Abstract
Background
People with low back pain (LBP) alter their motion patterns during level walking and stair climbing due to pain or fear. However, the alternations of load sharing during the two activities are largely unknown. The objective of this study was to investigate the effect of LBP caused by lumbar disc herniation (LDH) on the muscle activities of 17 main trunk muscle groups and the intradiscal forces acting on the five lumbar discs.
Material/Methods
Twenty-six healthy adults and seven LDH patients were recruited to perform level walking and stair climbing in the Gait Analysis Laboratory. Eight optical markers were placed on the bony landmarks of the spinous process and pelvis, and the coordinates of these markers were captured during the two activities using motion capture system. The coordinates of the captured markers were applied to developed musculoskeletal model to calculate the kinetic variables.
Results
LDH patients demonstrated higher muscle activities in most trunk muscle groups during both level walking and stair climbing. There were decreases in anteroposterior shear forces on the discs in the pathological region and increases in the compressive forces on all the lumbar discs during level walking. The symmetry of mediolateral shear forces was worse in LDH patients than healthy adults during stair climbing.
Conclusions
LDH patients exhibited different kinetic alternations during level walking and stair climbing. However, both adaptive strategies added extra burdens to the trunk system and further increased the risk for development of LDH.
MeSH Keywords: Activities of Daily Living, Intervertebral Disc Degeneration, Musculoskeletal Abnormalities
Background
Low back pain (LBP) is one of the most prevalent diseases afflicting people today. The lifetime prevalence of LBP is high and more than 70% of adults have suffered LBP at some time in their lives [1–3]. An abnormal motion pattern has been observed in people with LBP [4]. Moreover, the disabilities related to LBP are frequently associated with changes in the biomechanics of the lumbar spine.
Level walking and stair climbing are two common and inevitable activities of daily living (ADL). Most previous studies have mainly focused on the kinematic alternation in LBP patients during these two ADLs. It has been shown that LBP patients reduce trunk rotation [5,6] and diminish the change in pelvis-thorax coordination from more in-phase to more anti-phase [7] in the transverse plane, and spend more of the gait cycle in-phase coordination in the frontal plane [8] during level walking. Also, the range of motion (ROM) in the lumbar region has been found to have a reduction in LBP patients during stair climbing [9].
The kinematic alternation is usually accompanied by the kinetic adaptation during level walking and stair climbing. However, most kinetic studies investigating the kinetic alternation due to LBP have mainly focused on lifting activities [10–15]. Moreover, the spinal loads have mainly been simulated on only one lumbar segment unit such as L5S1. It has been shown that LBP patients display greater shear force and compressive force on L5S1 during lifting. Two previous kinetic studies have investigated the abnormal spinal loads during level walking [16,17]. However, the study patients were limited to the amputees. Other studies have reported on the abnormal muscle activities in LBP patients during level walking [18–21], but the analysis of muscle activity was mainly based on electromyography (EMG) measurements. The EMG recording from a muscle only indicates the electrical activity of the muscle but cannot provide information on the muscle force. In addition, many of the spinal muscles, such as deep muscles, are difficult to reach in vivo by EMG measurement. As for stair climbing, none of the previous studies in the literature have investigated abnormal trunk muscle activities in LBP patients during ADL. Many factors could induce LBP, such as lumbar disc herniation and spondylolisthesis. Different subgroups of LBP patients have reported adopting different adaptive strategies for LBP [22–24].
Thus, the purpose of this study was to investigate the impact of LBP induced by lumbar disc herniation (LDH) on the compressive forces, anteroposterior shear forces, and mediolateral shear forces acting on every lumbar disc and the maximum muscle activities of seventeen main trunk muscle groups during level walking and stair climbing.
Material and Methods
Study setting and design
This study was conducted at the Gait Analysis Laboratory in Shenzhen Second People’s Hospital from April 2016 to October 2016. The participants in this study included healthy adults and patients who were diagnosed with lumbar disc herniation. The healthy adults were recruited if they met the following criteria: a) no obvious motor dysfunction, b) no surgery in the recent one year, c) no back pain or lumbar disc herniation, d) no strenuous exercise 24 hour before trials. The selected patients had to meet the following criteria: a) the patients were diagnosed with lumbar disc herniation in the course of discopathy in lumbar spine. The diagnosis was made by at least two specialist orthopedic surgeons and confirmed by x-ray imaging and MRI. b) The disc herniation was diagnosed to occur at the lower lumbar level by MRI. c) The patients had the ability to conduct level walking and stair climbing. In the examination, the patients were required to attempt to walk and climb stairs. They were deemed to maintain the movement ability if they could perform at least 20 gait cycles. This study was approved by Shenzhen Second People’s Hospital and written informed consent was obtained for every participant.
Protocol and testing procedure
Prior to the experiment, the participant lay prone on the bed. One surgeon helped to find and locate the major landmarks on spine and pelvis. In this study, the landmarks included the third and seventh spinous process of the thoracic vertebra (T3, T7), the first, third, and fifth spinous process of lumbar vertebra (L1, L3, L5), the left posterior superior iliac spine, the right posterior superior iliac spine, and the iliac crest. Then, optical markers were placed on these landmarks and captured by Optotrak Certus motion analysis system (Northern Digital Inc., Ontario, Canada) at the rate of 100 Hz throughout the whole experiment. The detailed placements are illustrated in Figure 1A.
Figure 1.
(A, B) Schematic of marker placement and test procedure.
Before the trial of level walking and stair climbing, the participants were kept standing in a neutral position for at least five seconds for data collection to obtain baseline. Afterwards, the same surgeon demonstrated the requirements for level walking and stair climbing and then guided the participants to practice the two activities until they felt that they could carry out each activity naturally. The schematics of the level walking and stair climbing are showed in Figure 1B. Participants repeated each activity three times for data collection.
Musculoskeletal model and simulation
A generic FacetJointModel model in the Anybody Managed Model repository (AMMR, version 1.6) of Anybody Modeling System (Anybody Modeling System version 6.0.6, Aalborg, Denmark) was selected for its ability to predict the forces in a redundant system. In addition, the model includes more than one hundred muscle fascicles and all lumbar intervertebral joints in the spinal region. The model has been described and validated in the literature [25,26]. In brief, the model contained pelvis, five lumbar vertebrae, one lumped thoracic segment, and one lumped cervical segment. These segments were connected with spherical joints, and the location of each joint was based on the work by Pearcy and Bogduk [27]. In addition, the model featured the 17 main muscle groups in the spinal region: left and right erector spinae (ES), left and right lumbar multifidus (LMF), left and right thoracic multifidus (TMF), left and right semispinalis (SS), left and right oblique externus (OE), left and right internal externus (IE), left and right psoas major (PS), left and right quadratus lumborum (QL), and rectus abdominis (RA). Each muscle group consists of many muscle fascicle. The muscle fascicle force was solved as force component by minimum-maximum optimization algorithm and could only exert tensile force [25,26,28]. In the AnyBody Model System, muscle activity of every muscle fascicle was represented by the ratio of muscle fascicle force to its strength.
In the AnyBody Model System, the default spine rhythm was applied to drive the lumbar segmental motion. So only the determination of thoracic motion was essential. However, the default spine rhythm could not express the difference of intervertebral motion in healthy individuals and LDH patients. Therefore, the model was developed and driven by the captured markers’ coordinates. Since the determination of each segmental motion needed at least three points, the movements of the L2, L3, and L4 were determined by intervertebral joint, real marker and virtual marker. The virtual marker was determined by attributing different weights to the real markers (Table 1). The L1 and L5 were driven using the default coefficient of spine rhythm with respect to the adjacent lumbar vertebra.
Table 1.
The weight of markers in trunk section for lumbar vertebrae and thoracic segment.
| Marker T3 | Marker T7 | Marker L1 | Marker L3 | Marker L5 | |
|---|---|---|---|---|---|
| Thx | 1/2 | 1/2 | 0 | 0 | 0 |
| L2 | 0 | 0 | 1/2 | 1/2 | 0 |
| L3 | 0 | 0 | 1/6 | 2/3 | 1/6 |
| L4 | 0 | 0 | 0 | 1/2 | 1/2 |
Thx – the whole thoracic segment; L1 – the first lumbar vertebra; L2 – the second lumbar vertebra; L3 – the third lumbar vertebra; L4 – the fourth lumbar vertebra; L5 – the fifth lumbar vertebra; T3 – the third thoracic vertebra; T7 – the seven thoracic vertebra.
Data analysis
The output variables of the musculoskeletal simulation included the maximum muscle activity (MMA) of every main muscle groups and the compressive force, anteroposterior shear force, and mediolateral shear force of every lumbar intervertebral disc. The gait cycle was defined as the time interval between subsequent heel strikes of the same leg for both level walking and stair climbing. The data of every variable were time normalized and re-sampled using a cubic spline interpolation to 0–100% of the gait cycle. In this study, the variable of every participant was the average of three trials. All data analysis, except simulation, was completed using custom procedure implemented in MATLAB software (The MathWorks, Natick, MA, USA).
Results
Demographic data
We recruited 26 healthy male adults (mean age 23.6 (SD 1.92) years; height 169.9 (SD 5.9) cm; weight 63.5 (SD 8.4) kg) and seven male LDH patients (mean age 28.7 (SD 4.5) years; height 170.1 (SD 3.4) cm; weight 67.4 (SD 5.3) kg). The disc herniation was found to happen at the L4L5 level in 3 out of 7 cases, at the L5S1 level in 3 out of 7 cases and at both L4L5 and L5S1 level in 1 out of 7 cases.
Maximum muscle activities of the seventeen main trunk muscle groups
Figures 2 and 3 shows the maximum muscle activities (MMAs) of 17 main trunk muscle groups during level walking and stair climbing, respectively. Compared with healthy people, the MMAs of all eight main back muscle groups and eight of nine main front muscle groups were significantly larger in LDH patients during level walking (Figure 2, Table 2). During stair climbing, the MMAs of left and right ES, left and right LMF, right TMF, right SS, left and right EO, left and right IO, and left PM varied with time points (Figure 3). The other muscle groups showed greater MMAs in LDH patients than healthy participants throughout the gait cycle (Figure 3). In addition, all the 17 muscle groups’ mean MMAs were larger in LDH patients than healthy participants (Table 2). Moreover, the differences were significant (p<0.05) in 12 of 17 muscle groups (Table 2).
Figure 2.
The comparison of the maximum muscle activity of 17 main muscle groups in the spine between healthy participants and patients with lumbar disc herniation, during level walking. The red and blue solid line represents maximum muscle activity of healthy participants. The red and blue dash-dotted line represents maximum muscle activity of patients with lumbar disc herniation.
Figure 3.
The comparison of the maximum muscle activity of 17 main muscle groups in the spine between healthy participants and patients with lumbar disc herniation, during stair climbing. The red and blue solid line represents maximum muscle activity of healthy participants. The red and blue dash-dotted line represents maximum muscle activity of patients with lumbar disc herniation.
Table 2.
The mean of maximum muscle activities of each muscle group, the compressive force, the anteroposterior shear force and the mediolateral shear force of each lumbar intervertebral disc during level walking and stair climbing.
| Level walking | P value | Stair climbing | P value | |||
|---|---|---|---|---|---|---|
| Control (%) | Patient (%) | Control (%) | Patient (%) | |||
| Back muscle groups | ||||||
| Left ES | 21.49 | 28.14 | 0.00 | 21.46 | 30.18 | 0.01 |
| Right ES | 22.28 | 27.70 | 0.01 | 21.53 | 29.33 | 0.02 |
| Left LMF | 15.63 | 21.36 | 0.00 | 15.12 | 18.56 | 0.04 |
| Right LMF | 15.21 | 18.63 | 0.03 | 15.52 | 17.38 | 0.24 |
| Left SS | 20.94 | 27.89 | 0.00 | 21.37 | 25.30 | 0.03 |
| Right SS | 21.26 | 25.12 | 0.05 | 21.13 | 25.13 | 0.04 |
| Left TMF | 16.79 | 22.79 | 0.00 | 16.76 | 24.92 | 0.00 |
| Right TMF | 16.65 | 19.98 | 0.04 | 16.58 | 21.16 | 0.03 |
| Front muscle groups | ||||||
| Left IO | 15.22 | 16.08 | 0.53 | 16.24 | 17.77 | 0.43 |
| Right IO | 15.02 | 19.76 | 0.01 | 16.06 | 21.25 | 0.04 |
| Left EO | 14.45 | 19.00 | 0.02 | 14.37 | 20.80 | 0.01 |
| Right EO | 13.62 | 16.33 | 0.04 | 15.19 | 19.14 | 0.03 |
| Left PM | 25.50 | 30.88 | 0.04 | 26.36 | 31.24 | 0.12 |
| Right PM | 25.35 | 35.85 | 0.00 | 24.86 | 33.99 | 0.00 |
| Left QL | 13.75 | 18.42 | 0.02 | 15.66 | 17.60 | 0.40 |
| Right QL | 13.53 | 19.20 | 0.00 | 13.30 | 18.91 | 0.00 |
| RA | 17.23 | 24.17 | 0.02 | 18.59 | 21.57 | 0.30 |
| Compressive force | ||||||
| Sacrum L5 CF | 93.43 | 112.81 | 0.01 | 98.10 | 103.58 | 0.54 |
| L4L5 CF | 94.64 | 114.18 | 0.02 | 98.81 | 105.66 | 0.45 |
| L3L4 CF | 100.40 | 118.03 | 0.02 | 104.36 | 108.43 | 0.64 |
| L2L3 CF | 72.48 | 87.32 | 0.03 | 79.60 | 80.32 | 0.93 |
| L1L2 CF | 73.08 | 87.27 | 0.04 | 81.46 | 81.20 | 0.97 |
| Anteroposterior shear force | ||||||
| Sacrum L5 AF | 11.74 | 8.41 | 0.21 | 12.01 | 11.02 | 0.73 |
| L4L5 AF | 11.26 | 3.25 | 0.03 | 16.54 | 7.98 | 0.10 |
| L3L4 AF | −4.33 | −23.69 | 0.01 | −4.15 | −18.08 | 0.05 |
| L2L3 AF | −18.91 | −26.19 | 0.02 | −20.96 | −23.31 | 0.55 |
| L1L2 AF | −24.29 | −32.27 | 0.03 | −29.01 | −30.43 | 0.76 |
| Mediolateral shear force | ||||||
| Sacrum L5 MF | 1.07 | −1.42 | 0.11 | 2.14 | −4.53 | 0.01 |
| L4L5 MF | 1.13 | −1.64 | 0.09 | 2.15 | −4.91 | 0.01 |
| L3L4 MF | 1.10 | −0.95 | 0.22 | 2.20 | −4.88 | 0.01 |
| L2L3 MF | 0.68 | 0.58 | 0.93 | 0.85 | −3.28 | 0.02 |
| L1L2 MF | 0.65 | 1.05 | 0.76 | 0.62 | −3.28 | 0.03 |
ES – erector spinae; LMF – lumbar multifidus; TMF – thoracic multifidus; SS – semispinalis; OE – oblique externus; IE – internal externus; PS – psoas major; QL – quadratus lumborum; RA – rectus abdominis; CF – compressive force; AF – anteroposterior shear force; MF – mediolateral shear force.
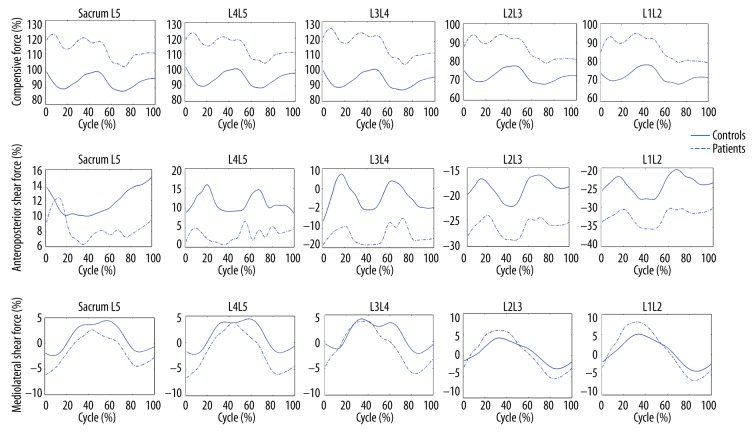
Intradiscal forces
During level walking, LDH patients exhibited smaller anteroposterior shear forces acting on the two discs in the pathological region and larger anteroposterior shear forces acting on the other three discs in terms of the magnitude (Figure 4, Table 2). The compressive forces acting on all the five lumbar discs were significantly larger in LDH patient than healthy participants (Figure 4, Table 2). During stair climbing, there was no significant difference in the compressive forces and anteroposterior shear forces between LDH patients and healthy participants (Figure 5, Table 2). However, the symmetry center of the mediolateral shear forces acting on the five discs all significantly offset laterally (Figure 5, Table 2).
Figure 4.
The comparison of the intradiscal force acting on five lumbar discs between healthy participants and patients with lumbar disc herniation, during level walking. The blue solid line represents intradiscal forces of healthy participants. The blue dash-dotted line represents intradiscal forces of patients with lumbar disc herniation.
Figure 5.
The comparison of the intradiscal force acting on five lumbar discs between healthy participants and patients with lumbar disc herniation, during stair climbing. The blue solid line represents intradiscal forces of healthy participants. The blue dash-dotted line represents intradiscal forces of patients with lumbar disc herniation.
Discussion
This study aimed to investigate the kinetic compensatory response to lumbar disc herniation during level walking and stair climbing. The kinetics involved the maximum muscle activities of 17 main muscle groups in the spinal region and the compressive forces, anteroposterior shear forces, and mediolateral shear forces acting on every lumbar disc. We explored three hypotheses, a) LDH patients would decrease anteroposterior shear forces and increase compressive forces in the pathological region during level walking; b) adaptive alteration of spinal loads for LDH mainly focused on mediolateral forces during stair climbing; c) there were more trunk muscle activities in LDH patients during the two ADLs. The finding in this study indicated that LDH patients reduced anteroposterior shear forces and increased compressive forces acting on the discs in the pathological region during level walking, supporting the first hypothesis. In addition, the patients increased anteroposterior shear forces and compressive forces on the upper lumbar discs. The MMAs of the majority of the 17 muscle groups were found increased in LDH patients during level walking, supporting the third hypothesis. Similar to level walking, the LDH patients also increased MMAs of most muscle groups but worsened the symmetry of all the five lumbar discs’ mediolateral shear forces during stair climbing, which was in agreement with the second and third hypotheses. No significant differences in compressive forces and anteroposterior shear forces were found between LDH patients and healthy participants, favoring the second hypothesis.
During level walking, the attempt to reduce shear forces in the pathological region was an adaption of the guarding mechanism. The annulus fibrosus tissue of the intervertebral disc has an interlamellar structure, which has been deemed especially sensitive to shear force [29]. Moreover, the intervertebral disc’s tolerance to shear loading is much lower than to compression [30]. Therefore, to protect the intervertebral discs in the pathological region and avoid provoking painful tissue, patients decreased the anteroposterior shear forces. But the costs of this decrease were the increase in the compressive forces on every lumbar disc and the increase in anteroposterior shear forces on the upper lumbar discs. Greater spinal load and repetitive lumbar flexion-extension increases the risk of LDH development [31,32], thus it would be better for LDH patients to conduct some interventions to decrease the spinal load before symptomatic development. As part of the trunk system, the musculature plays a critical role in stabilizing the spinal motion. In the Panjabi’s stabilizing theory [33], the neural control unit subsystem would coordinate the spinal column subsystem and spinal muscle subsystem to sustain the dynamic spinal stability. Therefore, the adaptive alteration in intradiscal forces is needed for the adaptive response in muscle activities. In this study, LDH patients displayed greater muscle forces in all the back muscle groups and the majority of the front muscle groups, findings which were in agreement with the tendencies in the EMG analysis [19,34]. Also, the adaptive response in muscle activities in this study was consistent with Van’s guarding hypothesis that deemed elevated lumbar muscle activities as a guarded response in LBP patients during level walking [19].
During stair climbing, the ROM of the lumbar spine in the frontal plane has been shown to have no significant difference from that during level walking [35,36]. But stair climbing requires more pelvic oblique at the initial and final part of the gait cycle [37]. In LDH patients, the greater oblique might increase the risk of provocation of painful tissue and further lead to excessive pelvic oblique and lumbar lateral bending throughout the gait cycle. This kinematic alternation would induce the offset in mediolateral shear force, which would be consistent with the current finding that the mediolateral shear forces acting on the five lumbar discs all offset away from zero in LDH patients. Similarly, to stabilize the spinal system, the majority of the muscle groups demonstrated more muscle activities in LDH patients during stair climbing. One noteworthy point was that larger pelvic oblique at the initial and final part of the gait cycle was in accordance with larger muscle activities at these part of the gait cycle, indicating that the alternations of muscle activities were mainly adaptive for abnormal spinal movement in the frontal plane.
Conclusions
The kinetic compensatory responses to lumbar disc herniation were different in level walking and stair climbing. However, both adaptions had negative impacts on the comprehensive spinal loadings and added to the burden on musculature. The adaptations found in this study might be a suboptimal load sharing for LDH patients. However, given the repetitive and inevitable nature of level walking and stair climbing, perpetually elevated loading likely increased the risk of the worsening of lumbar disc herniation. So, it is better for these patients to undergo some interventions before severe disability occurs. In the future, we will investigate the improvement of load sharing after different interventions for lumbar disc herniation.
Acknowledgements
The authors thank Shenzhen Second People’s Hospital and Research Institute of Tsinghua University in China. They provided the equipment and helped to collect the experimental data. The authors also thank all the participants.
Footnotes
Conflict of interest
No other relationships/conditions/circumstances present potential conflict of interest.
Source of support: This study was funded by the Economy, Trade and Information Commission of Shenzhen Municipality (Grant No. SMJKPT20140417010001), the Innovation Commission of Science and Technology of Shenzhen Municipality (Grant No. JCYJ20151030160526024, Grant No. CXZZ20130321163655) and Guangdong provincial department of science and technology (Grant No. 2014A020212655)
References
- 1.Dunn KM, Hestbaek L, Cassidy JD. Low back pain across the life course. Best Pract Res Clin Rheumatol. 2013;27(5):591–600. doi: 10.1016/j.berh.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 2.Deyo RA, Rainville J, Kent DL. What can the history and physical examination tell us about low back pain. JAMA. 1992;268(6):760–65. [PubMed] [Google Scholar]
- 3.Buchbinder R, Blyth FM, March LM, et al. Placing the global burden of low back pain in context. Best Pract Res Clin Rheumatol. 2013;27(5):575–89. doi: 10.1016/j.berh.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 4.Shum GL, Crosbie J, Lee RY. Movement coordination of the lumbar spine and hip during a picking up activity in low back pain subjects. Eur Spine J. 2007;16(6):749–58. doi: 10.1007/s00586-006-0122-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van den Hoorn W, Bruijn SM, Meijer OG, et al. Mechanical coupling between transverse plane pelvis and thorax rotations during gait is higher in people with low back pain. J Biomech. 2012;45(2):342–47. doi: 10.1016/j.jbiomech.2011.10.024. [DOI] [PubMed] [Google Scholar]
- 6.Muller R, Ertelt T, Blickhan R. Low back pain affects trunk as well as lower limb movements during walking and running. J Biomech. 2015;48(6):1009–14. doi: 10.1016/j.jbiomech.2015.01.042. [DOI] [PubMed] [Google Scholar]
- 7.Lamoth CJ, Meijer OG, Daffertshofer A, et al. Effects of chronic low back pain on trunk coordination and back muscle activity during walking: Changes in motor control. Eur Spine J. 2006;15(1):23–40. doi: 10.1007/s00586-004-0825-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seay JF, Van Emmerik RE, Hamill J. Influence of low back pain status on pelvis-trunk coordination during walking and running. Spine. 2011;36(16):E1070–79. doi: 10.1097/BRS.0b013e3182015f7c. [DOI] [PubMed] [Google Scholar]
- 9.Lee JK, Desmoulin GT, Khan AH, Park EJ. Comparison of 3D spinal motions during stair-climbing between individuals with and without low back pain. Gait Posture. 2011;34(2):222–26. doi: 10.1016/j.gaitpost.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 10.Marras WS, Ferguson SA, Burr D, et al. Functional impairment as a predictor of spine loading. Spine. 2005;30(7):729–37. doi: 10.1097/01.brs.0000157459.36970.62. [DOI] [PubMed] [Google Scholar]
- 11.Han JS, Goel VK, Ahn JY, et al. Loads in the spinal structures during lifting: Development of a three-dimensional comprehensive biomechanical model. Eur Spine J. 1995;4(3):153–68. doi: 10.1007/BF00298240. [DOI] [PubMed] [Google Scholar]
- 12.Marras WS, Davis KG, Ferguson SA, et al. Spine loading characteristics of patients with low back pain compared with asymptomatic individuals. Spine. 2001;26(23):2566–74. doi: 10.1097/00007632-200112010-00009. [DOI] [PubMed] [Google Scholar]
- 13.Shum GL, Crosbie J, Lee RY. Effect of low back pain on the kinematics and joint coordination of the lumbar spine and hip during sit-to-stand and stand-to-sit. Spine. 2005;30(17):1998–2004. doi: 10.1097/01.brs.0000176195.16128.27. [DOI] [PubMed] [Google Scholar]
- 14.Shum GL, Crosbie J, Lee RY. Three-dimensional kinetics of the lumbar spine and hips in low back pain patients during sit-to-stand and stand-to-sit. Spine. 2007;32(7):E211–19. doi: 10.1097/01.brs.0000259204.05598.10. [DOI] [PubMed] [Google Scholar]
- 15.Shum GL, Crosbie J, Lee RY. Back pain is associated with changes in loading pattern throughout forward and backward bending. Spine (Phila Pa 1976) 2010;35(25):E1472–78. doi: 10.1097/BRS.0b013e3181ecd71c. [DOI] [PubMed] [Google Scholar]
- 16.Shojaei I, Hendershot BD, Wolf EJ, Bazrgari B, et al. Persons with unilateral transfemoral amputation experience larger spinal loads during level-ground walking compared to able-bodied individuals. Clin Biomech. 2016;32:157–63. doi: 10.1016/j.clinbiomech.2015.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yoder AJ, Petrella AJ, Silverman AK. Trunk-pelvis motion, joint loads, and muscle forces during walking with a transtibial amputation. Gait Posture. 2015;41(3):757–62. doi: 10.1016/j.gaitpost.2015.01.016. [DOI] [PubMed] [Google Scholar]
- 18.Lamoth CJ, Daffertshofer A, Meijer OG, et al. Effects of experimentally induced pain and fear of pain on trunk coordination and back muscle activity during walking. Clin Biomech. 2004;19(6):551–63. doi: 10.1016/j.clinbiomech.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 19.van der Hulst M, Vollenbroek-Hutten MM, Rietman JS, et al. Back muscle activation patterns in chronic low back pain during walking: A “guarding” hypothesis. Clin J Pain. 2010;26(1):30–37. doi: 10.1097/AJP.0b013e3181b40eca. [DOI] [PubMed] [Google Scholar]
- 20.Ghamkhar L, Kahlaee AH. Trunk muscles activation pattern during walking in subjects with and without chronic low back pain: A systematic review. PM R. 2015;7(5):519–26. doi: 10.1016/j.pmrj.2015.01.013. [DOI] [PubMed] [Google Scholar]
- 21.Anders C, Scholle HC, Wagner H, et al. Trunk muscle co-ordination during gait: Relationship between muscle function and acute low back pain. Pathophysiology. 2005;12(4):243–47. doi: 10.1016/j.pathophys.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 22.Dankaerts W, O’Sullivan P, Burnett A, et al. Discriminating healthy controls and two clinical subgroups of nonspecific chronic low back pain patients using trunk muscle activation and lumbosacral kinematics of postures and movements a statistical classification model. Spine. 2009;34(15):1610–18. doi: 10.1097/BRS.0b013e3181aa6175. [DOI] [PubMed] [Google Scholar]
- 23.Gombatto SP, Collins DR, Sahrmann SA, et al. Patterns of lumbar region movement during trunk lateral bending in 2 subgroups of people with low back pain. Physic Ther. 2007;87(4):441–54. doi: 10.2522/ptj.20050370. [DOI] [PubMed] [Google Scholar]
- 24.Kim MH, Yi CH, Kwon OY, et al. Comparison of lumbopelvic rhythm and flexion-relaxation response between 2 different low back pain subtypes. Spine. 2013;38(15):1260–67. doi: 10.1097/BRS.0b013e318291b502. [DOI] [PubMed] [Google Scholar]
- 25.de Zee M, Hansen L, Wong C, et al. A generic detailed rigid-body lumbar spine model. J Biomech. 2007;40(6):1219–27. doi: 10.1016/j.jbiomech.2006.05.030. [DOI] [PubMed] [Google Scholar]
- 26.Christophy M, Faruk Senan NA, Lotz JC, et al. A musculoskeletal model for the lumbar spine. Biomech Model Mechanobiol. 2012;11(1–2):19–34. doi: 10.1007/s10237-011-0290-6. [DOI] [PubMed] [Google Scholar]
- 27.Pearcy MJ, Bogduk N. Instantaneous axes of rotation of the lumbar intervertebral joints. Spine. 1988;13(9):1033–41. doi: 10.1097/00007632-198809000-00011. [DOI] [PubMed] [Google Scholar]
- 28.Han KS, Zander T, Taylor WR, Rohlmann A, et al. An enhanced and validated generic thoraco-lumbar spine model for prediction of muscle forces. Med Eng Phys. 2012;34(6):709–16. doi: 10.1016/j.medengphy.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 29.Inoue N, Espinoza Orias AA. Biomechanics of intervertebral disk degeneration. Orthop Clin North Am. 2011;42(4):487–99. vii. doi: 10.1016/j.ocl.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ferguson SA, Marras WS, Burr DL, et al. Differences in motor recruitment and resulting kinematics between low back pain patients and asymptomatic participants during lifting exertions. Clin Biomech. 2004;19(10):992–99. doi: 10.1016/j.clinbiomech.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 31.Parkinson RJ, Callaghan JP. The role of dynamic flexion in spine injury is altered by increasing dynamic load magnitude. Clin Biomech (Bristol, Avon) 2009;24(2):148–54. doi: 10.1016/j.clinbiomech.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 32.Noguchi M, Gooyers CE, Karakolis T, et al. Is intervertebral disc pressure linked to herniation?: An in-vitro study using a porcine model. J Biomech. 2016;49(9):1824–30. doi: 10.1016/j.jbiomech.2016.04.018. [DOI] [PubMed] [Google Scholar]
- 33.Panjabi MM. Clinical spinal instability and low back pain. J Electromyogr Kinesiol. 2003;13(4):371–79. doi: 10.1016/s1050-6411(03)00044-0. [DOI] [PubMed] [Google Scholar]
- 34.van der Hulst M, Vollenbroek-Hutten MM, Rietman JS, Hermens HJ. Lumbar and abdominal muscle activity during walking in subjects with chronic low back pain: Support of the “guarding” hypothesis? J Electromyogr Kinesiol. 2010;20(1):31–38. doi: 10.1016/j.jelekin.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 35.Bible JE, Biswas D, Miller CP, et al. Normal functional range of motion of the lumbar spine during 15 activities of daily living. J Spinal Disord Tech. 2010;23:106–12. doi: 10.1097/BSD.0b013e3181981823. [DOI] [PubMed] [Google Scholar]
- 36.Breloff SP, Chou LS. Influence of various daily tasks on segmented trunk kinematics. Biomedical Engineering-Applications Basis Communications. 2015;27(6) [Google Scholar]
- 37.Nadeau S, McFadyen BJ, Malouin F. Frontal and sagittal plane analyses of the stair climbing task in healthy adults aged over 40 years: What are the challenges compared to level walking? Clin Biomech. 2003;18(10):950–59. doi: 10.1016/s0268-0033(03)00179-7. [DOI] [PubMed] [Google Scholar]