Abstract
Objective
To determine the predictive value of free and bioavailable testosterone levels on the detection of high-grade prostate cancer proven by histopathological examination of transrectal prostate biopsy specimens.
Material and methods
A total of 405 patients who underwent transrectal prostate biopsy due to high prostatic specific antigen (PSA) (>2.5 ng/mL) and/or abnormal findings at digital rectal examination were included in this study. Blood free and bioavailable testosterone levels were calculated by the formula recommended by International Society for the Study of the Aging Male (ISSAM). The patients were stratified according to the D’Amico classification based on PSA levels and histological outcomes of prostate biopsies as benign, low, intermediate and high-risk prostate cancer. Patients were also divided into five groups according to the percentage of cancerous cores.
Results
Prostate cancer was detected in 160 of 405 (39.5%) patients. Total, free and bioavailable testosterone levels did not differ significantly between the patients with benign or malign histology. However, mean free (6.2 vs. 5.2 ng/dL, p=0.02) and bioavailable (151 vs. 125 ng/dL, p=0.001) testosterone levels were found to be significantly different in men with low-intermediate and high-risk prostate cancer. Moreover, a significant correlation was found between free, and bioavailable testosterone levels and percentage of cores with cancer (p=0.002 for free and p=0.016 for bioavailable testosterone, respectively).
Conclusion
This prospective clinical study demonstrates that reduced levels of calculated blood free and bioavailable testosterone levels are associated with an increased risk of high-grade prostate cancer. Based on these findings blood free and bioavailable testosterone levels may be be thought to be an adjunctive factor in the prediction of high-risk prostate cancer.
Keywords: Prostate cancer, prostate-specific antigen, radical prostatectomy, testosterone, transrectal prostate biopsy
Introduction
Despite advancements in surgical techniques and recent technologic developments, dealing with prostate cancer (PCa) is currently drifted to conservative approach, particularly for the patients in low-intermediate risk group at the initial stage. Clinicians need accurate predictors to determine the appropriate treatment before counselling these patients to active surveillance, watchful waiting protocols, focal therapies or surgery. Current predictors for progression or aggressiveness of PCa are still far from satisfying.
The relationship between serum testosterone and PCa may play a key role in differentiating low vs high risk patients. It was previously demonstrated that the pretreatment serum androgen levels were related to histopathologic findings at radical prostatectomy (RP).[1] The available evidence obtained from clinically-localized PCa series of patients who underwent RP suggests that the levels of serum testosterone at pretreatment are associated with advanced pathologic stages.[2,3] More importantly, several studies have revealed that low testosterone levels were associated with high-grade PCa at the time of diagnosis.[3,4]
Historically, testosterone was discredited by many urologists as it may cause PCa or flare up occult PCa, and thereby aggravating the disease. This idea is based on the findings by Huggins and Hodges, who reported that PCa is androgen-dependent and it regressed when testosterone levels are reduced through castration or neutralization of its activity and progressed when exogenous testosterone is given.[5] Despite the central role of androgens in established PCa, whether androgens are responsible for the initiation of PCa has been a more controversial issue.[6] Recently published studies have failed to show increased risk of developing PCa in men with higher testosterone levels.[7,8]
Normal cells with mitochondria generate energy by metabolizing glucose both via inefficient glycolysis and more efficient mitochondrial oxidation. The Warburg effect is defined as the malignant transformation of normal cells to take up high levels of glucose and to secrete lactate in the presence of oxygen in most solid tumors.[9] It can be suggested that while glucose consumption is higher in cancer cells, testosterone consumption can be higher in PCa cells.
Several clinical studies reported that low total or free testosterone levels can be a marker for occult PCa and aggressive form of PCa regardless of the disease stage.[10–12] Others found that low testosterone levels were associated with high-grade PCa, worse presentation, lymph node and seminal vesicle involvement after radical prostatectomy, and poor responses to hormonal therapy.[13,14] In line with those findings, it can be speculated that low testosterone levels might be associated with the increased PCa risk, disease aggressiveness, late-stage diagnosis, and shorter life expectancy.[4,11,12,15–18]
The current study aims to test this association and to the best of our knowledge, the relationship of all pretreatment total, free and bioavailable testosterone levels with PCa has not been investigated in a prospectively designed study.
Material and methods
Study population
This study was conducted in compliance with recognized international standards, including the principles of the Declaration of Helsinki involving Human Subjects, and each patient’s written, undersigned informed consent for the use of their information was obtained. The study included 405 males who underwent first time transrectal ultrasound (TRUS)-guided prostate needle biopsies during a 3-year period. The indication for TRUS-guided prostate biopsy was suspicion of PCa on the basis of the results of digital rectal examination (DRE) and/or elevations of prostate- specific antigen (PSA) levels above 2.5 ng/mL. Patients who had acute prostatitis, symptomatic or asymptomatic urinary tract infection, and indwelling urethral catheter were excluded. Other exclusion criteria were current use of testosterone replacement therapy, 5-α reductase inhibitors or other drugs altering prostate growth and PSA levels; previous prostatic surgery or radiotherapy; histopathology-proven diagnosis of atypical small acinar proliferation, high-grade prostatic intraepithelial neoplasia, or ductal adenocarcinoma.
Biochemical assay
Blood samples for the measurements of total testosterone, sex hormone binding globulin (SHBG), albumin and PSA were taken between 07:00–10:00 am after an overnight fasting and processed immediately before any intervention, as recommended by the Endocrine Society Guideline.[19] Serum testosterone levels were measured in the same laboratory by using a commercially available radioimmunoassay kit. Free and bioavailable testosterone were calculated using the formula available on the web site of the International Society for the Study of the Aging Male ( http://www.issam.ch/freetesto.html).[19]
Transrectal prostate biopsy
A 12–core standard TRUS-guided prostate biopsy was taken using 18G Tru-cut biopsy needles. In cases with persistently high PSA levels 20-core re-biopsies including sampling of transition zone was performed. Other indications for saturation biopsy were included negative second biopsy, high prostate volume, high PSA levels and negative first biopsy. Patients those considered for active surveillance underwent 20-core re-biopsies. In patients who had multiple biopsies, the worst pathological results were taken as reference. Patients were classified based on tumor volume, histopathological findings, Gleason scores and PSA levels at diagnosis according to the classification of D’Amico et al.[20]. Therefore, the comparisons were also made regardless of PSA levels.
Statistical analysis
The distribution of continuous variables was evaluated according to the Kolmogorov-Simirnov normality test. If the distribution was normal, a parametric Student-t test or parametric one-way ANOVA tests were used for statistical analysis. If the distribution was not normal, a nonparametric Mann-Whitney U test or Kruskal-Wallis tests were used. The continuous variables were presented as means, medians and ranges where convenient, whereas categorical variables were reported as percentages. Statistical significance was considered at p<0.05. A statistical software package NCSS 2000 was used for all statistical analyses.
Results
A total of 405 patients who met the study criteria were included into this prospective work. Mean age of the study population was 63±8.1 (years, range 43–78). Median PSA and free PSA levels were 6.6 and 1.25 (range, 0.35–48.77 vs. 0.03–6.13 ng/mL) respectively. Demographic characteristics and baseline data of the study population are summarized in Table 1.
Table 1.
Baseline characteristics of the study patients
| Patients (n) | 405 |
|---|---|
| Mean age (years) | 63±8.1 |
| Median PSA (ng/mL) | 6.6 |
| Median free PSA (ng/mL) | 1.25 |
| Mean albumin (g/dL) | 4.4±0.33 |
| Mean sex hormone binding globulin (nmol/L) | 40.9±16 |
| Mean total testosterone (ng/dL) | 345±126 |
| Mean free testosterone (ng/dL) | 6±2 |
| Mean bioavailable testosterone (ng/dL) | 144±48 |
Differentiation between benign and malign histologies
The patients’ total free and bioavailable testosterone levels were compared in Table 2 by using Student’s t–test. Mean total, free and bioavailable testosterone levels were not significantly different in patients with (n=160) and without PCa (n=245) (p=0.87 for total, 0.26 for free and 0.18 for bioavailable testosterone) (Table 3).
Table 2.
Mean total, free and bioavailable testosterone levels between patients with benign and malign histology
| Benign (n=245) | Cancer (n=160) | p | |
|---|---|---|---|
| Total testosterone (ng/dL) | 347±124 | 344±128 | 0.877 |
| Free testosterone (ng/dL) | 6.1±2 | 5.8±1.9 | 0.266 |
| Bioavailable testosterone (ng/dL) | 148±49 | 141±47 | 0.187 |
Table 3.
Comparison of testosterone levels according to the risk groups
| Total testosterone (ng/dL) | p | Free testosterone (ng/dL) | p | Bioavailable testosterone (ng/dL) | p | |
|---|---|---|---|---|---|---|
| High risk cancer | 347±128 | 0.443 | 6.1±2 | 0.001 | 148±48 | 0.0001 |
| Benign, low and intermediate risk | 328±124 | 5.2±1.6 | 124±43 |
Differentiation between low risk and high risk groups
When all study populations were divided into two groups as high–risk and low–intermediate risk according to the D’Amico criteria, the high-risk group exhibited significantly lower mean free (6.1±2 vs. 5.2±1.6 ng/dL, p=0.001) and bioavailable (148±48 vs. 124±43 ng/dL, p=0.0001) but not total (347±128 vs. 328±124 ng/dL, p=0.443) testosterone levels than the group of low-intermediate–risk and benign pathology (Table 4).
Table 4.
Comparison of total, free and bioavailable testosterone levels according to the D’Amico criteria
| Benign | Low risk cancer | Intermediate risk cancer | High risk cancer | p | |
|---|---|---|---|---|---|
| Total testosterone (ng/dL) | 347±128 | 356±133 | 337±120 | 327±124 | 0.671 |
| Free testosterone (ng/dL) | 6.1±2 | 6.1±1.8 | 6.2±2 | 5.2±1.6* | 0.003 |
| Bioavailable testosterone (ng/dL) | 147±49 | 148±39 | 150±52 | 124±43* | 0.012 |
Free and bioavailable testosterone levels of the patients with high risk were significantly lower than the others
Comparison between testosterone levels and histopathological findings
Patients were also divided into benign, low risk, intermediate risk and high-risk groups. Among the patients with PCa, high-risk patients exhibited lower free (5.2±1.6 vs. 6.1±1.8 ng/dL and 6.2±2 ng/dL, respectively, p=0.003) and bioavailable (124±43 vs. 148±39 and 150±52 ng/dL, respectively, p=0.012) testosterone levels than low, and intermediate risk patients (Table 4).
The relationship between Gleason scores, core involvement rates and testosterone levels
The two parameters for the aggressiveness of PCa were also evaluated as Gleason score of <7 or ≥7 and core involvement of <50% or ≥50% in patients with diagnosed PCa according to their mean total, free and bioavailable testosterone levels (Table 5). Although mean total testosterone levels were comparable, patients who exhibited Gleason score of ≥7 had significantly lower mean free and bioavailable testosterone levels, evidencing the negative correlation between the aggressiveness of the cancer and blood testosterone levels. However, no significant difference was found between mean total, free and bioavailable testosterone levels and percentage of core involvement (Table 5).
Table 5.
Comparison of Gleason scores and core involvement rates with total, free and bioavailable testosterone levels in PCa diagnosed group
| TT | p | FT | p | BT | p | |
|---|---|---|---|---|---|---|
| Gleason score <7 | 348±130 | 0.414 | 6.1±2 | 0.044 | 146±48 | 0.036 |
| Gleason score ≥7 | 333±119 | 5.6±1.8 | 136±48 | |||
|
| ||||||
| Core involvement <50% | 346±149 | 0.679 | 5.87±1.84 | 0.51 | 141.27±43.58 | 0.59 |
| Core involvement ≥50% | 332±113 | 5.62±1.84 | 136.13±48.53 | |||
TT: total testosterone; FT: free testosterone; BT: bioavailable testosterone
Relationship between total testosterone and characteristics of PCa
Patients diagnosed with PCa were separated according to their total testosterone levels based on a cut–off value of 350 ng/dL. No significant difference was found between the cut-off levels for testosterone among high-risk patients regarding Gleason scores, cancerous core involvement rates or the risk stratification according to D’amico criteria (p=0.830 in patients with a Gleason score ≥7, p=0.188 in patients with ≥50% cancerous core involvement of cancer and p=0.682 in high risk group defined by D’amico criteria, respectively) (Table 6 and 7).
Table 6.
Comparison of Gleason scores and core involvement rates with patients’ free and bioavailable testosterone levels divided by thresholds in PCa diagnosed group
| TT<350 | TT≥350 | p | FT≤5.5 | FT>5.5 | p | BT≤135 | BT>135 | p | |
|---|---|---|---|---|---|---|---|---|---|
| Gleason score <7 n (%) | 61 (76.5) | 56 (72.8) | 0.91 | 49 (69) | 76 (85.4) | 0.02 | 48 (62.4) | 69 (83.1) | 0.004 |
| Gleason score ≥7 n (%) | 22 (23.5) | 21 (27.2) | 22 (31) | 13 (14.6) | 29 (37.6) | 14 (16.9) | |||
|
| |||||||||
| Core involvement <50% n (%) | 73 (85.9) | 59 (78.7) | 0.29 | 51 (72.9) | 79 (87.8) | 0.02 | 55 (72.4) | 74 (88.1) | 0.016 |
| Core involvement 50% n (%) | 12 (14.1) | 16 (21.3) | 19 (27.1) | 11 (12.2) | 21 (27.6) | 10 (11.9) | |||
TT: total testosterone; FT: free testosterone; BT: bioavailable testosterone
Table 7.
Differentiating between low and high risk patients according to the D’Amico criteria by using thresholds for total, free and bioavailable testosterone levels
| TT<350 | TT≥350 | p | FT≤5.5 | FT>5.5 | p | BT≤135 | BT>135 | p | |
|---|---|---|---|---|---|---|---|---|---|
| Patients with benign, low–intermediate risk n (%) | 180 (84.9) | 161 (83.4) | 0.682 | 141 (77.5) | 199 (89.2) | 0.001 | 147 (75.4) | 190 (90) | 0.0002 |
| Patients with high risk n (%) | 32 (15.1) | 32 (16.6) | 41 (22.5) | 24 (10.8) | 47 (24.6) | 21 (10) |
TT: total testosterone; FT: free testosterone; BT: bioavailable testosterone
Relationship between free testosterone and characteristics of PCa
When patients were compared according to free testosterone levels with a cut-off of value of 5.5 ng/dL, high-risk PCa detection rates were significantly higher in those with lower free testosterone levels than those with higher [22.5% (n=41) vs. 10.8% (n=24), p=0.001] (Table 7). Similarly, patients with Gleason score of ≥7 were significantly more prevalent in the low free testosterone group than in the high testosterone group [31% (n=22) vs. 14.6% (n=13), p=0.02]. Moreover, patients with decreased free testosterone levels exhibited significantly higher rates of cancerous core involvement of ≥50% as compared to those with increased free testosterone levels [27.1% (n=19) vs. 12.2% (n=11), p=0.02] (Table 6).
Relationship between bioavailable testosterone and characteristics of PCa
When patients diagnosed with PCa were stratified based on a cut-off value for bioavailable testosterone levels as ≤135 and >135 ng/dL, patients with bioavailable testosterone levels below cut–off were more likely to be classified as high–risk according to D’Amico criteria compared to those with bioavailable testosterone levels higher than 135 ng/dL [24.6% (n=47) vs. 10% (n=21), p=0.0001] (Table 7). Based on Gleason scores and the percentage of cancerous cores, in patients with bioavailable testosterone levels of ≤135 ng/dl, significantly higher Gleason scores [37.6% (n=29) vs. 16.9% (n=14), p=0.04] and higher number of cancerous cores with ≥50% involvement were reported compared to those with bioavailable testosterone level of >135 ng/dL and higher rates for ≥50% of core involved with cancer [27.6% (n=21) vs. 11.9% (n=10), p=0.016] compared to those with bioavailable testosterone levels of >135 ng/dL (Table 6).
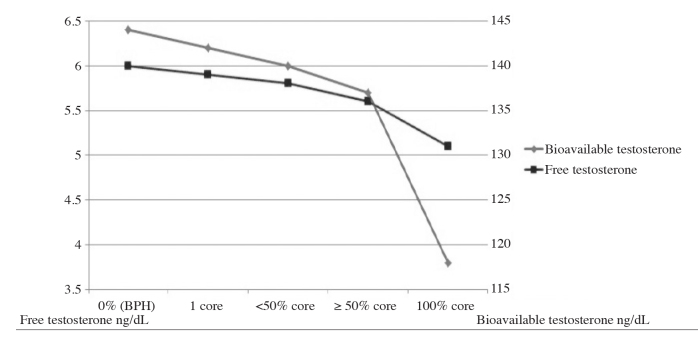
A negative correlation was found between increased rates of core involvement and lower free and bioavailable testosterone levels based on their cut-off levels (Figure 1).
Figure 1.
The relationship of free and bioavailable testosterone levels and the core involvement of PCa
Discussion
In this study, we evaluated total, free and bioavailable testosterone levels to predict the presence of PCa and its aggressiveness. Our results were based on the histology of TRUS-guided prostate needle biopsy specimens, and indicated a significant relationship between testosterone levels and PCa aggressiveness. Although the levels of total, free and bioavailable testosterone did not differ between patients with and without PCa, lower free and bioavailable testosterone levels were associated with the detection of high-grade cancer. Furthermore, when free and bioavailable testosterone levels were lower than 5.5 ng/dL for free and 135 ng/dL for bioavailable testosterone at the initial screening, both thresholds were likely to enhance the identification of men with high-risk PCa and Gleason score of ≥7. These thresholds were also correlated with aggressiveness evaluated based on the number of PCa cores with ≥50% involvement.
Our results revealed that using total testosterone levels alone for predicting these high-risk patients seems ineffective, because total testosterone levels were unable to reveal the presence of PCa and also to allow a risk stratification even in men with PSA level <10 ng/mL. Thereby, one of the main contribution of this study is that it has determined low-, and high-risk patients regardless of their PSA values.
As a matter of fact, the relationship between total testosterone levels and PCa is controversial. A broad review of the literature studies investigating this relationship was published by Klap et al.[21]. They selected 45 articles published between 1994–2004 referring to this relationship and found that 18 articles reported that Pca was related with low total testosterone, 17 articles implying an association with PCa and high total testosterone levels, and as in the current study in 10 articles any correlation could not be detected. In line with our results, previous evidence from Dai et al.[22] similarly revealed that patients’ preoperative total testosterone levels did not correlate with pathological tumor stage.
For years, it was believed that testosterone therapy for hypogonadal men and also higher total testosterone levels contribute to the development of PCa.[8,21,23–26] However, population-based studies which examined the association of high grade PCa with a long-term testosterone exposure were unable to find any relationship between testosterone therapy and the tumor aggressiveness.[27,28] Furthermore it has been shown that there is no significant causal or aggravating interaction between testosterone and PCa.[29]
Another study published by Hoffman et al showed the impact of the low free testosterone on the incidence of prostate cancer in hypogonadal men.[11] They found that in patients with low testosterone levels, an increased mean percent of biopsies indicated ther presence of cancer (43% vs. 22%, p=0.013) and an increased incidence of biopsy Gleason score of ≥8 (10.93% vs. 0%, p=0.025), comparing with patients having normal testosterone levels. In our study, we found no significant difference in free testosterone levels between patients with or without PCa. Therefore our results are in contrast with some of those studies, in which low total, free and bioavailable testosterone levels have been related to the presence of PCa.[4,11,12,15–17]
The major finding of our study is the presence of relationship between testosterone levels and tumor aggressivity. The reasons for the association between low serum testosterone and aggressiveness PCa are still under investigation. Presumably, higher grade and larger tumor volume due to increased metabolism and testosterone consumption reduces the serum free and bioavailable testosterone levels in patients with PCa.
Morgentaler et al.[30] described a saturation theory which explains this mechanism in a different way. In their saturation model, they observed that prostatic growth is extremely sensitive to low androgen levels which they call androgen dependent growth, but after a limit reached in serum androgen levels -determined as the saturation point-, this growth becomes androgen- independent.
The association between androgens and PCa aggressiveness may be also attributed to higher proportion of poorly differentiated cancer cells influenced by low androgen levels. A valuable data supporting this assumption has been reported by Song et al.[31], promising to explain the indicated relationship with an in vitro study. They demonstrated that low testosterone levels promote PCa proliferation whereas normal or higher testosterone levels show a dose-dependent inhibition.
Our results also indicated that at the time of the diagnosis, patients with free testosterone levels lower than 5.5 ng/dL were more likely to have higher Gleason scores and higher percentages of cores involved with cancer. In line with these results, a recent study from Germany by Schnoeller et al.[32] investigated the relationship between free and total testosterone levels and PCa in 137 patients who underwent radical prostatectomy. They reported that patients with low free testosterone levels (<0.047 mg/L) were associated with higher tumor stage (p=0.049) and higher rate of positive lymph node status (p=0.038) when compared with the patients with normal free testosterone levels. After the ROC analysis for the prognostic impact, they indicated the free testosterone levels as independent predictors of advanced disease.
Clinical impact of this relationship has been investigated by García-Cruz et al.[33]. Their retrospective study reported that lower total testosterone levels were poor prognostic factors for PCa and they were related to higher tumor burden, PCa bilaterality and higher D’Amico risk of progression. In our study, total testosterone levels did not differ between high-risk and low/intermediate risk groups (p=0.671), but according to D’Amico risk group classification high-risk patients had lower free and bioavailable testosterone levels than low-and intermediate risk patients.
Our study revealed the presence of a strong relationship between free and bioavaliable testosterone measurements with PCa aggressiveness, more significantly with bioavailable testosterone levels. The threshold of 5.5 ng/dL for free and 135 ng/dL for bioavailable testosterone levels seems to be appropriate to differentiate between high and low risk patients. Similar to our results, Léon et al demonstrated the relationship of total, free and bioavailable testosterone with tumor aggressiveness by using thresholds of 65 pg/mL for free and 1.5 ng/mL for bioavailable testosterone levels in patients who had undergone radical prostatectomy.[34] The preoperative total testosterone levels of their patients were not associated with aggressive PCa, however free and bioavailable testosterone levels were correlated with high-risk PCa.
The strengths of our study include its prospective design and evaluation of high number of patients with transrectal prostate biopsy results during pretreatment period. It was carried out at a single center with no discontinuity in recruitment, and all specimen evaluations were performed using a consistent method by a senior pathologist. All blood samples were drawn after an overnight fast between 7:00 AM and 10:00 AM to avoid a potential methodological flaw caused by different collection times and diurnal variation of the steroid hormones. A further strength is that we excluded patients using testosterone replacement therapy or 5-α reductase inhibitors or other drugs that alter prostate growth and PSA levels, and those with a history of prostatic surgery or radiotherapy, histopathology-proven diagnosis of atypical small acinar proliferation, high-grade prostatic intraepithelial neoplasia, or ductal adenocarcinoma.
Nevertheless, the present study has some limitations. First, our results indicating the association between lower testosterone levels and prediction of high–risk cancer only rely on histopathological examination of biopsy specimens and the final pathological results obtained from the RP specimens were not presented here. Histopathological analyses of biopsy specimens may not always predict the real aggressiveness of cancer. Collection of data from patients who underwent definitive therapies, is still in progress and intended to be presented in the near future. Second, the behavior of testosterone among men with PSA <2.5 ng/mL remains uncertain. As shown before, the risks of having a Gleason score of ≥7 are estimated to be 2%, 1% and 0.8% for PSA levels of 1.1–2, 0.6–1 and 0–0.5 ng/mL, respectively.[35] Therefore the effect of testosterone on the diagnosis of high risk patients with low PSA levels can be important. Third, we included all patients in our study without categorizing them based on hereditary factors. Finally, we did not use gas chromatography-mass spectrometry, which is considered gold standard for measuring circulating total testosterone levels.[35]
In conclusion, this prospective study demonstrated the presence of a significant relationship between free and bioavailable testosterone levels and PCa aggressiveness. Total, free and bioavailable testosterone measurements are not predictive for the diagnosis of PCa, but low free and bioavaliable testosterone levels are associated with advanced disease.
The results of this study may raise awareness to consider measuring free and bioavailable testosterone levels in addition to commonly used variables such as PSA, free PSA or DRE, before discussing the treatment alternatives with patients. Currently used PCa nomograms may be utilized in combination with free and bioavailable testosterone measurements at pretreatment. Nevertheless, such an advancement of nomograms using these variables remains to be investigated in multicenter clinical trials, conducted in different populations. The data gathered from these studies involving different subgroups of patients may help the researchers in the field. We hope that the outcomes of our prospective study would contribute to these efforts.
Footnotes
Ethics Committee Approval: Authors declared that the research was conducted according to the principles of the World Medical Association Declaration of Helsinki “Ethical Principles for Medical Research Involving Human Subjects”, (amended in October 2013).
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – M.Kendirci; Design – G.B., M.K., M.Kendirci; Supervision – M.Kendirci; Resources – G.B., H.Ş., M.A., A.Ö., O.T., M.K., M.Kendirci; Materials – G.B., H.Ş., M.A., A.Ö., O.T., M.K., M.Kendirci; Data Collection and/or Processing – G.B., H.Ş., M.A., A.Ö., M.K.; Analysis and/or Interpretation – M.K., G.B., M.Kendirci; Literature Search – G.B., M.K., H.Ş.; Writing Manuscript – M.K., H.Ş., M.Kendirci; Critical Review – M.Kendirci
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Isbarn H, Pinthus JH, Marks LS, Montorsi F, Morales A, Morgentaler A, et al. Testosterone and prostate cancer: revisiting old paradigms. Eur Urol. 2009;56:48–56. doi: 10.1016/j.eururo.2009.03.088. https://doi.org/10.1016/j.eururo.2009.03.088. [DOI] [PubMed] [Google Scholar]
- 2.Imamoto T, Suzuki H, Fukasawa S, Shimbo M, Inahara M, Komiya A, et al. Pretreatment serum testosterone level as a predictive factor of pathological stage in localized prostate cancer patients treated with radical prostatectomy. Eur Urol. 2005;47:308–12. doi: 10.1016/j.eururo.2004.11.003. https://doi.org/10.1016/j.eururo.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 3.Isom-Batz G, Bianco FJJ, Kattan MW, Mulhall JP, Lilja H, Eastham JA. Testosterone as a predictor of pathological stage in clinically localized prostate cancer. J Urol. 2005;173:1935–7. doi: 10.1097/01.ju.0000158040.33531.e7. https://doi.org/10.1097/01.ju.0000158040.33531.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schatzl G, Madersbacher S, Thurridl T, Waldmüller J, Kramer G, Haitel A, et al. High-grade prostate cancer is associated with low serum testosterone levels. Prostate. 2001;47:52–8. doi: 10.1002/pros.1046. https://doi.org/10.1002/pros.1046.abs. [DOI] [PubMed] [Google Scholar]
- 5.Huggins C, Hodges CV. Studies on prostatic cancer. I. The effect of castration, of estrogen and androgen injection on serum phosphatases in metastatic carcinoma of the prostate. Cancer Res. 1941;1:293–7. doi: 10.3322/canjclin.22.4.232. [DOI] [PubMed] [Google Scholar]
- 6.Grossmann M, Cheung AS, Zajac JD. Androgens and prostate cancer; pathogenesis and deprivation therapy. Best Pract Res Clin Endocrinol Metab. 2013;27:603–16. doi: 10.1016/j.beem.2013.05.001. https://doi.org/10.1016/j.beem.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 7.Khera M. Androgen replacement therapy after prostate cancer treatment. Curr Urol Rep. 2010;11:393–9. doi: 10.1007/s11934-010-0143-3. https://doi.org/10.1007/s11934-010-0143-3. [DOI] [PubMed] [Google Scholar]
- 8.Morgentaler A. Testosterone and prostate cancer: what are the risks for middle-aged men? Urol Clin North Am. 2011;38:119–24. doi: 10.1016/j.ucl.2011.02.002. https://doi.org/10.1016/j.ucl.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 9.Vander Heiden MG, Cantley LC, Thompson CB. Understanding the Warburg effect: the metabolic requirements of cell proliferation. Science. 2009;324:1029–33. doi: 10.1126/science.1160809. https://doi.org/10.1126/science.1160809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morgentaler A, Bruning CO, DeWolf WC. Occult prostate cancer in men with low serum testosterone levels. JAMA. 1996;276:1904–6. https://doi.org/10.1001/jama.276.23.1904. [PubMed] [Google Scholar]
- 11.Hoffman MA DW, Morgentaler A. Is low serum free testosterone a marker for high grade prostate cancer? J Urol. 2000;163:824–7. https://doi.org/10.1097/00005392-200003000-00027. [PubMed] [Google Scholar]
- 12.Massengill JC, Sun L, Moul JW, Wu H, McLeod DG, Amling C, et al. Pretreatment total testosterone level predicts pathological stage in patients with localized prostate cancer treated with radical prostatectomy. J Urol. 2003;169:1670–5. doi: 10.1097/01.ju.0000062674.43964.d0. https://doi.org/10.1097/01.ju.0000062674.43964.d0. [DOI] [PubMed] [Google Scholar]
- 13.Muller RL, Gerber L, Moreira DM, Andriole G, Castro-Santamaria R, Freedland SJ. Serum testosterone and dihydrotestosterone and prostate cancer risk in the placebo arm of the Reduction by Dutasteride of Prostate Cancer Events trial. Eur Urol. 2012;62:757–64. doi: 10.1016/j.eururo.2012.05.025. https://doi.org/10.1016/j.eururo.2012.05.025. [DOI] [PubMed] [Google Scholar]
- 14.Mearini L, Costantini E, Zucchi A, Mearini E, Bini V, Cottini E, et al. Testosterone levels in benign prostatic hypertrophy and prostate cancer. Urol Int. 2008;80:134–40. doi: 10.1159/000112602. https://doi.org/10.1159/000112602. [DOI] [PubMed] [Google Scholar]
- 15.Morgentaler A. Testosterone deficiency and prostate cancer: emerging recognition of an important and troubling relationship. Eur Urol. 2007;52:623–5. doi: 10.1016/j.eururo.2007.04.005. https://doi.org/10.1016/j.eururo.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 16.San Francisco IF, Regan MM, Dewolf WC, Olumi AF. Low age adjusted free testosterone levels correlate with poorly differentiated prostate cancer. J Urol. 2006;175:1341–5. doi: 10.1016/S0022-5347(05)00680-4. https://doi.org/10.1016/S0022-5347(05)00680-4. [DOI] [PubMed] [Google Scholar]
- 17.Teloken C, Da Ros CT, Caraver F, Weber FA, Cavalheiro AP, Graziottin TM. Low serum testosterone levels are associated with positive surgical margins in radical retropubic prostatectomy: hypogonadism represents bad prognosis in prostate cancer. J Urol. 2005;174:2178–80. doi: 10.1097/01.ju.0000181818.51977.29. https://doi.org/10.1097/01.ju.0000181818.51977.29. [DOI] [PubMed] [Google Scholar]
- 18.Ribeiro M, Ruff P, Falkson G. Low serum testosterone and a younger age predict for a poor outcome in metastatic prostate cancer. Am J Clin Oncol. 1997;20:605–8. doi: 10.1097/00000421-199712000-00015. https://doi.org/10.1097/00000421-199712000-00015. [DOI] [PubMed] [Google Scholar]
- 19.Wang C, Nieschlag E, Swerdloff R, Behre HM, Hellstrom WJ, Gooren LJ, et al. Investigation, treatment, and monitoring of late-onset hypogonadism in males: ISA, ISSAM, EAU, EAA, and ASA recommendations. Eur Urol. 2009;55:121–30. doi: 10.1016/j.eururo.2008.08.033. https://doi.org/10.1016/j.eururo.2008.08.033. [DOI] [PubMed] [Google Scholar]
- 20.D’Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Tomaszewski JE, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998;280:969–74. doi: 10.1001/jama.280.11.969. https://doi.org/10.1001/jama.280.11.969. [DOI] [PubMed] [Google Scholar]
- 21.Klap J, Schmid M, Loughlin KR. The relationship between total testosterone levels and prostate cancer: a review of the continuing controversy. J Urol. 2015;193:403–13. doi: 10.1016/j.juro.2014.07.123. https://doi.org/10.1016/j.juro.2014.07.123. [DOI] [PubMed] [Google Scholar]
- 22.Dai B, Qu Y, Kong Y, Ye D, Yao X, Zhang S, et al. Low pretreatment serum testosterone is associated with a high incidence of Gleason score 8–10 disease in prostatectomy specimen: data from ethnic Chinese patients with localized prostate cancer. BJU Int. 2012;110:E667–72. doi: 10.1111/j.1464-410X.2012.11465.x. https://doi.org/10.1111/j.1464-410X.2012.11465.x. [DOI] [PubMed] [Google Scholar]
- 23.Fowler JEJ, Whitmore WFJ. The response of metastatic adenocarcinoma of the prostate to exogenous testosterone. J Urol. 1981;126:372–5. doi: 10.1016/s0022-5347(17)54531-0. https://doi.org/10.1016/S0022-5347(17)54531-0. [DOI] [PubMed] [Google Scholar]
- 24.Morgentaler A. Testosterone replacement therapy and prostate cancer. Urol Clin North Am. 2007;34:555–63. doi: 10.1016/j.ucl.2007.08.002. https://doi.org/10.1016/j.ucl.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 25.Rhoden EL, Morgentaler A. Risks of testosterone-replacement therapy and recommendations for monitoring. N Engl J Med. 2004;350:482–92. doi: 10.1056/NEJMra022251. https://doi.org/10.1056/NEJMra022251. [DOI] [PubMed] [Google Scholar]
- 26.Klotz L. Testosterone therapy and prostate cancer--safety concerns are well founded. Nat Rev Urol. 2015;12:48–54. doi: 10.1038/nrurol.2014.338. https://doi.org/10.1038/nrurol.2014.338. [DOI] [PubMed] [Google Scholar]
- 27.Baillargeon J, Kuo YF, Fang X, Shahinian VB. Long-term Exposure to Testosterone Therapy and the Risk of High Grade Prostate Cancer. J Urol. 2015;194:1612–6. doi: 10.1016/j.juro.2015.05.099. https://doi.org/10.1016/j.juro.2015.05.099. [DOI] [PubMed] [Google Scholar]
- 28.Kaplan AL, Hu JC. Use of testosterone replacement therapy in the United States and its effect on subsequent prostate cancer outcomes. Urology. 2013;82:321–6. doi: 10.1016/j.urology.2013.03.049. https://doi.org/10.1016/j.urology.2013.03.049. [DOI] [PubMed] [Google Scholar]
- 29.Morgentaler A. Testosterone and prostate cancer: an historical perspective on a modern myth. Eur Urol. 2006;50:935–9. doi: 10.1016/j.eururo.2006.06.034. https://doi.org/10.1016/j.eururo.2006.06.034. [DOI] [PubMed] [Google Scholar]
- 30.Morgentaler A, Traish AM. Shifting the paradigm of testosterone and prostate cancer: the saturation model and the limits of androgen-dependent growth. Eur Urol. 2009;55:310–20. doi: 10.1016/j.eururo.2008.09.024. https://doi.org/10.1016/j.eururo.2008.09.024. [DOI] [PubMed] [Google Scholar]
- 31.Song W, Khera M. Physiological normal levels of androgen inhibit proliferation of prostate cancer cells in vitro. Asian J Androl. 2014;16:864–8. doi: 10.4103/1008-682X.129132. https://doi.org/10.4103/1008-682X.129132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schnoeller T, Jentzmik F, Rinnab L, Cronauer MV, Damjanoski I, Zengerling F, et al. Circulating free testosterone is an independent predictor of advanced disease in patients with clinically localized prostate cancer. World J Urol. 2013;31:253–9. doi: 10.1007/s00345-012-0902-5. https://doi.org/10.1007/s00345-012-0902-5. [DOI] [PubMed] [Google Scholar]
- 33.García-Cruz E, Piqueras M, Huguet J, Peri L, Izquierdo L, Musquera M, et al. Low testosterone levels are related to poor prognosis factors in men with prostate cancer prior to treatment. BJU Int. 2012;110:E541–6. doi: 10.1111/j.1464-410X.2012.11232.x. https://doi.org/10.1111/j.1464-410X.2012.11232.x. [DOI] [PubMed] [Google Scholar]
- 34.Leon P, Seisen T, Cussenot O, Drouin SJ, Cattarino S, Comperat E, et al. Low circulating free and bioavailable testosterone levels as predictors of high-grade tumors in patients undergoing radical prostatectomy for localized prostate cancer. Urol Oncol. 2015;33:384. doi: 10.1016/j.urolonc.2014.11.010. e21–7. https://doi.org/10.1016/j.urolonc.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 35.Huhtaniemi IT, Tajar A, Lee DM, O’Neill TW, Finn JD, Bartfai G, et al. Comparison of serum testosterone and estradiol measurements in 3174 European men using platform immunoassay and mass spectrometry; relevance for the diagnostics in aging men. Eur J Endocrinol. 2012;166:983–91. doi: 10.1530/EJE-11-1051. https://doi.org/10.1530/EJE-11-1051. [DOI] [PubMed] [Google Scholar]