position by people who have paraplegia.3 Any limitation in the ability to safely shift the body's center of gravity toward stability may restrict wheelchair mobility and activities of daily living (ADLs). Hence, sitting balance is very important for functional independence for people who cannot stand.4
The coordinated action of trunk, upper limbs, and lower limbs plays a critical role in seated reaching tasks.5,6 Individuals with complete paraplegia adopt different postural adjustments to face balance challenges because their lower limbs are not active. They compensate for postural muscle function loss by using parts of the sensory-motor system that are still intact, such as the latissimus dorsi and trapezius muscles, to maintain sitting balance.7,8
Virtual reality (VR) is an advanced form of human-computer interface that allows users to interact in a computer-generated environment.9 Users perform actions in a simulated environment. They interact with displayed images and move and manipulate virtual objects.10 VR programs attempt to stimulate real-world activities, which may provide enhanced ecological validity.11 Tasks that are unsafe to practice in the real world can be practiced in a safe and controlled environment through VR. Game-based exercises have been shown to improve balance control in people with SCI.12,13
Effective and early functional rehabilitation of balance problems promotes independent living in the community.13 Task-related motor training has been shown to improve balance performance.14 Kizony et al studied the feasibility of the GX-VR system in rehabilitation of people after SCI. The results of the study showed correlations between static balance ability and performance within VR.15 Investigations on the application of VR game–based balance training in the rehabilitation of SCI is limited. This study was designed to identify whether there is any difference between VR game–based balance training and real-world task-specific balance training in improving sitting balance and functional performance in individuals with paraplegia.
Materials and Methods
Participants
A sample of 30 individuals with traumatic SCI took part in the study. Thirty-six individuals were found eligible for the study during screening; 6 of them declined to participate in the study. The participants were recruited using convenience sampling techniques from the rehabilitation department of a tertiary spinal injury care center located in New Delhi. The eligibility for study participation was determined through physical examination screening and from medical records. Participants had neurological levels of injury between T6 and T12, A or B in American Spinal Injury Association Impairment Scale (ASIA),16 and a duration of injury less than 6 months. All the participants had the ability to sit unsupported for at least 10 seconds and had a minimum of active 90° of shoulder flexion. They were included in the study after they signed a written informed consent. The exclusion criteria were any deformity of the upper extremity; any other neurological, musculoskeletal, or psychiatric impairment; severe deficits of comprehension; pressure sores; severe spasticity; uncorrected hearing or visual impairment; and any recent history of severe urinary tract infection or autonomic dysreflexia.
Procedure
The demographic data and neurological details of the participants were collected first. These included the age (years), ASIA grade, neurological level, weight (kg), gender, trunk length (cm), and arm length (cm). Participants were randomly allocated to either of 2 groups, by computer-generated random numbers, with 15 individuals in each group. Participants in group A underwent VR game–based training and participants in group B underwent real-world task-specific balance training. All the participants in both the groups received training for 45 minutes a day, 5 times a week for 4 weeks along with conventional physical therapy. The exercises included in the conventional physiotherapy were stretching of lower limb muscles, range of motion exercises, and mat exercises. The duration of each session was 20 minutes. The VR game–based training, real-world task-specific balance training, and conventional exercises were done by different therapists who were blinded to the study. The study was a pre test–post test experimental design. It was approved by the research and ethical committee of the center in which the study was undertaken. Protocol of the study is given in Figure 1.
Figure 1.
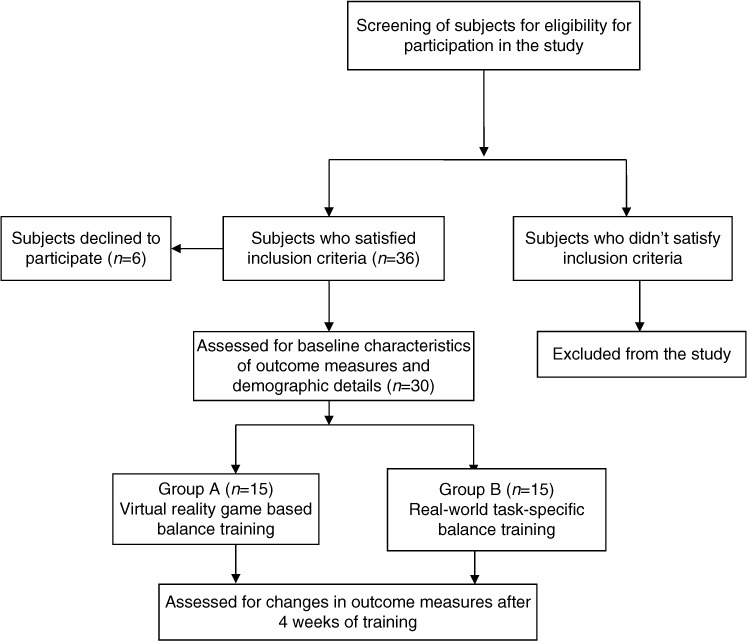
Protocol of the study design.
Instrumentation
Sony PlayStation 2 and EyeToy (Sony Computer Entertainment Inc., Beijing, China) were used with 3 virtual environments (birds and balls, soccer, and snowboard games).15,17 These environments had been adapted for rehabilitation purposes. All the virtual environments were used to challenge movements and positions of various body segments to train the sitting balance. Performance in all environments was measured in terms of rate of success.
Interventions
Training of group A
During the birds and balls game, balls of different colors emerged from the 4 edges of the screen in a single plane of action and flew toward the participant. Touching these balls with any part of the body turns them into birds or causes them to burst. In the soccer game, the participant acted as a goalkeeper. Balls flew from different locations and the participant had to stop the ball from crossing the goal line. Successfully repelled balls remained white while balls entering the goal area changed color. In the snowboard simulation, the participant saw a back view of themselves as on a snowboard. As the participant skied downhill, he or she had to avoid rocks and trees by leaning from side to side. In first 2 environments, 3 levels of difficulty were used; in the third situation, only one level was used. When a participant achieved an 80% success rate in a particular program, the difficulty level was raised.
Training of group B
The participants in group B repeatedly practiced a few specifically designed exercises, which involved moving the upper body over and outside the base of support. The activities were typing on a keyboard, tying and untying knots, picking up sticks, pegs on a line, catching and throwing balls and mini frisbee, picking objects up off the floor, passing objects around the body/carrying overhead, clapping games with a partner, taking clothing on/off, buttoning up the shirt, and mimicking the actions of swimming/fly fishing. The participants were instructed to move while doing the particular activity to increase the difficulty level. The exercises were done in an unsupported sitting position on a low-rise bed with hips and knees flexed to 90° and feet resting on the floor.
Outcome measures
Modified Functional Reach Test (mFRT), t-shirt test, and self-care components of the Spinal Cord Independence Measure–III (SCIM-III) were used as the outcome measures to assess and compare the effectiveness of the 2 training protocols. The participants were assessed on the outcome measures 1 day prior to the start of training. The posttraining assessment was done on the day following the last day of training. The assessment session lasted for around 45 minutes, and the assessment was performed by a therapist who was blinded to the participant's training protocol.
Developed by Lynch et al, mFRT is a highly useful test to assess sitting balance in non-standing persons with SCI.18 The intraclass correlation coefficient (ICC) value of mFRT was reported to be 0.85 to 0.94. For measuring the mFRT value, the participant sat in a standard wheelchair with his or her feet supported. Initial reach was measured against a yardstick mounted on the wall along the shoulder at the level of tip of acromion process as each participant rested against the back support of the wheelchair with the upper extremity flexed to 90°. The participant was then asked to reach forward as far as possible and come back without any support. The maximum forward reach was measured. The difference between the initial reach and maximum reach was the measure of functional reach in sitting. Each participant performed 3 trials. The mean of these 3 trials was used for further analysis.18 The anatomical landmark used for measuring reach was the ulnar styloid process.
The t-shirt test is a reliable and valid tool for assessing sitting balance in spinal cord–injured persons. The t-shirt test has a good ICC value (0.79–0.91). It measures the time taken by participants to put on and take off a t-shirt.19 For the test, one standard size pullover type t-shirt and one t-shirt that was one size larger than what the participant would normally wear were used. The t-shirts were placed on a table of standard height in front of the participant. No harness was worn during this test, but a research assistant was ready to support the participant if needed. The participant was required to put on and take off the t-shirt, resting between each maneuver. The time taken for the whole activity was recorded.19 The test was repeated twice for each size of the t-shirt provided, and the average was taken for final analysis.
The SCIM-III is a disability scale developed specifically for functional assessment in various areas such as self-care, respiration, sphincter management, and mobility in people with SCI. SCIM-III is sensitive to changes to function and is a reliable tool. Reliability studies of the scale have reported the ICC value above 0.94, Cronbach's alpha above 0.7, and the coefficient of Pearson correlation between FIM and SCIM-III as 0.79.20,21 Scores for components of self-care (bathing, feeding, dressing, and grooming; score range, 0–20) of SCIM-III were obtained by patient interview.22
Data analysis
Data analysis was done using IBM SPSS software version 17 (IBM, Armonk, NY). Independent t test was used to analyze the differences between group A and B on age, weight, arm length, trunk length, and preintervention scores of the outcome measures. Repeated measures analysis of variance (ANOVA) were used to analyze the changes in outcome measures in the 2 groups.The effect size (partial eta squared [η2]) was also calculated. The η2 in SPSS is calculated on the basis of the sum of the squared difference and the sum of the squared error for time, group, and Time × Group interaction effects. Pearson chi-square test was used to analyze the difference in neurological level between the groups. A significance level of p ≤ .05 was fixed.
Results
The mean ± SD of age, weight, arm length, trunk length, gender, and duration after injury for both groups is shown in Table 1. The neurological level frequency distribution is shown in Table 2. The mean ± SD of pre- and posttraining scores of mFRT, t-shirt test, and self-care components of the SCIM-III are given in Table 3. The findings showed no significant difference between the groups for the age, duration since injury, weight, arm length, trunk length (Table 1), neurological level of injury (p = .49) (Table 2), and pretraining scores of outcome measures (Table 3).
Table 1.
Comparison of demographic characteristics between the group of participants who received virtual reality–based balance training (group 1) and the group of participants who received real-world task-specific balance training
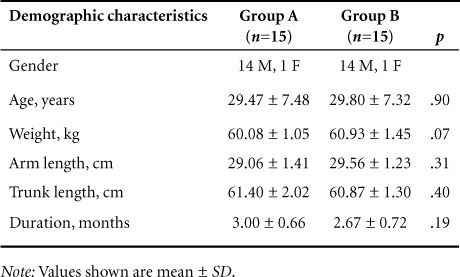
Table 2.
Comparison of neurological level of injury between the groups
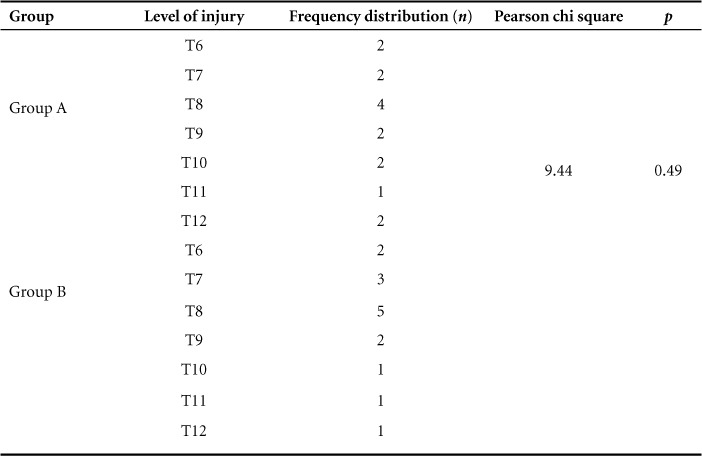
Table 3.
Pre-and posttraining measures of modified Functional Reach Test, t-shirt test, and self-care components of SCIM-III
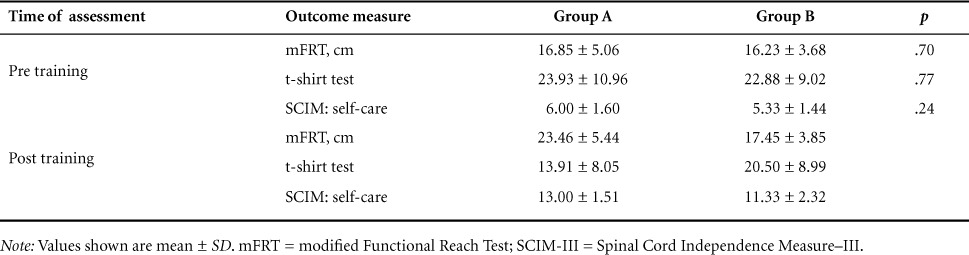
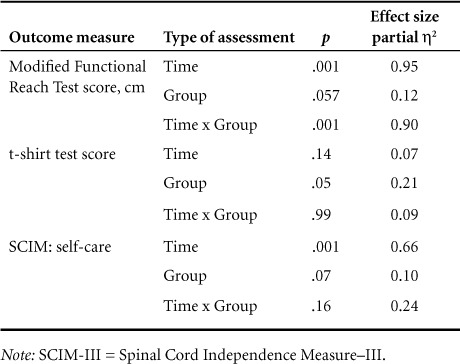
The mFRT scores showed a significant change for time (p = .001) and Time × Group (p = .001) but no significant change for group effect (p = .057). The t-shirt test scores showed a significant change for group effect (p = .05), but no significant change for time (p = .14) and Time × Group (p = .99). For the self-care components of SCIM-III, there was a significant change for time (p = .001), but no significant change for group (p = .07) and Time × Group (p = .16) (Table 4). Three participants in the group A missed 3 treatment sessions each, and 2 participants in group B missed 2 sessions each and 1 participant missed 1 treatment session. The intention-to-treat analysis was used where there was noncompliance. All the participants completed the study protocol in both groups.
Table 4.
Comparison outcome measures scores between groups with effect size using repeated measures analysis of variance
Discussion
This study was designed to compare the effectiveness of VR game–based training on balance and functional performance in people with paraplegia. The results revealed changes in outcome measures. In the mFRT, there were significant differences for time and Time × Group effect. In the t-shirt test, there was a significant difference for group; in the self-care components of SCIM-III, there was significant differences for time. The results suggests that mFRT scores were changing with time, and the changes were different for both groups. The t-shirt test scores were primarily affected by type of training. The self-care component scores of the SCIM-III changed with time. With respect to effect size, the largest change was observed in mFRT scores for time and then for Time × Group. When the effect size is more then 0.7, the change in the measured value is considered to be large.23 Wall et al have shown that the use of Nintendo Wii Fit produced greater improvements in gait speed and functional reach,24 whereas Harvey et al reported no improvement of balance in the early phase of rehabilitation using unsupported sitting.25
The differences observed imply that mFRT, which is used as a criterion measure for assessing balance, was affected by duration of training (time effect) and the type of training was influenced by duration of training (Time × Group). The t-shirt test scores were primarily affected by type of training (group effect) and the self-care component scores of the SCIM-III were changing with time (time effect). The changes noticed in group A participants in outcome measures may be due to the direct result of the games played using VR training, which required the participants to self-perturb themselves to a greater extent than participants of group B. The extent of the challenge that the participants experienced in controlling their center of gravity during dynamic activities might have lead to noticeable changes in balance measures. The self-care components were not affected much by type of training; this may be due to the fact that improvement in balance performance alone may not improve self-care.
The dynamic nature of the moving virtual stimuli in contrast to the relatively static nature of the stimuli presented during real-world task-specific training might also have contributed to a better outcome in group A. Presentation of virtual stimuli, especially at the higher levels of difficulty, facilitated therapy for diverse equilibrium reactions rather than being limited to the simple transfer of weight, which is usually the focus of conventional treatment. The ability to deliver several stimuli simultaneously from different directions and at different velocities with the EyeToy might have facilitated task manipulation to a larger extent.15
The most effective means for improving neuroplasticity and subsequent recovery of motor function following injury or disease to the nervous system is through intense skillful practice.26 In VR games, training can be progressed by gradually increasing the complexity of the tasks.9 Users who reach for objects within the VR environment become absorbed in the task and are less fearful of destabilizing and falling.27,28 In our study, participants showed great interest during VR training sessions, but we did not objectively measure the motivational level of the participants. In VR environment training, participants used to respond with enthusiasm to goal-directed movements.29 Chen et al showed significant correlation between dressing upper body and dressing lower body with sitting balance.3 The improved balance control mechanism might have resulted in improvement in self-care components of SCIM-III.
The participants in both training groups had low level of injury (T6 to T12). Individuals with high thoracic SCI use a more passive and simpler strategy to compensate for the lost sensorimotor functions, whereas individuals with low thoracic SCI use more active and complex strategy for maintaining sitting balance.8,30,31 There is also a significantly greater composite maximal weight shift during reaching activities in persons with low SCI.3 Thus it was thought that persons with low SCI would be better able to do the training programs used in the study. Although we included individuals with both ASIA A and B grades, none of them had muscle power greater than 1, according to Medical Research Council grading systems, in the muscles below the neurological level. Outcome measures for assessment of the functional performance were chosen, because these are the most essential tasks for self-care that require skill and balance.
In the present study, individuals with low paraplegia were recruited. Future studies can be performed with people with high paraplegia and incomplete SCI (ASIA C and D) to see how the training protocols affects their performance. Effects of VR-training regimens on electromyographic activity, biomechanical aspects, and ADLs may also be explored. Studies should include a larger sample size in order for their findings to be generalized. One limitation of our study was that PlayStation 2 and EyeToy were used for VR training instead of more sophisticated instruments. The participants included in the study were from a single source.
Conclusion
Participants who received VR game–based balance training showed better improvement on outcome measures as compared to participants who received real-world task-specific balance training. Hence it can be concluded that VR game–based training over a short duration can improve balance and functional performance in individuals with paraplegia better than real-world task-specific balance training.
REFERENCES
- 1. Somers MF. Spinal Cord Injury: Functional Rehabilitation. Englewood Cliffs, NJ: Appleton and Lange; 1992. [Google Scholar]
- 2. Westgren N, Levi R.. Quality of life and traumatic spinal cord injury. Arch Phys Med Rehabil. 1998; 79: 1433– 1439. [DOI] [PubMed] [Google Scholar]
- 3. Chen CL, Yeung KT, Bih LI, Wang CH, Chen MI, Chien JC.. The relationship between sitting stability and functional performance in patients with paraplegia. Arch Phys Med Rehabil. 2003; 84: 1276– 1281. [DOI] [PubMed] [Google Scholar]
- 4. Thompson M, Medley A.. Forward and lateral sitting functional reach in younger, middle-aged, and older adults. J Geriatr Phys Ther. 2007; 30: 43– 48. [DOI] [PubMed] [Google Scholar]
- 5. Kaminski TR, Bock C, Gentile AM.. The coordination between trunk and arm motion during pointing movements. Exp Brain Res. 1995; 106: 457– 466. [DOI] [PubMed] [Google Scholar]
- 6. Chari VR, Kirby RL.. Lower-limb influence on sitting balance while reaching forward. Arch Phys Med Rehabil. 1986; 67: 730– 733. [DOI] [PubMed] [Google Scholar]
- 7. Potten YJ, Seelen HA, Drukker J, Reulen JP, Drost MR.. Postural muscle responses in the spinal cord injured persons during forward reaching. Ergonomics. 1999; 42: 1200– 1215. [DOI] [PubMed] [Google Scholar]
- 8. Seelen HA, Vuurman EF.. Compensatory muscle activity for sitting posture during upper extremity task performance in paraplegic persons. Scand J Rehabil Med. 1991; 23: 89– 96. [PubMed] [Google Scholar]
- 9. Schultheis MT, Rizzo AA.. The application of virtual reality technology in rehabilitation. Rehabil Psychol. 2001; 46: 296– 311. [Google Scholar]
- 10. Nash EB, Edwards GW, Thompson JA, Barfield W.. A review of presence and performance in virtual environments. Int J Human-Computer Interact. 2000; 12: 1– 41. [Google Scholar]
- 11. Rizzo SA, Kim JG.. A SWOT analysis of the field of virtual reality rehabilitation and therapy. Presence. 2001; 14: 119– 146 [Google Scholar]
- 12. Katz N, Ring H, Naveh Y, Kizony R, Feintuch U, Weiss PL.. Interactive virtual environment training for safe street crossing of right hemisphere stroke patients with unilateral spatial neglect. Disabil Rehabil. 2005; 27: 1235– 1243. [DOI] [PubMed] [Google Scholar]
- 13. Betker AL, Desai A, Nett C, Kapadia N, Szturm T.. Game-based exercises for dynamic short-sitting balance rehabilitation of people with chronic spinal cord and traumatic brain injuries. Phys Ther. 2007; 87: 1389– 1398. [DOI] [PubMed] [Google Scholar]
- 14. Dean CM, Shepherd RB.. Task-related training improves performance of seated reaching tasks after stroke a randomized controlled trial. Stroke. 1997; 28: 722– 728. [DOI] [PubMed] [Google Scholar]
- 15. Kizony R, Raz L, Katz N, Weingarden H, Weiss PL.. Video-capture virtual reality system for patients with paraplegic spinal cord injury. J Rehabil Res Dev. 2005; 42: 595– 608. [DOI] [PubMed] [Google Scholar]
- 16. Maynard FM, Bracken MB, Creasey GJ, . et al. International standards for neurological and functional classification of spinal cord injury. Spinal Cord. 1997; 35: 266– 274. [DOI] [PubMed] [Google Scholar]
- 17. Rand D, Kizony R, Weiss PT.. The Sony PlayStation II EyeToy: Low-cost virtual reality for use in rehabilitation. J Neurol Phys Ther. 2008; 32: 155– 163. [DOI] [PubMed] [Google Scholar]
- 18. Lynch SM, Leahy P, Barker SP.. Reliability of measurement obtained with modified functional reach test in subjects with spinal cord injury. Phys Ther. 1998; 78: 28– 133. [DOI] [PubMed] [Google Scholar]
- 19. Boswell-Ruys CL, Sturnieks DL, Harvey LA, Sherrington C, Middleton JW, Lord SR.. Validity and reliability of assessment tools for measuring unsupported sitting in people with a spinal cord injury. Arch Phys Med Rehabil. 2009; 90: 1571– 1577. [DOI] [PubMed] [Google Scholar]
- 20. Itzkovich M, Gelernter I, Biering-Sorensen F, . et al. The Spinal Cord Independence Measure (SCIM) version III: Reliability and validity in a multi-center international study. Disabil Rehabil. 2007; 29: 1926– 1933. [DOI] [PubMed] [Google Scholar]
- 21. Catz A, Itzkovich M, Agranov E, Ring H, Tamir A.. The Spinal Cord Independence Measure (SCIM): Sensitivity to functional changes in subgroups of spinal cord lesion patients. Spinal Cord. 2001; 39: 97– 100 [DOI] [PubMed] [Google Scholar]
- 22. Itzkovich M, Tamir A, Philo O, . et al. Reliability of the Catz-Itzkovich Spinal Cord Independence Measure assessment by interview and comparison with observation. Am J Phys Med Rehabil. 2003; 82: 267– 272. [DOI] [PubMed] [Google Scholar]
- 23. Sullivan GM, Feinn R.. Using effect size – or why the P value is not enough. J Grad Med Educ. 2012; 4: 279– 282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wall T, Feinn R, Chui K, Cheng MS.. The effects of the Nintendo Wii Fit on gait, balance, and quality of life in individuals with incomplete spinal cord injury. J Spinal Cord Med. 2015; 38: 777– 783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Harvey LA, Ristev D, Hossain MS, . et al. Training unsupported sitting does not improve ability to sit in people with recently acquired paraplegia: A randomised trial. J Physiother. 2011; 57: 83– 90. [DOI] [PubMed] [Google Scholar]
- 26. Winstein C, Stewart J.. Conditions of task practice for individuals with neurologic impairments. : Selzer M, Clarke S, Cohen L, . et al. , eds Textbook of Neural Repair and Rehabilitation. New York: Cambridge University Press; 2006: 89– 102. [Google Scholar]
- 27. Lott A, Bisson E, Lajoie Y, McComas J, Sveistrup H.. The effect of two types of virtual reality on voluntary center of pressure displacement. Cyberpsychol Behav. 2003; 6: 477– 485. [DOI] [PubMed] [Google Scholar]
- 28. Sveistrup H. Motor rehabilitation using virtual reality. J Neuroeng Rehabil. 2004; 10: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Witmer BG, Singer MJ.. Measuring presence in virtual environments: A presence questionnaire. Presence. 1998; 7: 225– 240. [Google Scholar]
- 30. Seelen HA, Potten YJ, Adam JJ, Drukker J, Spaans F, Huson A.. Postural motor programming in paraplegic patients during rehabilitation. Ergonomics. 1998; 41: 302– 316. [DOI] [PubMed] [Google Scholar]
- 31. Seelen HA, Janssen-Potten YJ, Adam JJ.. Motor preparation in postural control in seated spinal cord injured people. Ergonomics. 2001: 44: 457– 472. [DOI] [PubMed] [Google Scholar]


