Abstract
Background
Penile plication techniques with or without degloving offer a minimally invasive option for the treatment of penile curvature.
Aim
To review the outcomes of penile plication surgery and patient satisfaction with and without degloving of the penis.
Methods
We conducted a retrospective analysis of 52 patients who underwent penile plication for the treatment of Peyronie disease or congenital penile curvature.
Outcomes
Surgical success rates, complications, and patient satisfaction determined with the Treatment Benefit Scale were compared between groups.
Results
The overall surgical success rate was 92.3% at a mean follow-up of 18.84 ± 23.51 months. There were no intraoperative complications. In the degloving group, 42.6% of patients were greatly satisfied and 42.6% had better outcomes; in the without degloving group, 61.5% of patients were greatly satisfied and 30.8% had better outcomes. Comparison of outcomes was not statistically significant between groups.
Clinical Implications
The results of the present study indicate the two techniques can be used for penile plication.
Conclusion
With or without degloving, penile plication is safe and effective and provides high patient satisfaction.
Kadirov R, Coskun B, Kaygisiz O, et al. Penile Plication With or Without Degloving of the Penis Results in Similar Outcomes. Sex Med 2017;5:e142–e147.
Key Words: Penile Plication, Peyronie's Disease, Congenital Penile Curvature, Degloving
Introduction
Congenital penile curvature and Peyronie's Disease (PD) represent two separate forms of penile curvature deformities. PD is more common than congenital curvature and its prevalence is 0.4% to 9%.1 An acute inflammatory process is present at the initial stage of the disease, which eventually leads to progression in 30% to 50% of patients.These conditions can be stressful and have negative effects on quality of life.2, 3
Surgical correction of the curvature is indicated when the curvature inhibits vaginal penetration or erectile dysfunction is severe.2, 4
The main objective of surgery is to correct the penile deformity. To minimize the risk of recurrence, the operation should be postponed until the plaque is mature and the curvature is stabilized. Although the optimal length of this delay is not clear, at least 3 months after stabilization of the deformity has been suggested by European Urological Association guidelines.2
The surgical techniques can be reviewed in three categories: tunica shortening procedures, tunica lengthening procedures, and penile prosthesis placement.5 Tunica shortening procedures, especially plication techniques, are the recommended first choice. Tunica lengthening procedures are recommended for a high degree of curvature. Penile prosthesis implantation remains the last resort for patients with erectile dysfunction who do not respond to pharmacologic therapy.2
Currently, penile plication is the most preferred surgical option for the appropriate patients.6 The best candidates for tunic shortening procedures have adequate erectile function and penile length (>13 cm). They should have a penile curvature less than 60° and a predicted shortening of 20% of the penis.5
Common complications after penile plication are shortening of penile length (18–75%), recurrence of curvature (0–20%), residual penile curvature, erectile dysfunction, numbness at the penis (60–75%), penile pain, or a palpable suture (50–100%). These complications are well tolerated by patients and good satisfaction rates are achieved.7, 8, 9, 10, 11
In most plication techniques, degloving (DG) of the penis is a standard stage of the surgery as described by many investigators.12 Less commonly, some perform penile plication without degloving (WDG) of the penis.9, 13, 14
In this study we reviewed the outcomes of penile plication surgery and patient satisfaction in our center. Furthermore, we reviewed the outcomes of penile plication in patients with DG and WDG.
Methods
After approval from the local ethical committee, the data of 52 patients who underwent penile plication from 2008 through 2016 were reviewed. These patients had a diagnosis of PD or congenital penile curvature. The preoperative data and operative outcomes were retrieved from the patients' charts.
A penile curvature angle greater than 30°, the ability to achieve an erection, and difficulty in vaginal penetration were the indications for penile plication surgery. Patients without at least 3-month follow-up were not included in this study.
The demographic characteristics of patients, the direction of curvature and its degree of angulation, the five-item International Erectile Function Index (IIEF-5) score, presence of plaque formation at physical examination, length of operation, length of hospital stay, and complications were recorded.
Patient satisfaction in correction of penile curvature and erectile function was assessed with the Treatment Benefit Scale (TBS). Patients were asked to reply to a single question during a telephone interview. Patients replied to the question “How do you describe your current condition when compared to preoperative condition” with one of the following scores: 1 = greatly improved, 2 = improved, 3 = did not change, and 4 = worse than before. The TBS was originally developed to compare overactive bladder symptoms before and after surgery.15
The DG plication technique is described elsewhere.16
WDG Plication Technique
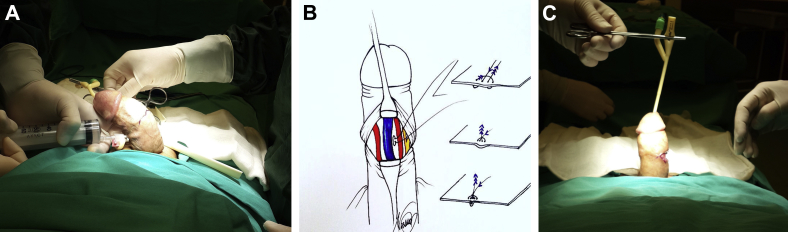
The surgical procedure was performed under general anesthesia. A 16-Fr silicone Foley catheter was inserted to locate the urethra and avoid any damage during dissections. To determine the localization of the curvature, an artificial erection was obtained by inserting a 20-gauge needle into the corpus cavernosum. The base of the penis was blocked with a tourniquet before administering saline solution. The site of maximum curvature was marked transversely (Figure 1A). A 2-cm-long transverse incision was performed and the dissection continued to expose the tunica albuginea. For ventral curvatures, the neurovascular bundle was marked with a pen to avoid suture damage to these structures. In addition, 2-0 non-absorbable sutures (Prolene, Ethicon, Somerville, NJ, USA) were used in an inverting and interrupting fashion for the tunica albuginea of the corpus cavernosa (Figure 1B). Each suture crossed a length of 15 mm and involved two needle passages covering approximately 7 mm with a 1-mm gap between sutures. All sutures were tied at the time of placement. Each plication suture was assumed to correct 5° of curvature as reported previously.14, 17 After placement of plication sutures, an artificial erection was produced to check for proper correction (Figure 1C). After closing the Buck fascia over the sutures, the incision was closed and an elastic bandage was maintained for 2 days.
Figure 1.
Panel A shows the marking of the maximum curvature site after an artificial erection. Panel B shows suture placement for ventral curvatures. The neurovascular bundle is identified and the 2-0 non-absorbable suture is passed between the dorsal vein and the neurovascular bundle in an inverted fashion. Panel C shows an artificial erection used to check for proper correction of the curvature.
Statistical Analysis
Statistical analysis was performed with SPSS 23.0 (SPSS, Inc, Chicago, IL, USA). The variables were compared according to groups. The Shapiro-Wilk test was applied to test the normality of continuous variables. Normally distributed variables were presented as mean ± SD and compared using Student t-test. Non-normally distributed variables were presented as median (minimum to maximum) and compared using the Mann-Whitney U-test. Nominal data were presented as number or percentage and compared using the χ2 test and Fisher exact test. A P value less than .05 was considered statistically significant.
Results
The mean age the 52 patients was 48.09 ± 17 years. Twenty-six patients underwent the DG procedure and 26 patients underwent the WDG technique. The diagnosis was PD in 40 patients and congenital penile curvature in 12. Preoperative characteristics of the patients are presented in Table 1. The two groups were similar in age; etiology, direction, and degree of curvature; presence of plaque; and IIEF scores.
Table 1.
Comparison of preoperative characteristics of patients with and without degloving
| With degloving (n = 26) | Without degloving (n = 26) | P value | |
|---|---|---|---|
| Age (y), mean ± SD | 47.84 ± 18.48 | 48.34 ± 17.51 | .922 |
| Direction of curvature, n (%) | .625 | ||
| Dorsal | 3 (11.5) | 2 (7.7) | |
| Lateral | 5 (19.2) | 8 (30.8) | |
| Ventral | 11 (47.8) | 12 (52.2) | |
| Combined | 7 (26.9) | 4 (15.4) | |
| Preoperative angulation (°), mean ± SD | 36.73 ± 6.47 | 38.07 ± 10.68 | .588 |
| Preoperative IIEF-5 score, mean ± SD | 17.69 ± 4.82 | 16.46 ± 4.34 | .338 |
| Preoperative erectile dysfunction, n (%) | 17 (65.40) | 13 (48.10) | .323 |
IIEF-5 = five-item International Index of Erectile Function.
The mean length of the operation was 61.73 ± 20.63 minutes in the DG group and 55.46 ± 30.29 in the WDG group. There was no statistically significant difference between groups (P = .387). The mean length of hospital stay was 3.07 ± 0.97 and 2.88 ± 2.00 days in groups DG and WDG, respectively (P = .662). There were no complications during surgery or the early postoperative period in either group.
The mean follow-up was 18.84 ± 23.51 months. Overall, the surgical success rate was 92.3%. Comparison of outcomes and long-term complications is presented in Table 2. There was no significant difference in recurrence rates, mean change in angulation, and complications. One patient (3.8%) in the DG group and three patients (11.8%) in the WDG group underwent reoperation because of insufficient surgical correction (P = .610).
Table 2.
Comparison of outcomes of patients with and without degloving
| With degloving (n = 26) | Without degloving (n = 26) | P value | |
|---|---|---|---|
| Change in angulation (°), mean ± SD | 28.84 ± 6.82 | 30.00 ± 9.48 | .617 |
| Palpation of sutures, n (%) | 6 (23.1) | 4 (15.4) | .726 |
| Penile shortening (cm), median (range) | 0 (0–3) | 0 (0–1) | .481 |
| Postoperative IEFF-5 scores, mean ± SD | 17.65 ± 4.90 | 17.03 ± 4.35 | .635 |
IIEF-5 = five-item International Index of Erectile Function.
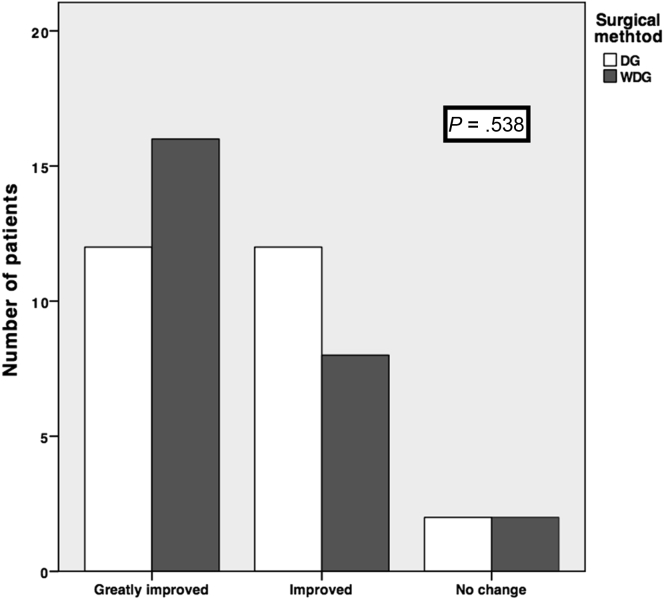
In the DG group, 42.6% of patients were greatly satisfied, 42.6% reported better outcomes, and 7.7% declared no changed according to the TBS score for the evaluation of satisfaction for correction of the curvature. In the WDG group, 61.5% of patients were greatly satisfied, 30.8% reported better outcomes, and 7.7% declared no changed with the TBS score for the evaluation of satisfaction for correction of the curvature (P = .538; Figure 2).
Figure 2.
Comparison of patient satisfaction regarding correction of curvature between groups. DG = degloving; WDG = without degloving.
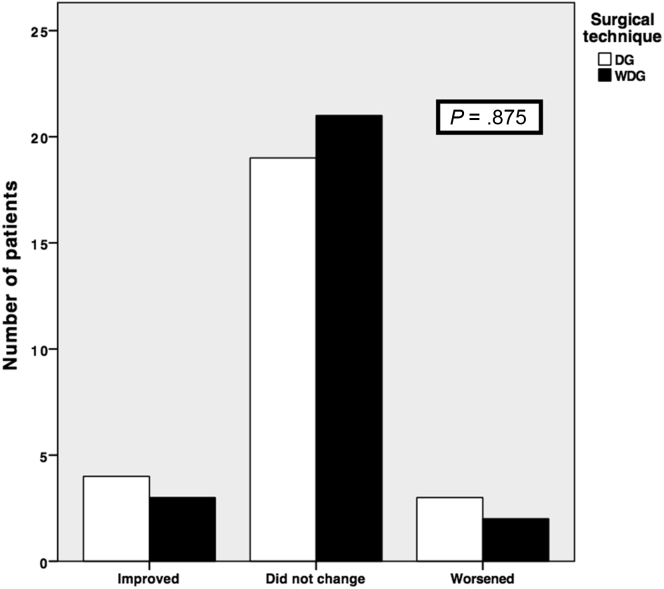
When satisfaction with erectile function after surgery was reviewed with the TBS score in the DG group, 73.1% of patients reported no change, 15.4% declared better erectile function, and 11.5% reported worse outcomes; in the WDG group, 80.8% of patients reported no change, 13.5% declared better erectile function, and 9.6% reported worse outcomes (P = .875; Figure 3).
Figure 3.
Comparison of patient satisfaction regarding erectile function after surgery between groups. DG = degloving; WDG = without degloving.
Discussion
Numerous surgical techniques have been developed for the correction of penile curvature disorders.5, 12 The decision for active treatment depends on the age of the patient, the degree and direction of the curvature, erectile function, degree of pain during erections, sexual satisfaction, ability for vaginal penetration, cosmetic concerns, and maturation of the plaque. Patients with good erectile function and mild degrees of curvature do not need treatment. Surgery should be planned 1 year after the emergence of symptoms and the patient should have stable symptoms for at least 3 months.2 In our series, 69.2% of patients received medical treatment during the active phase of the disease and all patients underwent surgery after a symptom-free period of 3 months.
Currently, penile plication surgeries are common for the correction of penile curvature disorders. In a recent survey carried out in Korea, 84% of urologists reported that they choose penile plication surgery as the first option.18 This technique is much easier and minimally invasive compared with other surgical techniques.4
In our series, sufficient correction of angulation was achieved in 48 of 52 patients (92.3%). The success rates of penile plication surgeries reported in other series are 58% to 100%.4, 9, 10, 11, 13, 14 It is critically important to achieve patient satisfaction and provide good surgical correction. Complications such as shortening of the penis, palpation of the sutures, and de novo erectile dysfunction can be bothersome for patients. The rate of patient satisfaction after plication surgeries has been reported at 62% to 96% in the literature.7, 19, 20, 21, 22 In our study, patient satisfaction was evaluated with the TBS. It was originally developed to determine satisfaction after treatment of overactive bladder.15 The TBS is a single question with four possible answers: great improvement, improvement, no change, and worse than before. The great majority of patients in the two groups were satisfied with the correction of the curvature (92.3%). Although the rate of great improvement was more predominant in the WDG group, this was statistically insignificant (P = .538; Figure 2).
There are limited data regarding the outcomes of the WDG technique in the literature. Dugi and Morey13 reported a success rate of 93% after penoscrotal plication WDG in 48 men at the University of Texas Southwestern Medical Center. This technique was performed in patients with dorsal and/or lateral curvature and no major complication was reported. Two years later, the outcomes of this technique were reported from the same center for 102 patients with severe and/or biplanar penile curvature with similar success rates. Only 4% of patients had reoperations because of insufficient correction and 4% had penile prosthesis placement because of progression of PD.14 Recently, Chung et al9 reported an overall satisfaction rate of 94% to 100% in patients with dorsal, ventral, lateral, or combined curvature, which was determined with the Patient Global Impression of Improvement. The satisfaction rates were found to be similar for direction of the curvature. Although high satisfaction rates have been reported with penile plication surgery, in a very recent study, Baldini et al7 reported a satisfaction rate of 57.5%, a dissatisfaction rate of 25%, and no opinion in 17.5% after various types of plication surgeries. Furthermore, in their study, 65% of patients reported some degree of worsening of their sexual life compared with their preoperative condition. They speculated the loss of penile length and involuntary vaginal exits were responsible for the dissatisfaction.
The shortening of penile length is another disadvantage of penile plication surgeries. Although the rate of loss in penile length is variable in the literature (5–80%), it is commonly well tolerated in selected patients.7 The risk of penile shortening is more common for patients with a curvature greater than 60°. Also, penile plication should not be recommended to patients with insufficient penile length.2 In the present study, the change in penile length was evaluated subjectively. Although 61.5% of patients stated no change in penile length, 0.5- and 1-cm shortenings were reported by 13.5% and 15% of patients, respectively. Furthermore, there was no significant difference in the DG and WDG groups.
Similarly, Li et al10 reported 40% shortening in their patients. Gholami and Lue20 reported penile shortening of 0.5 to 1.5 cm in 41% of 132 patients. However, this condition created dysfunction in only 7% of patients.
De novo erectile dysfunction is a potential complication of penile plication surgeries. Excision and grafting produce greater risk of de novo erectile dysfunction compared with plication surgeries. The neurovascular bundle can be injured during surgeries involving the dorsal side of the penis. In our clinical practice, we always mark the neurovascular bundle before inserting the correction sutures. The WDG technique carries no risk for identification of the neurovascular bundle. In this technique, the transverse incision is followed by meticulous retraction of the overlying fascia on the tunica albuginea, which allows good exposure.
In our series, there were no changes in IIEF-5 scores postoperatively compared with preoperative scores (17.34 ± 4.60 and 17.07 ± 4.58, respectively, P = .223). Furthermore, the TBS score showed no change in 76.9%, better erectile function in 13.5%, and worsened erectile function in 9.6% of patients. For patients with worsened erectile function, we speculate the natural course of PD could have played a role.
The ideal type of suture material for penile plication is not clear.4 Non-absorbable sutures are useful for avoiding recurrence. However, the sutures can be felt by the patients. Conversely, use of an absorbable suture can result in early recurrence.23 In the present study, we used only non-absorbable sutures and 15.4% of patients reported discomfort with palpation of the sutures.
In our opinion, the WDG technique resulted in a better cosmetic appearance compared with the DG technique, although we did not ask about this specific issue. Other aspects, including operative and functional outcomes, were similar for the two techniques. Although the limited number of patients in the two groups might not be sufficient to draw a conclusion, the DG technique did not provide additional benefits over the WDG technique.
Conclusion
Penile plication with or without degloving is safe and effective for the treatment of congenital penile curvature or PD with penile curvature. There is minimal shortening of the penis and the risk of de novo erectile dysfunction is minimal. The outcomes of the DG and WDG techniques were similar in operative results and patient outcomes. Prospective studies with more patients would be useful to determine more accurate results.
Statement of authorship
Category 1
-
(a)Conception and Design
- Hakan Kilicarslan
-
(b)Acquisition of Data
- Rustam Kadirov; Burhan Coskun; Onur Kaygisiz; Hakan Kilicarslan
-
(c)Analysis and Interpretation of Data
- Rustam Kadirov; Burhan Coskun; Yakup Kordan; Ismet Yavascaoglu; Hakan Kilicarslan
Category 2
-
(a)Drafting the Article
- Rustam Kadirov; Burhan Coskun; Hakan Kilicarslan
-
(b)Revising It for Intellectual Content
- Rustam Kadirov; Burhan Coskun; Onur Kaygisiz; Kadir Omur Gunseren; Yakup Kordan; Ismet Yavascaoglu; Hakan Kilicarslan
Category 3
-
(a)Final Approval of the Completed Article
- Rustam Kadirov; Burhan Coskun; Onur Kaygisiz; Kadir Omur Gunseren; Yakup Kordan; Ismet Yavascaoglu; Hakan Kilicarslan
Acknowledgments
We thank Neslihan Ozge Ozbey (third-year medical student) very much for drawing the illustration in Figure 1B.
Footnotes
Conflicts of Interest: The authors report no conflicts of interest.
Funding: None.
References
- 1.Sommer F., Schwarzer U., Wassmer G. Epidemiology of Peyronie's disease. Int J Impot Res. 2002;14:379–383. doi: 10.1038/sj.ijir.3900863. [DOI] [PubMed] [Google Scholar]
- 2.Hatzimouratidis K., Eardley I., Giuliano F. EAU guidelines on penile curvature. Eur Urol. 2012;62:543–552. doi: 10.1016/j.eururo.2012.05.040. [DOI] [PubMed] [Google Scholar]
- 3.Nelson C.J., Diblasio C., Kendirci M. The chronology of depression and distress in men with Peyronie’s disease. J Sex Med. 2008;5:1985–1990. doi: 10.1111/j.1743-6109.2008.00895.x. [DOI] [PubMed] [Google Scholar]
- 4.Langston J.P., Carson C.C., III Peyronie disease: plication or grafting. Urol Clin North Am. 2011;38:207–216. doi: 10.1016/j.ucl.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 5.Mobley E.M., Fuchs M.E., Myers J.B. Update on plication procedures for Peyronie's disease and other penile deformities. Ther Adv Urol. 2012;4:335–346. doi: 10.1177/1756287212448224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sullivan J., Moskovic D., Nelson C. Peyronie's disease: urologist's knowledge base and practice patterns. Andrology. 2015;3:260–264. doi: 10.1111/andr.292. [DOI] [PubMed] [Google Scholar]
- 7.Baldini A., Morel-Journel N., Paparel P. Patient-reported long-term sexual outcomes following plication surgery for penile curvature: a retrospective 58-patient study. Prog Urol. 2017;27:10–16. doi: 10.1016/j.purol.2016.08.018. [DOI] [PubMed] [Google Scholar]
- 8.Cantoro U., Polito M., Catanzariti F. Penile plication for Peyronie's disease: our results with mean follow-up of 103 months on 89 patients. Int J Impot Res. 2014;26:156–159. doi: 10.1038/ijir.2014.6. [DOI] [PubMed] [Google Scholar]
- 9.Chung P.H., Tausch T.J., Simhan J. Dorsal plication without degloving is safe and effective for correcting ventral penile deformities. Urology. 2014;84:1228–1233. doi: 10.1016/j.urology.2014.05.064. [DOI] [PubMed] [Google Scholar]
- 10.Li W.J., Yao H., Zhang K. Surgical treatment of Peyronie's disease by modified 16-dot placation in China. Transl Androl Urol. 2013;2:10–14. doi: 10.3978/j.issn.2223-4683.2013.02.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yafi F.A., Hatzichristodoulou G., Knoedler C.J. Comparative analysis of tunical plication vs. intralesional injection therapy for ventral Peyronie's disease. J Sex Med. 2015;12:2492–2498. doi: 10.1111/jsm.13072. [DOI] [PubMed] [Google Scholar]
- 12.Mandava S.H., Trost L.W., Hellstrom W.J. A critical analysis of the surgical outcomes for the treatment of Peyronie's disease. Arab J Urol. 2013;11:284–293. doi: 10.1016/j.aju.2013.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dugi D.D., III, Morey A.F. Penoscrotal plication as a uniform approach to reconstruction of penile curvature. BJU Int. 2010;105:1440–1444. doi: 10.1111/j.1464-410X.2009.08991.x. [DOI] [PubMed] [Google Scholar]
- 14.Adibi M., Hudak S.J., Morey A.F. Penile plication without degloving enables effective correction of complex Peyronie's deformities. Urology. 2012;79:831–835. doi: 10.1016/j.urology.2011.12.036. [DOI] [PubMed] [Google Scholar]
- 15.Colman S., Chapple C., Nitti V. Validation of treatment benefit scale for assessing subjective outcomes in treatment of overactive bladder. Urology. 2008;72:803–807. doi: 10.1016/j.urology.2008.05.033. [DOI] [PubMed] [Google Scholar]
- 16.Ebbehøj J., Metz P. New operation for “krummerik” (penile curvature) Urology. 1985;26:76–78. doi: 10.1016/0090-4295(85)90264-x. [DOI] [PubMed] [Google Scholar]
- 17.Hudak S.J., Morey A.F., Adibi M. Favorable patient reported outcomes after penile plication for wide array of Peyronie disease abnormalities. J Urol. 2013;189:1019–1024. doi: 10.1016/j.juro.2012.09.085. [DOI] [PubMed] [Google Scholar]
- 18.Ko Y.H., Moon K.H., Lee S.W. Urologists' perceptions and practice patterns in Peyronie's disease: a Korean nationwide survey including patient satisfaction. Korean J Urol. 2014;55:57–63. doi: 10.4111/kju.2014.55.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van der Horst C., Portillo F.J.M., Seif C. Treatment of penile curvature with Essed-Schroder tunical plication: aspects of quality of life from the patients' perspective. BJU Int. 2004;93:105–108. doi: 10.1111/j.1464-410x.2004.04566.x. [DOI] [PubMed] [Google Scholar]
- 20.Gholami S.S., Lue T.F. Correction of penile curvature using the 16-dot plication technique: a review of 132 patients. J Urol. 2002;167:2066–2069. [PubMed] [Google Scholar]
- 21.Thiounn N., Missirliu A., Zerbib M. Corporeal plication for surgical correction of penile curvature—experience with 60 patients. Eur Urol. 1998;33:401–404. doi: 10.1159/000019624. [DOI] [PubMed] [Google Scholar]
- 22.Geertsen U.A., Brok K.E., Andersen B. Peyronie curvature treated by plication of the penile fasciae. Br J Urol. 1996;77:733–735. doi: 10.1046/j.1464-410x.1996.97621.x. [DOI] [PubMed] [Google Scholar]
- 23.Hauck E.W., Bschleipfer T., Diemer T. Long-term results of Essed-Schroeder plication by the use of non-absorbable Gore-Tex sutures for correcting congenital penile curvature. Int J Impot Res. 2002;14:146–150. doi: 10.1038/sj.ijir.3900827. [DOI] [PubMed] [Google Scholar]