Abstract
The levels of satisfaction of the core self-determination needs (relatedness, autonomy, competence) among HIV-infected women of color as well as the association between need fulfillment and patient characteristics were examined. Having less than a high school education was associated with lowest need satisfaction: autonomy (β= −1.90; 95%CI= −3.20, −0.60), relatedness (β= −2.70; 95%CI= −4.30, −1.10), and competency (β= −2.50; 95%CI= −3.60, −1.30). Each additional point increase in affective symptoms of depression was associated with decrements in need satisfaction (−0.61 autonomy, −0.68 relatedness, −0.59 competency). Relatedness satisfaction was lower with higher responses on all three measures of violence (psychological abuse: β= −0.13, 95%CI= −0.19 to −0.07; adult traumatic experiences: β= −0.24, 95%CI= −0.35 to −0.13; childhood traumatic experiences: β= −0.24, 95%CI= −0.40 to −0.08). Interventions that address core self-determination needs, and the characteristics that influence them, may enhance the motivation for self-care of HIV-infected women.
Keywords: women-of-color, HIV, autonomy, relatedness, competence, retention-in-care, self-determination theory
INTRODUCTION
HIV-infected women experience a range of barriers to care (Cunningham et al., 1999; Toth et al., 2013; Webel et al., 2013); and related work suggests unique trajectories for the process of engaging and remaining in HIV care among women of color (WOC) (Messer et al., 2013; Quinlivan et al., 2013). Despite the need to facilitate adoption of HIV health behaviors for women, limited use has been made of motivation theory for understanding HIV medication adherence or engagement in care (Houston et al., 2012; Igreja, 2000; Kennedy et al., 2004 ; Lynam et al., 2009; Toth et al., 2013). Improving women’s internal motivation to engage with HIV care is important in light of the increasing evidence of the benefits of antiretroviral therapy (ART).
Self-determination theory (SDT)(Deci, 1995; Deci & Ryan, 2000; Ryan & Deci, 2000) is used to predict the adoption of a variety of behavioral changes and the motivation involved for successful change (Williams, Freedman, et al., 1998; Williams et al., 2002; Williams et al., 2011; Wilson & Rodgers, 2004). According to SDT, the inherent psychological needs for competence, relatedness, and autonomy must be fulfilled for the adoption of new behaviors to be internally motivated and sustained, and to achieve positive health outcomes. Autonomy refers to an individual’s need to act in a way that is congruent with their values and concept of self (Johnson, 2007). Competence is similar to self-efficacy, but refers to actual ability rather than belief about one’s ability (Johnston & Finney, 2010; Ryan & Deci, 2000). Relatedness refers to being connected to others and to feeling cared for (Johnson, 2007; Johnson et al., 2008; Johnston & Finney, 2010). Ryan and Deci posit that a “secure relational base” is important for the expression of intrinsic motivation (Ryan & Deci, 2000).
SDT studies have found that increasing autonomy leads to increased motivation and improvements in a variety of health behaviors: smoking cessation (Williams et al., 2002; Williams et al., 2011), weight loss (Williams & Deci, 1996; Williams et al., 1996), diabetes (Williams, Freedman, et al., 1998; Williams, Rodin, et al., 1998), hepatitis C treatment (Morse et al., 2012), and cardiac rehabilitation (Russell & Bray, 2010). To date, SDT has been used to understand HIV related medication adherence and treatment motivation (Houston et al., 2012) and self-reported well-being in a sample of HIV-infected men (Igreja, 2000). It has also been used to frame the experiences of testing and entry into care among a sample of HIV-infected WOC (Quinlivan et al., 2013; Toth et al., 2013). We aim to expand the literature on SDT and HIV treatment as measured in a population of WOC receiving HIV medical care. The purpose of this paper is to identify the distribution of relatedness, autonomy, and competence achievement among a sample of HIV-infected WOC and explore the demographic and health-related factors that appear associated with these precursors for intrinsic-motivation development.
METHODS
Research setting
The research was conducted as part of the Guide to Healing project, which is one of the 9 projects included in the Special Projects of National Significance Program’s ‘Enhancing Access to and Retention in Quality HIV/AIDS Care for Women of Color Initiative’. The site was located in an academic infectious diseases clinic that providing care to 1700 HIV-infected people in 2010. Of the 31% female patients, almost all (82%) belonged to racial/ethnic minorities, including 69% AA. Baseline study participants were recruited between April 2010 and February 2011 from a catchment area of rural and urban counties.
Data collection
Serial cross-sectional data were collected as part of an interrupted time series evaluation design. WOC were eligible if they met the following criteria: 1) were HIV-infected; 2) had an appointment that day at the clinic; 3) were 18 years or older; and 4) spoke English. All WOC attending appointments on an interview day were approached for interview. The response rate was 58% and represented 47% of the total WOC in the clinic and did not differ from the clinic population on sociodemographic variables. The survey questions were read to participants by trained interviewers who entered their responses into computers. Participants received a $25 gift card for their time and research protocols were approved by the site Institutional Review Board.
Basic Needs Satisfaction in General Scale
The Basic Needs Satisfaction in General (BNSG) Scale is a 21-item scale aimed at capturing autonomy, relatedness, and competency associated with self-determination and has been used with diverse samples (Gagne, 2003). The response options were changed from 7-items to 4-items (“never true,” “sometimes true,” “often true,” or “almost always or always true”) to facilitate ease of use. The autonomy scale included 7 items (range 7–28); relatedness included 8 items (range 8–32) and competency included 6 items (range 6–24). Negatively-framed items were reverse-coded. Summed scores were used as continuous outcomes.
Independent variables
Socio-demographic Variables
Insurance status was dichotomized to private insurance vs. no private insurance; employment was dichotomized as unemployed vs. any employment; and housing was categorized as institutional, a non-permanent setting or a permanent setting in order to include an indicator of personal resources.
Co-morbidities
The HIV Symptom Index (Justice et al., 2001) is a 20-question scale that asks about general health issues in the past 4 weeks. Anxiety and depression questions (n=3) were examined separately. Answers ranged from 1 (“I don’t have this symptom”) to 5 (“It bothers me a lot”). Depression was assessed with the PHQ-9 (Kroenke et al., 2001). PHQ-9 subscales (affective: anhedonia, depression, guilt, suicidality; somatic: sleep, fatigue, appetite, activity, concentration) were constructed to separate somatic symptoms that may result from HIV infection or treatment. Women also reported if they currently use alcohol (yes or no) and if they ever used drugs (yes or no).
Social environment
A modified version of the Barriers to Care Scale (Heckman et al., 1998) was used. The medical self-advocacy scale (12 items) captured communication with providers (Brashers et al., 1999) and coded with higher scores corresponding to more active communication. The availability of support, care and guidance for HIV care was assessed using the Treatment-Specific Social Support (TSSS) scale, a modified 12-item subset of the Social Provisions Scale (Myers & Durvasula, 1999; Thames et al., 2012). Responses ranged from 1 (“strongly disagree”) to 4 (“strongly agree”). Perceived emotional and practical social support available from friends and others was captured as a 7-item subset of the Social Relationships Scale (O'Brien et al., 1993).
Abuse environment
The Index of Psychological Abuse Scale (IPA Scale) captured frequency of experiences (never to often) of ridicule, harassment, criticism, and emotional withdrawal from their partner (Sullivan & Bybee, 1999). A trauma scale developed for use in a variety of settings (personal communication, K. Sikkema) included childhood-specific and adult-oriented trauma questions. Responses were summed and options revised to “never” (0), “once” (1) or “more than once” (2).
Data analysis
Means and standard deviations of the continuous variables, counts and percentages of the categorical variables were created. Each of these scales was modeled as continuous predictors in our model. Scale properties were examined, including Cronbach’s alphas for scale reliability. Spearman pairwise correlations assessed the relationships among the scales. Linear regression was used to assess the relationship between each continuous basic needs subscale (autonomy, competency, relatedness) and potential correlates.
Models were adjusted for age, education, employment, housing (dichotomized as permanent vs. all others) and insurance status; beta coefficients and 95% confidence intervals are reported.
RESULTS
Study participants (n=189) were WOC attending a medical visit in an academic infectious diseases clinic (Table 1). Their average age was 46 years, 37% were older than 50 years old; and 28% had less than a high school education; 14% had private insurance, most were unemployed (71%), and lived in permanent housing (89%).
TABLE 1.
Socio-demographic characteristics of WOC enrolled in baseline sample. (N=189).
| Socio-demographic Characteristics | |
|---|---|
| Age | N (%) |
| Continuous age [mean (sd)] | 46 (10.4) |
| <30 | 12 (6.4%) |
| 30–39 | 41 (21.7%) |
| 40–49 | 67 (35.5%) |
| 50+ | 69 (36.5%) |
| Education Years | |
| Continuous education [mean (sd)] | 12.0 (2.0) |
| < 12 years | 53 (28.0%) |
| = 12 years | 69 (36.5%) |
| >12 years | 67 (35.5%) |
| Insurance Status | |
| Public or Uninsured | 157 (83.1%) |
| Private | 26 (13.8%) |
| Missing | 6 (3.2%) |
| Employment Status | |
| Unemployed | 134 (70.9%) |
| Full or Part Time | 55 (29.1%) |
| Housing | |
| Institution | 8 (4.2%) |
| Non-permanent | 13 (6.9%) |
| Permanent | 168 (88.9%) |
Statements about satisfaction of autonomy needs (Table 2) had mixed responses when WOC were asked to indicate how accurately these statements described their own experiences. The majority of women reported that they usually had the ability to make their own decisions, as 66% agreed with the positively framed statement (“decide for myself”) and 75% rejected the negatively framed statement (“not much opportunity to decide”). However autonomy satisfaction was much lower when statements regarding interactions with others were asked, as 23% agreed that they “have to do what told”. Only 30% reported that it was almost always true that others took their feelings into consideration.
TABLE 2.
Autonomy, relatedness and competency basic needs reported by WOC in baseline sample. (N=189)
| Basic Needs Satisfaction in General | Not at all true | Some-times true | Often true | Almost always true |
|---|---|---|---|---|
| AUTONOMY SCALE | N (%) | N (%) | N (%) | N (%) |
| Positive framing | ||||
| … am free to decide for myself how to live … | 7 (3.7) | 25 (13.2) | 32 (16.9) | 125 (66.1) |
| … feel free to express ideas … | 6 (3.2) | 36 (19.1) | 55 (29.1) | 92 (48.7) |
| …People .. tend to take my feelings into consideration. | 19 (10.1) | 64 (33.9) | 49 (25.9) | 57 (30.6) |
| …can pretty much be myself in daily situations | 9 (4.8) | 25 (13.2) | 48 (25.4) | 107 (56.6) |
| Negative framing | ||||
| … feel pressured … | 89 (47.1) | 66 (34.9) | 18 (9.5) | 16 (8.5) |
| … have to do what I am told … | 91 (48.2) | 53 (28.0) | 22 (11.6) | 23 (12.2) |
| … not much opportunity for me to decide … | 142 (75.1) | 30 (15.9) | 13 (6.9) | 4 (2.1) |
| RELATEDNESS SCALE | N (%) | N (%) | N (%) | N (%) |
| Positive framing | ||||
| … like the people I interact with | 4 (2.1) | 39 (20.6) | 45 (23.8) | 101 (53.4) |
| … get along with people … | 1 (0.5) | 27 (14.3) | 50 (26.5) | 111 (58.7) |
| …I consider people … to be my friends | 26 (13.8) | 59 (31.2) | 39 (20.6) | 65 (34.4) |
| …People… care about me | 4 (2.1) | 27 (14.3) | 36 (19.1) | 122 (64.6) |
| … generally pretty friendly to me | 6 (3.2) | 31 (16.4) | 57 (30.2) | 95 (50.3) |
| Negative framing | ||||
| … don’t have a lot of social contacts… | 47 (24.9) | 47 (24.9) | 44 (23.3) | 54 (27.0) |
| … not many people that I am close to | 65 (34.4) | 39 (20.6) | 40 (21.2) | 45 (23.8) |
| … people … do not seem to like me much. | 133 (70.4) | 39 (20.6) | 10 (5.3) | 6 (3.2) |
| COMPETENCY SCALE | N (%) | N (%) | N (%) | N (%) |
| Positive framing | ||||
| … People … tell me I’m good at what I do | 12 (6.4) | 33 (17.5) | 64 (33.9) | 80 (42.3) |
| … able to learn interesting new skills.. | 38 (20.1) | 43 (22.8) | 51 (27.0) | 57 (30.2) |
| … feel a sense of accomplishment … | 9 (4.8) | 44 (23.3) | 63 (33.3) | 73 (38.6) |
| Negative framing | ||||
| … do not feel very competent | 96 (50.8) | 58 (30.7) | 23 (12.2) | 12 (6.4) |
| … do not get much … chance to show how capable I am | 83 (43.9) | 62 (32.8) | 30 (15.9) | 14 (7.4) |
| … do not feel very capable | 120 (63.5) | 47 (24.9) | 13 (6.9) | 9 (4.8) |
= 1 missing
Responses to relatedness statements were more evenly divided between agreement with and disagreement with the statements whether or not they were positively or negatively framed. The majority of WOC reported getting along with the people. However a number of WOC endorsed negative feelings (22% disagreed with “like the people I interact with” and 45% did not consider them friends). They also reported low numbers of contacts with others by agreeing with “don't have a lot of social contacts” (50%) and “not many people that I am close to” (45%).
Only a single statement of competency was endorsed by a majority of the WOC. The negatively framed statements “… do not feel capable” and “do not feel competent”) were endorsed by 36% and 49% respectively. At least 20% of the subjects rejected statements supporting their competency (24% “good at what I do”; 43% “able to learn new skills”; 28% “feel sense of accomplishment”). Overall feelings of competency were reported less frequently by the WOC.
Moderate levels of internal consistency were seen with the self-determination scores (Table 3). Cronbach’s alpha was 0.63 for autonomy, 0.61 for competency and 0.75 for relatedness. These moderate alphas suggest that the scale is not unidimensional but instead might be measuring more than one latent construct. A brief factor analysis of the autonomy (7 items), relatedness (8 items) and competency (6 items) scales did not indicate any one item that loaded particularly high or low (all items altered the scale alpha by ≤5%). Therefore all items were retained to allow comparison with scale results in other populations. The other scales resulted in high levels of internal consistency in this population, ranging from 0.80 for depression screening (PHQ-9) to 0.90 for the index of psychological abuse. The three constructs representing self-determination were reasonably correlated in these data (Table 4), ranging from 0.57 (autonomy to competency) to 0.60 (relatedness to competency). Comorbidities were inversely associated with all three self-determination components, as were the barriers to care scale and the trauma-related measures. Social support, and to a lesser extent, treatment-specific social support, was positively correlated with autonomy, relatedness and competency.
TABLE 3.
Distribution and reliability scores of scales constructed from baseline responses among HIV-infected WOC (n=189)
| Continuous scale | Mean (sd) | Theoretical range |
Observed range |
Cronbach’s alpha |
|---|---|---|---|---|
| Autonomy | 22.7 (3.5) | 7–28 | 11–28 | 0.63 |
| Competency | 18.7 (3.2) | 6–24 | 10–24 | 0.61 |
| Relatedness | 25.0 (4.5) | 8–36 | 13–32 | 0.75 |
| HIV symptom index | 21.5 (13.5) | 0–68 | 0–54 | 0.90 |
| PHQ-9 | 3.1 (3.7) | 0–27 | 0–16 | 0.80 |
| PHQ-4 (affective subscale) | 1.2 (1.8) | 0–12 | 0–9 | 0.69 |
| Barriers to care* | 19.7 (7.4) | 11–44 | 11–40 | 0.85 |
| Self-advocacy scale | 44.3 (6.2) | 12–60 | 24–59 | 0.64 |
| Social support | 24.0 (4.1) | 7–28 | 7–28 | 0.84 |
| Treatment-specific social support | 32.3 (3.3) | 12–48 | 21–43 | 0.87 |
| Index of psychological abuse (IPA)* | 32.7 (10.9) | 21–84 | 21–63 | 0.90 |
| Trauma - Childhood | 19.9 (5.4) | 13–52 | 13–38 | 0.80 |
| Trauma - Adult | 15.2 (3.9) | 9–32 | 9–27 | 0.71 |
Barriers to care and IPA scales were only assessed from April 2010 to December 2010 and n=156 and 152, respectively.
TABLE 4.
Spearman correlation between continuous scales among HIV-infected WOC (n= varies, based on pairwise comparisons)
| A | R | C | HIV Symptoms | PHQ-9 | PHQ-4 | B2C | SA | SS | TSSS | IPA | Trauma- Child | Trauma- Adult | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | 1.00 | ||||||||||||
| R | 0.60 | 1.00 | |||||||||||
| C | 0.57 | 0.60 | 1.00 | ||||||||||
| HIV-symptoms | −0.34 | −0.37 | −0.38 | 1.00 | |||||||||
| PHQ-9 | −0.40 | −0.40 | −0.50 | 0.59 | 1.00 | ||||||||
| PHQ-4 | −0.35 | −0.32 | −0.45 | 0.44 | 0.82 | 1.00 | |||||||
| B2C | −0.30 | −0.28 | −0.36 | 0.37 | 0.27 | 0.23 | 1.00 | ||||||
| SA | 0.12 | 0.03 | 0.03 | −0.02 | 0.19 | 0.14 | 0.07 | 1.00 | |||||
| SS | 0.50 | 0.52 | 0.52 | −0.41 | −0.38 | −0.30 | −0.41 | 0.04 | 1.00 | ||||
| TSSS | 0.03 | 0.12 | 0.08 | −0.10 | 0.03 | 0.00 | −0.10 | 0.03 | 0.19 | 1.00 | |||
| IPA | −0.29 | −0.29 | −0.29 | 0.25 | 0.24 | 0.18 | 0.21 | −0.06 | −0.31 | −0.18 | 1.00 | ||
| Trauma- Child | −0.19 | −0.32 | −0.21 | 0.33 | 0.23 | 0.12 | 0.26 | −0.01 | −0.25 | −0.02 | 0.20 | 1.00 | |
| Trauma-Adult | −0.09 | −0.23 | −0.17 | 0.38 | 0.27 | 0.13 | 0.24 | 0.05 | −0.23 | −0.06 | 0.30 | 0.73 | 1.00 |
Scales: A= autonomy R = relatedness ; C = competency; B2C = barriers to care ; SAS = self-advocacy; HIV-symptoms = HIV symptoms ; SS = social support; TSSS = treatment-specific social support; PHQ-9 = depression screener; PHQ-4 affective questions from the PHQ-9 depression screener (anhedonia, depression, guilt, suicidality); IPA = index of psychological abuse; Trauma-Child= Trauma scale of childhood events; Trauma-Adult= Trauma scale of adult events
The relationship between demographic covariates (age, education, housing, employment and insurance) and self-determination constructs were assessed in multivariate models (Figure 1). Lack of independent housing was associated with a 2 unit decrease in autonomy (β= −2.00; 95%CI= −3.70, −0.40) and a 2.5 unit decrease in relatedness (β= −2.50; 95%CI= −4.50, −0.50) but was not associated with competency (β= −0.30; 95%CI= −1.80, 1.20). In addition, not being employed was associated with a nearly 2-unit decrease in both relatedness and competency (β= −1.83; 95% CI=−0.02, −3.45 and β= −1.62 2; 95% CI= −0.44, −2.80, respectively) but not lower autonomy. Across all the constructs, having less than a high school education was associated with the greatest decreases in self-determination need satisfaction: lower autonomy (β= −1.90; 95%CI= −3.20, −0.60), relatedness (β= −2.70; 95%CI= −4.30, −1.10), and competency (β= −2.50; 95%CI= −3.60, −1.30). Overall, the most profound social disparities – unstable housing, low education and unemployment – were associated with lower levels of basic need satisfaction.
Figure 1.
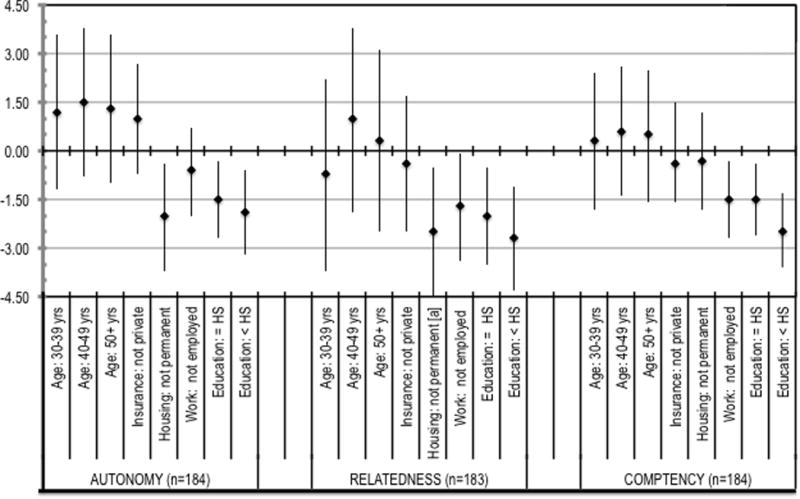
Covariate associations (beta coefficients and 95% confidence intervals) for autonomy, relatedness and competency among HIV-infected WOC as reported at baseline (n = 189). Reference categories: age (<30), education (>12 years), housing (permanent), employment status (employed) and insurance status (private insurance). a = 95%CI: −4.5 to −0.50.
Clinical and social characteristics were also examined for associations with self-determination needs (Figure 2). Both somatic symptoms (reported by HIV symptoms checklist) and psychological symptoms (reported by PHQ-9 affective subscale) were associated with lower need satisfaction. Each 1-unit increase in the somatic symptom scale (per point) was associated with a 0.09 decrement in autonomy, 0.12 decrement in relatedness and a 0.08 decrement in competency satisfaction. In contrast, each 1-unit increase in the PHQ-9 affective subscale was associated with a 0.61 decrement in autonomy, 0.68 decrement in relatedness and a 0.59 decrement in competency satisfaction. The larger change associated with affective rather than somatic symptoms suggests that the associations are more related to the psychiatric processes of depression rather than the physical processes.
Figure 2.
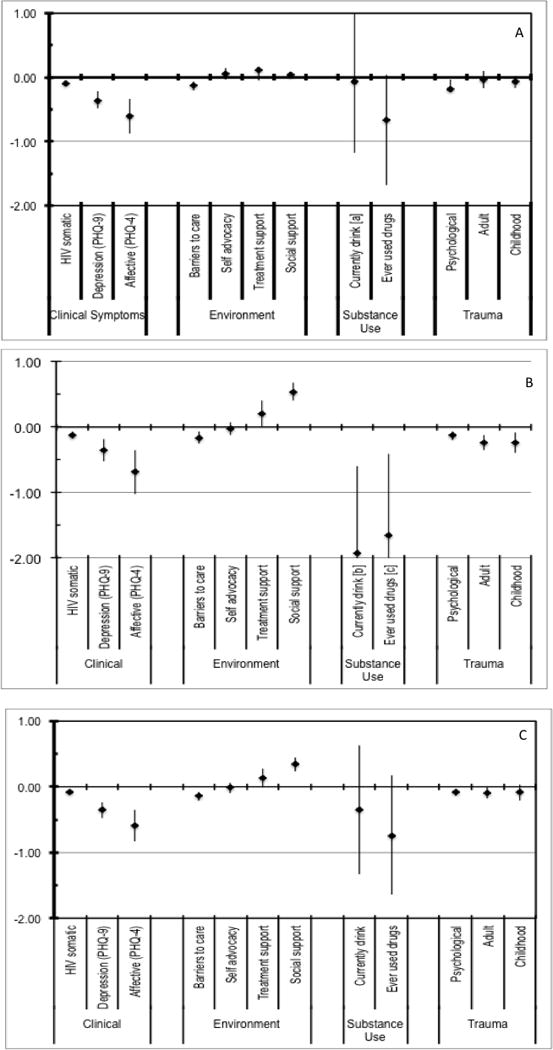
Adjusted beta coefficients and 95% confidence intervals for correlates of self-determination need satisfaction reported by HIV-infected WOC. Models were adjusted for categorical age, categorical education, dichotomous housing, employment and insurance status. N varies in each model. (a) Autonomy satisfaction. a = 95%CI = −1.17 to 1.03 (b) Relatedness satisfaction. a = 95%CI = −3.27 to −0.60; b = 95%CI = −2.89 to −0.41. (c) Competency satisfaction.
The care environment reported by WOC was also related to need satisfaction. Increased barriers to care were associated with loss of need satisfaction (autonomy: −0.13; relatedness: −0.16; competency: −0.13). General social support was consistently associated with satisfaction of needs, especially relatedness (autonomy: 0.04; relatedness: 0.54; competency: 0.34). This is consistent with barriers to care occurring in a social context and that social context is influenced by the relationship experiences of the WOC.
Violence and addiction are common co-occurring illnesses and experiences that overlap with HIV infection and are recognized as syndemic events that effect HIV outcomes including the HIV RNA in HIV-infected WOC (Sullivan et al., 2014). Alcohol and drug use were strongly associated with loss of relatedness (alcohol β= −1.93, 95%CI= −3.27 to −0.60; drug use β= −1.65; 95%CI= −2.89 to −0.41) but neither autonomy nor competency were associated. We measured traumatic experiences as psychological abuse, adult and childhood traumatic experiences. Psychological abuse was associated with a loss of satisfaction for all three needs (autonomy −0.18; relatedness: −0.13; competency: −0.08). Relatedness was the most strongly associated with reports of trauma and was associated with all three measures of violence.
DISCUSSION
In our cohort of HIV-infected WOC, reductions in all three basic need satisfaction were more strongly associated with affective depression symptoms (rather than somatic symptoms). Previously, autonomy satisfaction and to a lesser extent relatedness satisfaction have been shown to be associated with depression in studies conducted in long-term care facilities in Europe (Custers et al., 2010; Ferrand et al., 2014). The current study contributes the observation that the psychological symptoms of depression are the keys aspects of depression in this association. The association between affective clinical symptoms and low need satisfaction suggests an explanation for observations that self-care, including HIV medication adherence, may be impaired by depression.
The social environmental context experienced by the subjects is also related to the satisfaction of autonomy, relatedness and competency needs. This observation is important because social support is a key aspect for access to care (Cooper et al., 2002). Prior research on social support and needs satisfaction included them as joint influences on depression or post-cancer diagnosis resiliency but not on the association of one with the other (Ibarra-Rovillard & Kuiper, 2011; Scrignaro et al., 2011). To our knowledge the relationship between reported social support and basic self-determination needs has not been described in HIV-infected WOC. In addition to promoting a fuller understanding of the social environment in which WOC access HIV care, the observations from our study may be used to inform the development of interventions that provide supportive and care services. Currently many trials are underway using cash incentives as external motivators to motivate care and prevention behaviors in HIV infected or HIV-at-risk populations (Galarraga et al., 2013). Our findings suggest that interventions that focus on provision of material resources but do not address basic need satisfaction may have limited impact.
Low educational attainment (< high school) was the strongest predictor of low basic psychological need satisfaction. Many examples exist of motivation for education being affected by satisfaction of the core needs (cited in (Reeve, 2002)). The analysis presented here tested the reverse relationship (education influencing need satisfaction), however this is a cross-sectional analysis and does not provide directional information about the association. In addition, we do not have information about the duration of the low core need achievements. It is possible that low need satisfaction has been a life-long problem for these WOC, preceding and contributing to low educational attainment.
Two common aspects of trauma are helplessness and loss of autonomy. Consequently, associations between trauma and basic need satisfaction might be expected. WOC in drug treatment court attributed unmet needs for relatedness to a history of trauma and inability to trust individuals (Morse et al., 2014). We also report statistically significant but very small effect sizes between trauma and need satisfaction. The subjects were middle-aged WOC and the traumatic events may have happened at some very distant time, leaving muted effects. Therefore, the potential associations between trauma and basic needs satisfaction should be explored further.
We acknowledge several limitations of the results presented here. First, the consistency of the autonomy, competency and relatedness scales, as indicated by their Cronbach’s alpha, were in the moderate range (0.61–0.75). While not as high as one would like, this level of reliability is similar to prior reports and consistent with prior qualitative work (Quinlivan et al., 2013). Secondly, the WOC represented here, had a mean age of 46 years and almost 40% were over 50 years of age. It is expected that women who are younger may not be represented by this sample. Additionally, the findings of this study are only applicable to those HIV-infected WOC who are in care. WOC who were not in care were not reached by this study, as WOC had to be attending a medical visit to be eligible. R2 values below 0.50 (as reported here) are commonly found when assessing human behavior, which is complex and multifactorial; these assessments of fit do not change the interpretation of the results found with these models. However these R2 values do suggest that there are unmeasured factors, outside autonomy, competency, relatedness, and the included covariates, that explain a portion of the variability observed in our outcomes among these women. Despite these limitations, the selected instruments have been validated and are commonly used. The results are applicable to WOC in care as the 189 WOC interviewed for this report represent 40% of the population of HIV-infected WOC in the study site.
This paper suggests that HIV-infected WOC in medical care have only moderate levels of basic psychological needs satisfaction. Additionally, depression, educational attainment, trauma and social support are key elements associated with the level of need satisfaction reported. Interventions that address the psychological needs, along with the characteristics that influence them, may enhance the motivation for self-care of HIV-infected WOC. Basic need satisfaction and self-care by PLWH should be further explored.
Acknowledgments
This research was supported by funds from HRSA’s Special Projects of National Significance Initiative: Enhancing Engagement and Retention in Quality HIV Care for Women of Color (HA15148) and the Center of AIDS Research at the University of North Carolina at Chapel Hill (P30-AI50410). This study was conducted with the approval of the Institutional Review Boards of the participating institutions. The authors also acknowledge the clinic staff, providers, and patients for their invaluable contributions to this research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Health Resources and Services Administration.
Footnotes
None of the authors have conflicts of interest to report.
References
- Brashers DE, Haas SM, Neidig JL. The patient self-advocacy scale: measuring patient involvement in health care decision-making interactions. Health Commun. 1999;11:97–121. doi: 10.1207/s15327027hc1102_1. [DOI] [PubMed] [Google Scholar]
- Cooper LA, Hill MN, Powe NR. Designing and Evaluating Interventions to Eliminate Racial and Ethnic Disparities in Health Care. Journal of General Internal Medicine. 2002;17:477–486. doi: 10.1046/j.1525-1497.2002.10633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham WE, Andersen RM, Katz MH, Stein MD, Turner BJ, Crystal S, Shapiro MF. The impact of competing subsistence needs and barriers on access to medical care for persons with human immunodeficiency virus receiving care in the United States. Med Care. 1999;37:1270–1281. doi: 10.1097/00005650-199912000-00010. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10599608. [DOI] [PubMed] [Google Scholar]
- Custers AF, Westerhof GJ, Kuin Y, Riksen-Walraven M. Need fulfillment in caring relationships: Its relation with well-being of residents in somatic nursing homes. Aging Ment Health. 2010;14:731–739. doi: 10.1080/13607861003713133. [DOI] [PubMed] [Google Scholar]
- Deci EI. Why we do what we de: understanding self-motivation. New York City: Penguin; 1995. [Google Scholar]
- Deci EL, Ryan RM. The “what” and “why” of goal pursuits: Human needs and the self-determination of behavior. Psychological Inquiry. 2000;11:227–268. doi: 10.1207/S15327965PLI1104_01. [DOI] [Google Scholar]
- Ferrand C, Martinent G, Durmaz N. Psychological need satisfaction and well-being in adults aged 80 years and older living in residential homes: Using a self-determination theory perspective. J Aging Stud. 2014;30:104–111. doi: 10.1016/j.jaging.2014.04.004. [DOI] [PubMed] [Google Scholar]
- Gagne M. The role of autonomy support and autonomy orientation in prosocial behavior engagement. Motivation and Emotion. 2003;27:199–223. Retrieved from http://www.selfdeterminationtheory.org/basic-psychological-needs-scale/ [Google Scholar]
- Galarraga O, Genberg BL, Martin RA, Barton Laws M, Wilson IB. Conditional economic incentives to improve HIV treatment adherence: literature review and theoretical considerations. AIDS Behav. 2013;17:2283–2292. doi: 10.1007/s10461-013-0415-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckman TG, Somlai AM, Peters J, Walker J, Otto-Salaj L, Galdabini CA, Kelly JA. Barriers to care among persons living with HIV/AIDS in urban and rural areas. AIDS Care. 1998;10:365–375. doi: 10.1080/713612410. [DOI] [PubMed] [Google Scholar]
- Houston E, McKirnan DJ, Cervone D, Johnson MS, Sandfort TG. Assessing treatment motivation among patients receiving antiretroviral therapy: a multidimensional approach. Psychol Health. 2012;27:674–687. doi: 10.1080/08870446.2011.618536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibarra-Rovillard MS, Kuiper NA. Social support and social negativity findings in depression: perceived responsiveness to basic psychological needs. Clin Psychol Rev. 2011;31:342–352. doi: 10.1016/j.cpr.2011.01.005. [DOI] [PubMed] [Google Scholar]
- Igreja I, Zuroff D, Koestner R, Saltaris C, Brouillette M, Lalonde R. Applying self-determination theory to the prediction of distress and well-being in gay men with HIV and AIDS. J Appl Soc Psychol. 2000;30:686–706. doi: 10.1111/j.1559-1816.2000.tb02819.x. [DOI] [Google Scholar]
- Johnson VD. Promoting behavior change: making healthy choices in wellness and healing choices in illness - use of self-determination theory in nursing practice. Nurs Clin North Am. 2007;42:229–241. doi: 10.1016/j.cnur.2007.02.003. [DOI] [PubMed] [Google Scholar]
- Johnson WD, Diaz RM, Flanders WD, Goodman M, Hill AN, Holtgrave D, McClellan WM. Behavioral interventions to reduce risk for sexual transmission of HIV among men who have sex with men. Cochrane Database Syst Rev. 2008:CD001230. doi: 10.1002/14651858.CD001230.pub2. [DOI] [PubMed] [Google Scholar]
- Johnston MM, Finney SJ. Measuring basic needs satisfaction: Evaluating previous research and conducting new psychometric evaluations of the basic needs satisfaction in general scale. Contemp Educ Psychol. 2010;35:280–296. Retrieved from http://www.selfdeterminationtheory.org/domains/basic-psychological-needs-domain/ [Google Scholar]
- Justice AC, Holmes W, Gifford AL, Rabeneck L, Zackin R, Sinclair G, Adult AIDS Clinical Trials Unit Outcomes Committee Development and validation of a self-completed HIV symptom index. J Clin Epidemiol. 2001;54:S77–90. doi: 10.1016/s0895-4356(01)00449-8. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11750213. [DOI] [PubMed] [Google Scholar]
- Kennedy S, Goggin K, Nollen N. Adherence to HIV medications: Utility of the theory of self-determination. Cognitive therapy and research. 2004;28:611–628. doi: 10.1023/B:COTR.0000045568.95219.e2. [DOI] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11556941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynam I, Catley D, Goggin K, Rabinowitz JL, Gerkovich MM, Williams K, Wright J. Autonomous regulation and locus of control as predictors of antiretroviral medication adherence. J Health Psychol. 2009;14:578–586. doi: 10.1177/1359105309103577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messer LC, Quinlivan EB, Parnell H, Roytburd K, Adimora AA, Bowditch N, DeSousa N. Barriers and facilitators to testing, treatment entry, and engagement in care by HIV-positive women of color. AIDS Patient Care STDS. 2013;27:398–407. doi: 10.1089/apc.2012.0435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morse DS, Cerulli C, Bedell P, Wilson JL, Thomas K, Mittal M, Chin N. Meeting health and psychological needs of women in drug treatment court. J Subst Abuse Treat. 2014;46:150–157. doi: 10.1016/j.jsat.2013.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morse DS, Schiff M, Levit S, Cohen-Moreno R, Williams GC, Neumark Y. A pilot training program for a motivational enhancement approach to hepatitis C virus treatment among individuals in Israeli methadone treatment centers. Subst Use Misuse. 2012;47:56–66. doi: 10.3109/10826084.2011.628735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers HF, Durvasula RS. Psychiatric disorders in African American men and women living with HIV/AIDS. Cultur Divers Ethnic Minor Psychol. 1999;5:249–262. doi: 10.1037/1099-9809.5.3.249. [DOI] [Google Scholar]
- O’Brien K, Wortman CB, Kessler RC, Joseph JG. Social relationships of men at risk for AIDS. Soc Sci Med. 1993;36:1161–1167. doi: 10.1016/0277-9536(93)90236-w. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8511645. [DOI] [PubMed] [Google Scholar]
- Quinlivan EB, Messer LC, Adimora AA, Roytburd K, Bowditch N, Parnell H, Pierce JK. Experiences with HIV Testing, Entry, and Engagement in Care by HIV-Infected Women of Color, and the Need for Autonomy, Competency, and Relatedness. AIDS Patient Care STDS. 2013;27:408–415. doi: 10.1089/apc.2012.0434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reeve J. Self-determination theory applied to educational settings. In: Deci E, Ryan R, editors. Handbook of self-determination research. Rochester, NY, US: University of Rochester Press; 2002. pp. 183–203. [Google Scholar]
- Russell KL, Bray SR. Promoting self-determined motivation for exercise in cardiac rehabilitation: the role of autonomy support. Rehabil Psychol. 2010;55:74–80. doi: 10.1037/a0018416. [DOI] [PubMed] [Google Scholar]
- Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist. 2000;55:68–78. doi: 10.1037//0003-066x.55.1.68. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11392867. [DOI] [PubMed] [Google Scholar]
- Scrignaro M, Barni S, Magrin ME. The combined contribution of social support and coping strategies in predicting post-traumatic growth: a longitudinal study on cancer patients. Psycho-Oncology. 2011;20:823–831. doi: 10.1002/pon.1782. [DOI] [PubMed] [Google Scholar]
- Sullivan CM, Bybee DI. Reducing violence using community-based advocacy for women with abusive partners. J Consult Clin Psychol. 1999;67:43–53. doi: 10.1037//0022-006x.67.1.43. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10028208. [DOI] [PubMed] [Google Scholar]
- Sullivan KA, Messer LC, Quinlivan EB. Substance abuse, violence, and HIV/AIDS (SAVA) syndemic effects on viral suppression among HIV positive women of color. AIDS Patient Care STDS, e-publication. 2014 doi: 10.1089/apc.2014.0278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thames AD, Moizel J, Panos SE, Patel SM, Byrd DA, Myers HF, Hinkin CH. Differential predictors of medication adherence in HIV: findings from a sample of African American and Caucasian HIV-positive drug-using adults. AIDS Patient Care STDS. 2012;26:621–630. doi: 10.1089/apc.2012.0157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toth M, Messer LC, Quinlivan EB. Barriers to HIV care for women of color living in the southeastern US are associated with physical symptoms, social environment, and self-determination. AIDS Patient Care STDS. 2013;27:613–620. doi: 10.1089/apc.2013.0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webel AR, Cuca Y, Okonsky JG, Asher AK, Kaihura A, Salata RA. The impact of social context on self-management in women living with HIV. Soc Sci Med. 2013;87:147–154. doi: 10.1016/j.socscimed.2013.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams GC, Deci EL. Internalization of biopsychosocial values by medical students: a test of self-determination theory. J Pers Soc Psychol. 1996;70:767–779. doi: 10.1037//0022-3514.70.4.767. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8636897. [DOI] [PubMed] [Google Scholar]
- Williams GC, Freedman ZR, Deci EL. Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care. 1998;21:1644–1651. doi: 10.2337/diacare.21.10.1644. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9773724. [DOI] [PubMed] [Google Scholar]
- Williams GC, Gagne M, Ryan RM, Deci EL. Facilitating autonomous motivation for smoking cessation. Health Psychol. 2002;21:40–50. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11846344. [PubMed] [Google Scholar]
- Williams GC, Grow VM, Freedman ZR, Ryan RM, Deci EL. Motivational predictors of weight loss and weight-loss maintenance. J Pers Soc Psychol. 1996;70:115–126. doi: 10.1037//0022-3514.70.1.115. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8558405. [DOI] [PubMed] [Google Scholar]
- Williams GC, Patrick H, Niemiec CP, Ryan RM, Deci EL, Lavigne HM. The Smoker’s health project: A self-determination theory intervention to facilitate maintenance of tobacco abstinence. Contemporary Clinical Trials. 2011;32:535–543. doi: 10.1016/j.cct.2011.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams GC, Rodin GC, Ryan RM, Grolnick WS, Deci EL. Autonomous regulation and long-term medication adherence in adult outpatients. Health Psychol. 1998;17:269–276. doi: 10.1037//0278-6133.17.3.269. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9619477. [DOI] [PubMed] [Google Scholar]
- Wilson PM, Rodgers WM. The relationship between perceived autonomy support, excersie regulations and behavioral interventions in women. Psychology of Sport and Exercise. 2004;5:229–242. doi: 10.1016/S1469-0292(03)00003-7. [DOI] [Google Scholar]


