Abstract
Objective:
This review provides an in-depth overview of diagnostic schema and risk factors influencing recovery during the acute, subacute (operationally defined as up to 3 months postinjury), and chronic injury phases across the full spectrum of individuals (e.g., athletes to neurosurgery patients) with mild traumatic brain injury (mTBI). Particular emphasis is placed on the complex differential diagnoses for patients with prolonged postconcussive symptoms.
Methods:
Select literature review and synthesis.
Results:
In spite of an increase in public awareness surrounding the acute and potential long-term effects of mTBI, the medical field remains fragmented both in terms of the diagnostic (different criteria proffered by multiple medical organizations) and prognostic factors that influence patient care.
Conclusions:
Given the lack of objective biomarkers and the spectrum of different disorders that likely encompass mTBI, clinicians are encouraged to adopt a probabilistic, rather than definitive, diagnostic and prognostic framework. The relevance of accurately diagnosing and managing the different manifestations of mTBI becomes clear when one considers the overall incidence of the disorder (42 million people each year worldwide), and the different treatment implications for patients with a true neurodegenerative disorder (e.g., chronic traumatic encephalopathy; rare) vs potentially treatable conditions (e.g., depression or posttraumatic headache; frequent).
There has been a sea change regarding the potential long-term consequences of mild traumatic brain injury (mTBI).1 Initial results suggested limited and transient behavioral changes and no long-term neuropsychiatric consequences for the majority of mTBI patients.2,3 The first decade of the 21st century was marked by an increased incidence of blast-related mTBI in the military and associated reports of high disability rates.4 Recent studies, predominantly based on autopsy and late-life data collected in select cohorts of semiprofessional and professional athletes, suggest that the effects of mTBI may be more severe.5,6 A more realistic assessment suggests an actively evolving field with an incomplete understanding of the neuronal and neuropsychiatric consequences of single vs repetitive mTBIs. The type of injury, medical comorbidities, and stage of injury determine the type of care sought (i.e., isolated mTBI treated by emergency room providers vs repetitive mTBI/subconcussive blows treated by sports medicine specialists vs subdural hematomas treated by neurologists/neurosurgeons). This skews both diagnostic and prognostic perspectives, resulting in research relevant only to narrow subsets of mTBI patients, and inadvertently raises barriers to academic discourse between medical specialties.
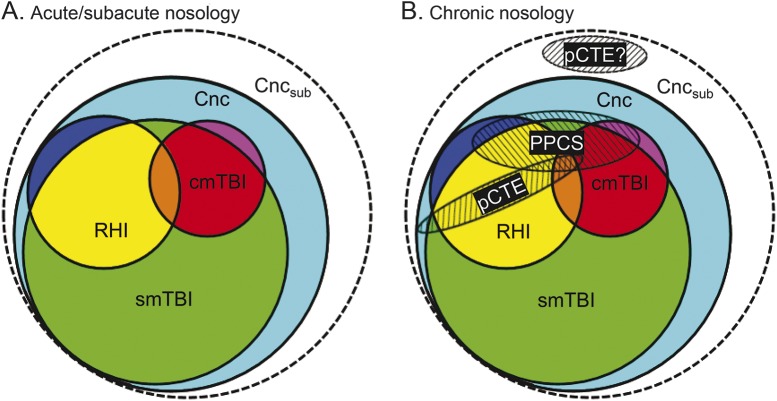
A pertinent example is the current interchangeable use of multiple, separate diagnostic labels (concussion, sports-related concussion, mTBI, complicated mTBI) to describe clinical entities that may or may not be similar (figure 1 and table). The differences in nosology and their associated comorbidities likely contribute to the varying outcomes reported for large-scale cohort studies of injured athletes (i.e., rapid return to play/typical activity levels for the majority)2 vs a much higher (i.e., majority of sample) 6-month disability rate for emergency room/hospitalized patients.7 Therefore, a critical first step is the development of common diagnostic and prognostic nomenclature that spans the fields of neurology, emergency medicine, sports medicine, psychiatry, neurosurgery, and physiatry as well as the full continuum of care (i.e., acute to chronic phases).
Figure 1. Current diagnostic nosology for mild traumatic brain injury (mTBI).
In spite of its confusing nature, figure 1 accurately depicts current diagnostic conceptualizations of mTBI across the continuum of care. According to some official diagnostic conceptualizations for acute mTBI (panel A and table), concussion (Cnc; cyan) represents the least severe form of recognized injury, and is necessary but not sufficient for all other diagnoses (i.e., all other diagnoses fall within the sphere of concussion). Single mTBI (smTBI; green) therefore represents a subset of concussion, although currently there are no clinical or diagnostic criteria proffered for distinguishing smTBI from concussion. A head injury associated with a positive imaging finding constitutes complicated mTBI (cmTBI; red, orange, and purple). Repetitive head injury (RHI) can occur in any of these diagnostic categories or across injury types (yellow, orange, and blue). Subconcussive blows and associated exposure history (Cncsub) are speculative and not officially recognized by any organizational body (represented with dashed rather than solid lines). (B) The superimposition of chronic conditions, operationally defined here as greater than 3 months postinjury, on acute diagnoses. Prolonged postconcussive symptoms (PPCS) can potentially span all acute diagnostic entities, and are currently diagnosed as major or mild neurocognitive disorder due to traumatic brain injury per the DSM-V. Although the prevalence of probable chronic traumatic encephalopathy (pCTE; clinical diagnosis) following a smTBI remains an active area of debate, it is included for thoroughness.
Table.
Current and past diagnostic criteria from several professional medical organizations regarding the diagnosis of mild traumatic brain injury
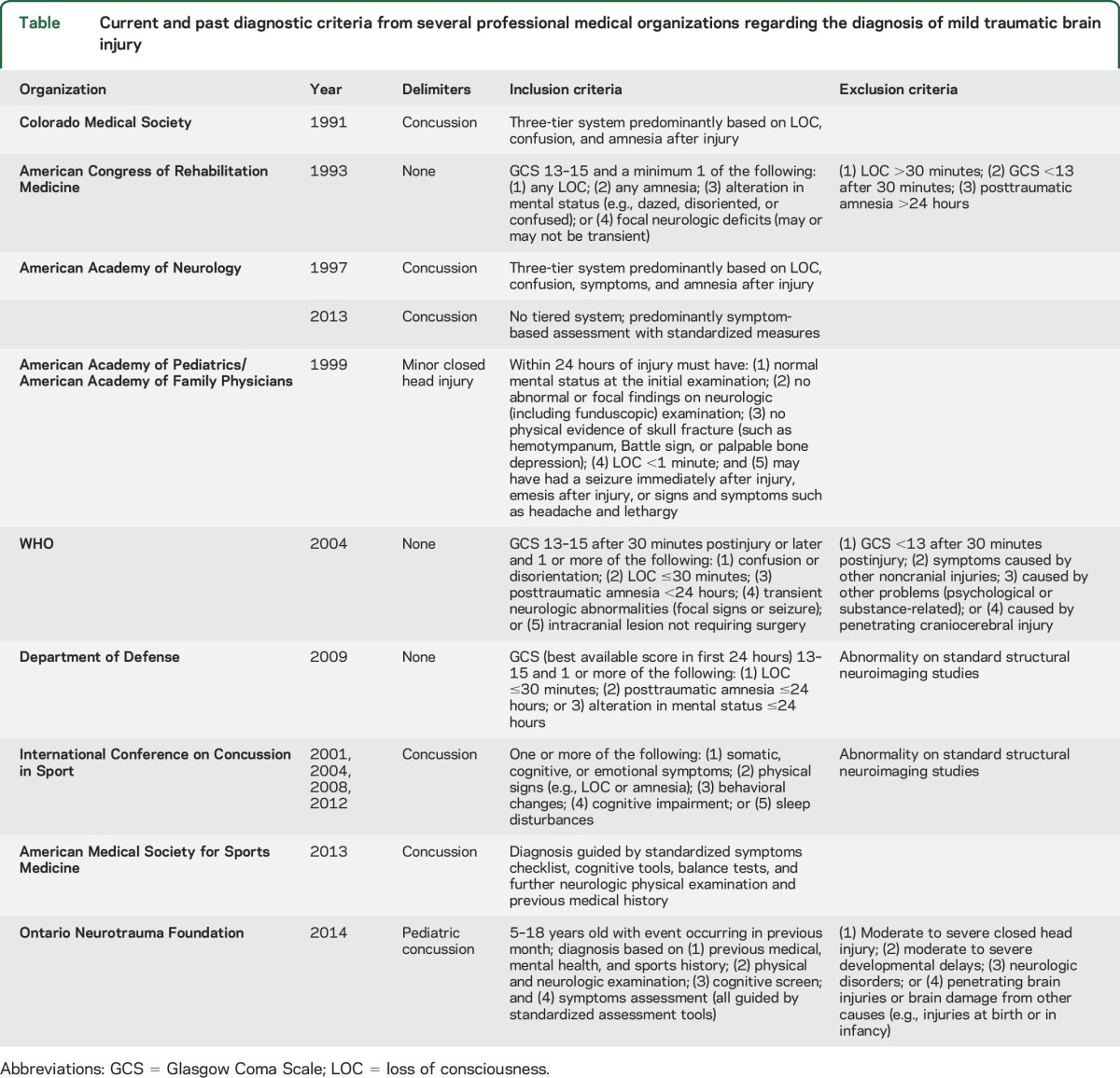
OVERVIEW
The diagnosis of mTBI currently includes patients with widely disparate injury characteristics, from patients who only report symptoms following a head impact to patients with long (i.e., 30 minutes) periods of unconsciousness. Since initial attempts by the Congress of Neurological Surgeons in 1966, criteria for diagnosing mTBI have been clinical in nature.8 The table and figure 1 summarize the different, and sometimes conflicting, diagnostic criteria currently proffered by multiple professional organizations for acute/subacute and chronic stages of mTBI.9 All diagnostic schema require that the patient experience an external force to the head followed by some alteration in brain function.10 Additional common diagnostic criteria include a 30-minute postinjury Glasgow Coma Scale score (GCS) ranging between 13 and 15, duration of loss of consciousness/amnesia, focal neurologic signs, and postconcussive symptoms. With the exception of excluding patients with neuroimaging abnormalities, it is notable that diagnostic criteria for concussion have become more broad and inclusive over time, predominantly focusing on symptom self-report. It is currently unknown how the broader characterization of mTBI will ultimately affect the sensitivity and specificity of future biomarkers and treatment efficacy.
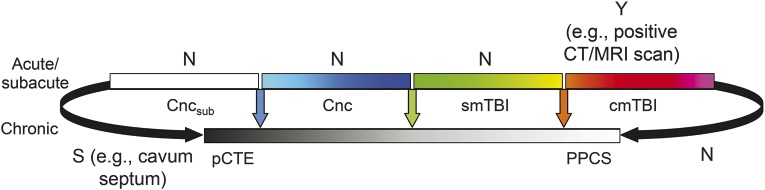
Although the terms concussion and mTBI have traditionally been used interchangeably by most medical practitioners, there has been a recent emphasis in some medical specialties towards classifying concussion as a less severe form of mTBI (table, column 3). However, currently there are no distinct symptom profiles, diagnostic criteria, or objective biomarkers that distinguish concussion from mTBI. The lack of a single and specific diagnostic nosology for classifying the different types of mTBI at different stages represents the greatest existing barrier within the field (i.e., comparison of figure 2 vs figure 1). A consensus diagnostic system is necessary to determine the medical, psychosocial, and demographic factors influencing prognosis, potentially reducing variability in outcomes reported in the field.2,7
Figure 2. Ideal diagnostic nosology for mild traumatic brain injury (mTBI).
In contrast to figure 1, figure 2 depicts a set of linear diagnostic entities that represent the full spectrum of mTBI across both acute and chronic phases. The adopted color scheme is similar to figure 1 for single head injury (subconcussive blows [Cncsub]; concussion [Cnc] = cyan to blue; single mTBI [smTBI] = green to yellow; complicated mTBI [cmTBI] = orange to purple) as well as repetitive head injury (yellow, orange, and blue within each category). In this idealized system, each of the individually proposed entities is diagnostically distinct (denoted by the separating white space between entities) rather than conflated (as indicated by overlapping circles in figure 1). Each entity would ideally be defined by a specific and objective in-life biomarker or independent measurement (represented by multicolored vertical arrows), which currently only exists for cmTBI. Existing evidence for in vivo biomarkers is denoted by Y for yes, S for some, or N for none. pCTE = probable chronic traumatic encephalopathy; PPCS = prolonged postconcussive symptoms.
The main injury factors influencing prognostic considerations include severity, number, and types of previous mTBIs (single vs repetitive injuries) and extracranial injuries. Williams et al.11 were among the first to recognize that mTBI patients with neuroimaging abnormalities on standard CT and MRI scans (i.e., complicated mTBI) had greater impairment in neurobehavioral functioning and worse outcomes. Additional studies have generally replicated this finding and highlighted the divergence in recovery that occurs among patients as they transition from a subacute phase, where both groups are symptomatic, to a more chronic injury phase, where complicated mTBI patients are more symptomatic than typical mTBI patients.12,13 These findings have influenced several medical organizations to exclude patients with positive imaging findings from the diagnostic category of concussion or to automatically classify them as moderate traumatic brain injury (TBI; table, column 5).
The number of previous injuries and their temporal proximity (i.e., clustered together) represent other important injury factors. A history of concussion not only increases the risk of future concussions, but also increases baseline symptoms, as well as long-term cognitive and psychiatric dysregulation in athletes.14 Similar findings have been observed within emergency department samples15 and in animal models of repetitive mTBI.6,16 The long-term effects of subconcussive blows remain indeterminate and are currently not included in any official diagnostic schema (indicated by dashed rather than solid lines in figure 1). Repeated and frequent subconcussive blows, such as intentional heading and unintentional contact that occur in soccer, have recently been linked to neurologic symptoms.17 It has also been suggested that subconcussive blows may represent an important risk factor for developing chronic traumatic encephalopathy (CTE).1
Similarly, although it is still debated as to whether an isolated single mTBI can result in long-term neuropathologic changes (including CTE), most evidence suggests a dose-dependent response curve.5,18 The effects of repetitive mTBI, and potentially of subconcussive blows, have been implicated in a 4-fold increase in neurodegenerative disease19 and the accumulation of tau in perivascular spaces in deep cortical sulci in athletes.5,6 A recent study reported elevated plasma tau levels in both injured and athlete controls relative to nonathletes, with increased tau also associated with delayed return to play.20 As such, a detailed history of previous organized contact or collision sports participation (i.e., exposure history) represents a critical part of the clinical evaluation of chronic symptomatology.1 However, it is critical to note that CTE represents a diagnosis made postmortem based on neuropathologic evidence. Currently there are no clear in-life clinical criteria for diagnosing probable CTE.21,22
A complex, multifaceted, and time-dependent pattern of pathologies (i.e., the neurometabolic cascade of concussion) has been observed in animal models following injury.23 Therefore, it is paramount to recognize that recovery does not represent a unitary concept as frequently conceptualized by most clinicians. Deficits on formal cognitive testing may or may not resolve prior to self-reported symptoms24 and different recovery curves exist for somatic, relative to cognitive, symptoms.25 Similarly, although advanced neuroimaging is still in its infancy for detecting pathophysiologic markers of trauma,26 current data suggest a complex, differential pattern of resolution occurring over weeks or months, depending on the biomarker.27,28 Importantly, these27,28 and other29 studies have preliminarily indicated the presence of abnormal biomarker levels after clinical symptoms have resolved based on traditional neuropsychological testing.29 These findings are intuitively similar to other physical injuries where certain signs (e.g., scar tissue) are present long after the patient ceases to report symptoms (e.g., pain). Symptom resolution, in conjunction with abnormal biomarker levels, may reflect a degree of redundancy within neural networks in which gross behavioral performance can be compensated for, even in the presence of a subtly damaged node or network connection.29 Therefore, defining recovery based on any single variable (i.e., symptom-free) potentially risks premature return to play/work/learn decisions, putting patients at risk for potentially worse outcomes should a repeat, temporally proximate trauma occur. As our ability to detect deficits advances, our understanding and definition of return to normal function following mTBI must also evolve.
The majority of single-episode, noncomplicated adult mTBI patients exhibit a rapid and spontaneous recovery within the first few days to weeks postinjury, with an inability to detect impairment in 80%–95% of adult patients on traditional neurobehavioral measures 3–6 months postinjury.2,3 The recovery time frame for pediatric patients is less well-understood, with some evidence suggesting 4 weeks30,31 to greater than a year32 postinjury for recovery to preinjury function. Assessment of pediatric mTBI is further complicated by ongoing neurodevelopment. The recent development of a 12-point clinical risk score shows promise in identifying children at the time of injury who will have persisting symptoms at 28 days postinjury.31 Longer symptom durations among studies likely reflect differences in medical comorbidities (polytrauma) and associated injury severity levels (positive vs negative cranial imaging) that are frequently confounded with location of subject recruitment (e.g., athletes vs neurosurgery patients).33
ACUTE/SUBACUTE EVALUATION AND MANAGEMENT OF MTBI (IMMEDIATE TO 3 MONTHS)
Any head impact with the subsequent manifestation of signs or symptoms consistent with mTBI warrants immediate removal from the inciting context (e.g., sports participation). In cases with loss of consciousness or impact seizure, patients should receive a comprehensive evaluation for serious brain or cervical spine injury, possibly including a CT scan. CT scans remain the gold standard for mTBI imaging due to cost savings and increased ability to detect acute blood (e.g., subdural or epidural hematoma) and fractures relative to MRI. However, concerns about unnecessary radiation have led to the development of guidelines for CT use,34,35 with recent studies indicating the potential of blood-based biomarkers as an adjunctive diagnostic tool.36
The Canadian CT Head Rule recommends all patients with GCS score <15 at 2 hours postinjury; open, depressed, or basilar skull fracture; more than one episode of vomiting; or age ≥65 years receive a CT. The New Orleans Criteria are similar to the Canadian rules (for details, see table 1 from reference 35). CT scans are also recommended for any patient with a deteriorating clinical course in the first few hours postinjury. In children over 2 years of age, the presence of normal mental status, no loss of consciousness, no vomiting, nonsevere injury mechanism, no signs of basilar skull fracture, and no severe headache had a negative predictive value of 99.95% for a clinically important TBI requiring neurosurgical intervention.34
Acute clinical assessment during the first 48 hours should include a thorough history of the injury (loss of consciousness, retrograde/anterograde amnesia, impact seizure, focal neurologic signs, and postconcussive symptoms [PCS]), history of recent/previous concussions, preexisting medical conditions (depression, migraines, learning disabilities, substance use), and a general neurologic examination. Efforts to standardize mTBI assessment include the Common Data Elements from the National Institute of Neurological Disorders and Stroke, and should be adhered to whenever possible to facilitate comparisons of data derived from different samples.37 The GCS was developed for use in more severely injured patients and thus has limited discriminative or prognostic value in mTBI. A normal GCS score, in conjunction with negative structural imaging (CT or traditional MRI), was traditionally assumed to indicate that mTBI was not associated with neurologic damage.38 In contrast, the systematic use of concussion symptom scales is helpful for assisting with concussion diagnosis and documenting symptom progression as a function of time.
PCS are typically divided into 4 major categories spanning cognitive (e.g., attention, executive functioning, and memory problems), somatic (e.g., headache, nausea, dizziness, balance, and sensitivity to light/noise), affective (e.g., irritability, anxiety, and depression), and sleep-arousal complaints (e.g., fatigue). Complex interactions exist between categories, with affective or sleep disturbances worsening cognitive symptomatology.39 Not surprisingly, greater symptom burden at initial presentation is associated with poorer recovery. However, the subjective and nonspecific nature of self-reported PCS inherently limits their utility.40 Additional caution with symptom self-report is warranted in pediatric populations due to developmental issues,41 necessitating the use of secondary sources of information (guardian/parent/teacher) whenever possible. PCS underreporting in athletes, overreporting in the presence of secondary gain (e.g., not returning to school, sport, or work, or litigation), and sex-related (female > male PCS) differences have also been observed.42
All mTBI patients should temporarily discontinue activities that present a risk of additional head injury. This simple strategy greatly reduces the potential exacerbation of the initial injury, as well as the likelihood of second impact syndrome, a controversial, rare, and frequently deadly condition associated with cerebral autodysregulation and edema.43 Although there is preclinical and clinical evidence suggesting the benefit of early cognitive and physical rest, the duration of rest remains actively debated,44 with a brief, rather than extended, period of acute rest comprising the currently recommended primary management strategy. There is evidence that exercise, beyond the immediate acute injury timeframe, is likely rehabilitative rather than dangerous.45 Thus, return to sports, learning, and work activities at a low risk for head injury should occur in a timely, stepwise fashion.46,47
Auditory (e.g., high-frequency hearing loss, tinnitus, and sound sensitivity), visual (e.g., difficulty with saccades, smooth pursuits, and convergence), olfactory (anosmia), and vestibular (dizziness and difficulty with balance) symptoms resulting from concussion and associated trauma (e.g., fractures of the temporal bone, shearing of olfactory nerve on cribriform plate) must also be assessed given their influence on recovery and available treatments.48 A brief Vestibular Oculomotor Screen can be used to evaluate concussion in a standardized fashion.49 Targeted vestibular therapy, including habituation and adaptation exercises (e.g., saccadic substitution exercises, head motion during fixation), may help patients who have prolonged symptoms (e.g., dizziness, balance and motion sensitivity).50 Similarly, binocular visual oculomotor deficits (e.g., saccadic deficiency, convergence insufficiency) represent another target for rehabilitation.51
CHRONIC POSTCONCUSSIVE EVALUATION AND MANAGEMENT
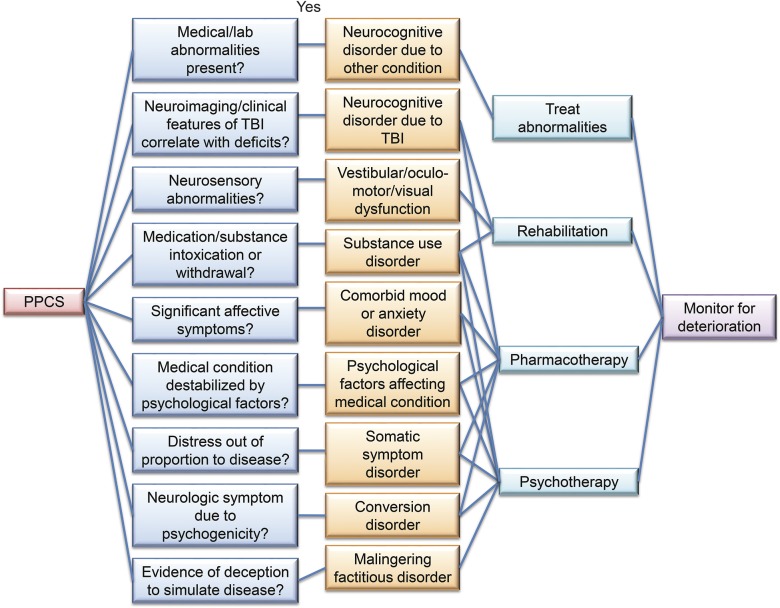
Patients who manifest prolonged PCS are challenging to conceptualize and properly treat (figure 3). The first diagnostic barrier is the lack of consensus on a definition of prolonged in terms of symptom duration.52 Until 2014, the 2 available consensus criteria for postconcussion syndrome were found in the DSM-IV-TR and the ICD-10. Although both classifications required a minimum of 3 postconcussive symptoms, the DSM-IV-TR specified that symptoms must last more than 3 months, whereas ICD-10 does not have a minimum symptom duration. This likely contributed to differences in incidence rates when using the 2 diagnostic criteria.53 Other significant differences between the 2 sets of criteria included the following: (1) only ICD-10 required loss of consciousness at the time of injury; (2) DSM-IV-TR required presence of objective cognitive impairment, whereas ICD-10 required absence; and (3) ICD-10 required PCS onset within 4 weeks of injury, whereas DSM-IV-TR specified only that PCS begin “shortly” after injury.
Figure 3. Differential diagnosis and management strategy for prolonged postconcussive symptoms (PPCS).
Multiple etiologies may contribute simultaneously to PPCS; testing for these should proceed in parallel, as should multimodal treatment. Long-term monitoring for evidence of transition from PPCS to other neurodegenerative disorders in high-risk individuals (i.e., patients with multiple head injuries) is recommended following appropriate treatments. TBI = traumatic brain injury.
The DSM-5 (released in May 2014) does not include postconcussion syndrome as a separate diagnostic entity. As a major change, clinicians are now instructed to diagnose “major or mild neurocognitive disorder due to traumatic brain injury” depending on the severity of cognitive deficits and functional disability present, regardless of initial injury severity (e.g., whether a patient's initial GCS score was 13–15 or below 8). Clinicians should consider a comprehensive list of potential organic, as well as psychological, contributors to prolonged PCS (figure 3).
CLINICAL EVALUATION
A second diagnostic barrier is the tension between perspectives on PCS as a biological effect of mTBI vs a psychological coping response to a stressor. PCS are nonspecific and frequently observed in both healthy and orthopedically injured samples.40 Similar to other non-TBI patients with persistent neurobehavioral complaints, laboratory tests for serum electrolytes, complete blood count, thyroid-stimulating hormone level, thiamine, B12, folate level, erythrocyte sedimentation rate, and HIV/Treponema pallidum antibodies may be considered for the purpose of a thorough differential diagnosis. However, these ancillary tests are generally not indicated when the history, physical examination, and course of events support the diagnosis of mTBI. Patients presenting with prolonged PCS should undergo a careful reassessment of all history and clinical data pertaining to the initial injury, including the presence of polytrauma, neurosurgical intervention, and inpatient hospital admission, all of which negatively influence clinical outcomes.54
Advanced MRI scans (e.g., susceptibility-weighted imaging, fluid-attenuated inversion recovery, or T2*-weighted sequences) may be considered for patients who do not fully recover from their injuries for improved prognostication. It has been estimated that diffuse axonal injury and petechial hemorrhages are not detected in up to 25%–30% of CT scans,13 and lesion-positive MRI scans may have emerging prognostic implications.12,13 Formal neuropsychological testing should be obtained to determine any objective cognitive deficits. The majority of mTBI patients in unselected samples have normal testing at 3 months postinjury, with only a small fraction of patients demonstrating subtle cognitive deficits 1 year postinjury.2,3 Self-reported complaints of impaired cognition in spite of a lack of objective deficits or neuroimaging abnormalities33,55 should elicit a reexamination of the original severity of the injury, history of prior mTBIs, and a comprehensive assessment of psychological risk factors. Finally, patients with prolonged PCS and a predominant pattern of neurosensory dysfunction should be referred to appropriate specialists (e.g., occupational/physical/language therapists) for rehabilitation.
DEMOGRAPHIC AND CLINICAL FACTORS
Demographic and clinical (non-TBI) factors associated with prolonged PCS include psychiatric illness, prior learning disability/attentional disorder, lower levels of education, young age or elderly status, and physical illness.3,55 Depression represents the most commonly diagnosed neuropsychiatric complication across all levels of TBI severity.56 Similarly, posttraumatic stress disorder (PTSD) is highly comorbid with mTBI in military settings, with a lower rate (between 10% and 25%) observed in civilian injuries.57,58 Military mTBI is also somewhat unique in terms of the mechanism of injury (blast-related vs traditional acceleration/deceleration), as well as the presence of extreme combat-related stressors both pre- and postinjury, the presence of which may exacerbate PTSD symptoms.59 Substance use/intoxication both increases the risk of sustaining a TBI and complicates outcome,60 with 30%–50% of all new mTBI cases occurring under the influence of alcohol.61
Psychiatric illness or vulnerability preceding TBI, including family history of mood disorders, and history of substance use, predict the presence/severity of PCS.56 This historically promoted a long-standing belief that prolonged PCS primarily resulted from premorbid psychiatric illness, rather than resulting from the mTBI itself. While it is true that premorbid psychiatric illness represents a significant risk factor, an alternative hypothesis for consideration is that the neurobiological changes associated with psychiatric illnesses (e.g., dysregulation of hypothalamic–pituitary–adrenal axis, upregulation or downregulation of neuroreceptors within the mesocorticolimbic dopaminergic circuits) may predispose the brain to more severe consequences following physical injury.
Affective dysregulation or substance abuse following mTBI may result from changes in lifestyle (e.g., decreased occupational, social, and interpersonal functioning) indirectly associated with injury56 or due to psychological trauma experienced during the injury. Alternatively, mesocorticolimbic networks or their white matter connections may be directly (e.g., limbic cortex impacting upon bony protuberances) or indirectly (e.g., secondary processes such as neuroinflammation) affected by mTBI,26 leading to organically induced neuropsychiatric syndromes, which appear to be purely psychological in nature. Regardless of etiologic mechanisms, the amount of psychological distress among concussed high school and collegiate athletes (ranges between 17% and 46%) is greater than observed base rates,62 with reports of long-term affective dysregulation persisting years postinjury following concussion in athletes,63 retired boxers, and professional football players.6,22 Depression, PTSD, and substance abuse mimic the cognitive, emotional, and physical symptoms of concussion and must be screened for first and addressed with standard of care treatments (figure 3) regardless of suspected etiology.
In general, patients who coped poorly with stress before mTBI will be more likely to adopt maladaptive coping strategies following mTBI. Persons with low resilience, who cope via avoidance, who recall preinjury functioning as better than it was (the “good old days” phenomenon), or who magnify symptoms once given a diagnosis (“diagnosis threat”), typically experience worse PCS.64 PCS that are distressing out of proportion to observable disease for at least 6 months may indicate a somatic symptom disorder (SSD), which replaced somatization disorder in DSM-5. The primary criterion includes the presence of high anxiety, persistent thoughts about the seriousness of physical symptoms, or excessive time and energy devoted to symptoms. Conversion disorder, a neurologic subtype of SSD, is diagnosed when signs or physical findings are present that positively suggest that the symptom is psychogenic. Even with these diagnoses, however, these manifestations may reflect underlying pathophysiology following mTBI. In the DSM-5, SSD must be distinguished from psychological factors affecting a medical illness, in which genuine medical instability results from habitual thoughts or behaviors, such as a recurrence of posttraumatic seizures due to nonadherence with anticonvulsant medications.
The intentional simulation or amplification of prolonged PCS for material gain (malingering) or psychological benefit (factitious disorder) is rare in the general population. Patients may be observed to manifest poor effort or overelaboration of symptoms during neuropsychological testing in conjunction with strong evidence of external gain (i.e., litigation)65; however, this should not be automatically construed as malingering. Mild deceptive behavior is commonplace in all levels of a medical system66 and brain injuries can damage neural structures mediating such effort. An open clinical approach is therefore recommended, taking into account the spectrum of possible factors involved in prolonged PCS.
DISCUSSION
Given the current lack of objective in vivo biomarkers (figure 2), clinicians should adopt a probabilistic, rather than definitive, diagnostic framework, based on history and presenting symptoms, for diagnosing the spectrum of mTBI as a function of time postinjury. The need for a probabilistic framework is best typified by a recent case report where a 25-year-old athlete developed prolonged and debilitating PCS over a multiyear period after experiencing more than 10 concussions.67 As recently as 5 years ago, and even in some clinics today, this young man would have likely been diagnosed with SSD or other related psychiatric disorders. However, autopsy results following a sudden cardiac arrest revealed neurodegenerative signs pathognomonically associated with CTE, indicating that mTBI factors may have played a role in his constellation of symptoms in addition to other clinical diagnoses (i.e., history of substance abuse). This published case report is contrasted with lay press reports of the suicide of another patient who incorrectly assumed he had probable CTE (negative at autopsy).68 Importantly, this latter patient's symptoms (e.g., depression) would likely have responded to effective existing therapies. Instead, the patient incorrectly attributed his symptoms to a diagnosis that currently can only be confirmed postmortem and further assumed a progressive, degenerative disease process. These cases illustrate the importance of comprehensive phenotyping of postconcussion injury status, premorbid personal and family history, neurosensory disturbances, neuropsychological testing, advanced imaging, and laboratory examinations for fully informed care.
GLOSSARY
- CTE
chronic traumatic encephalopathy
- DSM-IV-TR
Diagnostic and Statistical Manual–IV–Text Revision
- DSM-5
Diagnostic and Statistical Manual–5
- GCS
Glasgow Coma Scale
- ICD-10
International Classification of Diseases, 10th revision
- mTBI
mild traumatic brain injury
- PCS
postconcussive symptoms
- PTSD
posttraumatic stress disorder
- SSD
somatic symptom disorder
- TBI
traumatic brain injury
AUTHOR CONTRIBUTIONS
Dr. Mayer: study concept and design. Drs. Mayer, Master, and Quinn: analysis and interpretation. Drs. Mayer, Master, and Quinn: critical revision of the manuscript for important intellectual content. Drs. Mayer, Master, and Quinn: study supervision.
STUDY FUNDING
No targeted funding reported.
DISCLOSURE
A. Mayer: NIH grant 1 R01 NS098494-01A1 and 1 P20 GM109089-01. D. Quinn: NIH grant 1 P20 GM109089-01. C. Master: NIH grant 1 R01 NS097549-01A1. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Gardner RC, Yaffe K. Epidemiology of mild traumatic brain injury and neurodegenerative disease. Mol Cell Neurosci 2015;66:75–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McCrea M, Guskiewicz KM, Marshall SW, et al. Acute effects and recovery time following concussion in collegiate football players: the NCAA Concussion Study. JAMA 2003;290:2556–2563. [DOI] [PubMed] [Google Scholar]
- 3.Karr JE, Areshenkoff CN, Garcia-Barrera MA. The neuropsychological outcomes of concussion: a systematic review of meta-analyses on the cognitive sequelae of mild traumatic brain injury. Neuropsychology 2014;28:321–336. [DOI] [PubMed] [Google Scholar]
- 4.DeKosky ST, Ikonomovic MD, Gandy S. Traumatic brain injury: football, warfare, and long-term effects. N Engl J Med 2010;363:1293–1296. [DOI] [PubMed] [Google Scholar]
- 5.Bieniek KF, Ross OA, Cormier KA, et al. Chronic traumatic encephalopathy pathology in a neurodegenerative disorders brain bank. Acta Neuropathol 2015;130:877–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McKee AC, Stein TD, Nowinski CJ, et al. The spectrum of disease in chronic traumatic encephalopathy. Brain 2013;136:43–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lingsma HF, Yue JK, Maas AI, Steyerberg EW, Manley GT. Outcome prediction after mild and complicated mild traumatic brain injury: external validation of existing models and identification of new predictors using the TRACK-TBI pilot study. J Neurotrauma 2015;32:83–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gurdjian ES, Volis HC. Congress of Neurological Surgeons Committee on head injury nomenclature: glossary of head injury. Clin Neurosurg 1966;12:386–394. [Google Scholar]
- 9.Ruff RM, Iverson GL, Barth JT, Bush SS, Broshek DK. Recommendations for diagnosing a mild traumatic brain injury: a National Academy of Neuropsychology education paper. Arch Clin Neuropsychol 2009;24:3–10. [DOI] [PubMed] [Google Scholar]
- 10.Menon DK, Schwab K, Wright DW, Maas AI. Position statement: definition of traumatic brain injury. Arch Phys Med Rehabil 2010;91:1637–1640. [DOI] [PubMed] [Google Scholar]
- 11.Williams DH, Levin HS, Eisenberg HM. Mild head injury classification. Neurosurgery 1990;27:422–428. [DOI] [PubMed] [Google Scholar]
- 12.Kashluba S, Hanks RA, Casey JE, Millis SR. Neuropsychologic and functional outcome after complicated mild traumatic brain injury. Arch Phys Med Rehabil 2008;89:904–911. [DOI] [PubMed] [Google Scholar]
- 13.Yuh EL, Mukherjee P, Lingsma HF, et al. Magnetic resonance imaging improves 3-month outcome prediction in mild traumatic brain injury. Ann Neurol 2013;73:224–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harmon KG, Drezner JA, Gammons M, et al. American Medical Society for Sports Medicine position statement: concussion in sport. Br J Sports Med 2013;47:15–26. [DOI] [PubMed] [Google Scholar]
- 15.Dams-O'Connor K, Spielman L, Singh A, et al. The impact of previous traumatic brain injury on health and functioning: a TRACK-TBI study. J Neurotrauma 2013;30:2014–2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Giza CC, Hovda DA. The neurometabolic cascade of concussion. J Athl Train 2001;36:228–235. [PMC free article] [PubMed] [Google Scholar]
- 17.Stewart WF, Kim N, Ifrah CS, et al. Symptoms from repeated intentional and unintentional head impact in soccer players. Neurology 2017;88:901–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith DH, Johnson VE, Stewart W. Chronic neuropathologies of single and repetitive TBI: substrates of dementia? Nat Rev Neurol 2013;9:211–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lehman EJ, Hein MJ, Baron SL, Gersic CM. Neurodegenerative causes of death among retired National Football League players. Neurology 2012;79:1970–1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gill J, Merchant-Borna K, Jeromin A, Livingston W, Bazarian J. Acute plasma tau relates to prolonged return to play after concussion. Neurology 2017;88:595–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hanlon FM, McGrew CA, Mayer AR. Does a unique neuropsychiatric profile currently exist for chronic traumatic encephalopathy? Curr Sports Med Rep 2017;16:30–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stern RA, Daneshvar DH, Baugh CM, et al. Clinical presentation of chronic traumatic encephalopathy. Neurology 2013;81:1122–1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Giza CC, Hovda DA. The new neurometabolic cascade of concussion. Neurosurgery 2014;75:S24–S33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ponsford J, Cameron P, Fitzgerald M, Grant M, Mikocka-Walus A, Schonberger M. Predictors of postconcussive symptoms 3 months after mild traumatic brain injury. Neuropsychology 2012;26:304–313. [DOI] [PubMed] [Google Scholar]
- 25.Taylor HG, Dietrich A, Nuss K, et al. Post-concussive symptoms in children with mild traumatic brain injury. Neuropsychology 2010;24:148–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bigler ED, Maxwell WL. Neuropathology of mild traumatic brain injury: relationship to neuroimaging findings. Brain Imaging Behav 2012;6:108–136. [DOI] [PubMed] [Google Scholar]
- 27.Meier TB, Bellgowan PS, Singh R, Kuplicki R, Polansky M, Mayer AR. Recovery of cerebral blood flow following sports-related concussion. JAMA Neurol 2015;72:530–538. [DOI] [PubMed] [Google Scholar]
- 28.Vagnozzi R, Signoretti S, Cristofori L, et al. Assessment of metabolic brain damage and recovery following mild traumatic brain injury: a multicentre, proton magnetic resonance spectroscopic study in concussed patients. Brain 2010;133:3232–3242. [DOI] [PubMed] [Google Scholar]
- 29.Mayer AR, Mannell MV, Ling J, Gasparovic C, Yeo RA. Functional connectivity in mild traumatic brain injury. Hum Brain Mapp 2011;32:1825–1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Henry LC, Sandel N. Adolescent subtest norms for the ImPACT Neurocognitive Battery. Appl Neuropsychol Child 2015;4:266–276. [DOI] [PubMed] [Google Scholar]
- 31.Zemek R, Barrowman N, Freedman SB, et al. Clinical risk score for persistent postconcussion symptoms among children with acute concussion in the ED. JAMA 2016;315:1014–1025. [DOI] [PubMed] [Google Scholar]
- 32.Yeates KO, Kaizar E, Rusin J, et al. Reliable change in postconcussive symptoms and its functional consequences among children with mild traumatic brain injury. Arch Pediatr Adolesc Med 2012;166:615–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McMahon P, Hricik A, Yue JK, et al. Symptomatology and functional outcome in mild traumatic brain injury: results from the prospective TRACK-TBI study. J Neurotrauma 2014;31:26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kuppermann N, Holmes JF, Dayan PS, et al. Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet 2009;374:1160–1170. [DOI] [PubMed] [Google Scholar]
- 35.Stein SC, Fabbri A, Servadei F, Glick HA. A critical comparison of clinical decision instruments for computed tomographic scanning in mild closed traumatic brain injury in adolescents and adults. Ann Emerg Med 2009;53:180–188. [DOI] [PubMed] [Google Scholar]
- 36.Diaz-Arrastia R, Wang KK, Papa L, et al. Acute biomarkers of traumatic brain injury: relationship between plasma levels of ubiquitin C-terminal hydrolase-L1 and glial fibrillary acidic protein. J Neurotrauma 2014;31:19–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grinnon ST, Miller K, Marler JR, et al. National Institute of Neurological Disorders and Stroke Common Data Element Project: approach and methods. Clin Trials 2012;9:322–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hawryluk GW, Manley GT. Classification of traumatic brain injury: past, present, and future. Handb Clin Neurol 2015;127:15–21. [DOI] [PubMed] [Google Scholar]
- 39.King PR, Donnelly KT, Donnelly JP, et al. Psychometric study of the neurobehavioral symptom inventory. J Rehabil Res Dev 2012;49:879–888. [DOI] [PubMed] [Google Scholar]
- 40.Iverson GL, Lange RT. Examination of “postconcussion-like” symptoms in a healthy sample. Appl Neuropsychol 2003;10:137–144. [DOI] [PubMed] [Google Scholar]
- 41.Gilbert F, Johnson LS. The impact of American tackle football-related concussion in youth athletes. AJOB Neurosci 2011;2:48–59. [Google Scholar]
- 42.Merritt VC, Arnett PA. Premorbid predictors of postconcussion symptoms in collegiate athletes. J Clin Exp Neuropsychol 2014;36:1098–1111. [DOI] [PubMed] [Google Scholar]
- 43.Cantu RC, Voy R. Second impact syndrome: a risk in any contact sport. Phys Sportsmed 1995;23:27–34. [DOI] [PubMed] [Google Scholar]
- 44.Thomas DG, Apps JN, Hoffmann RG, McCrea M, Hammeke T. Benefits of strict rest after acute concussion: a randomized controlled trial. Pediatrics 2015;135:213–223. [DOI] [PubMed] [Google Scholar]
- 45.Leddy JJ, Willer B. Use of graded exercise testing in concussion and return-to-activity management. Curr Sports Med Rep 2013;12:370–376. [DOI] [PubMed] [Google Scholar]
- 46.Master CL, Balcer L, Collins M. In the clinic: concussion. Ann Intern Med 2014;160:ITC2–1. [DOI] [PubMed] [Google Scholar]
- 47.McCrory P, Meeuwisse WH, Aubry M, et al. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med 2013;47:250–258. [DOI] [PubMed] [Google Scholar]
- 48.Hoffer ME. Mild traumatic brain injury: neurosensory effects. Curr Opin Neurol 2015;28:74–77. [DOI] [PubMed] [Google Scholar]
- 49.Mucha A, Collins MW, Elbin RJ, et al. A brief Vestibular/Ocular Motor Screening (VOMS) assessment to evaluate concussions: preliminary findings. Am J Sports Med 2014;42:2479–2486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Aligene K, Lin E. Vestibular and balance treatment of the concussed athlete. NeuroRehabilitation 2013;32:543–553. [DOI] [PubMed] [Google Scholar]
- 51.Master CL, Scheiman M, Gallaway M, et al. Vision diagnoses are common after concussion in adolescents. Clin Pediatr 2016;55:260–267. [DOI] [PubMed] [Google Scholar]
- 52.Rose SC, Fischer AN, Heyer GL. How long is too long? The lack of consensus regarding the post-concussion syndrome diagnosis. Brain Inj 2015;29:798–803. [DOI] [PubMed] [Google Scholar]
- 53.McCauley SR, Boake C, Pedroza C, et al. Postconcussional disorder: are the DSM-IV criteria an improvement over the ICD-10? J Nerv Ment Dis 2005;193:540–550. [DOI] [PubMed] [Google Scholar]
- 54.Levin HS, Diaz-Arrastia RR. Diagnosis, prognosis, and clinical management of mild traumatic brain injury. Lancet Neurol 2015;14:506–517. [DOI] [PubMed] [Google Scholar]
- 55.Ponsford J, Cameron P, Fitzgerald M, Grant M, Mikocka-Walus A. Long-term outcomes after uncomplicated mild traumatic brain injury: a comparison with trauma controls. J Neurotrauma 2011;28:937–946. [DOI] [PubMed] [Google Scholar]
- 56.Dikmen SS, Bombardier CH, Machamer JE, Fann JR, Temkin NR. Natural history of depression in traumatic brain injury. Arch Phys Med Rehabil 2004;85:1457–1464. [DOI] [PubMed] [Google Scholar]
- 57.Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in U.S. soldiers returning from Iraq. N Engl J Med 2008;358:453–463. [DOI] [PubMed] [Google Scholar]
- 58.Haarbauer-Krupa J, Taylor CA, Yue JK, et al. Screening for post-traumatic stress disorder in a civilian emergency department population with traumatic brain injury. J Neurotrauma 2016;34:50–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Reger ML, Poulos AM, Buen F, Giza CC, Hovda DA, Fanselow MS. Concussive brain injury enhances fear learning and excitatory processes in the amygdala. Biol Psychiatry 2012;71:335–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wilde EA, Bigler ED, Gandhi PV, et al. Alcohol abuse and traumatic brain injury: quantitative magnetic resonance imaging and neuropsychological outcome. J Neurotrauma 2004;21:137–147. [DOI] [PubMed] [Google Scholar]
- 61.Scheenen ME, de Koning ME, van der Horn HJ, et al. Acute alcohol intoxication in patients with mild traumatic brain injury: characteristics, recovery, and outcome. J Neurotrauma 2016;33:339–345. [DOI] [PubMed] [Google Scholar]
- 62.Kontos AP, Covassin T, Elbin RJ, Parker T. Depression and neurocognitive performance after concussion among male and female high school and collegiate athletes. Arch Phys Med Rehabil 2012;93:1751–1756. [DOI] [PubMed] [Google Scholar]
- 63.Konrad C, Geburek AJ, Rist F, et al. Long-term cognitive and emotional consequences of mild traumatic brain injury. Psychol Med 2011;41:1197–1211. [DOI] [PubMed] [Google Scholar]
- 64.Broshek DK, De Marco AP, Freeman JR. A review of post-concussion syndrome and psychological factors associated with concussion. Brain Inj 2015;29:228–237. [DOI] [PubMed] [Google Scholar]
- 65.Larrabee GJ, Rohling ML. Neuropsychological differential diagnosis of mild traumatic brain injury. Behav Sci Law 2013;31:686–701. [DOI] [PubMed] [Google Scholar]
- 66.Bass C, Halligan P. Factitious disorders and malingering: challenges for clinical assessment and management. Lancet 2014;383:1422–1432. [DOI] [PubMed] [Google Scholar]
- 67.Mez J, Solomon TM, Daneshvar DH, Stein TD, McKee AC. Pathologically confirmed chronic traumatic encephalopathy in a 25-year-old former college football player. JAMA Neurol 2016;73:353–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Branch J. Autopsy shows the N.H.L.'s Todd Ewen did not have C.T.E. The New York Times 2016. Available at: nytimes.com/2016/02/11/sports/hockey/autopsy-shows-the-nhls-todd-ewen-did-not-have-cte.html. Accessed March 26, 2017. [Google Scholar]