Abstract
The neophallus creation is still a mystery and it remains challenging even today. In this article, we performed a comprehensive review of the literature regarding phalloplasty and penile reconstructive surgery between January 2008 and May 2016. In this review, we have included 15 research articles and the results of 276 patients were examined. Studies revealed several indications and when indications were reviewed, 191 patients were female-to-male transgender, 9 patients had disorder of sex development/micropenis, 16 had penile amputation/trauma, 9 had ambiguus genitalia, 40 had exstrophy and/or epispadias, 11 had other problems. As a result of this review, phalloplasty is a reliable and useful operation with good functional and aesthetical results.
Keywords: Gender reassignment surgery, phalloplasty, penile reconstructive surgery, surgical flaps
Introduction
The neophallus creation is still a mystery and it remains challenging even today.[1] Bogoras et al.[2] reported the first penile reconstruction with successful micturation and coitus in 1936 by using a rib cartilage and an abdominal flap. Female to male gender reassignment surgery was firstly performed by Sir Harold Gillies.[3] Despite the technologic developments and the new equipments, phalloplasty operation is still a dream-like operation. There are several indications for phalloplasty operation such as congenital anomalies (ambiguus genitalia, aphallia, epispadias, bladder exstrophy, micropenis, etc.), surgical amputation of penis (penile cancer), traumatic penile amputation, female to male gender reassignment.[1,4] (Figure 1, 2). The bladder exstrophy ranges from 1/10000 to 1/50000 and males with bladder exstrophy may have ambiguus genitalia that requires surgical reconstruction.[4] Gender identity disorder prevelance varies depending on populations and according to DSM-IV it is 1/30000 for men and 1/100000 for women.[5,6] Penile fractures and traumas are one of the other reasons and it is highly underreported an uncommon in America and Europe.[7,8]
Figure 1.

Bladder extrophy (Mr. Ralph’s photo archive)
Figure 2.

Traumatic penile amputation and phalloplasty result (Mr. Ralph’s photo archive)
There are several surgical techniques and different types of flaps used for phalloplasty. Random pattern flaps, pedicled flaps (groin flap, anterolateral thigh flap, island tensor fascia lata flap), free flaps (radial forearm free flap, osteocutaneous radial forearm free flap, lateral arm free flap, osteocutaneous free fibula, anterolateral thigh free flap, latissimus dorsi free flap, free scapular flap) would be used for phalloplasty operations (Figure 3).[9] Neophallus should provide a satisfying and aesthetitc appearance and also neourethra should allow comfortable voiding while standing.[1,9,10] In addition, tactile and erogeneous sensibility, enough bulk for a stiffener insertion are also important features.[1,9,10]
Figure 3.
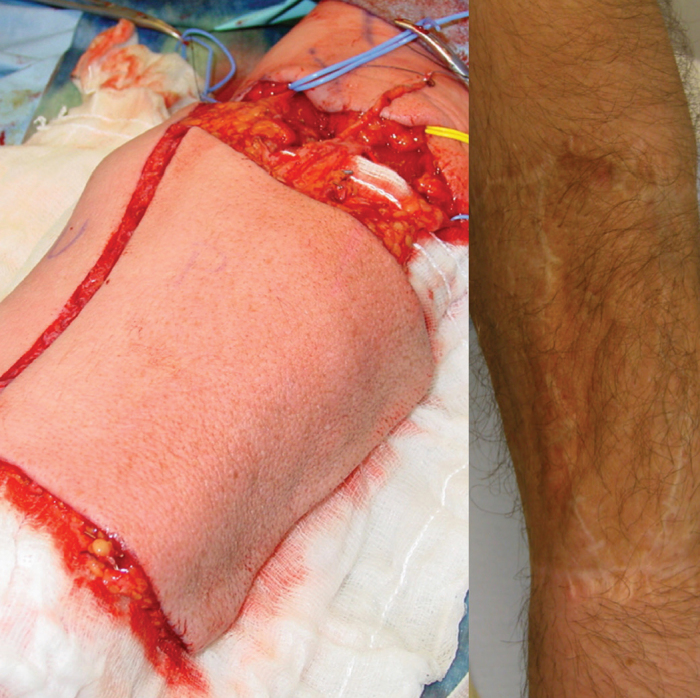
Radial forearm flap-donor site and postoperative period (Mr. Ralph’s photo archive)
This study was designed for reviewing the literature for phalloplasty articles and comparing the results and complications of this surgery.
Material and methods
In this article, we performed a comprehensive review of the literature regarding phalloplasty and penile reconstructive surgery between January 2008 and May 2016. 15 research articles and the results of 276 patients were included. Our research was stricted to English-language studies. This article mainly reviews the outcomes of recent studies about phalloplasty reported in the literature. We searched the Medline and Cochrane Library with the following MeSH terms; ‘phalloplasty’, ‘transsexualism’, ‘radial forearm’, ‘free flap’, ‘sex reassignment surgery’, ‘surgical flaps’. Original research articles were included in the study. Patient numbers, indications, operative techniques, postoperative results and complications were reported in detail. Also the results and the complications of the similar techniques were compared.
Results
In this review, we have included 15 research articles and the results of 276 patients were examined.
Studies revealed several indications and when these indications were reviewed (Table 1):
Table 1.
Indications and operative techniques
| Author | No of patients | Indications | Type of phalloplasty |
|---|---|---|---|
| Rieger et al.[11] | 27 | Female-to-male transgender | Radial forearm free-flap |
| Kim et al.[12] | 58 | Female-to-male transgender | Radial forearm osteocutaneous flap |
| Callens et al.[12] | 18 | 4 (46 XY DSD and micropenis), 8 (bladder or cloacal exstrophy), 5 (trauma), 1 (idiophatic) | 14 Radial forearm free-flap, 4 Anterolateral thigh flap |
| Garcia et al.[12] | 25 | Female-to-male transgender | 15 Radial artery forearm-flap, 10 pedicle-flap suprapubic phalloplasty |
| Massanyi et al.[12] | 10 | 8 classic bladder exstrophy, 2 cloacal exstrophy | Radial forearm free-flap |
| Garaffa et al.[12] | 16 | Bladder/cloacal exstrophy and micropenis-epispadias complex | Total phallic reconstruction with radial artery based forearm free flap phalloplasty |
| Bajpai et al.[12] | 4 | Disorder of sex development with 46 XY and severe penile deficency | Bird-Wing’ abdominal phalloplasty |
| Elhaggagy et al.[12] | 9 | Intersex patients with ambiguus genitalia as a result of female cicumcision | Radial forearm free-flap |
| Lumen et al.[12] | 7 | Female-to-male transgender | 6 Radial forearm free-flap, 1 Anterolateral thigh flap |
| Timsit et al.[12] | 6 | Bladder exstrophy and unsatisfactory penile appearance | Radial forearm free-flap |
| Lumen et al.[12] | 11 | 6 shrivelled penis, 2 penile necrosis, 1 micropenis, 1 crippled penis, 1 penile amputation | 7 Radial forearm free-flap, 4 Anterolateral thigh flap |
| Terrier et al.[12] | 24 | 23 Female-to-male transgender 1 Penil amputation | Suprapubic phalloplasty (3 stages) |
| Song et al.[12] | 19 | Female-to-male transgender | Radial forearm free-flap |
| Falcone et al.[12] | 10 | 2 self-amputation (schizophrenic episode 3 traffic accident, 3 blast injury, 1 donkey bite, 1 fournier gangrene | Radial forearm free-flap |
| Papadopulos et al.[12] | 32 | Female-to-male transgender | Osteofasciocutaneous fibular flap |
Female-to-male transgender-191,
Extraphy-40,
Penile amputation/trauma-16,
DSD and micropenis-9,
Ambiguus genitalia-9,
Other-11.
Due to these conditions, several phalloplasty techniques were performed (Table 1):
Radial forearm flap-197,
Anterolateral thigh flap-9,
Bird-wing phalloplasty-4,
Suprapubic phalloplasty-34,
Fibular flap-32.
Rieger et al.[11] reported 27 radial forearm free-flap operations for female-to-male transgender patients. In this study, 7 free groin flaps and 20 full-thickness skin grafts were used for donor site coverage. Mean functional rating was 3.6/4 for free groin flap group and 3.1/4 for full-thickness skin graft group (1=poor, 2=satisfacory, 3=good, 4=excellent), mean aesthetical rating was 3.7/4 for free groin flap group and 2.9/4 for full-thickness skin graft group. In another study by Kim et al.[12] 58 radial forearm osteocutanous flap operations were reported as gender reassignment. Satisfaction score of rigidity and volume were assessed using a scla from 1 to 5 (1=very poor, 2=poor, 3=not good, 4=good, 5=very good). Most of the patients had softened neophallus after the surgery and 12 patients, who wanted corrective operation, were reviewed. Two of these cases were due to shallow bony component and 10 of them were due to fat absorption.[12] Shallow bony components were treated with rib bone graft, 6 of fat absorptions were treated with using implant, 3 of them with fat injection and 1 with artificial dermis.[12]
After the surgery:
4 patients were very good satisfied,
7 of them were good satisfied,
1 of them was dissatisfied.[12]
Callens et al.[13] reported 18 patients:
4 had disorder of sex development,
8 had exstrophy,
5 had trauma,
1 was idiophatic.
Fourteen radial forearm free-flaps and 4 anterolateral thigh flaps used for these patients.[13] Ten of these patients were assessed for sexual satisfaction. Sexual quality of life outcomes were compared to the patients with hypospadias repair. All patients were sexually active (80% intercourse and 100% masturbation). 75% of the patients were inhibited in seeking sexual contacts while it was 40% for hypospadias. Garcia et al.[14] used radial forearm free-flap for 15 patients and 10 pedicle-flap suprapubic phalloplasty operations were included for femal-to-male transgender patients. Mean satisfaction score was 9.1/10 for suprapubic phalloplasty and 9/10 for radial artery forearm-flap phalloplasty Massanyi et al.[15] reported 8 patients with bladder, 2 patients with cloacal exstrophy and radial forearm free-flap operations were performed. Transferred flap survived in all 10 patients. Garaffa et al.[16] reported 16 patients with bladder/cloacal exstrophy and radial artery forearm free-flaps were used. 15 patients (93%) were fully satisfied with phallic cosmesisand size. 1 patient had distal part loss due to acute thrombosis. Bajpai et al.[17] reported Bird-Wing abdominal phalloplasty technique for 4 patients who had disorder of sex development and severe penile deficiency. The neophallus remained viable and survived in all patients and also there was no problem about the donor site. Elhaggagy et al. [18] operated 9 intersex patients with using radial artery forearm free-flap. All patients were fully satisfied. Lumen et al.[19,20] reported two studies about phalloplasty. In the first study, 11 patients were included and indications were different.[19] 6 patients with shrivelled penis, 2 patients with penile necrosis, 1 patient had micropenis, 1 patient had crippled penis and 1 had penile amputation.[19] For 7 patients, radial forearm free-flaps were used and for 4 patients, anterolateral thigh flaps were used.[19] All flaps survived and there were no complications about the donor site. In the second study, 7 female-to-male transgender surgeries were included. 6 of the surgeries were radial forearm free-flap phalloplasty operations and 1 of them was anterolateral thigh flap phaloplasty.[20] Graft suvival was noticed for all patients, patient satisfaction was high for 6/7 patients and was moderate for 1 patient. Timsit et al. [21] reported 6 radial forearm free-flap phalloplasty operastions due to bladder exstrophy and unsatisfactory penile appearance and there were 3 complications in the postoperative period. Terrier et al.[1] reported the results of 24 patients and 23 of them were due to female-to-male gender reassignment,1 of them was due to penile amputation. Neophallus survived in all patients and overall satisfaction was 95%. Song et al.[22] reported 19 radial forearm free-flap phalloplasties due to female-to-male gender reassignment. There were good aesthetic results but unfortunately there were 2 comlete flap loss. Falcone et al.[23] reported 10 patients with several indications. Two patients had self-amputation due to schizophrenic episode, 3 had traffic accident, 3 had blast injury, 1 had donkey bite and 1 had fournier gangrene. All patients were fully satisfied and urinary functions were normal. Radial forearm free-flaps were used for these patients. Papadopulos et al.[24] reported 32 osteocutaneous fibular flap phalloplasty operations. All patients were sexually active and reported good results during the intercourse. When considering the overall results of these studies, succesful outcomes were reported. Most of the patients were fully satisfied with both appearence and the function. Also very good quality of life results were obtained.
When all the complications in the studies were reviewed (Table 2):
Table 2.
Operative results and complications
| Author | Results | Complications |
|---|---|---|
| Rieger et al.[12] | 7 free groin flaps (Group groin (Group B) used for the donor site coverage | 1 patient required revision due to haematoma (Group A), A),20FTSGsfromthe 2 patients (Group B) required revision at the forearm 1 patient (Group B) had wound dehiscence at donor site |
| Kim et al.[12] | 12 patients had softened phalli (2 due to shallow, bony component and 10 due to fat absorption) | 6 patients were treated with implant, 3 with fat injection, 2 with rib bone graft and 1 with artificial dermis |
| Callens et al.[12] | 10 patients were assessed with Sexual quality of life (QoL). All men were sexually active | No complications with donor area, 8 urethral complications, 3 infections, 1 pilonidal sinus |
| Garcia et al.[12] | Overall satisfaction was 9.1/10 for SP, 9.4/10 for RAP without nerve anastomosis, 8.7/10 for RAP with nerve anastomosis. Mean flaccid phallus length during follow-up was 13.3cm for SP, 11.95 cm for RAP | No complications indicated |
| Massanyi et al.[12] | 10/10 flap survival. | 1 patient required operative debridement for small area of partial necrosis, 1 required revision of arterial anastomosis due to arterial thrombosis |
| Garaffa et al.[12] | 3 stages were completed in 12 patients, 4 had undergone phallus construction only. | 2 had acute arterial trombosis, 1 had phallic partial necrosis, 3 had incomplete arm graft take, 6 had fistula, 2 had stricture, 2 had prosthesis infection, 1 cylinder was too short |
| Bajpai et al.[12] | The phalloplasty remained viable during follow-up for all cases and wound healing was excellent. | No complications indicated |
| Elhaggagy et al.[12] | The length of the new phallus was 11–15 cm and all patients were fully satisfied with the size and cosmetic appearance. | No complications were seen. |
| Lumen et al.[12] | In all patients the graf survived. | 1 pulmonary embolism, 1 severe haematuria with clotting and obstruction of the urinary catheters. 5 had urethral reconstruction due to fistula/stricture. No complications with donor area. |
| Timsit et al.[12] | Flap survival was 100% the mean penile length was 12.6 cm in traction. | 1 late prosthesis extorsion and infection of artifical sphincter, 2 urethral stricture |
| Lumen et al.[12] | Total flap survival was noticed in all patients. In 9 patients aesthetic appearance was excellent and in 2 appearance was moderate. | No complications for the donor area, 8 patients underwent urethral reconstruction, 4 urethral complications, persistent fistula at anastomosisi developed in 3 patients |
| Terrier et al.[12] | Overall satisfaction was 95%, Appearance 95%, Penile length 81%, Circumference 71% | Stage 1 (Tissue expanders)-17% minor complications (2 migration, 1 perforation, 1 abscess) / Stage 2 (Tubing)-54% minor complications(10 infections, 18 shearing sutures) / Stage 3 (Liberation)-4% (1 distal necrosis) |
| Song et al.[12] | Total flap survival was noticed in all patients. In 9 patients aesthetic appearance was excellent and in 2 appearance was moderate. | 2 tip necrosis, 1 distal flap loss, 3 forearm celulitis surrounding the tube-shaped skin graft, 2 complete flap loss, 2 neoscrotal abscess, 1 fistula, 5 stricture, 9 fistula+stricture, 1 chronic moderate left hydronephrosis |
| Falcone et al.[12] | All patients were fully satisfied and urinary functions were normal | 2 patients had acute arterial thrombosisof the microsurgical anastomosis, 3 patients had urethral fistula, 1 patient developed stricture, no complications about the donor site. |
| Papadopulos et al.[12] | All patients were sxually active and reported good to very good sexual intercourse | 2 total, 4 partial necrosis, 10 urethral stricture, 7 fistula, donor site morbidity was moderate |
Softened phalli-12,
Infection-19,
Thrombosis/necrosis-16,
Urethral complications-60,
Flap loss-3,
Other-36.
There were some rare systemic problems like pulmonary embolism. There were urethral complications and most of them were urethral stricture and fistula that required reconstruction. Most of the complications related with neophallus were arterial thrombosis and necrosis that caused total or partial flap loss. Reconstructive additional procedures were performed for that complications.
Discussion
Phalloplasty is a challenging and a mysterious operation that has several indications. This reconstructive operation is usually performed for gender reassignment and penile amputation(usually postoncologic).[25] Micropenis, epispadias, hypospadias are the less frequent indications.[25] Different surgical techniques would be used and for each techniques there are several benefits and limitations.[26] Metoidioplasty is one of these techniques and easier when comparing to other techniques but there are some important limitations like short phallus that does not allow for sexual penetration.[26] Radial forearm-flap, first described by Song et al.[22], Chang and Hwang[26–28], has probably the best cosmetic and functional results (Figure 3). Radial forearm free-flap provides superior cosmetic results with a cylindirical phallus and it is better than the wedge-shaped neophallus as in infraumbilical and groin flap phalloplasties (Figure 2, 4).[27,29–33] Salgado et al.[34] used uterine mucosa for prelamination of neourethra for a patient who underwnt hysterectomy and vaginectomy before the stage of radial forearm phalloplasty and reported good result.
Figure 4.
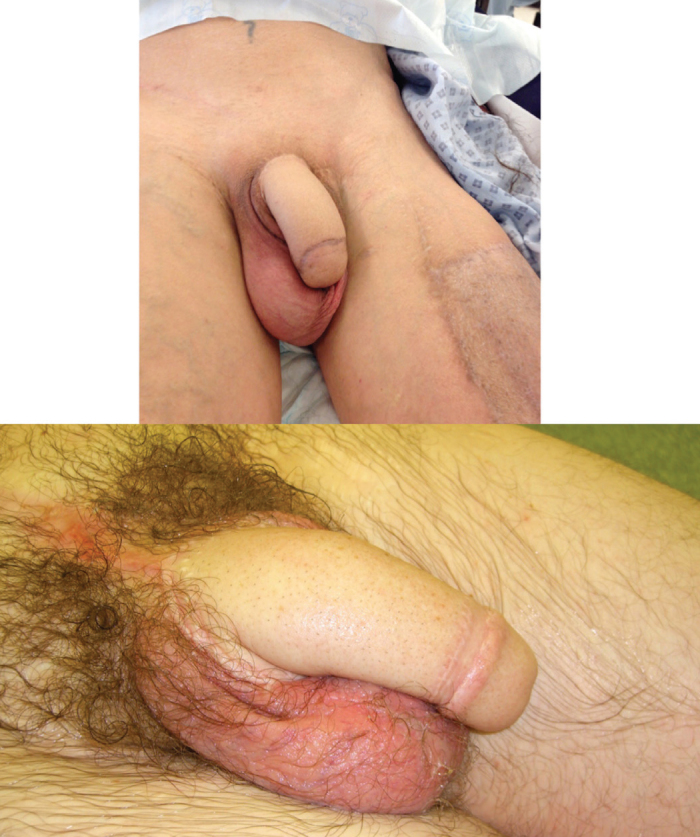
Postoperative appearance and aesthetic neophallus (Mr. Ralph’s photo archive)
With fibula flap and latissimus dorsi flap, there is no need for an erection device.[26] For thigh flap, it is easier to hide the donor site and the suprapubic flap phalloplastiy is an easier technique.[26] When compared to radial forearm flap, there are some advantages of using anterolateral thigh flaps.[33] With anterolateral thigh flap, there is no need for a microsurgical procedure, no scars are seen at the noticable sites, no major vessel damage and small functional loss at donor site.[35]
Types of procedures would be classified as microsurgical and non-microsurgical.[35] Microsurgical procedures are myocutaneous latissimus dorsi flap, radial forearm free-flap and osteocutaneous fibular flap phalloplasties.[36] Non-microsurgical operations are extended pedicle island groin flap, De Castro neophalloplasty and scrotal phalloplasty operations.[36] Penil reconstructive surgery has also psycological effects beside it’s functional and aesthetic effects.[37] Several techniques are commonly used for penile lengthening and penile girth enhancement.[37] Penile girth enhancement is mainly performed by two different techniques.[37] Cavernosal and albugineal surgeries are used for this purpose.[37] Autologous dermal or dermis-fat grafts are used for enhancement during pericavernosal surgery and alloplastic or saphenous-patch grafts are used for enlargement of the cavernous body in albugineal surgery.[37–40] Also there are some techniques used for penile lengthening such as suspensory ligament release, augmentation corporoplasty, ventral phalloplasty, and suprapubic lipectomy, monsplasty.[41] Ventral phalloplasty would be used for penile lengthening with or after partial penectomy as Wallen et al.[42] reported good results. Aphallia is a rare congenital defect with the ratio of 1/30 million births.[43] Phallic reconstruction is challenging and there are several microsurgical techniques are used but also several limitations for these techniques are known. Lack of furher growth is one of the limitations and also the large size of neophallus would a problem for a child at younger age. [43] There are several suggestions about the timing of surgery and according to most of them phalloplasty should be performed before or at around the time of puberty.[4,33,44] Most of the techniques use somatic tissues that are not reponsive to hormones and for pediatric patients, adult-size phallus should be planned.[4,33,45] Scrotal phalloplasty described by Bajpai et al.[43] would be considered for the childs at early school ages. Parascrotal flap phalloplasty is a similar technique that provides a physiological and psychological satisfaction with a realistic penis with urethra.[46] ‘Bird-wing’ abdominal phalloplasty is a different technique by Bajpai et al.[17] that would be used at around the time of puberty for minimising the psychological trauma. Gender reassignment surgeries have become more common in different population worldwide and a signficant decrease in age for the recent years, is clearly obtained in a study by Aydin et al.[47] in Denmark. In this study, the sex ratio was 1.9/1 (female-to-male/male-to-female) that is similar with Belgium and Netherlands.[47–49]
Awareness of gender dysphoria and its treatment are increasing.[50] Female-to-male transgender surgery includes some components such as hysterectomy, ovariectomy, flap preparation for urethral elongation, formation of distal urethra, metoidioplasty and phalloplasty (if the patient wants a neophallus).[5] Penile cancer is a rare malignency and the most common form is squamous cell carcinoma.[51] Penile cancers are generally treated with subtotal or total penectomy bu if the patient refuses amputation different techniques would be used.[51] Penile amputations are also uncommon conditions that would ocur with self mutilation, accident or felonious assault.[52] The treatment of amputation includes basic forms such as surgical replantation, taiolring the penile stamp and total phallic reconstruction.[52]
Penile fracture is one the indications of penile reconstructive surgery as a cause of rupture of tunica albuginea of the corpora cavernosa after blunt trauma to erected penis and it is an uncommon condition in Europe and America.[7] There are conservative and surgical managements of penile fracture.[7] Electrical burn is one of the other rare coauses of penile loss and Sridhar et al.[53] reported a challenging case that was treated with phalloplasty using a right-side groin flap. In recent years, augmentation phalloplasty of normal penis is gaining popularity among men but there would be some complications.[54] Spyriounis et al. [54] reported a case with dorsal penile skin necrosis and a pedicled anterolateral thigh flap was used for reconstruction. The donor-site morbidity is another problem during the postoperative period of phalloplasty operations. Van Caenegem et al. [55] reported the donor-site morbidity results and there were no functional limitations for daily activities, pain-free aesthetically acceptable appearance with a favorable bone health (Figure 5).
Figure 5.

Direct closure of donor site and outcomes (Mr. Ralph’s photo archive)
In conclusion, phalloplasty is a mysterious operation that would be performed due to several indications. There are different types of surgical techniques and lots of benefits and limitations for these techniques. Several studies were reported in order to present the results and complications for this operation. In this review, different techniques, results and complications of these techniques are evaluated and compared.
As a result of this review, phalloplasty is a reliable and useful operation with good functional and aesthetical results. There are some major and minor complications but most of these complications are treated with different reconstructive tecniques.
Footnotes
Peer-review: This manuscript was prepared by the invitation of the Editorial Board and its scientific evaluation was carried out by the Editorial Board.
Author Contributions: Concept – S.S.; Design – S.S., D.J.R.; Supervision – D.J.R.; Resources – S.S., D.J.R.; Materials – D.J.R.; Data Collection and/or Processing – S.S.; Analysis and/or Interpretation – D.J.R.; Literature Search – S.S.; Writing Manuscript – S.S., D.J.R.; Critical Review – D.J.R.; Other – S.S., D.J.R.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Terrier JE, Courtois F, Ruffion A, Morel Journel N. Surgical outcomes and patients’ satisfaction with suprapubic phalloplasty. J Sex Med. 2014;11:288–98. doi: 10.1111/jsm.12297. https://doi.org/10.1111/jsm.12297. [DOI] [PubMed] [Google Scholar]
- 2.Bogoras N. Uber die volle plastische Wiederherstellung eines zum Koitus fahigen Penis (Peniplastica totalis) Zentralbl Chir. 1936;63:1271–6. [Google Scholar]
- 3.Gillies H. Congenital absence of the penis. Br J Plast Surg. 1948;1:8–28. doi: 10.1016/s0007-1226(48)80006-8. https://doi.org/10.1016/S0007-1226(48)80006-8. [DOI] [PubMed] [Google Scholar]
- 4.Bluebond-Langner R, Redett RJ. Phalloplasty in complete aphallia and ambiguous genitalia. Semin Plast Surg. 2011;25:196–205. doi: 10.1055/s-0031-1281489. https://doi.org/10.1055/s-0031-1281489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Masumori N. Status of sex reassignment surgery for gender identity disorder in Japan. Int J Urol. 2012;19:402–14. doi: 10.1111/j.1442-2042.2012.02975.x. https://doi.org/10.1111/j.1442-2042.2012.02975.x. [DOI] [PubMed] [Google Scholar]
- 6.American Psychiatric Association., American Psychiatric Association. Task Force on DSM-IV. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. 4th ed. xxxvii. Washington, DC: American Psychiatric Association; 2000. p. 943. [Google Scholar]
- 7.Garaffa G, Raheem AA, Ralph DJ. Penile fracture and penile reconstruction. Curr Urol Rep. 2011;12:427–31. doi: 10.1007/s11934-011-0201-5. https://doi.org/10.1007/s11934-011-0201-5. [DOI] [PubMed] [Google Scholar]
- 8.McAninch JW. Traumatic and reconstructive urology. xxii. Philadellphia: Saunders; 1996. p. 743. [Google Scholar]
- 9.Rashid M, Tamimy MS. Phalloplasty: The dream and the reality. Indian J Plast Surg. 2013;46:283–93. doi: 10.4103/0970-0358.118606. https://doi.org/10.4103/0970-0358.118606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hage JJ, De Graaf FH. Addressing the ideal requirements by free flap phalloplasty: some reflections on refinements of technique. Microsurg. 1993;14:592–8. doi: 10.1002/micr.1920140910. https://doi.org/10.1002/micr.1920140910. [DOI] [PubMed] [Google Scholar]
- 11.Rieger UM, Majenka P, Wirthmann A, Sohn M, Bozkurt A, Djedovic G. Comparative Study of the Free Microvascular Groin Flap: Optimizing the Donor Site After Free Radial Forearm Flap Phalloplasty. Urology. 2016;95:192–6. doi: 10.1016/j.urology.2016.04.007. https://doi.org/10.1016/j.urology.2016.04.007. [DOI] [PubMed] [Google Scholar]
- 12.Kim SK, Kim TH, Yang JI, Kim MH, Kim MS, Lee KC. The etiology and treatment of the softened phallus after the radial forearm osteocutaneous free flap phalloplasty. Arch Plast Surg. 2012;39:390–6. doi: 10.5999/aps.2012.39.4.390. https://doi.org/10.5999/aps.2012.39.4.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Callens N, De Cuypere G, T’Sjoen G, Monstrey S, Lumen N, Van Laecke E, et al. Sexual quality of life after total phalloplasty in men with penile deficiency: an exploratory study. World J Urol. 2015;33:137–43. doi: 10.1007/s00345-014-1283-8. https://doi.org/10.1007/s00345-014-1283-8. [DOI] [PubMed] [Google Scholar]
- 14.Garcia MM, Christopher NA, De Luca F, Spilotros M, Ralph DJ. Overall satisfaction, sexual function, and the durability of neophallus dimensions following staged female to male genital gender confirming surgery: the Institute of Urology, London U.K. experience. Transl Androl Urol. 2014;3:156–62. doi: 10.3978/j.issn.2223-4683.2014.04.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Massanyi EZ, Gupta A, Goel S, Gearhart JP, Burnett AL, Bivalacqua TJ, et al. Radial forearm free flap phalloplasty for penile inadequacy in patients with exstrophy. J Urol. 2013;190(Suppl 4):1577–82. doi: 10.1016/j.juro.2012.12.050. [DOI] [PubMed] [Google Scholar]
- 16.Garaffa G, Spilotros M, Christopher NA, Ralph DJ. Total phallic reconstruction using radial artery based forearm free flap phalloplasty in patients with epispadias-exstrophy complex. J Urol. 2014;192:814–20. doi: 10.1016/j.juro.2014.03.105. https://doi.org/10.1016/j.juro.2014.03.105. [DOI] [PubMed] [Google Scholar]
- 17.Bajpai M. “Bird-Wing” abdominal phalloplasty: A novel surgical technique for penile reconstruction. J Indian Assoc Pediatr Surg. 2013;18:49–52. doi: 10.4103/0971-9261.109351. https://doi.org/10.4103/0971-9261.109351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Elhaggagy A, Elgammal M, Gadelmoula M, Elgammal T. Phalloplasty for an amputated phallus in intersex patients. Arab J Urol. 2012;10:382–7. doi: 10.1016/j.aju.2012.06.002. https://doi.org/10.1016/j.aju.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lumen N, Monstrey S, Ceulemans P, van Laecke E, Hoebeke P. Reconstructive surgery for severe penile inadequacy: phalloplasty with a free radial forearm flap or a pedicled anterolateral thigh flap. Adv Urol. 2008:704343. doi: 10.1155/2008/704343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lumen N, Monstrey S, Selvaggi G, Ceulemans P, De Cuypere G, Van Laecke E, et al. Phalloplasty: a valuable treatment for males with penile insufficiency. Urology. 2008;71:272–7. doi: 10.1016/j.urology.2007.08.066. https://doi.org/10.1016/j.urology.2007.08.066. [DOI] [PubMed] [Google Scholar]
- 21.Timsit MO, Mouriquand PE, Ruffion A, Bouillot A, Dembele D, Mejean A, et al. Use of forearm free-flap phalloplasty in bladder exstrophy adults. BJU Int. 2009;103:1418–21. doi: 10.1111/j.1464-410X.2008.08286.x. https://doi.org/10.1111/j.1464-410X.2008.08286.x. [DOI] [PubMed] [Google Scholar]
- 22.Song R, Gao Y, Song Y, Yu Y, Song Y. The forearm flap. Clin Plast Surg. 1982;9:21–6. [PubMed] [Google Scholar]
- 23.Falcone M, Garaffa G, Raheem A, Christopher NA, Ralph DJ. Total Phallic Reconstruction Using the Radial Artery Based Forearm Free Flap After Traumatic Penile Amputation. J Sex Med. 2016;13:1119–24. doi: 10.1016/j.jsxm.2016.05.003. https://doi.org/10.1016/j.jsxm.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 24.Papadopulos NA, Schaff J, Biemer E. The use of free prelaminated and sensate osteofasciocutaneous fibular flap in phalloplasty. Injury. 2008;39(Suppl 3):S62–7. doi: 10.1016/j.injury.2008.05.019. [DOI] [PubMed] [Google Scholar]
- 25.Thione A, Cavadas PC, Rubi CG. Microvascular Staged Phalloplasty Preserving Original Glans in a Severe Hypospadias: A Case Report. Plast Reconstr Surg Glob Open. 2015;3:e588. doi: 10.1097/GOX.0000000000000562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blaschke E, Bales GT, Thomas S. Postoperative imaging of phalloplasties and their complications. AJR Am J Roentgenol. 2014;203:323–8. doi: 10.2214/AJR.13.12190. https://doi.org/10.2214/AJR.13.12190. [DOI] [PubMed] [Google Scholar]
- 27.Garaffa G, Raheem AA, Christopher NA, Ralph DJ. Total phallic reconstruction after penile amputation for carcinoma. BJU Int. 2009;104:852–6. doi: 10.1111/j.1464-410X.2009.08424.x. https://doi.org/10.1111/j.1464-410X.2009.08424.x. [DOI] [PubMed] [Google Scholar]
- 28.Chang TS, Hwang WY. Forearm flap in one-stage reconstruction of the penis. Plast Reconstr Surg. 1984;74:251–8. doi: 10.1097/00006534-198408000-00014. https://doi.org/10.1097/00006534-198408000-00014. [DOI] [PubMed] [Google Scholar]
- 29.Bouman FG. The first step in phalloplasty in female transsexuals. Plast Reconstr Surg. 1987;79:662–4. https://doi.org/10.1097/00006534-198704000-00038. [PubMed] [Google Scholar]
- 30.McGregor IA, Jackson IT. The groin flap. Br J Plast Surg. 1972;25:3–16. doi: 10.1016/s0007-1226(72)80003-1. https://doi.org/10.1016/S0007-1226(72)80003-1. [DOI] [PubMed] [Google Scholar]
- 31.Perovic S. Phalloplasty in children and adolescents using the extended pedicle island groin flap. J Urol. 1995;154:848–53. doi: 10.1097/00005392-199508000-00142. https://doi.org/10.1016/S0022-5347(01)67183-0. [DOI] [PubMed] [Google Scholar]
- 32.Puckett CL, Montie JE. Construction of male genitalia in the transsexual, using a tubed groin flap for the penis and a hydraulic inflation device. Plast Reconstr Surg. 1978;61:523–30. doi: 10.1097/00006534-197804000-00005. https://doi.org/10.1097/00006534-197804000-00005. [DOI] [PubMed] [Google Scholar]
- 33.Hasegawa K, Namba Y, Kimata Y. Phalloplasty with an innervated island pedicled anterolateral thigh flap in a female-to-male transsexual. Acta Med Okyama. 2014;68:183–90. doi: 10.18926/AMO/52660. [DOI] [PubMed] [Google Scholar]
- 34.Salgado CJ, Fein LA, Chim J, Medina CA, Demaso S, Gomez C. Prelamination of Neourethra with Uterine Mucosa in Radial Forearm Osteocutaneous Free Flap Phalloplasty in the Female-to-Male Transgender Patient. Case Rep Urol. 2016;2016:8742531. doi: 10.1155/2016/8742531. https://doi.org/10.1155/2016/8742531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hasegawa K, Namba Y, Kimata Y. Phalloplasty with an innervated island pedicled anterolateral thigh flap in a female-to-male transsexual. Acta Med Okayama. 2013;67:325–31. doi: 10.18926/AMO/51869. [DOI] [PubMed] [Google Scholar]
- 36.Oliveira DE, da Cruz ML, Liguori R, Garrone G, Leslie B, Ottoni SL, et al. Neophalloplasty in boys with aphallia: A systematic review. J Pediatr Urol. 2016;12:19–24. doi: 10.1016/j.jpurol.2015.10.003. https://doi.org/10.1016/j.jpurol.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 37.Alei G, Letizia P, Ricottilli F, Simone P, Alei L, Massoni F, et al. Original technique for penile girth augmentation through porcine dermal acellular grafts: results in a 69-patient series. J Sex Med. 2012;9:1945–53. doi: 10.1111/j.1743-6109.2012.02744.x. https://doi.org/10.1111/j.1743-6109.2012.02744.x. [DOI] [PubMed] [Google Scholar]
- 38.Austoni E, Guarneri A, Cazzaniga A. A new technique for augmentation phalloplasty: albugineal surgery with bilateral saphenous grafts--three years of experience. Eur Urol. 2002;42:245–53. doi: 10.1016/s0302-2838(02)00264-6. https://doi.org/10.1016/S0302-2838(02)00264-6. [DOI] [PubMed] [Google Scholar]
- 39.Alter GJ. Augmentation phalloplasty. Urol Clin North Am. 1995;22:887–902. [PubMed] [Google Scholar]
- 40.Alter GJ. Penile enlargement surgery. Tech Urol. 1998;4:70–6. [PubMed] [Google Scholar]
- 41.Caso JR, Myers MD, Wiegand L, Rodriguez A, Hann S, Carrion R. Phalloplasty and penile implant surgery. Curr Urol Rep. 2009;10:475–7. doi: 10.1007/s11934-009-0075-y. https://doi.org/10.1007/s11934-009-0075-y. [DOI] [PubMed] [Google Scholar]
- 42.Wallen JJ, Baumgarten AS, Kim T, Hakky TS, Carrion RE, Spiess PE. Optimizing penile length in patients undergoing partial penectomy for penile cancer: novel application of the ventral phalloplasty oncoplastic technique. Int Braz J Urol. 2014;40:708–9. doi: 10.1590/S1677-5538.IBJU.2014.05.18. https://doi.org/10.1590/S1677-5538.IBJU.2014.05.18. [DOI] [PubMed] [Google Scholar]
- 43.Bajpai M. Scrotal phalloplasty: A novel surgical technique for aphallia during infancy and childhood by pre-anal anterior coronal approach. J Indian Assoc Pediatr Surg. 2012;17:162–4. doi: 10.4103/0971-9261.102335. https://doi.org/10.4103/0971-9261.102335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Djordjevic ML, Bumbasirevic MZ, Vukovic PM, Sansalone S, Perovic SV. Musculocutaneous latissimus dorsi free transfer flap for total phalloplasty in children. J Pediatr Urol. 2006;2:333–9. doi: 10.1016/j.jpurol.2006.05.003. https://doi.org/10.1016/j.jpurol.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 45.Perovic SV, Djinovic R, Bumbasirevic M, Djordjevic M, Vukovic P. Total phalloplasty using a musculocutaneous latissimus dorsi flap. BJU Int. 2007;100:899–905. doi: 10.1111/j.1464-410X.2007.07084.x. https://doi.org/10.1111/j.1464-410X.2007.07084.x. [DOI] [PubMed] [Google Scholar]
- 46.Goyal A, Bianchi A. The parascrotal flap phallo-urethroplasty for aphallia reconstruction in childhood: report of a new technique. J Pediatr Urol. 2014;10:769–72. doi: 10.1016/j.jpurol.2014.01.007. https://doi.org/10.1016/j.jpurol.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 47.Aydin D, Buk LJ, Partoft S, Bonde C, Thomsen MV, Tos T. Transgender Surgery in Denmark From 1994 to 2015: 20-Year Follow-Up Study. J Sex Med. 2016;13:720–5. doi: 10.1016/j.jsxm.2016.01.012. https://doi.org/10.1016/j.jsxm.2016.01.012. [DOI] [PubMed] [Google Scholar]
- 48.Bakker A, van Kesteren PJ, Gooren LJ, Bezemer PD. The prevalence of transsexualism in The Netherlands. Acta Psychiatr Scand. 1993;87:237–8. doi: 10.1111/j.1600-0447.1993.tb03364.x. https://doi.org/10.1111/j.1600-0447.1993.tb03364.x. [DOI] [PubMed] [Google Scholar]
- 49.De Cuypere G, Janes C, Rubens R. Psychosocial functioning of transsexuals in Belgium. Acta Psychiatr Scand. 1995;91:180–4. doi: 10.1111/j.1600-0447.1995.tb09763.x. https://doi.org/10.1111/j.1600-0447.1995.tb09763.x. [DOI] [PubMed] [Google Scholar]
- 50.Majumder A, Sanyal D. Outcome and preferences in female-to-male subjects with gender dysphoria: Experience from Eastern India. Indian J Endocrinol Metab. 2016;20:308–11. doi: 10.4103/2230-8210.179988. https://doi.org/10.4103/2230-8210.179988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Horton CE, Dean JA. Reconstruction of traumatically acquired defects of the phallus. World J Surg. 1990;14:757–62. doi: 10.1007/BF01670522. https://doi.org/10.1007/BF01670522. [DOI] [PubMed] [Google Scholar]
- 52.Jezior JR, Brady JD, Schlossberg SM. Management of penile amputation injuries. World J Surg. 2001;25:1602–9. doi: 10.1007/s00268-001-0157-6. https://doi.org/10.1007/s00268-001-0157-6. [DOI] [PubMed] [Google Scholar]
- 53.Sridhar R, Jayaraman V. A challenging case of total phalloplasty. Indian J Plast Surg. 2012;45:148–50. doi: 10.4103/0970-0358.96618. https://doi.org/10.4103/0970-0358.96618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Spyriounis PK, Karmiris NI. Partial penile reconstruction following fat augmentation with anterolateral thigh perforator flap. J Plast Reconstr Aesthet Surg. 2012;65:e15–7. doi: 10.1016/j.bjps.2011.07.025. [DOI] [PubMed] [Google Scholar]
- 55.Van Caenegem E, Verhaeghe E, Taes Y, Wierckx K, Toye K, Goemaere S, et al. Long-term evaluation of donor-site morbidity after radial forearm flap phalloplasty for transsexual men. J Sex Med. 2013;10:1644–51. doi: 10.1111/jsm.12121. https://doi.org/10.1111/jsm.12121. [DOI] [PubMed] [Google Scholar]


