One in nine women in the United Kingdom will develop breast cancer.1 The surgical treatment of these patients will involve either breast conserving surgery or mastectomy, both of which can result in considerable asymmetry of the breasts. Breast reconstruction offers restoration of breast symmetry to such women, achieved by creating a breast mound that is similar in size, shape, contour, and position to the opposite breast. Women thus gain the freedom to wear a variety of clothing, without needing external breast prostheses, and have been shown to have less psychological morbidity than those who have mastectomy without reconstruction.2
Here we review the indications, timing, principles, and techniques of breast reconstruction in patients who need tumour ablative surgery. We concentrate predominantly on women who have had mastectomies.
Sources and selection criteria
We searched Medline and the Cochrane database search by using the term “breast reconstruction.” We reviewed abstracts and selected articles that were relevant to our review subheadings. We selected only articles written in English and those up to October 2004.
Indications for breast reconstruction
Breast reconstruction is increasingly an integral aspect of the management of patients with breast cancer. Some patients, who have had radical tumour resections, may simply need wound closure. Typically, however, breast reconstruction is an option.
Suitable candidates are those who have, or are expected to have, considerable asymmetry of the breasts after tumour ablative surgery. The vast majority of reconstructions are therefore done in patients having a mastectomy, who should be counselled about reconstructive options before their surgery.3 Even women with locally advanced disease may be suitable for breast reconstruction and should not be excluded.4 Contraindications include metastatic disease and anaesthetic risk factors such as significant cardiopulmonary disease.
Principles of breast reconstruction
Mastectomy involves the removal of breast tissue, varying amounts of skin, and, invariably, the nipple-areola complex. The removal of these tissues results in the loss of volume, shape, and contour of the breast. Breast reconstruction aims to restore these attributes and uses the opposite breast as an aesthetic reference point. The process of reconstruction typically involves:
Reconstruction of the breast mound—excision of breast tissue results in loss of breast volume (that is, size) and breast shape, both of which can be recreated with a variety of reconstructive techniques, although matching the other breast may not be possible with all methods
Reconstruction of skin—this is needed in most cases and can be achieved by using local skin or by transferring skin from distant sites to the anterior chest wall. As mastectomy techniques have evolved, the amount of skin needed in breast reconstruction has decreased. This is particularly true of skin sparing mastectomy.
Summary points
The indications for breast reconstruction are wide
Breast reconstruction may be done by breast surgeons or by plastic surgeons
The process of reconstruction usually requires multiple operations
A wide spectrum of reconstructive techniques may be used in breast reconstruction
Radiotherapy can increase the complications of breast reconstruction and adversely affect aesthetic outcomes
Further reconstructive surgery is optional and can involve nipple-areola reconstruction and, in some cases, surgery on the other breast, which is needed if symmetry has not been achieved. The process of breast reconstruction thus involves multiple surgical procedures, and both patients and surgeons need to be highly motivated.
Skin sparing mastectomy
The technique of skin sparing mastectomy has greatly improved the aesthetic outcomes possible with breast reconstruction. It is oncologically safe in selected T1/T2 tumours and allows mastectomy with preservation of the natural breast skin envelope andinfra-mammary fold.5 Breast tissue is excised through limited skin incisions, which may simply be circumareola in nature. Although more time consuming than traditional methods, this technique permits maximal preservation of skin and provides excellent cosmetic results when combined with immediate reconstruction.
Objectives, timing, and techniques for breast reconstruction
Objectives
Restore symmetry by recreating volume, shape, contour, and position of the breast mound, taking the opposite breast as the aesthetic reference
Timing
Immediate
Delayed
Techniques
Non-autologous methods
Fixed volume breast implants
Breast expanders
Combination of non-autologous and autologous methods
• Latissimus dorsi flap with breast implants
Purely autologous methods
Extended latissimus dorsi flap
Transverse rectus abdominus myocutaneous (TRAM) flap
Deep inferior epigastric artery perforator (DIEP) flap
Superior gluteal artery perforator (SGAP) flap
Oncoplastic methods
Breast reduction techniques
Breast lift techniques
Timing of reconstruction
Reconstruction may be either immediate, at the time of mastectomy, or delayed until after adjuvant treatment. Traditionally, breast reconstruction was done as a delayed procedure. However, increasing evidence of the benefits, and in particular the oncological safety,6-8 of immediate reconstruction has led to it becoming the first choice of treatment in many centres. The advantages of immediate reconstruction include reduced cost and superior cosmetic results.9,10 Patients also have less psychological morbidity than those who have delayed reconstruction.11
Immediate reconstruction may not be appropriate for all patients, however, for several reasons. Some women are so overwhelmed by the diagnosis of breast cancer that they are unable to make an informed decision on immediate reconstruction. Such patients are probably best managed with a delayed reconstruction, with the initial emphasis being on tumour ablation. In addition, the timing of reconstruction needs careful consideration in patients due to have adjuvant radiotherapy, as this can adversely affect the outcomes of immediate procedures.12 Finally, not all patients will have access to a surgeon familiar with the spectrum of reconstructive techniques at the time of mastectomy, and some may therefore have to have delayed reconstruction.
Reconstructive techniques
Reconstructive techniques (box) can be divided into:
Non-autologous methods that use breast implants
Autologous methods in which the patient's own tissues are used
A combination of autologous and non-autologous methods
Oncoplastic techniques.
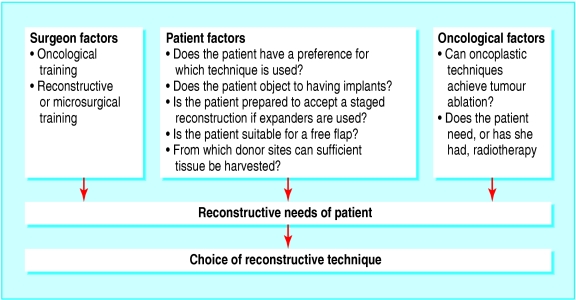
These techniques pose a spectrum of surgical challenges for the reconstructive surgeon, from the relatively straightforward insertion of breast implants to the technically demanding free flaps, which involve microvascular surgical techniques. The decision as to which technique to use is multifactorial. First and fore-most, the choice has to address the patient's individual reconstructive needs, by being able to restore attributes lost during tumour ablative surgery. However, as fig 1 illustrates, several additional factors need to be taken into account. Of particular concern is whether a patient needs or has had radiotherapy, which leads to higher rates of complications with non-autologous methods.13 In contrast, superior aesthetic results are seen in such patients when autologous methods are used.14
Fig 1.
Choosing a reconstructive technique
Non-autologous breast reconstruction
Breast implants
Breast implants may have a fixed volume or their volume may be adjustable, in which case they are known as breast expanders. Both are used in breast reconstruction.
Fixed volume implants
Fixed volume breast implants are a useful means of restoring breast volume in breast reconstruction, but, unlike breast expanders, they do not create additional skin. This limits their use to either reconstructing breasts that are small in volume and minimally ptotic or augmenting the volume of autologous reconstructions such as the latissimus dorsi flap. In both cases sufficient skin is present to obtain complete coverage of the prosthesis. Despite these restrictions, fixed volume implants offer a simple and effective method of reconstruction in selected patients; benefits include shorter general anaesthesia and hospital stays compared with purely autologous methods.
Potential complications of fixed volume breast implants (and breast expanders) include malposition, infection, deflation, extrusion, rupture, and capsule formation with contracture. In capsular contracture, scar tissue forms around the breast implant and contracts, which can result in pain and loss of breast contour. Capsular contracture can be reduced by the use of implants with a textured shell15 and by positioning implants in a subpectoral muscle pocket. Higher rates of capsular contracture are seen in patients who have post-reconstruction radiotherapy.13
Breast expanders
Breast expanders are in effect inflatable breast implants and are often called Becker implants. Injection of saline into the implant, typically through a remote port (fig 2), allows the volume to be adjusted. When used in breast reconstruction they can not only recreate breast volume but also create additional skin. Suitable candidates are women with a relative lack of skin post-mastectomy and whose other breast is small and minimally ptotic.
Fig 2.
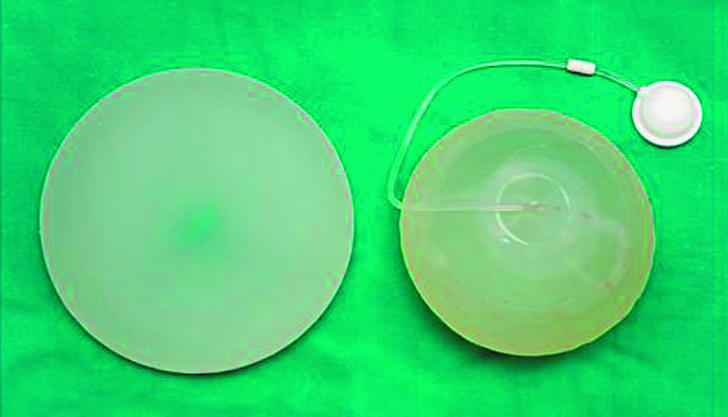
Fixed volume silicone breast implant (left), with an expandable implant for comparison. Note the remote port into which saline is injected. Patients occasionally complain of discomfort from the port, which is placed subcutaneously so as to be readily palpable
The expander, which the surgeon places in a subpectoral pocket, is subsequently inflated in an outpatient setting. This inflation causes stretching of the overlying tissue and allows skin gain by a combination of stretching and mitosis. The expanded skin is sensate and has the same colour and texture as local skin. The process of inflation is started after wounds are healed and usually repeated on a weekly basis, continuing until a volume is reached that not only matches but exceeds the opposite breast. This overexpansion aims to recreate a degree of ptosis in the expanded breast, and therefore a more natural shape and contour.
When inflation is complete, expanders may be exchanged for fixed volume breast implants or the expander may be left in place with only the remote port being removed. A realistic time frame for this method of reconstruction is therefore approximately 6-9 months. This form of breast reconstruction requires a commitment to regular outpatient visits, is classically a two staged procedure, and can involve revision surgery in up to 30% of patients.16
Silicone and breast reconstruction
Adverse publicity about the safety of silicone gel filled implants, in particular a possible association with connective tissue diseases, has led to concern among patients needing breast reconstruction. Although the Food and Drug Administration Board in the United States imposed a moratorium on the use of silicone gel filled implants in 1992, no such moratorium has ever been imposed in the United Kingdom.
The Department of Health commissioned several independent reviews of the hazards of breast implants, the last in 1998. These concluded that no increase in connective tissue diseases occurred in patients with silicone gel implants. This was confirmed by a subsequent meta-analysis, which found no evidence of an increase in breast cancer among women with implants.17
As a result of the reviews, the National Breast Implant Registry, based in Salisbury, was created. This is a prospective register of women having implant surgery. This registry has been used to facilitate research projects and has identified 2400 recipients of the now withdrawn Trilucent breast implants.18
Autologous breast reconstruction
Autologous reconstruction relies on the transfer of flaps of tissue from donor sites to the anterior chest wall. These flaps can be transferred still attached to their original blood supply, when they are known as pedicled flaps; or as free flaps, in which tissue is isolated, transferred, and anastamosed to recipient blood vessels by microsurgical techniques. Here we discuss several commonly used flaps.
Transverse rectus abdominus myocutaneous flap
The transverse rectus abdominus myocutaneous (TRAM) flap and its variants constitute the gold standard for breast reconstruction. This is because better cosmetic results are generally achievable with this technique than with other methods of reconstruction. This flap also permits large ptotic breasts to be reconstructed without recourse to breast implants.
Although a pedicled version of this flap exists, it has been superseded by the free TRAM flap. This has a more reliable blood supply and consequently a reduced rate of complications such as partial flap loss and fat necrosis (which can affect aesthetic outcome).
The free flap consists of a large ellipse of skin and underlying fat from the lower abdomen, together with a portion of the rectus abdominis muscle. The muscle is incorporated because it acts as a vehicle for perforating blood vessels that supply the overlying skin and fat and that originate from the deep inferior epigastric artery. Disadvantages of the free TRAM flap include an average operation time of 4-6 hours, a risk of total flap failure of between 0.4% and 5.0%,19,20 and, because a portion of rectus muscle and fascia is harvested, an abdominal hernia rate of up to 11.6%.20
Deep inferior epigastric artery perforator flap
The deep inferior epigastric artery perforator (DIEP) flap (fig 3) is a refinement of the free TRAM flap and represents an important advance in autologous breast reconstruction. It has replaced the free TRAM as the autologous flap of choice in many centres, because of its reduced donor site morbidity. By dissecting free perforating blood vessels that traverse the rectus muscle, the flap can be raised without sacrificing any rectus muscle. As a result the DIEP flap consists of only lower abdominal skin and fat.
Fig 3.


Top: Left skin sparing mastectomy with immediate DIEP flap reconstruction. Note abdominal donor site scar, which would be similar to that seen in a TRAM flap and can be hidden by underwear. Bottom: The nipple in this patient has been reconstructed with a local flap
Despite being technically demanding (approximately 1.5 hours added to the operation time), the DIEP flap has all the advantages of the free TRAM flap but has a lower incidence of abdominal hernias and weakness.21 Complication rates are otherwise comparable to those seen with the TRAM flap.21
Latissimus dorsi flap
The latissimus dorsi myocutaneous flap (fig 4, top) is an example of a pedicled flap. Based on the thoracodorsal blood vessels, it is a robust flap that can be used to reconstruct small to moderate sized breasts. In its classic form, a paddle of skin, with underlying subcutaneous fat and part of the latissimus dorsi muscle, is raised and transposed to the anterior chest wall. Both volume and skin can be reconstructed with this technique, although a breast implant is invariably needed to achieve adequate volume reconstruction.
Fig 4.


Top: Immediate left breast reconstruction with latissimus dorsi flap reconstruction; the patient has also had the nipple-areola complex reconstructed. Bottom: Donor site scar, seen on left of photograph, located in bra strap line
The extended latissimus dorsi flap, by comparison, allows a completely autologous method of breast reconstruction. Extra volume is created by including all the latissimus muscle and most of its overlying fat.
Complications of the latissimus dorsi flap are primarily related to the donor site and the implant. Donor site seroma are common, occurring in up to 80% of patients,22 and may need draining in an outpatient setting. The stitching of donor site flaps to the underlying tissues, by a technique known as “quilting,” has, however, been shown to significantly reduce seroma formation.22,23 One study showed a reduction in seroma rates from 56% to 0% after the technique was introduced23. The scar on the back is acceptable to most patients and can be located in the bra line (fig 4, bottom).
Superior gluteal artery perforator flap
The superior gluteal artery perforator (SGAP) flap may be used in thin patients who have insufficient abdominal tissue for a DIEP flap. The flap, which is harvested from the buttock, consists of skin and fat only. This produces a scar that is easily hidden by underwear and is therefore readily accepted by patients.
Additional educational resources
Useful websites for doctors
Emedicine (www.emedicine.com/plastic/BREAST.htm)—a selection of review articles on techniques involved in breast reconstruction
Center for Microsurgical Breast Reconstruction (www.diepflap.com)—commercial website providing information on a wide selection of perforator flap reconstructions, with access to peer reviewed publications on perforator based breast reconstruction
Silicone gel breast implants (www.silicone-review.gov.uk)—detailed report by the Independent Review Group on the safety of silicone breast implants
Center for Restorative Breast Surgery (www.centerforrestoration.com)—commercial website on breast reconstruction with an excellent section containing peer reviewed publications of breast reconstruction
Medline Plus (www.nlm.nih.gov/medlineplus/breastreconstruction.html)—excellent resource with a wealth of information and articles
Useful websites for patients
Royal Marsden NHS Trust (www.royalmarsden.org)—website of Europe's largest comprehensive cancer centre, providing concise text based information for patients
Breast Cancer Care (www.breastcancercare.org.uk)—comprehensive text and pictorial overview of reconstruction
Cancer BACUP (www.cancerbacup.org.uk)—website of registered charity, with comprehensive text and pictorial overview of reconstruction
Breastcancer.org (www.breastcancer.org)—excellent text and pictorial overview of breast reconstruction, with booklets and chat rooms for patients
Department of Health (www.dh.gov.uk)—covers government policy on silicone implants, with downloadable informational leaflet for women having silicone implants (www.dh.gov.uk/assetRoot/04/01/45/74/04014574.pdf)
Oncoplastic techniques
If the tumour lies within the area of breast that is usually excised during a reduction or mastopexy (breast lift) operation, then these procedures themselves can achieve both wide local excision of the tumour and reconstruction of the affected breast. Symmetry can then be restored by breast reduction or mastopexy of the other breast.
Nipple-areola reconstruction
Although reconstruction of the nipple-areola complex is an optional procedure, it significantly improves patients' satisfaction with breast reconstruction.24 In our centre it is typically done six months after reconstruction of the breast mound. Nipple reconstruction can be done with a variety of techniques, including nipple sharing, in which a part of the nipple from the opposite breast is grafted to the reconstructed breast, and the use of local flaps. Both can be done under local anaesthetic as day case procedures. The areola is now commonly reconstructed with intradermal tattooing.
Contralateral breast surgery
Contralateral breast surgery is used when breast reconstruction has not achieved symmetry. It may involve breast reduction, breast mastopexy, or augmentation by implant of the opposite breast.
Further surgery
Further surgery can involve procedures to improve both the volume and contour symmetry of the breasts; scar revision, including that of donor sites; further areolar tattooing (because of the propensity of currently used pigments to fade); and secondary procedures to improve nipple height. Patients should be counselled that several operations may be needed to complete the breast reconstruction process. They should also be informed that delayed reconstruction, the need for radiotherapy, and any complication of the primary procedure may all lead to an increase in the number of operative procedures needed to complete the reconstructive process.25
Conclusion
Breast reconstruction has become an integral aspect of breast cancer management. It can be done safely and effectively either at the time of tumour ablative surgery or as a delayed procedure. Irrespective of the timing of reconstruction, a spectrum of techniques is available from which the patient and surgeon can choose.
These techniques can involve breast implants, autologous tissue, or both. Implant based techniquesare a simple and effective method of breast reconstruction, but they may not be suitable for all patients, particularly those who need or have had radiotherapy. Autologous methods in contrast are more surgically demanding, but they consistently yield better aesthetic results than non-autologous methods, particularly when combined with skin sparing mastectomy.
A patient's perspective
The bad news was that I had been diagnosed as having breast cancer and I needed to have a mastectomy. The good news was that I was lucky enough to be referred to a plastic surgeon who explained what was available to me by way of a breast reconstruction. There were several options, but the one I went for involved using fat tissue harvested from my abdomen to construct a new breast.
I was taken to the operating theatre early in the morning, and my surgeon, together with his team, took several hours creating a new breast, while at the same time giving me a tummy tuck and a new belly button.
On coming round from the anaesthetic, I felt like I had been hit by a train. I was put into a small side ward with my reconstructed breast covered with a blanket, and I was kept extremely warm for the next couple of days, because the success of the procedure depended on the blood supply to the replacement breast tissue being maintained. I discovered that I could hardly move as I had various drains and drips attached to my torso. Although this was uncomfortable, I felt no real pain, and during the next few days these were gradually removed.
My reconstruction was a complete success, and I left hospital after nine days. As it had been necessary to remove the nipple during the procedure, I returned to hospital six months later and my surgeon created a new one, which was “the icing on the cake.”
Three months after my operation I was sunbathing in a bikini. What a result.
JW, 59 year old patient who had a left skin sparing mastectomy with immediate DIEP flap reconstruction
We thank Peter Shakespeare, Valerie Shakespeare, and Jawad Khan for their helpful comments during the preparation of this manuscript. We also thank Nigel Horlock for his help in selecting appropriate photographs for this paper, and of course the patients themselves.
Contributors: SA, AS, and MB wrote the commentary, which was critically reviewed by IHW. SA is the guarantor.
Funding: None.
Competing interests: None declared.
Ethical approval: Not needed.
References
- 1.National Statistics 2000. www.statistics.gov.uk (search for “breast cancer”) (accessed Oct 2004).
- 2.Al-Ghazal SK, Fallowfield L, Blamey RW. Comparison of psychological aspects and patient satisfaction following breast conserving surgery, simple mastectomy and breast reconstruction. Eur J Surg Oncol 2000;36: 1938-43. [DOI] [PubMed] [Google Scholar]
- 3.Blamey RW. The British Association of Surgical Oncology guidelines for surgeons in the management of symptomatic breast disease in the UK (1998 revision). Eur J Surg Oncol 1998;24: 464-76. [DOI] [PubMed] [Google Scholar]
- 4.Newman LA, Kuerer HM, Hunt KK, Ames FC, Ross MI, Theriault R, et al. Feasibility of immediate breast reconstruction for locally advanced breast cancer. Ann Surg Oncol 1999;6: 671-5. [DOI] [PubMed] [Google Scholar]
- 5.Cunnick GH, Mokbel K. Skin-sparing mastectomy. Am J Surg 2004;188: 78-84. [DOI] [PubMed] [Google Scholar]
- 6.Noguchi M, Fukushima W, Ohta N, Koyasaki N, Thomas M, Miyazaki I, et al. Oncological aspect of immediate breast reconstruction in mastectomy patients. J Surg Oncol 1992;50: 241-6. [DOI] [PubMed] [Google Scholar]
- 7.Noone RB, Frazier TG, Noone GC, Blanchet NP, Murphy JB, Rose D. Recurrence of breast carcinoma following immediate reconstruction: a 13-year review. Plast Reconstr Surg 1994;93: 96-106. [PubMed] [Google Scholar]
- 8.Furey PC, Macgillivray DC, Castiglione CL, Allen L. Wound complications in patients receiving adjuvant chemotherapy after mastectomy and immediate breast reconstruction for breast cancer. J Surg Oncol 1994;55: 194-7. [DOI] [PubMed] [Google Scholar]
- 9.Khoo A, Kroll SS, Reece GP, Miller MJ, Evans GR, Robb GL, et al. A comparison of resource costs of immediate and delayed breast reconstruction. Plast Reconstr Surg 1998;101: 964-8. [DOI] [PubMed] [Google Scholar]
- 10.Kroll SS, Coffey JA, Winn RJ, Schusterman MA. A comparison of factors affecting aesthetic outcomes of TRAM flap breast reconstructions. Plast Reconstr Surg 1995;96: 860-4. [DOI] [PubMed] [Google Scholar]
- 11.Al-Ghazal SK, Sully L, Fallowfield L, Blamey RW. The psychological impact of immediate rather than delayed breast reconstruction. Eur J Surg Oncol 2000;26: 17-9. [DOI] [PubMed] [Google Scholar]
- 12.Kronowitz SJ, Robb GL. Breast reconstruction with postmastectomy radiation therapy: current issues. Plast Reconstr Surg 2004;114: 950-60. [DOI] [PubMed] [Google Scholar]
- 13.Spear SL, Spittler CJ. Breast reconstruction with implants and expanders. Plast Reconstr Surg 2001;107: 177-87. [DOI] [PubMed] [Google Scholar]
- 14.Chawla AK, Kachnic LA, Taghian AG, Niemierko A, Zapton DT, Powell SN. Radiotherapy and breast reconstruction: complications and cosmesis with TRAM versus tissue expander/implant. Int J Radiat Oncol Biol Phys 2002;54: 520-6. [DOI] [PubMed] [Google Scholar]
- 15.Malata CM, Feldberg L, Coleman DJ, Foo IT, Sharpe DT. Textured or smooth implants for breast augmentation? Three year follow-up of a prospective randomised controlled trial. Br J Plast Surg 1997;50: 99-105. [DOI] [PubMed] [Google Scholar]
- 16.Clough KB, O'Donoghue JM, Fitoussi AD, Nos C, Falcou MC. Prospective evaluation of late cosmetic results following breast reconstruction. Ann Plast Surg 2001;107: 1702-16. [DOI] [PubMed] [Google Scholar]
- 17.Janowsky EC, Kupper LL, Hulka BS. Meta-analysis of the relationship between silicone breast implants and the risk of connective tissue diseases. N Engl J Med 2000;342: 781-90. [DOI] [PubMed] [Google Scholar]
- 18.National Breast Implant Registry Annual Report 2000. Salisbury: National Breast Implant Registry, 2000. [Available on request from the registry at the Plastic Surgery Department, Salisbury General Hospital, Salisbury SP2 8BJ or 01722 425059.]
- 19.Banic A, Boeckx W, Greulich M, Guelickx P, Marchi A, Rigotti G, et al. Late results of breast reconstruction with free TRAM flaps: a prospective multicentric study. Plast Reconstr Surg 1995;95: 1195-204. [PubMed] [Google Scholar]
- 20.Reece GP, Kroll SS. Abdominal wall complications: prevention and treatment. Clin Plast Surg 1998;25: 235-49. [PubMed] [Google Scholar]
- 21.Gill PS, Hunt JP, Guerra AB, Dellacroce FJ, Sullivan SK, Boraski J, et al. A 10-year retrospective review of 758 DIEP flaps for breast reconstruction. Plast Reconstr Surg 2004;113: 1153-60. [DOI] [PubMed] [Google Scholar]
- 22.Schwabegger A, Ninkovic M, Brenner E, Anderl H. Seroma as a common donor site morbidity after harvesting the latissimus dorsi flap: observations on cause and prevention. Ann Plast Surg 1997;38: 594-7. [DOI] [PubMed] [Google Scholar]
- 23.Titley OG, Spyrou GE, Fatah MF. Preventing seroma in the latissimus dorsi flap donor site. Br J Plast Surg 1997;50: 106-8. [DOI] [PubMed] [Google Scholar]
- 24.Shaik-Nadu N, Preminger BA, Rogers K, Messina P, Gayle LB. Determinants of aesthetic satisfaction following TRAM and implant breast reconstruction. Ann Plast Surg 2004;52: 465-70. [DOI] [PubMed] [Google Scholar]
- 25.Losken A, Carlson GW, Schoeman MB, Jones GE, Culbertson JH, Hester TR. Factors that influence the completion of breast reconstruction. Ann Plast Surg 2004;52: 258-61. [DOI] [PubMed] [Google Scholar]