Abstract
BACKGROUND
Earlier use of in-hospital plasma, platelets and red blood cells (RBCs) has improved survival in trauma patients with severe hemorrhage. Retrospective studies have associated improved early survival with prehospital blood product transfusion (PHT). We hypothesized that PHT of plasma and/or RBCs would result in improved survival after injury in patients transported by helicopter.
METHODS
Adult trauma patients transported by helicopter from the scene to nine Level 1 trauma centers were prospectively observed from Jan–Nov 2015. Five helicopter systems had plasma and/or RBCs while the other four helicopter systems used only crystalloid resuscitation. All patients meeting predetermined high risk criteria were analyzed. Patients receiving PHT were compared to patients not receiving PHT. Our primary analysis compared mortality at 3 hours, 24 hours, and 30 days, using logistic regression to adjust for confounders and site heterogeneity to model patients who were matched on propensity scores.
RESULTS
25,118 trauma patients were admitted, 2341 (9%) were transported by helicopter, of which 1058 (45%) met the highest risk criteria. 585/1058 patients were flown on helicopters carrying blood products. In the systems with blood available, prehospital median systolic blood pressure (125 vs 128) and GCS (7 vs 14) was significantly lower, while median ISS was significantly higher (21 vs 14). Unadjusted mortality was significantly higher in the systems with blood products available, at 3 (8.4% vs 3.6%), 24 (12.6% vs 8.9%) hours and 30 days (19.3% vs 13.3%). 24% of eligible patients received a prehospital transfusion. A median of 1 unit of RBCs and plasma were transfused prehospital. Of patients receiving PHT, 24% received only plasma, 7% received only RBCs and 69% received both. In the propensity score matching analysis (n=109), PHT was not significantly associated with mortality at any time point, although only 10% of the high risk sample were able to be matched.
CONCLUSIONS
Because of the unexpected imbalance in systolic blood pressure, GCS and ISS between systems with and without blood products on helicopters, matching was limited and the results of this study are inconclusive. With few units transfused to each patient and small outcome differences between groups, it is likely large, multicenter, randomized studies will be required to detect survival differences in this important population.
Keywords: trauma, transfusion, prehospital, plasma, resuscitation, damage control resuscitation
Background
Injury is the leading cause of death in adults and children between the ages of 1 and 44 years.1 The staggering numbers of years of productive life lost due to 199,800 deaths (with 20–30% potentially preventable) annually from injuries demands more urgent attention be paid to this major public health problem.2 Approximately 40% of in-hospital deaths among injured patients involve massive truncal hemorrhage that is considered potentially salvageable.3–5 Multiple retrospective military and civilian studies have reported that blood component ratios (i.e., Plasma: Platelets: red blood cells [RBC]) approaching whole blood (1:1:1) are associated with significant decreases in 24-hour and 30-day mortality among injured patients.6–20 However, platelets are virtually impossible to pre-position prehospital or in the emergency department (ED). Therefore, many centers have placed thawed or liquid plasma and RBCs in the ED and in pre-hospital settings, allowing earlier infusion of blood products and avoiding delayed achievement of a balanced transfusion.21–23 Recent prehospital transfusion (PHT) studies from the military and civilian hospitals have shown that prehospital plasma and RBCs are not only feasible, but associated with improved coagulation status on arrival and subsequent early outcomes.24–29
Prehospital resuscitation practices in the US differ significantly in approach, with most systems using crystalloids while a few offer red blood cells (RBCs) or a combination of plasma and RBCs. Use of blood product concentrates is much less common. To date, no large multicenter civilian studies have evaluated the use of prehospital plasma and RBCs in severely injured patients compared to crystalloids. Thus we proposed a pragmatic, multicenter, observational study to compare two different prehospital resuscitation approaches. The hypothesis of this study was that patients with severe traumatic injuries evacuated to level 1 trauma centers on air ambulances who received prehospital red blood cells and/or plasma would have lower in-hospital mortality compared to patients transferred by air ambulance who received only crystalloid.
Methods
Study Population
The Prehospital Resuscitation on Helicopter Study (PROHS) was a multicenter, prospective pragmatic, observational study of prehospital resuscitation approaches. Patients estimated to be greater than 15 years old (or greater than 50kg if age unknown) with traumatic injuries, who were transported by helicopter directly from the scene of injury to one of nine Level I trauma centers between January 26, 2015 and November 2, 2015 were eligible for the study. Of the 9 centers, 5 helicopter systems had plasma and/or red blood cells available on the helicopter and 4 helicopter systems used only crystalloid resuscitation. The study excluded prisoners and any transfers between hospitals. As this was an observational study, there were no study guidelines dictating resuscitation practice (i.e., blood products, crystalloids, or end of resuscitation). Sites agreed not to change resuscitation practices for the duration of the study. A subset of patients considered the highest risk population were directly observed by study staff based on at least one of the following criteria measured during prehospital helicopter transport: 1) heart rate greater than 120 beats per minute, 2) systolic blood pressure less than or equal to 90mmHg, 3) penetrating truncal injury, 4) tourniquet applied, 5) pelvic binder applied, 6) intubated prehospital, or 7) received blood products during transport. All analyses were performed among this highest risk population. All sites received appropriate approvals from their local institutional review boards and the US Army Human Research Protections Office.
Statistical Methods
Clinical data were entered and stored in a web based database, OpenClinica 3.9 Enterprise Edition. Unadjusted comparisons between the groups were performed using Wilcoxon rank sum tests on continuous variables and chi-squared tests to test proportions. Propensity score analysis, logistic regression, and Cox proportional hazards models were employed to analyze the primary outcome. Data analysis was performed using SAS 9.4 and R versions 3.2.3 and 3.3. Propensity scores were computed using the TWANG package.30 All analyses used a two-sided type 1 error level of 0.05.
Primary Analysis
The primary analysis utilized propensity scoring to estimate the average treatment effect of prehospital blood use on 3 hour, 24 hour and 30 day mortalities. The propensity for receiving prehospital blood products was modeled as a function of potential demographic and clinical confounders: age, gender, race (white, black, other), injury severity score (ISS), prehospital vital signs (systolic blood pressure, diastolic blood pressure, pulse), whether or not patients satisfied more than one of the highest risk criteria (yes/no), presence of any penetrating injury (yes/no), use of a prehospital lifesaving intervention (yes/no), time from the air team call to arrival to the ED (in minutes), whether the bleeding source was identified prehospital (yes/no) and site volume (the total number of trauma patients arriving via helicopter). Generalized boosted modeling (GBM) was used to compute the propensity score,31 which was defined as the predicted probability of receiving blood on the helicopter given baseline variables. After computing each patient’s propensity score, patients were matched using nearest neighbors matching without replacement with a caliper of 0.2, and with a 2:1 ratio of no prehospital blood received to prehospital blood received. Balance was obtained for the variables in the propensity model.
Matched patients were analyzed using generalized estimating equations (GEE), a procedure that accounts for the matching.32 The outcome was mortality (yes/no) and the covariate of interest was treatment; we present the average treatment effect for the treated (ATT) who received PHT. All models adjusted for site heterogeneity and results show the adjusted odds of death at 3 hours, 24 hours, or 30 days.
Pre-Planned Secondary Analyses
To investigate sensitivity of results to the propensity model, additional analyses were performed using all highest risk patients (unmatched). Logistic regression with a random intercept for site to adjust for heterogeneity, and Cox regression with a random intercept were both used to examine 3 hour, 24 hour and 30 day mortality. Residuals were assessed to verify model assumptions. For Cox regression, the proportional hazard assumption was assessed using the Supremum test and violations were further investigated using standard techniques. Age, sex and race were included in both models regardless of significance. All other covariates were retained if the Wald statistic p-value was less than 0.15. For logistic regression, ISS was categorized (1–8, 9–15, 16–24 and greater than 24). Final models included age, gender, race, and significant covariates, detailed in the result section. Odds ratios (OR) and 95% confidence intervals (95% CI) are reported for logistic regression models while hazard ratios (HR) and the 95% CIs are reported for Cox regression.
Results
A total of 25,118 trauma patients were admitted during the 10 month enrollment period to the nine participating centers, of which 2341 arrived by helicopter, and 1,058 met the highest risk criteria. Of the high risk sub-set, 585 arrived on helicopters with blood products available and 473 patients arrived via helicopters without blood available. (Table 1). One hundred forty two patients (24%) of patients transported on helicopters with blood products available actually received PHT and 916 patients did not (Table 2).
Table 1.
Patient characteristics by blood availability
| Prehospital Blood Products Available | |||||
|---|---|---|---|---|---|
|
| |||||
| Overall (N = 1058) |
No (N = 473) |
Yes (N = 585) |
P- value1 |
||
| Age (yrs) | Median (P25,P75) | 38 (25,55) | 39 (25,57) | 37 (26,54) | 0.36 |
|
| |||||
| Gender | Male N (%) | 751 (71.0) | 325 (68.7) | 426 (72.8) | 0.14 |
|
| |||||
| Race Group | White N (%) | 770 (72.8) | 371 (78.4) | 399 (68.2) | <.01 |
|
| |||||
| Other N (%) | 164 (15.5) | 34 (7.2) | 130 (22.2) | ||
|
| |||||
| Black N (%) | 124 (11.7) | 68 (14.4) | 56 (9.6) | ||
|
| |||||
| Systolic (mmHg) Blood Pressure | Median (P25,P75) | 126 (105,146) | 128 (109,148) | 125 (104,145) | 0.04 |
| Diastolic (mmHg) Blood Pressure | Median (P25,P75) | 78 (62,91) | 77 (63,91) | 78 (61,92) | 0.92 |
|
| |||||
| Pulse | Median (P25,P75) | 100 (83.5,122) | 102 (84,124) | 98 (83,120) | 0.10 |
|
| |||||
| GCS Score Total - Prehospital | Median (P25,P75) | 12 (3,15) | 14 (5,15) | 7 (3,15) | <.01 |
|
| |||||
| Injury Severity Score (ISS) | Median (P25,P75) | 17 (9,29) | 14 (5,26) | 21 (10,29) | <.01 |
|
| |||||
| ANY Penetrating Injury | Yes N (%) | 210 (19.8) | 84 (17.8) | 126 (21.5) | 0.13 |
|
| |||||
| Prehospital Lifesaving Interventions | Yes N (%) | 632 (59.7) | 197 (41.6) | 435 (74.4) | <.01 |
|
| |||||
| Air Team Call Time to ED Arrival(minutes) | Median (P25,P75) | 58 (48,73) | 60 (50,77) | 56 (47,70) | <.01 |
| Air Team Departure from Scene to ED Arrival (minutes) | Median (P25,P75) | 19 (15,27) | 21 (16,29) | 17 (14,24) | <.01 |
|
| |||||
| Satisfied More Than One Highest Risk Criteria | Yes N (%) | 362 (34.2) | 170 (35.9) | 192 (32.8) | 0.37 |
|
| |||||
| Bleeding Source Identified Prehospital | Yes N (%) | 549 (51.9) | 317 (67.0) | 232 (39.7) | <.01 |
|
| |||||
| 30-Day Status | Deceased N (%) | 176 (16.6) | 63 (13.3) | 113 (19.3) | <.01 |
|
| |||||
| 24-Hour Status | Deceased N (%) | 116 (11.0) | 42 (8.9) | 74 (12.6) | 0.05 |
|
| |||||
| 3-Hour Status | Deceased N (%) | 66 (6.2) | 17 (3.6) | 49 (8.4) | <.01 |
|
| |||||
| Time to Death from ED Arrival (hours) | Median (P25,P75) | 8.3 (0.8,45.8) | 13.5 (0.8,51.5) | 6.6 (0.8,42.0) | 0.49 |
The Wilcoxon rank sum and χ2 tests were used to compare groups for continuous and categorical characteristics, respectively
Table 2.
Patient characteristics by prehospital blood received
| Received Prehospital Blood | |||||
|---|---|---|---|---|---|
|
| |||||
| Overall (N = 1058) |
No (N = 916) |
Yes (N = 142) |
P-value1 | ||
| Age (yrs) | Median (P25,P75) | 38 (25,55) | 38 (25,55) | 41 (26,57) | 0.63 |
|
| |||||
| Gender | Male N (%) | 751 (71.0) | 650 (71.0) | 101 (71.1) | 0.97 |
|
| |||||
| Race Group | White N (%) | 770 (72.8) | 680 (74.2) | 90 (63.4) | <.01 |
|
| |||||
| Other N (%) | 164 (15.5) | 128 (14.0) | 36 (25.4) | ||
|
| |||||
| Black N (%) | 124 (11.7) | 108 (11.8) | 16 (11.3) | ||
|
| |||||
| Systolic (mmHg) Blood Pressure | Median (P25,P75) | 126 (105,146) | 129 (110,149) | 98 (80,124) | <.01 |
| Diastolic (mmHg) Blood Pressure | Median (P25,P75) | 78 (62,91) | 79 (65,92) | 62 (44,88) | <.01 |
|
| |||||
| Pulse | Median (P25,P75) | 100 (83.5,122) | 99 (83,121) | 107 (85,128) | 0.04 |
|
| |||||
| GCS Score Total - Prehospital | Median (P25,P75) | 12 (3,15) | 11.5 (3,15) | 13 (3,15) | 0.88 |
|
| |||||
| Injury Severity Score (ISS) | Median (P25,P75) | 17 (9,29) | 17 (6,27) | 25 (13,34) | <.01 |
|
| |||||
| ANY Penetrating Injury | Yes N (%) | 210 (19.8) | 164 (17.9) | 46 (32.4) | <.01 |
|
| |||||
| Prehospital Lifesaving Interventions | Yes N (%) | 632 (59.7) | 525 (57.3) | 107 (75.4) | <.01 |
|
| |||||
| Air Team Call Time to ED Arrival (minutes) | Median (P25,P75) | 58 (48,73) | 58 (48,74) | 55 (48,68) | 0.04 |
| Air Team Departure from Scene to ED Arrival (minutes) | Median (P25,P75) | 19 (15,27) | 19 (15,27) | 18 (14,24) | 0.14 |
|
| |||||
| Satisfied More Than One Highest Risk Criteria | Yes N (%) | 362 (34.2) | 277 (30.2) | 85 (59.9) | <.01 |
|
| |||||
| Bleeding Source Identified Prehospital | Yes N (%) | 549 (51.9) | 431 (47.1) | 118 (83.1) | <.01 |
|
| |||||
| 30-Day Status | Deceased N (%) | 176 (16.6) | 140 (15.3) | 36 (25.4) | <.01 |
|
| |||||
| 24-Hour Status | Deceased N (%) | 116 (11.0) | 89 (9.7) | 27 (19.0) | <.01 |
|
| |||||
| 3-Hour Status | Deceased N (%) | 66 (6.2) | 43 (4.7) | 23 (16.2) | <.01 |
|
| |||||
| Time to Death from ED Arrival (hours) | Median (P25,P75) | 8.3 (0.8,45.8) | 13.2 (1.1,50.5) | 2.2 (0.2,23.7) | 0.03 |
The Wilcoxon rank sum and χ2 tests were used to compare groups for continuous and categorical characteristics, respectively
Comparison of systems with prehospital blood available vs. not available
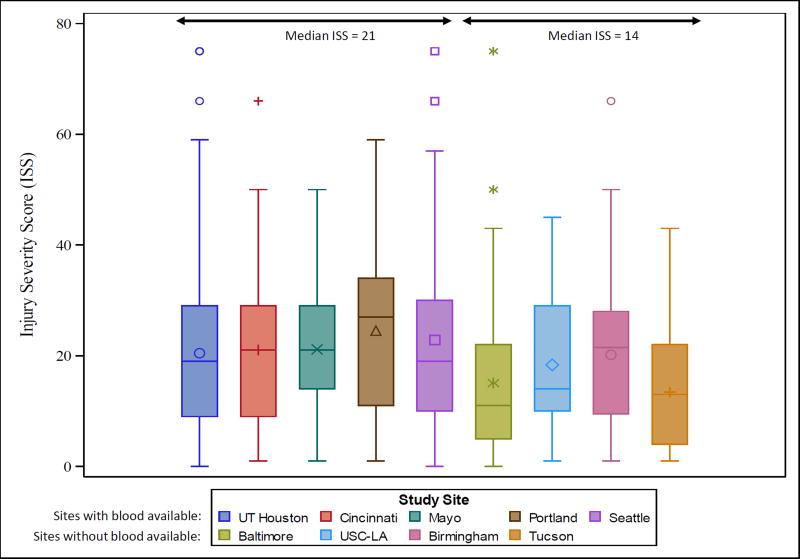
Comparing patients with prehospital blood available versus not available (Table 1), there were no significant differences in age, gender, prehospital diastolic blood pressure or pulse, any penetrating injury or having met more than one highest risk criteria. However, there was a lower proportion of patients classified as other race (not white or black) in the no blood available group compared to the blood available group. Median prehospital systolic blood pressure and GCS were higher among patients who did not have prehospital blood available, while median ISS was lower. Patients on helicopters with blood available had shorter median time from air team call to arrival in the ED. Patients with blood available on the helicopter also had a significantly higher use of prehospital lifesaving interventions and fewer patients whose bleeding sources were identified compared to those without blood available. Figure 1 presents the boxplots for ISS of the patients from each site, showing the higher ISS among sites with blood available. This difference created substantial difficulty in balancing the group of patients who received PHT with those who did not. The imbalance in GCS, SBP and ISS contributed to the difference in unadjusted mortality. In the systems with blood products available, unadjusted mortality was significantly higher at 3 hours (8.4% vs 3.6%, p<0.01) and 24 hours (12.6% vs 8.9%, p=0.05) and at 30 days (19.3% vs 13.3%).
Figure 1. Distribution of ISS for study sites.
Figure 1 presents boxplots of the distribution of ISS for each center of the study. Note that the medians of the sites with blood available on the helicopter all have distributions that are shifted higher than those of the sites without blood available. This shift shows that the ISS of patients arriving to sites with blood available prehospital are generally higher than the ISS of patients arriving to sites without blood available prehospital.
Comparison of patients with PHT and those not administered PHT
Considering patient characteristics in those receiving PHT (Table 2), there were no differences in age, gender or prehospital GCS versus those who did not. Those who did not receive PHT had significantly higher median prehospital systolic and diastolic blood pressures, a longer median number of minutes from air team call to ED arrival, and lower median ISS and prehospital heart rate than those who received PHT. The group who did not receive PHT also had a higher proportion of whites, fewer penetrating injuries, received fewer lifesaving interventions, had fewer bleeding sources identified and had a lower proportion of patients who met more than one of the highest risk criteria. Of patients receiving prehospital transfusion, 24% received only plasma, 7% received only RBCs and 69% received both. Those receiving PHT had a higher unadjusted mortality at 3 hours (16.2% vs 4.7%) and 24 hours (19.0% vs 9.7%) and at 30 days (25.4% vs 15.3%), all p < 0.01.
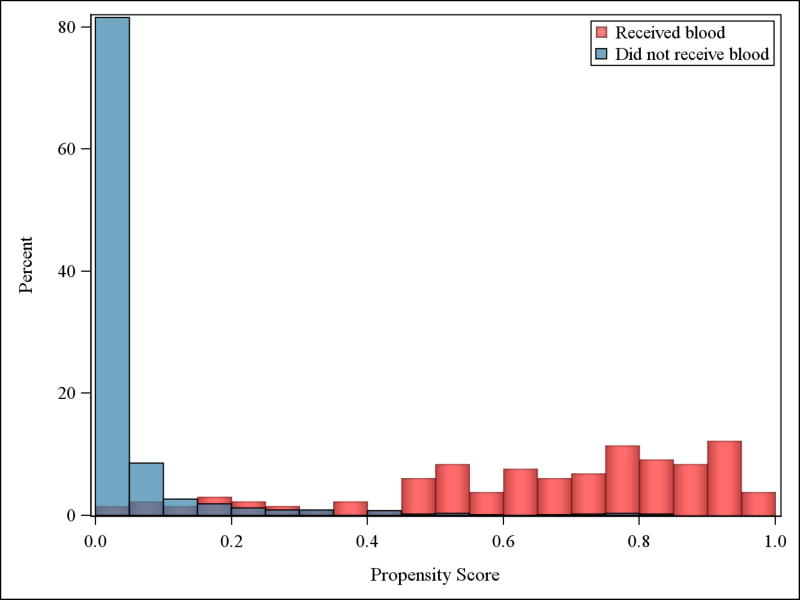
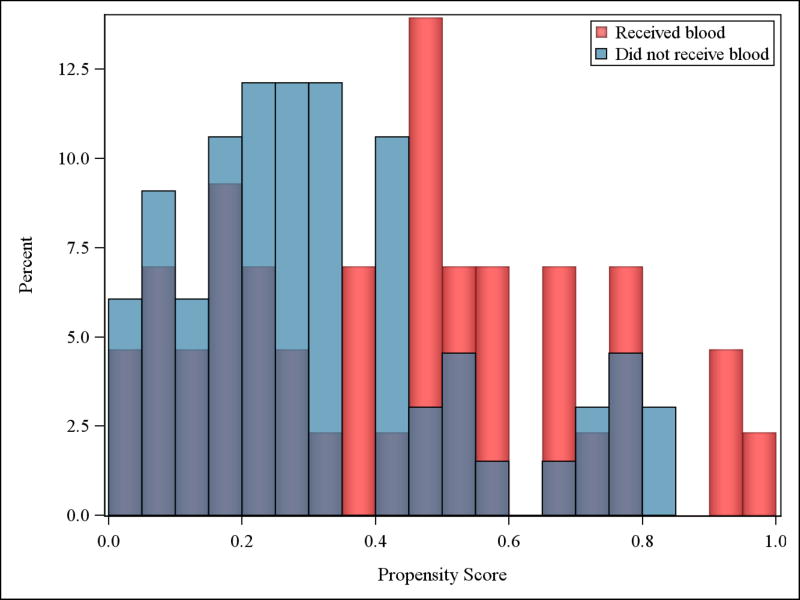
Results of the preplanned primary analysis
Patients were matched based on their propensity score, resulting in only 43 patients who received PHT and 66 patients who did not, for a total sample of 109 subjects (10% of our total sample). Although the statistical design called for matching 2 patients who did not receive prehospital blood products to one patient who did receive prehospital blood products, there were not enough matches within the caliper of 0.2 to maintain a 2:1 ratio for all patients who received prehospital blood products. The distributions of the propensity scores for the full data set (panel a) and the matched data set (panel b) are shown in Figure 2. The distribution of propensity scores among those who received blood (red bars) had definitive characteristics that gave them mostly high propensity scores, while those who did not receive blood had primarily low propensity scores (blue bars), including those who did not have blood available on the helicopters. Once matched, the propensity scores had more overlap, (figure 2, panel b) but there are still fewer patients who received blood and had a low propensity score (red bars), and likewise fewer patients who did not receive blood with a high propensity score (blue bars). After matching, the twelve variables included in the propensity score (see table 3) were balanced, except for age. A difference in median age, of close to 9 years, remained.
Figure 2. Distributions of propensity scores among matched and unmatched patients.
Panel A shows the distribution of propensity scores for all patients in the highest risk group who did not receive prehospital transfusion (PHT) (n=916, blue bars) relative to the distribution of propensity scores for all patients in the highest risk group who did receive PHT (n=142, red bars). Panel B shows the distribution of propensity scores in the matched patients who did not receive PHT (n=66, blue bars), relative to the distribution of propensity scores in the matched patients who received PHT (n=43, red bars). Among those patients who did not receive a PHT, very few had a high propensity score. Similarly, among those patients who did receive a PHT, very few had a low propensity score. This striking difference produces a small area of overlap between the two distributions (denoted by the purple area), representing the limited pool of similar patients across treatment groups from which to form suitable matched pairs. As expected, the distribution of the matched sample shows better overlap in purple, but still represents a small number of patients compared to the total population. Also note that the scale on the y-axis is different for panels A and B.
Table 3.
Demographic and baseline injury characteristics of the matched sample
| Received Blood Prehospital | ||||
|---|---|---|---|---|
|
| ||||
| Overall (N = 109) |
No (N = 66) |
Yes (N = 43) |
||
| Age (yrs) | Median (P25,P75) | 41 (26,60) | 39 (26,56) | 48 (27,62) |
|
| ||||
| Gender | Male N (%) | 77 (70.6) | 48 (72.7) | 29 (67.4) |
|
| ||||
| Race Group | White N (%) | 78 (71.6) | 45 (68.2) | 33 (76.7) |
|
| ||||
| Black N (%) | 9 (8.3) | 7 (10.6) | 2 (4.7) | |
|
| ||||
| Other N (%) | 22 (20.2) | 14 (21.2) | 8 (18.6) | |
|
| ||||
| Systolic (mmHg) Blood Pressure | Median (P25,P75) | 110 (88,129) | 105 (88,128) | 110 (88,133) |
| Diastolic (mmHg) Blood Pressure | Median (P25,P75) | 67 (52,88) | 66.5 (52,88) | 67 (50,90) |
|
| ||||
| Pulse | Median (P25,P75) | 105 (90,123) | 100 (86,123) | 110 (94,125) |
|
| ||||
| Injury Severity Score (ISS) | Median (P25,P75) | 24 (10,34) | 22 (10,34) | 24 (10,34) |
|
| ||||
| ANY Penetrating Injury | Yes N (%) | 27 (24.8) | 18 (27.3) | 9 (20.9) |
|
| ||||
| Prehospital Lifesaving Interventions | Yes N (%) | 75 (68.8) | 45 (68.2) | 30 (69.8) |
|
| ||||
| Air Team Call Time to ED Arrival (minutes) | Median (P25,P75) | 57 (47,71) | 56 (46,68) | 58 (50,76) |
|
| ||||
| Satisfied More than One Highest Risk Criteria | Yes N (%) | 51 (46.8) | 31 (47.0) | 20 (46.5) |
|
| ||||
| Bleeding Source Identified Prehospital | Yes N (%) | 73 (67.0) | 45 (68.2) | 28 (65.1) |
|
| ||||
| 30-Day Status | Deceased N (%) | 22 (20.2) | 14 (21.2) | 8 (18.6) |
|
| ||||
| 24-Hour Status | Deceased N (%) | 15 (13.8) | 10 (15.2) | 5 (11.6) |
|
| ||||
| 3-Hour Status | Deceased N (%) | 12 (11.0) | 8 (12.1) | 4 (9.3) |
|
| ||||
| Time to Death from ED Arrival (hours) | Median (P25,P75) | 2.6 (0.1,42.0) | 2.1 (0.1,33.2) | 5.6 (0.2,155) |
The results of the generalized estimating equation models after matching on propensity scores are presented in Table 4. There were no significant associations with receiving prehospital blood products on 3-hour mortality (OR 0.74, 95% CI 0.24–2.26, p=0.60), 24-hour mortality (OR 0.74, 95% CI 0.25–2.17, p=0.58), or 30-day mortality (OR 0.85, 95% CI 0.32–2.28, p=0.75).
Table 4.
Results of primary and sensitivity analyses
| Primary Analysis | Sensitivity Analysis | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
Propensity Scorea adjusted GEE (n=109) |
Logistic Regression (N=1030) |
Cox Regression (N=1020) | |||||||
| Mortality | Odds ratio |
95% CI | P- value |
Odds ratio |
95% CI | P- value |
Hazard ratio |
95% CI |
P- value |
| 3-hour | 0.74 | (0.24, 2.26) | 0.60 | 1.69b | (0.88, 3.26) | 0.12 | 1.40e | (0.82, 2.39) | 0.22 |
| 24-hour | 0.74 | (0.25, 2.17) | 0.58 | 0.83c | (0.44, 1.57) | 0.56 | 1.12f | (0.41, 3.06) | 0.83 |
| 30-day | 0.85 | (0.32, 2.28) | 0.75 | 0.75d | (0.40, 1.42) | 0.38 | 1.97g | (0.81, 4.79) | 0.13 |
GEE Generalized Estimating Equations; CI Confidence Interval
Propensity score included: age, gender, race, injury severity score (ISS), systolic blood pressure, diastolic blood pressure, pulse, whether or not the patient satisfied more than one of the highest risk criteria, presence of any penetrating injury, use of a prehospital lifesaving intervention, time from the air team call time to arrival at the emergency department (ED), if the bleeding site was identified prehospital, and site volume.
Adjusted for age, race, gender, systolic blood pressure, and having a prehospital lifesaving intervention
Adjusted for age, race, gender, systolic blood pressure, satisfying more than one high risk criteria, having any penetrating injury, having a prehospital lifesaving intervention, and ISS.
Adjusted for age, race, gender, pulse, minutes form the air team call time to arrival at the ED, satisfying more than one high risk criteria, having a prehospital lifesaving intervention, having the bleeding source identified prehospital and ISS.
Adjusted for age, race, gender, systolic blood pressure and having a prehospital lifesaving intervention
Adjusted for age, race, gender, systolic blood pressure, bleeding source identified prehospital, having a prehospital lifesaving intervention, ISS, and survival time interactions with systolic blood pressure, ISS, and prehospital blood transfusion
Adjusted for age, race, gender, pulse satisfying more than one high risk criteria, use of a lifesaving intervention, having bleeding source identified prehospital, ISS, and time interactions with pulse, selected more than one high risk criteria, ISS, and prehospital blood transfusion
Results of the pre-planned secondary analyses
Additional preplanned secondary analyses were performed to further examine any potential association of mortality with PHT in all highest risk patients adjusting for baseline covariates. The logistic regression models for each mortality endpoint (3 hours, 24 hours, and 30 days) differed in the covariates included (shown in the footnotes of Table 4). Receiving blood prehospital was not significantly associated with mortality at 3 hours (OR 1.69 95% CI 0.88–3.26, p=0.12) in the adjusted logistic regression model. Similarly, there was no significant association in the logistic regression models for 24 hour (OR 0.83, 95% CI 0.44–1.57, p=0.56) or 30 day mortality (OR 0.75, 95% CI 0.40–1.42 p=0.38) after adjustment for covariates.
Each of the three adjusted Cox regression models also differed in the covariates included in the models depending on the significance of covariates for that model/ timepoint (see footnotes of Table 4). The Cox proportional hazard model failed to converge when modeling deaths within 3 hours of arrival because one site did not have any patient deaths within 3 hours. Therefore, the model for 3 hour survival excluded the random effect for site, and prehospital blood product administration was not significantly associated with mortality at 3 hours (HR 1.40, 95% CI 0.82–2.39, p=0.22). No significant associations in the Cox models were seen at 24 hours (HR 1.12, 95% CI 0.41–3.06, p=0.83) or 30 days (HR 1.97, 95% CI 0.81–4.79, p=0.13) after adjustment for covariates including site.
Discussion
This study investigated the effect of the use of prehospital blood products in resuscitation at nine different sites. It is well known that as a group, patients arriving to level 1 trauma centers via helicopter have greater injury severity compared to those arriving by ground ambulance.33–35 The design of this study was based on the assumption that the distribution of severely injured patients on helicopters was independent of prehospital blood product availability. However, in this study, the patient population arriving on helicopters with prehospital blood products available were more severely injured than those arriving on helicopters without prehospital blood available. This created substantial difficulty in balancing the groups using propensity score matching, which resulted in a very small number of patients who were able to be matched on a similar propensity score (10%), despite using a large caliper of 0.2. In the primary analysis, prehospital blood product use was not significantly associated with 3 hour, 24 hour or 30 day mortality. However, the unexpected and significant differences in injury severity score, GCS and SBP resulted in lower power and therefore, the results are inconclusive.
The preplanned secondary analysis utilizing logistic and Cox regression models were also not able to correctly adjust for differences between the patients receiving and not receiving PHT. In these models, different covariates were necessary in each model to adjust for baseline differences. These models also revealed nonsignificant results in the opposite direction as the primary analysis using propensity score matching, suggesting that a large randomized trial will be required to answer this question. Using the estimated mortality rates from the 109 matched individuals and the proportion of patients with and without PHT in our study, to obtain 80% power to detect a 4% absolute reduction in all-cause mortality would require 3996 patients for 3 hour, 4970 patients for 24 hour and 6672 patients for a 30 day survival study.
Prehospital transfusion is a logical extension of the concept of damage control resuscitation. In 2007, several authors of this current study proposed that damage control resuscitation (DCR) resuscitation for rapidly bleeding patients should include limited crystalloid and increased amounts of plasma and platelets.6 Over the last decade, many investigators have validated this concept by publishing single and multicenter retrospective, prospective observational studies, and prospective randomized clinical trials.7–20 These studies have been performed at multiple combat and civilian sites totaling many thousands of hemorrhaging patients. As a result, hospital-based transfusion practice for injured patients has changed, with decreased use of crystalloid and increased use of blood products as a primary resuscitation modality, resulting in decreased complications and improved survival.37–43
To reach the ideal of a seamless continuum of care between the prehospital and hospital environments, the concept of damage control resuscitation has been extended to the prehospital arena.44–51 The military has led this approach by carrying red blood cells (RBCs) and plasma on some of their helicopters in Afghanistan, publishing a prehospital transfusion rate of greater than 15% and a significant association with improved outcomes.24 Subsequently, multiple civilian centers have placed plasma and/or RBCs on their helicopters and published improved outcomes.25–29 Building on this military and civilian experience, in 2011 Memorial Herman Hospital- Texas Medical Center placed 2 units of thawed/liquid plasma and 2 units of RBCs on their 4 civilian helicopters. They documented a 19% transfusion rate in severely injured civilian trauma patients, and similar to the military experience there was an association with improved outcomes.25 The Pittsburg and Mayo trauma groups have likewise documented an association between prehospital transfusion and improved outcomes.26–29
Prehospital plasma and RBCs are now the standard of care on many helicopter and several ground EMS systems, with rates of transfusion in line with the 24% shown in the present study. Liquid and thawed plasma are now used early in the prehospital environment in a number of health care systems. In several centers, dried plasma, PCCs, cryoprecipitate and fibrinogen concentrates are available for prehospital use as well.52–56 Finally, position papers from civilian and military thought leaders have been recently published, clearly stating the desire for prehospital blood products and high quality studies to determine their efficacy.44– 51, 57, 58 In summary, a series of retrospective studies have shown associations with improved outcomes with blood product based resuscitation compared to crystalloid. However a recent comprehensive review of this subject by Smith et al has concluded that there is no effect, albeit the quality of all available data are very low.59 To help answer this issue, over the last two years the Department of Defense (DoD) has initiated two multicenter randomized studies of prehospital plasma versus crystalloid resuscitation in severely injured patients.60–61
In our study, in the systems that have blood available prehospital, 142 patients received a transfusion, with site specific rates of transfusion ranging from 4–47% for an average of 24% (142/585). This rate is similar to earlier studies, and that reported by the military in the experience in Afghanistan. There was a significant difference (3 minutes) between groups in call time to ED arrival (median 58 minutes), with PHT patients arriving faster than those not receiving blood (Table 2). It appears that PHT does not negatively affect flight time. A median of 1 unit of RBCs and plasma were transfused prehospital during a flight time of 18 minutes. Of patients receiving PHT, 24% received only plasma, 7% received only RBCs and 69% received both. It will be interesting in future studies to evaluate the impact of different PHT strategies on outcome.
The strengths of our study are its prospective and observational design, with in house 24/7 research personnel observing the patients, facilitating the collection of high quality data at nine centers over a short period of time. The major weakness of the study was the unexpected difference in SBP, GCS and ISS between sites with and without blood products available. It is unclear why this occurred, as our previous multicenter trauma transfusion studies did not demonstrate significant site differences in severity of injury.9, 18, 19 In regions with helicopter agencies that have the capability of PHT, there might be a bias for prehospital personnel to call those helicopter services with blood products on board to transport more severely injured patients, however trying to define this issue at nine different trauma regions across the country is beyond the scope of this effort. Clearly, future studies must take this issue into account when designing non-randomized studies.
Conclusion
Because of the unexpected imbalance in injury severity between systems with and without blood products on helicopters, all analyses were inconclusive. With few units transfused to each patient and small outcome differences between groups, large randomized studies will be required to detect significant survival differences in this important population.
Acknowledgments
Source of Funding/ Role of Sponsors: This work was sponsored by the U.S. National Heart, Lung, and Blood Institute (U01HL077863) and the U.S. Department of Defense. No sponsors were involved in the design, collection, management, or analysis of the data; preparation of the manuscript; or the decision to submit the manuscript for publication. The content is the sole responsibility of the authors and is not to be construed as official or as reflecting the views of any sponsor.
Prehospital Resuscitation on Helicopter Study (PROHS) Study Group:
Clinical Coordinating Center: John B. Holcomb, MD; Charles E. Wade, PhD; Erin E. Fox, PhD; Jeanette M. Podbielski, RN. Jeffrey S. Tomasek, MD; Deborah J. del Junco, PhD.
Data Coordinating Center: Michael D. Swartz, PhD; Stacia M. DeSantis, PhD; Savitri N. Appana, MS; Thomas J. Greene, MPH; Misung Yi, MS; Michael O. Gonzalez, MS; Sarah Baraniuk, PhD.
Resuscitation Outcomes Consortium at the University of Washington: Gerald van Belle, PhD; Brian G. Leroux, PhD.
PROHS Clinical Sites (listed in order of number of highest risk patients enrolled): University of Texas Health Science Center at Houston: Carrie L. Howard, MA, MBA; Amanda Haymaker.
Shock, Trauma and Anesthesiology Research - Organized Research Center (STAR-ORC), R Adams Cowley Shock Trauma Center, University of Maryland Medical Center: Deborah M. Stein, MD, MPH; Thomas M. Scalea, MD; Benjamin Ayd; Pratik Das; Anthony V. Herrera, MS.
University of Washington: Eileen M. Bulger, MD; Bryce R. H. Robinson, MD; Patricia Klotz, RN; Aniqa Minhas, BS.
University of Alabama at Birmingham: Jeffrey D. Kerby, MD, PhD; Sherry M. Melton, MD, MSHA; Carolyn R. Williams, RN, MSHI; Shannon W. Stephens, EMTP.
University of Cincinnati: Michael Goodman, MD; Jay A. Johannigman, MD; Jason McMullan, MD; Richard D. Branson, MSc, RRT; Dina Gomaa, BS, RRT; Christopher Barczak, BS, MT(ASCP).
Oregon Health and Science University: Martin A. Schreiber, MD; Samantha J. Underwood, MS; Cheri Watson, BS.
Mayo Clinic: Martin D. Zielinski, MD; James R. Stubbs, MD; Amy Headlee.
University of Arizona: Terence O’Keeffe, MBChB, MSPH; Peter Rhee, MD; Laurel L. Rokowski, RN, BSN, MKT; John Santoro, AA; Andrea Seach, BS; David Bradford, BS; Michelle Fealk, BA; Fortesa Latifi, BS.
University of Southern California: Kenji Inaba, MD; Henry Kim, MD; Carl Chudnofsky, MD; Monica D. Wong, MS.
Footnotes
Trial Registration: Clinicaltrials.gov, NCT02272465
Conflicts of Interest: No conflicts of interest have been declared by any author in regards to this manuscript.
Presentation: This manuscript was presented at the 2016 Military Health System Research Symposium
Author Contributions:
Study concept and design: Holcomb, Fox, Wade, Podbielski
Acquisition of data: Bulger, Goodman, Holcomb, Inaba, Kerby, O’Keeffe, Schreiber, Stein, Zielinski, Podbielski, Tomasek
Analysis and interpretation of data: Swartz, DeSantis, Greene, Fox, Appana, Yi
Drafting of the manuscript: Holcomb, Fox, Swartz
Critical revision of the manuscript for important intellectual content: Holcomb, Swartz, DeSantis, Greene, Fox, Stein, Bulger, Kerby, Goodman, Schreiber, Zielinski, O’Keeffe, Inaba, Tomasek, Podbielski, Appana, Yi, Wade
References
- 1.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS) Fatal Injury Data. 2016 [Google Scholar]
- 2.A National Trauma Care System: Integrating Military and Civilian Trauma Systems to Achieve Zero Preventable Deaths After Injury. [Accessed November 22, 2016]; http://www.nationalacademies.org/hmd/Reports/2016/A-National-Trauma-Care-System-Integrating-Military-and-Civilian-Trauma-Systems.aspx. [PubMed]
- 3.Oyeniyi BT, Fox EE, Scerbo M, Tomasek JS, Wade CE, Holcomb JB. Trends in 1029 trauma deaths at a level 1 trauma center: Impact of a bleeding control bundle of care. Injury. 2016 Nov;:3. doi: 10.1016/j.injury.2016.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tisherman SA, Schmicker RH, Brasel KJ, Bulger EM, Kerby JD, Minei JP, Powell JL, Reiff DA, Rizoli SB, Schreiber MA. Detailed description of all deaths in both the shock and traumatic brain injury hypertonic saline trials of the Resuscitation Outcomes Consortium. Ann Surg. 2015 Mar;261(3):586–90. doi: 10.1097/SLA.0000000000000837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rhee P, Joseph B, Pandit V, Aziz H, Vercruysse G, Kulvatunyou N, et al. Increasing trauma deaths in the united states. Ann Surg. 2014;260(1):13–21. doi: 10.1097/SLA.0000000000000600. [DOI] [PubMed] [Google Scholar]
- 6.Holcomb JB, Jenkins D, Rhee P, Johannigman J, Mahoney P, Mehta S, Cox ED, Gehrke MJ, Beilman GJ, Schreiber M, Flaherty SF, Grathwohl KW, Spinella PC, Perkins JG, Beekley AC, McMullin NR, Park MS, Gonzalez EA, Wade CE, Dubick MA, Schwab CW, Moore FA, Champion HR, Hoyt DB, Hess JR. Damage control resuscitation: directly addressing the early coagulopathy of trauma. J Trauma. 2007;62:307–10. doi: 10.1097/TA.0b013e3180324124. [DOI] [PubMed] [Google Scholar]
- 7.Borgman MA, Spinella PC, Perkins JG, Grathwohl KW, Repine T, Beekley AC, Sebesta J, Jenkins D, Wade CE, Holcomb JB. The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital. J Trauma. 2007;63:805–13. doi: 10.1097/TA.0b013e3181271ba3. [DOI] [PubMed] [Google Scholar]
- 8.Huber-Wagner S, Qvick M, Mussack T, et al. Massive blood transfusion and outcome in 1062 polytrauma patients: a prospective study based on the Trauma Registry of the German Trauma Society. Vox Sang. 2007 Jan;92(1):69–78. doi: 10.1111/j.1423-0410.2006.00858.x. [DOI] [PubMed] [Google Scholar]
- 9.Holcomb JB, Wade CE, Michalek JE, Chisholm GB, Zarzabal LA, Schreiber MA, Gonzalez EA, Pomper GJ, Perkins JG, Spinella PC, Williams KL, Park MS. Increased plasma and platelet to red blood cell ratios improves outcome in 466 massively transfused civilian trauma patients. Ann Surg. 2008;248:447–58. doi: 10.1097/SLA.0b013e318185a9ad. [DOI] [PubMed] [Google Scholar]
- 10.Duchesne JC, Hunt JP, Wahl G, et al. Review of current blood transfusions strategies in a mature level I trauma center: were we wrong for the last 60 years? J Trauma. 2008 Aug;65(2):272–276. doi: 10.1097/TA.0b013e31817e5166. discussion 276–278. [DOI] [PubMed] [Google Scholar]
- 11.Perkins JG, Cap AP, Spinella PC, Blackbourne LH, Grathwohl KW, Repine TB, Ketchum L, Waterman P, Lee RE, Beekley AC, Sebesta JA, Shorr AF, Wade CE, Holcomb JB. An evaluation of the impact of apheresis platelets used in the setting of massively transfused trauma patients. J Trauma. 2009 Apr;66(4 Suppl):S77–84. doi: 10.1097/TA.0b013e31819d8936. discussion S84-5. [DOI] [PubMed] [Google Scholar]
- 12.Maegele M. Frequency, risk stratification and therapeutic management of acute post-traumatic coagulopathy. Vox Sang. 2009 Jul;97(1):39–49. doi: 10.1111/j.1423-0410.2009.01179.x. [DOI] [PubMed] [Google Scholar]
- 13.Shaz BH, Dente CJ, Nicholas J, et al. Increased number of coagulation products in relationship to red blood cell products transfused improves mortality in trauma patients. Transfusion. 2010 Feb;50(2):493–500. doi: 10.1111/j.1537-2995.2009.02414.x. [DOI] [PubMed] [Google Scholar]
- 14.Cotton BA, Reddy N, Hatch QM, LeFebvre E, Wade CE, Kozar RA, Gill BS, Albarado R, McNutt MK, Holcomb JB. Damage control resuscitation is associated with a reduction in resuscitation volumes and improvement in survival in 390 damage control laparotomy patients. Ann Surg. 2011;254:598–605. doi: 10.1097/SLA.0b013e318230089e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pidcoke HF, Aden JK, Mora AG, Borgman MA, Spinella PC, Dubick MA, Blackbourne LH, Cap AP. Ten-year analysis of transfusion in Operation Iraqi Freedom and Operation Enduring Freedom: increased plasma and platelet use correlates with improved survival. J Trauma Acute Care Surg. 2012;73:S445–52. doi: 10.1097/TA.0b013e3182754796. [DOI] [PubMed] [Google Scholar]
- 16.Cap AP, Spinella PC, Borgman MA, Blackbourne LH, Perkins JG. Timing and location of blood product transfusion and outcomes in massively transfused combat casualties. J Trauma Acute Care Surg. 2012;73:S89. doi: 10.1097/TA.0b013e318260625a. [DOI] [PubMed] [Google Scholar]
- 17.Kautza BC, Cohen MJ, Cuschieri J, Minei JP, Brackenridge SC, Maier RV, Harbrecht BG, Moore EE, Billiar TR, Peitzman AB, Sperry JL. Changes in massive transfusion over time: an early shift in the right direction? J Trauma Acute Care Surg. 2012;72:106–11. doi: 10.1097/TA.0b013e3182410a3c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holcomb JB, del Junco DJ, Fox EE, Wade CE, Cohen MJ, Schreiber MA, Alarcon LH, Bai Y, Brasel KJ, Bulger EM, Cotton BA, Matijevic N, Muskat P, Myers JG, Phelan HA, White CE, Zhang J, Rahbar MH. The prospective, observational, multicenter, major trauma transfusion (PROMMTT) study: comparative effectiveness of a time-varying treatment with competing risks. JAMA Surg. 2013;148:127–36. doi: 10.1001/2013.jamasurg.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holcomb JB, Tilley BC, Baraniuk S, Fox EE, Wade CE, Podbielski JM, del Junco DJ, Brasel KJ, Bulger EM, Callcut RA, Cohen MJ, Cotton BA, Fabian TC, Inaba K, Kerby JD, Muskat P, O'Keeffe T, Rizoli S, Robinson BR, Scalea TM, Schreiber MA, Stein DM, Weinberg JA, Callum JL, Hess JR, Matijevic N, Miller CN, Pittet JF, Hoyt DB, Pearson GD, Leroux B, van Belle G PROPPR Study Group. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA. 2015 Feb 3;313(5):471–82. doi: 10.1001/jama.2015.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johansson PI, Sorensen AM, Larsen CF, et al. Low hemorrhage-related mortality in trauma patients in a Level I trauma center employing transfusion packages and early thromboelastography-directed hemostatic resuscitation with plasma and platelets. Transfusion. 2013 Dec;53(12):3088–3099. doi: 10.1111/trf.12214. [DOI] [PubMed] [Google Scholar]
- 21.Radwan ZA, Bai Y, Matijevic N, del Junco DJ, McCarthy JJ, Wade CE, Holcomb JB, Cotton BA. An emergency department thawed plasma protocol for severely injured patients. JAMA Surg. 2013;148:170–5. doi: 10.1001/jamasurgery.2013.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wehrli G, Taylor NE, Haines AL, Brady TW, Mintz PD. Instituting a thawed plasma procedure: it just makes sense and saves cents. Transfusion. 2009;49:2625–30. doi: 10.1111/j.1537-2995.2009.02342.x. [DOI] [PubMed] [Google Scholar]
- 23.Mehr CR, Gupta R, von Recklinghausen FM, Szczepiorkowski ZM, Dunbar NM. Balancing risk and benefit: maintenance of a thawed group A plasma inventory for trauma patients requiring massive transfusion. J Trauma Acute Care Surg. 2013;74:1425–31. doi: 10.1097/TA.0b013e31828b813e. [DOI] [PubMed] [Google Scholar]
- 24.Morrison JJ, Oh J, DuBose JJ, O’Reilly DJ, Russell RJ, Blackbourne LH, Midwinter MJ, Rasmussen TE. En-route care capability from point of injury impacts mortality after severe wartime injury. Ann Surg. 2013;257:330–4. doi: 10.1097/SLA.0b013e31827eefcf. [DOI] [PubMed] [Google Scholar]
- 25.Holcomb JB, Donathan DP, Cotton BA, Del Junco DJ, Brown G, Wenckstern TV, Podbielski JM, Camp EA, Hobbs R, Bai Y, Brito M, Hartwell E, Duke JR, Wade CE. Prehospital Transfusion of Plasma and Red Blood Cells in Trauma Patients. Prehosp Emerg Care. 2015 Jan-Mar;19(1):1–9. doi: 10.3109/10903127.2014.923077. [DOI] [PubMed] [Google Scholar]
- 26.Kim BD, Zielinski MD, Jenkins DH, Schiller HJ, Berns KS, Zietlow SP. The effects of prehospital plasma on patients with injury: a prehospital plasma resuscitation. J Trauma Acute Care Surg. 2012;73:S49–53. doi: 10.1097/TA.0b013e31826060ff. [DOI] [PubMed] [Google Scholar]
- 27.Zielinski MD, Smoot DL, Stubbs JR, Jenkins DH, Park MS, Zietlow SP. The development and feasibility of a remote damage control resuscitation prehospital plasma transfusion protocol for warfarin reversal for patients with traumatic brain injury. Transfusion. 2013;53(Suppl 1):59S–64S. doi: 10.1111/trf.12037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brown JB, Cohen MJ, Minei JP, Maier RV, West MA, Billiar TR, Peitzman AB, Moore EE, Cuschieri J, Sperry JL Inflammation and the Host Response to Injury Investigators. Pretrauma center red blood cell transfusion is associated with reduced mortality and coagulopathy in severely injured patients with blunt trauma. Ann Surg. 2015 May;261(5):997–1005. doi: 10.1097/SLA.0000000000000674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brown JB, Sperry JL, Fombona A, Billiar TR, Peitzman AB, Guyette FX. Pre-trauma center red blood cell transfusion is associated with improved early outcomes in air medical trauma patients. J Am Coll Surg. 2015 May;220(5):797–808. doi: 10.1016/j.jamcollsurg.2015.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ridgeway Greg, et al. Toolkit for Weighting and Analysis of Nonequivalent Groups: A tutorial for the twang package. R vignette. RAND. 2016 [Google Scholar]
- 31.McCaffery DF, Ridgeway G, Morral AR. Propensity Score Estimation With Boosted Regression for Evaluating Causal Effects in Observational Studies. Psychological Methods. 2004;9(4):403–425. doi: 10.1037/1082-989X.9.4.403. [DOI] [PubMed] [Google Scholar]
- 32.Hardin, James W. Generalized estimating equations (GEE) John Wiley & Sons, Ltd; 2005. [Google Scholar]
- 33.Galvagno SM, Jr, Haut ER, Zafar SN, Millin MG, Efron DT, Koenig GJ, Jr, Baker SP, Bowman SM, Pronovost PJ, Haider AH. Association between helicopter vs ground emergency medical services and survival for adults with major trauma. JAMA. 2012;307:1602–10. doi: 10.1001/jama.2012.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brown JB, Gestring ML, Guyette FX, Rosengart MR, Stassen NA, Forsythe RM, Billiar TR, Peitzman AB, Sperry JL. Helicopter transport improves survival following injury in the absence of a time-saving advantage. Surgery. 2016 Mar;159(3):947–59. doi: 10.1016/j.surg.2015.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bulger EM, Guffey D, Guyette FX, MacDonald RD, Brasel K, Kerby JD, Minei JP, Warden C, Rizoli S, Morrison LJ, Nichol G Resuscitation Outcomes Consortium Investigators. Impact of prehospital mode of transport after severe injury: a multicenter evaluation from the Resuscitation Outcomes Consortium. J Trauma Acute Care Surg. 2012 Mar;72(3):567–73. doi: 10.1097/TA.0b013e31824baddf. discussion 573-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Johansson PI, Stensballe J, Oliveri R, Wade CE, Ostrowski SR, Holcomb JB. How I treat patients with massive hemorrhage. Blood. 2014;124(20):3052–8. doi: 10.1182/blood-2014-05-575340. [DOI] [PubMed] [Google Scholar]
- 37.Shafi S, Collinsworth AW, Richter KM, Alam HB, Becker LB, Bullock MR, et al. Bundles of care for resuscitation from hemorrhagic shock and severe brain injury in trauma patients - Translating knowledge into practice. J Trauma Acute Care Surg. 2016 doi: 10.1097/TA.0000000000001161. [DOI] [PubMed] [Google Scholar]
- 38.Camazine MN, Hemmila MR, Leonard JC, Jacobs RA, Horst JA, Kozar RA, Bochicchio GV, Nathens AB, Cryer HM, Spinella PC. Massive transfusion policies at trauma centers participating in the American College of Surgeons Trauma Quality Improvement Program. J Trauma Acute Care Surg. 2015 Jun;78(6 Suppl 1):S48–53. doi: 10.1097/TA.0000000000000641. [DOI] [PubMed] [Google Scholar]
- 39.Chay J, Koh M, Tan HH, Ng J, Ng HJ, Chia N, Kuperan P, Tan J, Lew E, Tan LK, Koh PL, Desouza KA, Bin Mohd Fathil S, Kyaw PM, Ang AL. A national common massive transfusion protocol (MTP) is a feasible and advantageous option for centralized blood services and hospitals. Vox Sang. 2016 Jan;110(1):36–50. doi: 10.1111/vox.12311. [DOI] [PubMed] [Google Scholar]
- 40.Treml AB, Gorlin JB, Dutton RP, Scavone BM. Massive Transfusion Protocols: A Survey of Academic Medical Centers in the United States. Anesth Analg. 2016 Oct;:3. doi: 10.1213/ANE.0000000000001610. [DOI] [PubMed] [Google Scholar]
- 41.Haider AH, Piper LC, Zogg CK, Schneider EB, Orman JA, Butler FK, Gerhardt RT, Haut ER, Mather JP, MacKenzie EJ, Schwartz DA, Geyer DW, DuBose JJ, Rasmussen TE, Blackbourne LH. Military-to-civilian translation of battlefield innovations in operative trauma care. Surgery. 2015 Dec;158(6):1686–95. doi: 10.1016/j.surg.2015.06.026. [DOI] [PubMed] [Google Scholar]
- 42.National Institute for Health and Care Excellence. Major trauma: assessment and initial management. https://www.nice.org.uk/guidance/ng39/resources/major-trauma-assessment-and-initial-management-1837400761285. [PubMed]
- 43.Glen J, Constanti M, Brohi K Guideline Development Group. Assessment and initial management of major trauma: summary of NICE guidance. BMJ. 2016 Jun 22;353:i3051. doi: 10.1136/bmj.i3051. [DOI] [PubMed] [Google Scholar]
- 44.Gerhardt RT, Strandenes G, Cap AP, Rentas FJ, Glassberg E, Mott J, Dubick MA, Spinella PC. Remote damage control resuscitation and the Solstrand Conference: defining the need, the language, and a way forward. Transfusion. 2013;53(Suppl 1):9S–16S. doi: 10.1111/trf.12030. [DOI] [PubMed] [Google Scholar]
- 45.Holcomb JB, Pati S. Optimal trauma resuscitation with plasma as the primary resuscitative fluid: the surgeon's perspective. Hematology Am Soc Hematol Educ Program. 2013;2013:656–9. doi: 10.1182/asheducation-2013.1.656. [DOI] [PubMed] [Google Scholar]
- 46.Moore EE, Chin TL, Chapman MC, Gonzalez E, Moore HB, Silliman CC, Hansen KC, Sauaia A, Banerjee A. Plasma first in the field for postinjury hemorrhagic shock. Shock. 2014;41(Suppl 1):35–8. doi: 10.1097/SHK.0000000000000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cap AP, Pidcoke HF, DePasquale M, Rappold JF, Glassberg E, Eliassen HS, Bjerkvig CK, Fosse TK, Kane S, Thompson P, Sikorski R, Miles E, Fisher A, Ward KR, Spinella PC, Strandenes G. Blood far forward: Time to get moving! J Trauma Acute Care Surg. 2015 Jun;78(6 Suppl 1):S2–6. doi: 10.1097/TA.0000000000000626. [DOI] [PubMed] [Google Scholar]
- 48.Butler FK, Holcomb JB, Schreiber MA, Kotwal RS, Jenkins DA, Champion HR, Bowling F, Cap AP, Dubose JJ, Dorlac WC, Dorlac GR, McSwain NE, Timby JW, Blackbourne LH, Stockinger ZT, Standenes G, Weiskopf RB, Gross KR, Bailey JA. Fluid Resuscitation for Hemorrhagic Shock in Tactical Combat Casualty Care: TCCC Guidelines Change 14-01 - 2 June 2014. J Spec Oper Med. 2014 Fall;14(3):13–38. doi: 10.55460/DPOC-JWIY. [DOI] [PubMed] [Google Scholar]
- 49.Jenkins DH, Rappold JF, Badloe JF, Berséus O, Blackbourne L, Brohi KH, Butler FK, Cap AP, Cohen MJ, Davenport R, DePasquale M, Doughty H, Glassberg E, Hervig T, Hooper TJ, Kozar R, Maegele M, Moore EE, Murdock A, Ness PM, Pati S, Rasmussen T, Sailliol A, Schreiber MA, Sunde GA, van de Watering LM, Ward KR, Weiskopf RB, White NJ, Strandenes G, Spinella PC. Trauma hemostasis and oxygenation research position paper on remote damage control resuscitation: definitions, current practice, and knowledge gaps. Shock. 2014 May;41(Suppl 1):3–12. doi: 10.1097/SHK.0000000000000140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hervig T, Doughty H, Ness P, Badloe JF, Berseus O, Glassberg E, Heier HE. Prehospital use of plasma: the blood bankers' perspective. Shock. 2014 May;41(Suppl 1):39–43. doi: 10.1097/SHK.0000000000000144. [DOI] [PubMed] [Google Scholar]
- 51.Dubick MA. Current concepts in fluid resuscitation for prehospital care of combat casualties. US Army Med Dep J. 2011 Apr-Jun;:18–24. [PubMed] [Google Scholar]
- 52.Maegele M. Coagulation factor concentrate-based therapy for remote damage control resuscitation (RDCR): a reasonable alternative? Transfusion. 2016 Apr;56(Suppl 2):S157–65. doi: 10.1111/trf.13526. [DOI] [PubMed] [Google Scholar]
- 53.Sunde GA, Vikenes B, Strandenes G, Flo KC, Hervig TA, Kristoffersen EK, Heltne JK. Freeze dried plasma and fresh red blood cells for civilian prehospital hemorrhagic shock resuscitation. J Trauma Acute Care Surg. 2015 Jun;78(6 Suppl 1):S26–30. doi: 10.1097/TA.0000000000000633. [DOI] [PubMed] [Google Scholar]
- 54.Glassberg E, Nadler R, Gendler S, Abramovich A, Spinella PC, Gerhardt RT, Holcomb JB, Kreiss Y. Freeze-dried plasma at the point of injury: from concept to doctrine. Shock. 2013;40:444–50. doi: 10.1097/SHK.0000000000000047. [DOI] [PubMed] [Google Scholar]
- 55.Schöchl H, Schlimp CJ, Maegele M. Tranexamic acid, fibrinogen concentrate, and prothrombin complex concentrate: data to support prehospital use? Shock. 2014 May;41(Suppl 1):44–6. doi: 10.1097/SHK.0000000000000093. [DOI] [PubMed] [Google Scholar]
- 56.Curry N, Rourke C, Davenport R, Beer S, Pankhurst L, Deary A, Thomas H, Llewelyn C, Green L, Doughty H, Nordmann G, Brohi K, Stanworth S. Early cryoprecipitate for major haemorrhage in trauma: a randomised controlled feasibility trial. Br J Anaesth. 2015 Jul;115(1):76–83. doi: 10.1093/bja/aev134. [DOI] [PubMed] [Google Scholar]
- 57.Pidcoke HF, Spinella PC. RDCR Symposium fifth-year anniversary edition: global prehospital care rooted in a history of military innovation. Transfusion. 2016 Apr;56(Suppl 2):S107–9. doi: 10.1111/trf.13606. [DOI] [PubMed] [Google Scholar]
- 58.Powell-Dunford N, Quesada JF, Malsby RF, Chou V, Gerhardt RT, Gross KR, Shackelford SA. Risk management analysis of air ambulance blood product administration in combat operations. Aviat Space Environ Med. 2014 Nov;85(11):1130–5. doi: 10.3357/ASEM.3851.2014. [DOI] [PubMed] [Google Scholar]
- 59.Smith IM, James RH, Dretzke J, Midwinter MJ. Prehospital Blood Product Resuscitation for Trauma: A Systematic Review. Shock. 2016 Jul;46(1):3–16. doi: 10.1097/SHK.0000000000000569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Prehospital Air Medical Plasma Trial (PAMPer) [Accessed November 22, 2016]; Available at: clinicaltrials.gov/show/ NCT01818427.
- 61.Control of Major Bleeding after Trauma Study (COMBAT) [Accessed November 22, 2016]; Available at: clinicaltrials.gov/show/ NCT01838863.