To the Editor
Several complications can occur after LASIK due to the creation of a non-physiological potential space, including epithelial ingrowth, diffuse lamellar keratitis, and infectious keratitis. Although some of these complications can be mild and not visually significant, others can be vision-threatening and require medical or surgical intervention. Treatment of complications after LASIK depends on the etiology and severity but, in general, flap amputation is considered a last option when alternative treatment options fail.1 There are few reports in the literature that examine the long-term outcomes of this treatment modality. We present all cases of flap amputation after LASIK at our institution during the past 15 years to evaluate long-term visual and structural outcomes of this procedure.
Eight eyes of 7 patients with a history of LASIK, performed at outside institutions, were identified. Flap amputation was performed at Bascom Palmer Eye Institute by three surgeons (AG, CLK, and SHY) to treat epithelial ingrowth after LASIK in 2 patients and infectious keratitis after LASIK in 5 patients. Two eyes of 2 patients with a history of bilateral LASIK underwent unilateral flap amputation due to recurrent and uncontrollable epithelial ingrowth (Figure A, available in the online version of this article). Mean uncorrected visual acuity (UCVA) was 20/80 preoperatively and improved to 20/302 years after amputation.
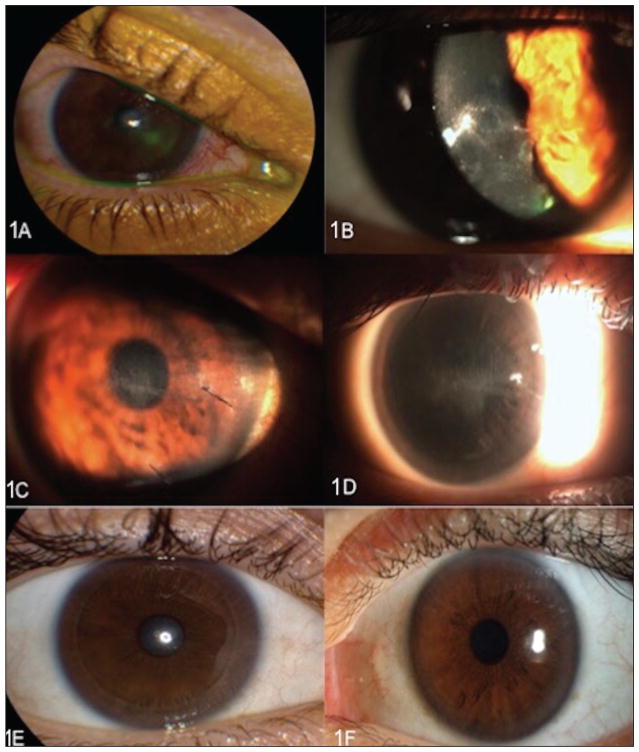
Figure A.
Slit-lamp findings of the patient with epithelial ingrowth. (A) At presentation, fluorescein stain at the 4-o’clock position suggests mild flap lift along with obvious epithelial defect over flap. (B) A few days later, white infiltrate in the interface is consistent with epithelial ingrowth and overlying flap melt. (C) The flap was lifted, epithelial cells scraped, and two 10-0 nylon sutures placed; corneal haze was noted in stroma under flap but no epithelial cells remained in the interface. (D) Two months after flap lift/scrape/suture and 1 month after removal of sutures, the patient presented with flap contracture as evident by macrostriae on examination and haze underneath flap. Cornea (E) 6 months and (F) 3 years after flap amputation.
Additionally, 6 eyes of 5 patients with a history of bilateral LASIK underwent flap amputation (4 unilateral, 1 bilateral) due to infectious keratitis. Five eyes had Mycobacterium infections soon after LASIK (8.4 ± 3 weeks), whereas 1 eye had an Acanthamoeba infection 10 years after LASIK. The patient with Acanthamoeba keratitis had a UCVA of 20/200 and persistent infection despite medical management. Thus, LASIK flap amputation was performed 3.5 weeks after diagnosis, and UCVA was 20/40 6 months after the procedure (Figure B, available in the online version of this article). The 5 eyes with Mycobacterium infection (including Mycobacterium chelonae, M. mucogenicum, M. atypical, and M. abscessus) also had persistent infection despite medical management. Mean preoperative UCVA was 20/200 and UCVA improved to 20/50 at 6 years after flap amputation. In all patients, corneal topography remained stable through follow-up with no signs of ectasia.
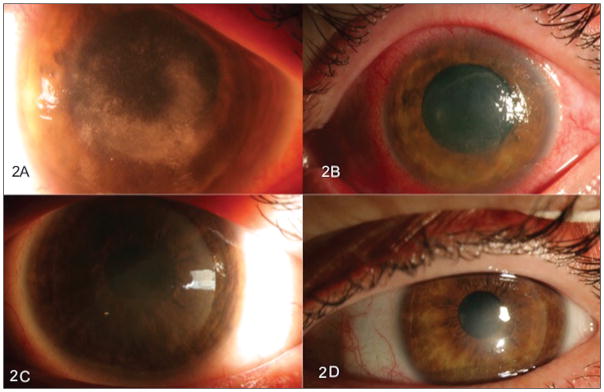
Figure B.
Clinical slit-lamp photographs of the patient with Acanthamoeba infection. (A) Prior to flap amputation, corneal haziness and scarring are visible interfering with the visual axis. Corneal irregularity can be observed (B) 3 days and (C) 3 months after flap amputation. (D) The cornea has become more regular with less haze 5 months after flap amputation.
Our study demonstrates that flap removal after LASIK-induced complications is a viable option in patients unresponsive to medical treatment. Similar to our results after epithelial ingrowth, Kymionis et al. reported good visual outcomes with corrected visual acuity of 20/32 at 6 months after amputation.2 After infectious keratitis due to Mycobacterium infection, Giaconi et al. also reported good visual outcomes with corrected visual acuity of 20/30.3 On the contrary, flap amputation related to other etiologies such as central flap necrosis syndrome and trauma have been reported to result in less optimal visual outcomes (from 20/90 to 20/40 at 4 months after flap amputation).4,5
This study demonstrates that flap amputation after epithelial ingrowth and infectious keratitis can lead to good long-term visual (corrected visual acuity of 20/30 or better) and structural (no ectasia) outcomes.
Acknowledgments
Supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Clinical Sciences Research and Development’s Career Development Award CDA-2-024-10S (Dr. Galor), NIH Center Core Grant P30EY014801, Research to Prevent Blindness Unrestricted Grant, The Ronald and Alicia Lepke Grant, The Lee and Claire Hager Grant, The Jimmy and Gaye Bryan Grant, The Gordon Charitable Trust, The Robert Baer Family Grant, and the Richard Azar Family Grant (institutional grants).
Dr. Yoo is a consultant for Alcon, Allergan, Bausch & Lomb, Carl Zeiss Meditec, Abbott Medical Optics, and Transcend Medical. The remaining authors have no financial or proprietary interest in the materials presented herein.
References
- 1.McLeod SD, Holsclaw D, Lee S. Refractive, topographic, and visual effects of flap amputation following laser in situ keratomileusis. Arch Ophthalmol. 2002;120:1213–1217. [PubMed] [Google Scholar]
- 2.Kymionis G, Ide T, Yoo S. Flap amputation with phototherapeutic keratectomy (PTK) and adjuvant mitomycin C for severe post-LASIK epithelial ingrowth. Eur J Ophthalmol. 2009;19:301–303. doi: 10.1177/112067210901900223. [DOI] [PubMed] [Google Scholar]
- 3.Giaconi J, Pham R, Ta CN. Bilateral Mycobacterium abscessus keratitis after laser in situ keratomileusis. J Cataract Refract Surg. 2002;28:887–890. doi: 10.1016/s0886-3350(01)01096-3. [DOI] [PubMed] [Google Scholar]
- 4.Garcia-Gonzalez M, Gil-Cazorla R, Teus MA. Surgical flap amputation for central flap necrosis after laser in situ keratomileusis. J Cataract Refract Surg. 2009;35:2018–2021. doi: 10.1016/j.jcrs.2009.05.045. [DOI] [PubMed] [Google Scholar]
- 5.Tetz M, Werner L, Muller M, et al. Late traumatic LASIK flap loss during contact sport. J Cataract Refract Surg. 2007;33:1332–1335. doi: 10.1016/j.jcrs.2007.03.033. [DOI] [PubMed] [Google Scholar]