Adolescence is a time of enormous change in weight and eating. Average weight gain during puberty is 14 kg for girls and 15 kg for boys, with marked differences in body shape between the sexes becoming evident. About 40% of girls (25% of boys) begin dieting in adolescence. Reported dieting may often reflect dissatisfaction with their body rather than actual calorie restriction. Six to 12 per cent of adolescents choose to become vegetarian, giving them increased independence from family eating patterns.
Table 1.
Prevalence of eating behaviours and eating problems in adolescence in United Kingdom
| Eating behaviour | Prevalence (%) | Sex ratio (female to male) |
|---|---|---|
| Dieting |
35 |
1.5:1 |
| Anorexia nervosa |
0.4 |
9:1 |
| Bulimia nervosa |
1 |
30:1 |
| Obesity | 7-10 | 1.3:1 |
Eating disorders, anorexia nervosa, and bulimia nervosa, are characterised by morbid preoccupation with weight and shape and manifest through distorted or chaotic eating behaviour. This behaviour differentiates these disorders from other types of psychological problems associated with abnormal eating behaviour—such as extreme faddy (selective) eating and various types of food phobia—and from obesity, in which primary psychological mechanisms are rarely implicated or are part of a more complex picture.
Table 2.
Risk factors for developing eating disorder in adolescence
| • Female sex |
| • Repeated dieting |
| • Early puberty |
| • Temperament |
| • Perfectionism |
| • Teasing about weight and dieting |
| • Low self esteem |
| • Losses and major life events |
| • Family dysfunction |
Eating disorders
Studies have found anorexia nervosa to be the third commonest chronic illness of adolescence, affecting 0.5% of adolescent girls. Bulimia nervosa is slightly more common (1%), but the secretive nature of the disorder and adolescents' reluctance to seek help mean that it is often hidden.
Eating disorders occur in all ethnic groups, and about 90% of cases are in females. Social, psychological (perception of ideal body weight and individual temperament), and genetic mechanisms all contribute to the development of an eating disorder.
Table 3.
Differentiation of anorexia from bulimia
| Anorexia nervosa | Bulimia nervosa |
|---|---|
| Low weight | Normal weight |
| Presents early | Presents late |
| Patient rarely seeks help | Patient may seek help |
| Onset early to middle teens | Onset late teens |
| Can be premenarcheal | Is rarely premenarcheal |
| Can affect boys | Usually affects girls |
| Acute or chronic | Fluctuating course |
| No previous illness | Previous anorexia nervosa |
| Associated with anxiety, obsessive compulsive disorder, depression | Associated with depression, self harm, substance misuse |
| Prognosis poor without early intervention | Up to 60% respond to specific treatments |
Recognition
The diagnosis of eating disorders in adolescents should take into consideration the context of normal pubertal growth and adolescent development. Although the problem may present as a result of other people's concern, assessment of the young person on their own is necessary to establish diagnosis, risk, and attitude to help. Diagnostic criteria are helpful, but intervention should also be considered in adolescents with severely abnormal eating attitudes and behaviours (such as those who vomit or take laxatives regularly but do not binge) or whose rate of weight loss is of more concern than degree of underweight.
Table 4.
Diagnostic criteria for anorexia nervosa and bulimia nervosa*
| Anorexia nervosa | Bulimia nervosa |
|---|---|
| • Body weight is maintained at least 15% below that expected or body mass index is 17.5 or lower† | • Persistent preoccupation with eating; overeating episodes in which large amounts of food are eaten in short periods of time |
| • Weight loss is self induced by avoidance of “fattening foods” plus one or more of: self induced vomiting; self induced purging; excessive exercise; use of appetite suppressants or diuretics | • The patient tries to counteract the “fattening” effects of food by one or more of: self induced vomiting or purgative abuse; alternating starvation and eating; use of appetite suppressants, thyroid preparations, or diuretics |
| • Body image distortion in which dread of fatness persists as an intrusive, overvalued idea | • The psychopathology consists of a morbid dread of fatness, and the patient sets herself or himself a precise weight threshold, well below the premorbid weight that constitutes the optimum or healthy weight in the opinion of the physician |
| • Widespread endocrine disorder involving the hypothalamic-pituitary-gonadal and manifesting as amenorrhoea in women and loss of sexual interest and potency in men | • Often a history of previous anorexia nervosa, with the interval ranging from a few months to several years |
| • If onset is prepubertal, puberty is delayed or arrested. With recovery, puberty is often normal, but the menarche is late |
*Based on ICD-10 (international classification of diseases, 10th revision); †Body mass index criterion does not apply for young people aged under 17
For some young people, eating behaviours such as dieting that develop during adolescence can herald the onset of more serious eating problems
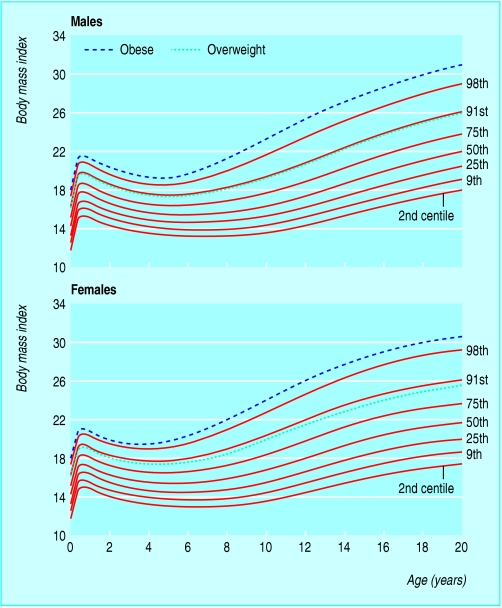
The body mass index (BMI (kg/m2)) is misleading in children and adolescents, and BMI centiles must be used to define underweight. A BMI lower than the ≤2nd centile indicates serious underweight and should be a trigger for referral. An eating disorder should also be considered if an adolescent fails to attain or maintain a healthy weight, height, or stage of sexual maturity for age.
Figure 1.
Body mass index charts (showing centiles and BMI values for overweight and obesity at age 18) for assessing underweight; the trigger for referring a young person with serious underweight to a specialist is a body mass index lower than or equal to the second centile
Once the patient has been weighed and their height measured, a few key questions (how much would you like to weigh? how do you feel about your weight? are you or is anyone else worried about your eating or exercising?)—asked in a non-judgmental manner—can be helpful in deciding whether further assessment is needed. An adolescent's distress about being asked about weight and food should heighten concern. If the concern is equivocal, a further appointment within a month is advisable.
Table 5.
Psychological or behavioural markers of potential eating disorder
| • Is a reluctant attender at the surgery or clinic |
| • Seeks help for physical symptoms |
| • Resists weighing and examination |
| • Covers body |
| • Is secretive or evasive |
| • Has increased energy (and in some cases agitation) |
| • Gets angry or distressed when asked about eating problems |
Physical signs of malnutrition and purging include thinning hair, parotid gland swelling, enamel erosion, hypothermia, bradycardia, lanugo hair, dry skin, hypotension, underweight, cold hands and blue/mottled peripheries, poor capillary return, carotenaemia, insensitivity to pain, constipation, amenorrhoea, shrunken breasts
After an eating disorder is identified, direct challenge or confrontation is unlikely to be helpful. At first presentation aim to (a) feed back findings from physical examination, including degree of underweight if relevant; (b) establish weight monitoring plus a plan to follow if weight falls; (c) discuss psychiatric risk as needed; and (d) provide the family and young person with information about the nature, course, and treatment of eating disorders. In general, the threshold for intervention should be lower for adolescents than for adults.
Table 6.
Criteria for considering admission to hospital for anorexia nervosa
| • Very rapid weight loss or very low energy intake |
| • Body mass index substantially below the second centile |
| • High risk of suicide |
| • Signs of physical compromise (severe dehydration; capillary return ≥1.5 seconds; resting pulse ≤45 beats/min; diastolic blood pressure ≤40 mm Hg and/or very wide pulse pressure or severe postural hypotension) |
Management
Assessment and management of a young person with an identified eating disorder needs to tackle medical, nutritional, and psychological aspects of care and be delivered by healthcare staff who are knowledgeable about normal adolescent development. When management is shared between primary and secondary care, clear agreement is needed about who is responsible for monitoring patients, and this should be communicated to the patient and his or her family.
Table 7.
Consequences of eating disorders
| Short term |
| • Sinus bradycardia; T wave inversions; ST segment depression; prolonged corrected QT interval; dysrhythmias with supraventricular beats and ventricular tachycardia |
| • Slowed gastrointestinal motility and constipation; abnormal results on liver function tests; superior mesenteric artery syndrome |
| • Raised blood urea nitrogen concentration with increased risk of renal stones |
| • Leucopenia; anaemia; iron deficiency; thrombocytopenia |
| • Sick euthyroid syndrome; amenorrhoea |
| Long term |
| • Pubertal delay or arrest |
| • Growth retardation and short stature |
| • Impairment of bone mineral acquisition, leading to osteopenia or osteoporosis |
| • Psychological sequelae—for example, anxiety and depression |
Management of nutritional disturbances in adolescents with eating disorders should take into account the pubertal development and activity level. This is likely to mean that they will need a higher calorie intake for adequate weight gain than the intake required by adult patients with eating disorders.
Family interventions that directly tackle the eating disorder should be offered to adolescents with anorexia nervosa. Adolescents with bulimia nervosa may best be treated with cognitive behaviour therapy specific to the disorder, with the family included as appropriate. Consideration should be givento the impact of the problem on siblings, who should be involved in treatment when possible.
For young people under 16 years who present alone with an eating disorder, communication with parents or carers will need to be discussed
Admission to hospital is necessary if there is acute physical compromise, high psychiatric risk, or after an adequate trial of outpatient treatment. Admission may be to a paediatric ward, an adolescent psychiatric unit, or a specialist eating disorders unit. These facilities should provide skilled feeding with careful physical monitoring (particularly in the first few days) together with psychosocial interventions.
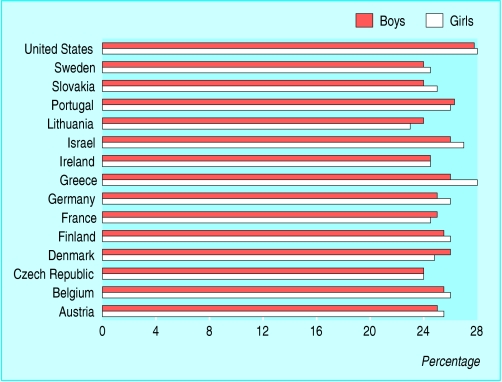
Figure 2.
Percentage of 15 year olds who are obese in Europe and the United States. Adapted from Lissau et al. Arch Pediatr Adolesc Med 2004158 27-33
Obesity
Rates of obesity have increased substantially among children and adolescents in almost all developed countries in the past two decades. In the United Kingdom, an estimated 7-8% of adolescents of both sexes are seriously obese, with a further 15% being seriously overweight but not obese. The great majority of child and adolescent obesity is primary in origin, due to a long term imbalance between nutritional intake and energy expenditure. Identified monogenic syndromes and secondary causes of obesity probably account for less than 1% of adolescent obesity.
Table 8.
Conditions associated with obesity
| Current |
| • Type 2 diabetes |
| • Insulin resistance (metabolic) syndrome: hyperinsulinism, dyslipidaemia, hypertension |
| • Polycystic ovarian syndrome |
| • Non-alcoholic steatohepatitis |
| • Asthma |
| • Psychological morbidity, including higher rates of low self esteem, depression, suicide attempts |
| • Poor academic achievement |
| • Arthritis |
| Future |
| • Excess mortality (from cardiovascular disease, cancer, all causes) |
| • Reduced professional, financial, and marital expectations |
Obesity in adolescence is a concern because it is associated with current as well as future health problems. Type 2 diabetes and the insulin resistance (metabolic) syndrome are emerging as problems in adolescence. Clinical data suggest that as many as 4% of obese adolescents may have silent type 2 diabetes and a further 30% may have three or more components of the insulin resistance syndrome.
Assessment
The most useful definition of obesity is that developed by the International Obesity Task Force, which found that the BMI 99th centile approximately equates to 30 (which in adults is the level linked with adverse health outcomes). As highly muscular young people can have a high BMI yet a low fat mass, it is best to also use a second method of assessing body fat mass, such as waist circumference (for which centiles are now available) or bioimpedance measure (centiles being developed). Those with both a high BMI and a high waist circumference are probably at highest risk.
Table 9.
Aims of obesity assessment
| • To categorise cardiovascular risk profile (elements of the insulin resistance syndrome: fasting hyperinsulinaemia; hypertension; dyslipidaemia; obesity, particularly abdominal obesity; type 2 diabetes) |
| • To identify current or potential complications of obesity |
| • To exclude secondary causes of obesity: genetic causes (such as Prader-Willi syndrome, Bardet Biedl syndrome, and rare monogenic syndromes) and endocrine syndromes such as hypothyroidism and Cushing's syndrome |
Medical assessment
Family history of obesity and the family risk profile in terms of history of diabetes and components of the insulin resistance syndrome should be noted. Ethnic background should also be considered, as those from a black or South Asian background have a significantly higher risk of the insulin resistance syndrome and diabetes.
On clinical examination, important signs include fat distribution (generalised or abdominal), acanthosis nigricans (a marker of hyperinsulinism), pubertal development, and blood pressure (measured with an appropriate size cuff). In girls, hirsuitism and acne may suggest polycystic ovarian syndrome. It is useful to search for signs of hypothyroidism and Cushing's syndrome, although obesity is rarely the sole presentation of these conditions in adolescence. Striae and a prominent nuchal fat pad (“buffalo hump”) are extremely common in adolescents with simple obesity.
Table 10.
Important issues in taking a history in adolescent obesity
| Plotting the “obesity trajectory” |
| To do this we ask about birth weight; about early feeding history; whether onset of obesity was sudden or gradual, and at what age; whether progression of obesity was rapid or gradual; whether there have been any periods of very rapid weight gain, particularly recently; whether there have been any periods of weight loss (and why and how achieved); who else in the family is obese or has trouble controlling their weight |
| Family risk profile |
| To place the child in the appropriate risk category ask about family history of components of the insulin resistance syndrome (morbid obesity; type 2 diabetes; hypertension; dyslipidaemia; polycystic ovarian syndrome; early cardiovascular disease (defined as development of cardiovascular disease at age 50-59 or younger) |
Minimal investigations should be done in primary care in adolescents thought to be at high risk (high BMI, abdominal obesity, family history of diabetes or of the insulin resistance syndrome). These include simple biochemistry and haematology tests, fasting insulin and glucose tests, fasting lipid tests, and thyroid function tests.
Treatment
The treatment of obesity is notoriously difficult, and a lack of belief that obesity can be treated is widespread. In the United Kingdom, the Royal College of Paediatrics and Child Health has recently issued excellent brief guidance on managing obesity in primary care.
Table 11.
Guidelines for treatment of obesity in primary care*
| Features that should trigger referral to paediatrician | Weight management options and contraindications |
|---|---|
| • Serious morbidity related to obesity (such as sleep apnoea, orthopaedic problems, type 2 and non-insulin dependent diabetes mellitus, hypertension) | • No weight gain as height increases |
| • Height below 9th centile, unexpectedly short for family, or slowed growth rate | • Weight gain slower than height gain |
| • Precocious or late puberty (before 8 years, or no signs at 13 in girls or 15 in boys) | • Rapid weight loss and strict dieting are not appropriate for growing children unless under specialist care |
| • Severe learning disability | Action |
| • Symptoms and signs of genetic or endocrine abnormalities | • Successful interventions involve the family and are tailored to each individual |
| • Severe and progressive obesity before age 2 | • The multidisciplinary team needed may include a general practitioner, practice nurse, health visitor, school nurse, and other professionals if available (such as paediatric dietician, clinical psychologist, community paediatrician) |
| • Other serious concerns | • Negotiate realistic goals and monitoring plans |
| • Provide information on local physical activity facilities, healthy eating, local parenting support groups |
Adapted from the Royal College of Paediatrics and Child Health and National Obesity Forum. An Approach to Weight Management in Children and Adolescents (2-18 years) in Primary Care. 2002 (www.rcpch.ac.uk/)
The most successful obesity treatments are multidisciplinary programmes that urge changes in eating habits and family systems and promote exercise and a reduction in sedentary activities. Dietary interventions alone are unlikely to produce substantial change.
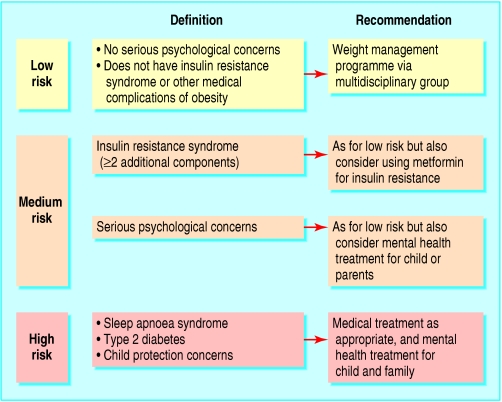
A treatment plan should be guided by an assessment of risk in both the medical and psychological domains. The psychological domains include emotional overeating, substantial distress, parental mental health, and (rarely) child protection concerns. Substantial weight loss is extremely difficult to achieve, and setting overambitious targets can reduce motivation. Our primary aim in adolescents who are still growing is weight maintenance, thereby producing loss of overweight. As this is achievable only before the end of the pubertal growth spurt, obesity should be treated before puberty if possible. Secondary aims may include improvement in psychological wellbeing; family functioning; and insulin sensitivity, liver function, and lipid concentrations.
Table 12.
Evidence for prevention of child and adolescent obesity
| Evidence for prevention | Longitudinal studies into adulthood | Longitudinal studies within childhood | Cross sectional studies in childhood |
|---|---|---|---|
| Sedentary activities |
Yes |
Yes |
Yes |
| Exercise |
Yes |
Yes |
Yes |
| Diet |
No |
No |
Yes |
| Eating pattern (breakfast, family) |
No |
No |
Yes |
| Breastfed as infant | Yes | Yes | Yes |
The limited effectiveness of treatment has prompted a reconsideration of the role of drugs in severe obesity. No drugs for the treatment of obesity in childhood are currently approved in the United Kingdom or the United States. Metformin, orlistat, and sibutramine may be used in specialist centres. Drug treatment is more effective when combined with a behavioural intervention.
The most effective ways to prevent and treat obesity are likely to be actions at the macroeconomic level. However, in local communities, individual clinicians may be able to encourage change by promoting simple measures to allow adolescents to participate in sport and activity and eat more healthily.
Figure 3.
Assessment of risk and treatment options
The ABC of adolescence is edited by Russell Viner, consultant in adolescent medicine at University College London Hospitals NHS Foundation Trust and Great Ormond Street Hospital NHS Trust (rviner@ich.ucl.ac.uk). The series will be published as a book in summer 2005.
Dasha Nicholls is consultant child and adolescent psychiatrist at the Feeding and Eating Disorders Service, Great Ormond Street Hospital, London.
Competing interests: None declared.
References
- • Mulvihill C, Quigley R. Review of prevention of obesity. The management of obesity and overweight: an analysis of reviews of diet, physical activity and behavioural approaches. London: Health Development Agency, 2003. (Evidence briefing.) (www.hda.nhs.uk/evidence)
- • Campbell K, Waters E, O'Meara S, Kelly S, Summerbell CD. Interventions for preventing obesity in children. Cochrane Database Syst Rev 2004;(2): CD001871. [DOI] [PubMed]
- • Gowers S, Bryant-Waugh R. The management of children and adolescents with eating disorders. J Child Psychol Psychiatry 2004;45: 63-83 [DOI] [PubMed] [Google Scholar]
- • Child Growth Foundation, 2 Mayfield Avenue, London W4 1PW and Harlow Printing, Maxwell Street, South Shields NE33 4PU UK (for BMI centile charts based on the UK 1990 growth reference and waist centile charts)
- • www.nice.org.uk (for guidelines on eating disorders from the National Institute for Clinical Evidence)