Abstract
Objective
The incidence of ureteral stricture is showing a rising trend due to increased use of laparoscopic and upper urinary tract endoscopic procedures. Boari flap is the preferred method of repairing long- segment ureteral defects of 8–12 cm. The procedure has undergone change from classical open (transperitoneal and retroperitoneal) method to laparoscopic surgery and recently robotic surgery. Laparoscopic approach is cosmetically appealing, less morbid and with shorter hospital stay. In this case series, we report our experience of performing laparoscopic ureteral reimplantation with Boari flap in 3 patients.
Material and methods
This prospective study was conducted between January 2011 December 2014. The patients with a long- segment ureteral defect who had undergone laparoscopic Boari flap reconstruction were included in the study. Outcome of laparoscopic ureteral reimplantation with Boari flap for the manangement of long segment ureteral defect was evaluated.
Results
The procedure was performed on 3 patients, and male to female ratio was 1:2. One patient had bilateral and other two patient had left ureteral stricture. The mean length of ureteral stricture was 8.6 cm (range 8.2–9.2 cm). The mean operative time was 206 min (190 to 220 min). The average estimated blood loss was 100 mL (range 90–110 mL) and mean hospital stay was 6 days (range 5 to 7 days). The mean follow up was 19 months (range 17–22 months). None of the patients experienced any complication related to the procedure in perioperative period.
Conclusion
Laparoscopic ureteral reimplantation with Boari flap is safe, feasible and has excellent long term results. However, the procedure is technically challenging, requires extensive experience of intracorporeal suturing.
Keywords: Boari flap, laparoscopic, ureter
Indroduction
The incidence of ureteral stricture is rising due to increased use of laparoscopic and upper urinary tract endoscopic procedures.[1,2] Ureteral reimplantation with Boari flap has undergone change from classical open (transperitoneal and retroperitoneal) method to laparoscopic surgery and recently there are reports of robot-assisted laparoscopic repairs.[3,4] With increasing skills and availability of laparoscopic instruments, there are studies on managing long- segment ureteral stricture by laparoscopic reimplantation with Boari flap. However, the reconstruction is technically challenging and needs considerable expertise of intracorporeal suturing. This procedure is indicated for management of long -segment ureteral defect (≥8 cm). This approach is cosmetically appealing, less morbid with shorter hospital stay.
Material and methods
This prospective study was conducted between 1st January 2011 to 31st December 2014, in the department of Urology, King George’s Medical University situated in North India. Informed consent was obtained from all patients. A total of 3 patients with a long- segment ureteral defect (median, 8.6 cm; range 8.2–9.2 cm) who had undergone laparoscopic Boari flap reconstruction were included in the study. A detailed history and clinical examination was performed in all cases. Ultrasonographic examination of kidney, ureter and bladder (KUB) was done in all cases. Other imaging studies like intravenous urography (IVU) (n=3), and computed tomography urography (CTU) (n=2) were performed to delineate the site and length of ureteral stricture. In one patient with bilateral ureteral stricture had history of radical hysterectomy for cervical cancer. DTPA (diethylenetriaminepentaacetic acid) scan was done in all cases to assess the split renal function. Initially all patients had undergone percutaneous nephrostomy (PCN) and a nephrostogram was performed. Cystoscopy and retrograde ureterogram were performed before proceeding for reconstruction. At three months of follow up, a renal and bladder ultrasound, intravenous urography and DTPA scan were done. Resolution of hydronephrosis and unobstructed drainage were considered as successful outcome.
Surgical technique
All procedures were performed under general anaesthesia. Patient was placed in supine position with 45 degree tilt on the affected side. A 14 Fr Foley urethral catheter was inserted before the procedure. Transperitoneal approach was employed in all cases and all repair was done by a single urologist using three ports only. After creation of pneumoperitoneum, incision was made at white line of Toldt and colon was reflected medially. Ureter was identified and dissected caudally till the level of stricture. Ureter was handled meticulously with preservation of periureteral adventitia, and stenosed segment of ureter was resected. Ureteral cut end was then spatulated posteriorly at 6 O’ clock position for 2.5 cms. Bladder then distended with 300 mL of normal saline (0.9%) and all adhesions were cleared. On anterolateral bladder wall, a flap was raised with the base and tip being 4 and 3 cm in width respectively. The tip of the flap was localized just proximal to the bladder neck and its base at dome. Tension-free anastomosis of spatulated ureter and bladder flap was performed with 4-0 polyglactin sutures over a 6Fr/26 cm double J stent. Anastomosis was performed over double J stent in continous watertight fashion. Bladder was closed in a single layer with continuous sutures (Figure 1–6). A soft silastic tube drain was inserted into pelvis at the end of the procedure. Drain was removed after 48 hrs and double J stent after six weeks.
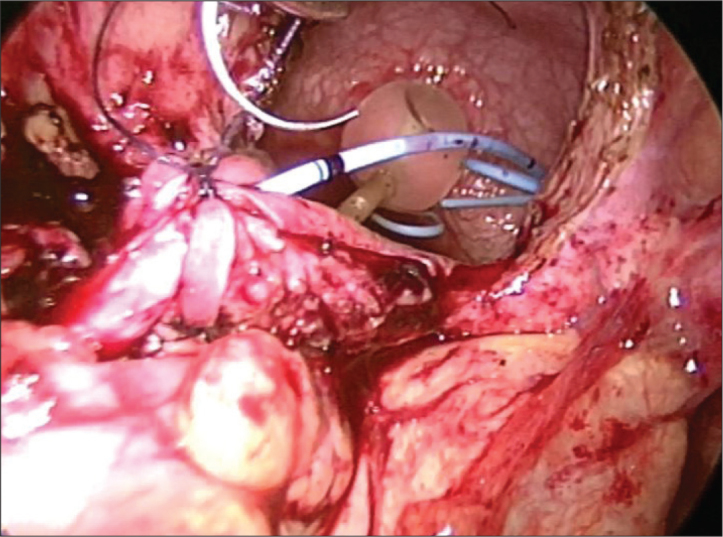
Figure 1.
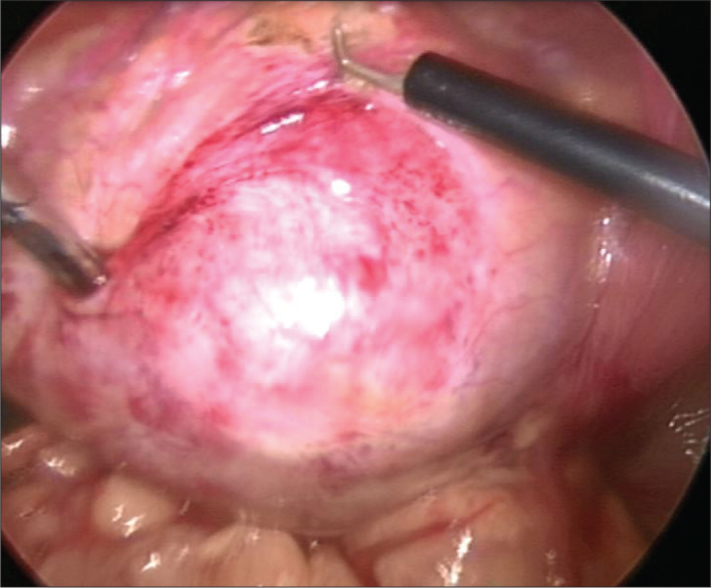
Preparing for Boari flap
Figure 2.
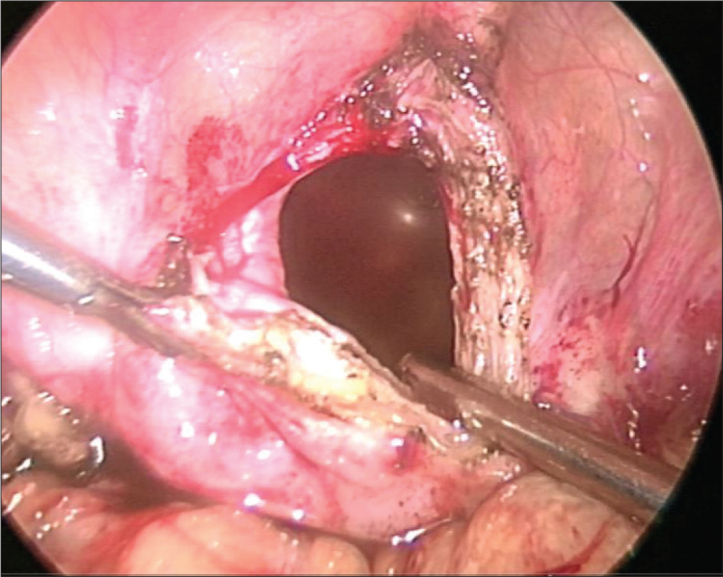
Elevating Boari flap
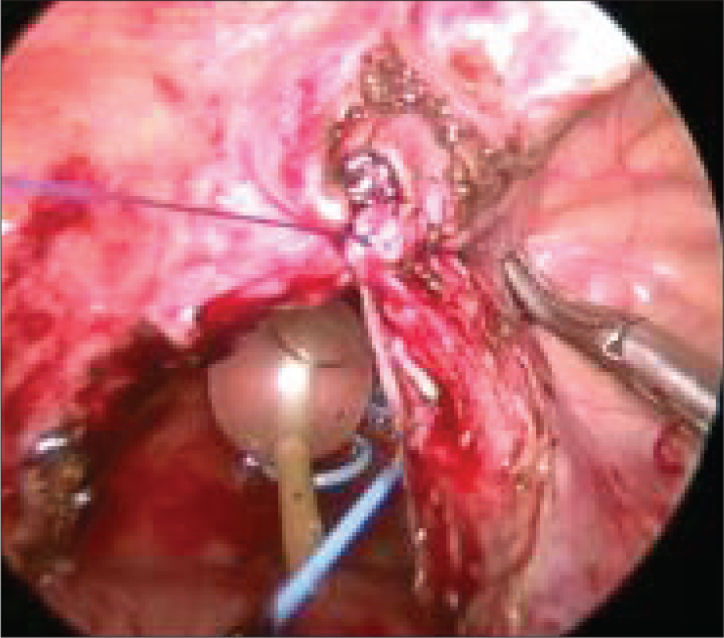
Figure 3.
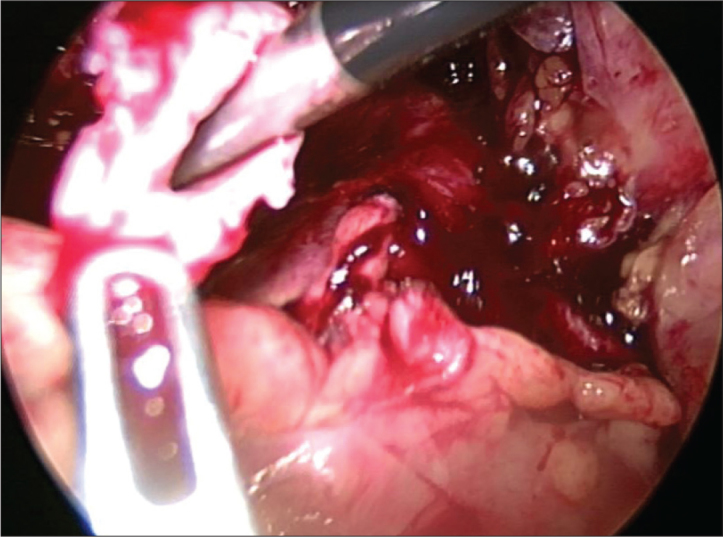
Spatulation of ureter
Figure 4.
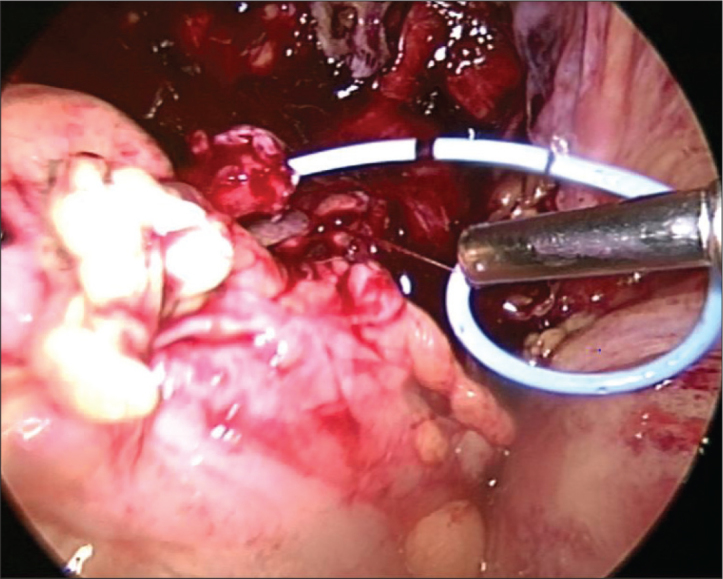
Antegrade placement of Double J stent
Figure 5.
Spatulated ureter anastomosed end- to- end with the apex of flap and flap being tubularised over double J stent
Figure 6.
Closure of bladder defect with continous vicryl suture
Results
A total of 3 patients underwent ureteral reconstruction. Demographic characteristics of the patients are shown in Table 1. The median age of the patients was 43.3 years (range 36 to 54 years) with male to female ratio of 1:2. The left side involvement was predominant (R:L, 1:2). The cause for ureteral defect was hysterectomy in 2 patients (66.6%), and colorectal surgery in one patient (33.33%). The median interval between injury and repair was 3 months (2–4 months). One patient had history of radical hysterectomy for carcinoma of cervix. She developed bilateral ureteral stricture following the procedure. She underwent right sided laparoscopic ureteroneocystostomy followed by laparoscopic ureteral reimplatation Boari flap on the contralateral side 3 months later. The median length of ureteral defect was 8.6 cm (range 8.2–9.2 cm). The median operative time was 206 min (range 190 to 220 min). The average estimated blood loss was 100 mL (range 90–110 mL) and the median hospital stay was 6 days (range 5 to 7 days). There were no intraoperative complications. Procedure was completed successfully in all three patients. None of the patients developed any postoperative complications. The median follow up was 19 months (17–22 months). Following stent removal, renal ultrasound showed resolution of hydronephrosis in all cases with unobstructed drainage pattern on DTPA scan. Periperative data is summarised in Table 2.
Table 1.
Baseline demographic and clinical data of the patients
| Parameters | Case 1 | Case 2 | Case 3 |
|---|---|---|---|
| Age (years) | 40 | 54 | 36 |
| BMI (kg/m2) | 25.2 | 26.5 | 3.2 |
| Sex (Male: female) | Female | Female | Male |
| Laterality | Left | Bilateral | Left |
| Ureteral defect (cm) | 9.2 | 8.4 | 8.2 |
| Interval between injury and operative intervention (months) | 2 | 3 | 4 |
| Serum creatinine (mg/dL) | 1.5 | 1 | 1.1 |
| Cause | Post-hysterectomy | Post-radical Hysterectomy | Post-colorectal surgery |
| Pre op PCN | PCN | Bilateral PCN | PCN |
BMI: body mass index; PCN: percutaneous nephrestomy
Table 2.
Perioperative data of patients
| Parameters | Case 1 | Case 2 | Case 3 |
|---|---|---|---|
| Operative time (min) | 190 | 220 | 210 |
| Blood loss (mL) | 90 | 110 | 100 |
| Time to drain removal (hours) | 48 | 48 | 48 |
| Hospital stay (days) | 6 | 7 | 5 |
| Pain score (VAS) at POD 1 | 3 | 3 | 3 |
| Analgesic requirement (Tramadol in mg) | 200 | 400 | 300 |
| Follow up (months) | 18 | 17 | 22 |
| Conversion to open | No | No | No |
| Post- Op US KUB | HDN resolved | HDN resolved | HDN resolved |
| DTPA Renal Scan | Non-Obstructive | Non-obstructive | Non-obstructive |
VAS: visual analogue scale; USG KUB: ultrasound kidney, ureter, bladder; DTPA: diethylenetriaminepentaacetic acid
Discussion
Boari described this method of ureteral reconstruction in 1894 in a canine model[4] and in human it was first described in 1947.[5] Open Boari flap procedures have good long-term results. However, open procedure is associated with excessive pain, longer hospital stay, and surgical scar. As the skill of the urologist is increasing in performing laparoscopic surgeries, there is a rapid transition from open to laparoscopic Boari flap reconstruction technique.
Fugita et al.[6] in 2001, first successfully performed laparoscopic reconstruction with Boari flap in three patients with long- segment ureteral stricture and concluded that the procedure is effective and feasible (Table 3).[3,6–17] Rassweiler et al.[7] observed longer operative time (253 minutes vs. 220 minutes), shorter hospital stay (8 days vs.17 day) with 100% successs rate in the laparoscopic group as compared with open ureteral reimplantation with Boari flap.
Table 3.
Literature review: reported series of laparoscopic ureteral reimplantation with Boari flap
| Authors | Cases (n) | Stricture length (cms) | Etiology | M/F | Side | OT Time (min) | Hospital stay (d) | Blood loss(ml) | F-up (mo) | Analgeic requirement |
|---|---|---|---|---|---|---|---|---|---|---|
| Fergany et al.[10] | 6 pigs | 140 | ||||||||
|
| ||||||||||
| Fugita et al.[6] | 3 | 6.6 | 1M | 1 R | ||||||
| 2 F | 2 L | 220 | 6.3 | 470 | 11 | 45 g morphine | ||||
|
| ||||||||||
| Castillo et al.[9] | 9 | 4–7 | 8US | 156 | 3 | 124 | 17.6 | 32 mg morphine | ||
| 1 UT | ||||||||||
|
| ||||||||||
| Modi et al.[11] | 1 | 210 | 3 | 90 | 50 mg morphine | |||||
|
| ||||||||||
| Rasweiler et al.[7] | 4 | 2M | 3 R | 254 | 8.2 | 270 | 4.9 mg piritramide | |||
| 2 F | 1 L | |||||||||
|
| ||||||||||
| Basiri et al.[12] | 1 | UT | M | L | 406 | 5 | 300 | |||
|
| ||||||||||
| Nerli et al.[13] | 1 | 5 | H | F | L | 160 | ||||
|
| ||||||||||
| Ramalingam et al.[8] | 3 | 8 | POM | 1 M | 3 R | 320 | 100 | 6m–3yrs | ||
| US | 2 F | |||||||||
|
| ||||||||||
| Symons et al.[14] | 3 | 5.6 | US | 3 M | 1R | 307 | 7.3 | 0.8 g/dl | 5 | 175 mg diclofenac |
| 2 L | Hb drop | 150 mg tramadol | ||||||||
|
| ||||||||||
| Schimpf and Wegner[3] | 2 RALBF | US | 1 F | R | 172 | 2 | 0 | 12 | ||
| UT | 1 M | 224 | 5 | 200 | 4 | |||||
|
| ||||||||||
| Allarpathi et al.[15] | 2 RALBF | UT | 1 M | 2R | 245 | 2 | 30 | 6 | 22 mg morphine | |
| 1F | ||||||||||
|
| ||||||||||
| Soares et al.[16] | 2 | H | 2F | 1R | ||||||
| US | 1L | 120 | 2 | 140 | 6 | |||||
|
| ||||||||||
| Gozen et al.[17] | 9 | US | 247.4 | 8 | 283 | 35 | ||||
M: male; F: female; R: right; L: left; RALBF: robot-assisted laparoscopic reimplantation withBoari flap; US: ureteral stricture; UT: ureteral tumor; H: hysterectomy; min: minute; d: days; mo: months; F-up: follow up; yrs: years
Ramalingam et al.[8] performed laparoscopic ureteral reimplantation with Boari flap in 3 patients successfully with median operative time of 320 mins (range 300–320 min). Castillo et al.[9] reported 9 cases of laparoscopic reimplantation procedure with Boari flap. In their study, median operative time was 156 mins, median hospital stay was 3 days and median length of follow- up was 17.6 months. Abraham et al.[18] reported comparable results between early and delayed repair with Boari flap, however early repair is challenging. Schimpf and Wagner[3] performed first robotic Boari flap procedure. The operative time was 172 minutes, with hospital stay of 2 days with 12 months of follow-up without any evidence of recurrence of stricture. Robotic surgery may make this procedure easier with better vision and dexterity during suturing. However, this approach has major limitations in terms of high cost, limited availability and inexperience of most of the surgeons worldwide. The present study is a prospective study which comprised 3 patients with median stricture length of 8.6 cm (range 8.2–9.2 cm), the median operative time of 206 min (range 190–220 min), median hospital stay of 6 days (range 5–7 days), and median follow up of 19 months (17–22 months) with 100% the success rate. These results are comparable to the literature findings. The interesting part of our study is pain scoring (VAS) done on the first postoperative day (POD1) and analgesic requirement. The median pain score was 3.33 (range 3–4) and the mean analgesic requirement was 300 mg of tramadol (200–400 mg). These findings are also comparable to the literature data. One patient had bilateral ureteral stricture developed following radical hysterectomy. In this patient laparoscopic ureteroneocystomy was performed first on one side and then laparoscopic reconstruction with Boari flap was performed on the contralateral side after 3 months with excellent results.
Laparoscopic reimplantation with Boari flap is a safe, feasible and less morbid procedure for the management of long- segment ureteral defects. However, the reconstruction is technically challenging and require extensive intracorporeal suturing. This surgical approach provides obvious advantage to the patient in terms of cosmesis and decreased morbidity.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of King George’s Medical University.
Informed Consent: Written informed consent was obtained from all individuals who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – A.J, R.J.S., A.B.; Design – A.J., R.J.S., A.B.; Supervision – A.B., G.P., B.P., V.S.; Resources – A.J., R.J.S., A.B., V.S.; Materials – A.B., G.P., B.P., V.S.; Data Collection and/or Processing – A.J., R.J.S., A.B., G.P., B.P., V.S.; Analysis and/or Interpretation – A.J., R.J.S., A.B., G.P., B.P., V.S.; Literature Search – A.J., R.J.S., A.B., G.P., B.P., V.S.; Writing Manuscript – A.J., R.J.S., A.B., G.P., B.P., V.S.; Critical Review – A.J., R.J.S., A.B., G.P., B.P., V.S.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Grainger DA, Soderstrom RM, Schiff SF, Glickman MG, DeCherney AH, Diamond MP. Ureteral injuries at laparoscopy: Insight into diagnosis, management, and prevention. Obstet Gynecol. 1990;75:839–43. https://doi.org/10.1016/0020-7292(90)90558-3. [PubMed] [Google Scholar]
- 2.Smith A. Management of iatrogenic ureteral strictures after urological procedures. J Urol. 1988;140:1372–4. doi: 10.1016/s0022-5347(17)42048-9. https://doi.org/10.1016/S0022-5347(17)42048-9. [DOI] [PubMed] [Google Scholar]
- 3.Schimpf MO, Wagner JR. Robot assisted laparoscopic Boari flap ureteral reimplantation. J Endourol. 2008;22:2691–4. doi: 10.1089/end.2008.0166. https://doi.org/10.1089/end.2008.0166. [DOI] [PubMed] [Google Scholar]
- 4.Casati E, Boari A. A contribution to the experimental plastic surgery of ureter. Atti Acad Med Natl. 1894;14:149. [Google Scholar]
- 5.Ockerblad NF. Reimplantation of the ureter into the bladder by a flap method. J Urol. 1947;57:845–7. doi: 10.1016/S0022-5347(17)69714-3. https://doi.org/10.1016/S0022-5347(17)69714-3. [DOI] [PubMed] [Google Scholar]
- 6.Fugita OE, Dinlenc C, Kavoussi L. The laparoscopic Boari flap. J Urol. 2001;166:51–3. https://doi.org/10.1016/S0022-5347(05)66074-0. [PubMed] [Google Scholar]
- 7.Rassweiler JJ, Gozen AS, Erdogru T, Sugiono M, Teber D. Ureteral reimplantation for management of ureteralstrictures: a retrospective comparison of laparoscopic and open techniques. Eur Urol. 2007;51:512–22. doi: 10.1016/j.eururo.2006.08.004. https://doi.org/10.1016/j.eururo.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 8.Ramalingam M, Senthil K, Ganapathy M. Laparoscopic Boari Flap Repair: Report of 3 cases. J Laparoendosc Adv Surg Tech A. 2008;18:271–5. doi: 10.1089/lap.2007.0025. https://doi.org/10.1089/lap.2007.0025. [DOI] [PubMed] [Google Scholar]
- 9.Castillo OA, Litvak JP, Kerkebe M, Olivares R, Urena RD. Early experience with the laparoscopic boari flap at a single institution. J Urol. 2005;173:862–5. doi: 10.1097/01.ju.0000152157.25984.ae. https://doi.org/10.1097/01.ju.0000152157.25984.ae. [DOI] [PubMed] [Google Scholar]
- 10.Fergany A, Gill IS, Abdel-Samee A, Kaouk J, Meraney A, Sung G. Laparoscopic bladder flap ureteral reimplantation: survival porcine study. J Urol. 2001;166:1920–3. https://doi.org/10.1097/00005392-200111000-00084. [PubMed] [Google Scholar]
- 11.Modi P, Goel R, Dodia S, Devra A. Case report: laparoscopic Boari flap. J Endourol. 2006;20:642–5. doi: 10.1089/end.2006.20.642. https://doi.org/10.1089/end.2006.20.642. [DOI] [PubMed] [Google Scholar]
- 12.Basiri A, Karami H, Mehrabi S, Javaherforooshzadeh A. Laparoscopic distal ureterectomy and Boari flap ureteroneocystostomy for a low-grade distal ureteral tumor. Urol J. 2008;5:120–2. [PubMed] [Google Scholar]
- 13.Nerli RB, Reddy MR, Ravish IR, Amarkhed SS. Laparoscopic bladder (Boari) flap ureteroneocystostomy. J Multidiscip Healthc. 2008;1:15–6. [PMC free article] [PubMed] [Google Scholar]
- 14.Symons S, Kurien A, Desai M. Laparoscopic ureteral reimplantation: a single center experience and literature review. J Endourol. 2009;23:269–74. doi: 10.1089/end.2008.0266. https://doi.org/10.1089/end.2008.0266. [DOI] [PubMed] [Google Scholar]
- 15.Allaparthi S, Ramanathan R, Balaji KC. Robotic distal ureterectomy with boari flap reconstruction for distal ureteral urothelial cancers: a single institutional pilot experience. J Laparoendosc Adv Surg Tech A. 2010;20:165–71. doi: 10.1089/lap.2009.0269. https://doi.org/10.1089/lap.2009.0269. [DOI] [PubMed] [Google Scholar]
- 16.Soares RS, Abreu RA, Jr, Tavora JE. Laparoscopic ureteral reimplant for ureteral stricture. International Braz J Urol. 2010;36:38–43. doi: 10.1590/s1677-55382010000100006. https://doi.org/10.1590/S1677-55382010000100006. [DOI] [PubMed] [Google Scholar]
- 17.Gözen AS, Cresswell J, Canda AE, Ganta S, Rassweiler J, Teber D. Laparoscopic ureteral reimplantation: prospective evaluation of medium-term results and current developments. World J Urol. 2010;28:221–6. doi: 10.1007/s00345-009-0443-8. https://doi.org/10.1007/s00345-009-0443-8. [DOI] [PubMed] [Google Scholar]
- 18.Abraham GP, Das K, Ramaswami K, George DP, Abraham JJ, Thachil T. Laparoscopic reconstruction of iatrogenic-induced lower ureteric strictures: Does timing of repair influence the outcome? Indian J Urol. 2011;27:465–9. doi: 10.4103/0970-1591.91433. https://doi.org/10.4103/0970-1591.91433. [DOI] [PMC free article] [PubMed] [Google Scholar]


