SUMMARY
Short sleep duration is associated with excess body mass among adolescents and young adults. The mechanisms theorized to drive that association suggest that persistent exposure to short sleep should be associated with greater accumulations of body mass. We use prospective cohort data from four waves of the National Longitudinal Study of Adolescent to Adult Health (1994–2009; N=14,800) to examine associations between cumulative exposure to short sleep throughout adolescence and early adulthood, and obesity and elevated waist circumference outcomes. We compare several clinical and distribution-based standards of short sleep to assess which measures are most strongly associated with body mass. Cumulative exposure to short sleep exhibits dose-response associations with obesity and elevated waist circumference. Relative to respondents with no instances of short sleep, those who slept −0.50 standard deviations or less than the age and sex-specific average sleep hours in all four waves had 1.45 (95% CI=1.03, 2.04) times the odds of being obese and 1.45 (95% CI=1.02, 2.06) times the odds of having an elevated waist circumference. Our findings suggest that cumulative exposure to short sleep during adolescence and young adulthood may play an important role in the development of obesity and elevated waist circumference during this important developmental period.
Keywords: short sleep duration, cumulative exposure to short sleep, body mass index, waist circumference, adolescence, young adults
A growing body of evidence finds that shorter sleep durations among children and adolescents are associated with higher body masses, adverse cardiovascular and metabolic outcomes, and unhealthy diets (Javaheri et al., 2008, Kruger et al., 2014, Larkin et al., 2005, Magee and Hale, 2012, Patel and Hu, 2008, Reither et al., 2014, Taheri et al., 2004). Some researchers have linked declines in average sleep time among U.S. children and adolescents to the increasing prevalence of obesity (Calamaro et al., 2009, Chen et al., 2008), and others promote additional sleep to help youth maintain healthy weights (Taheri, 2006). However, most research on the association between sleep and body mass is cross-sectional (Magee and Hale, 2012, Patel and Hu, 2008). Existing longitudinal studies often focus on young children (Lumeng et al., 2007, Reilly et al., 2005, Taveras et al., 2008, Touchette et al., 2008) or adults (Chaput et al., 2008, Patel et al., 2006) rather than on adolescents who experience developmental changes in sleep duration, height, and weight, and who have growing control over their sleep, physical activity, diet, and sedentary behaviors. Further, longitudinal studies sometimes rely on small, regional samples (Agras et al., 2004, Landhuis et al., 2008, Taveras et al., 2008, Touchette et al., 2008), and rarely consider long-term exposures to short sleep.
Our first aim is to examine associations between cumulative exposure to short sleep duration throughout adolescence and early adulthood, and body mass outcomes including obesity and elevated waist circumference in early adulthood. Short sleep duration may be linked to increased body mass and adverse metabolic and cardiovascular outcomes through pathways including hormonal dysregulation (Hitze et al., 2008), changes in the quality and quantity of food consumed (Beebe et al., 2013, Kruger et al., 2014), and reduced energy expenditure (McKnight-Eily et al., 2011). Each of those pathways implies that persistent exposures to short sleep over long time periods will be more strongly associated with body mass than short-term exposures.
Longitudinal studies often use sleep duration at one point in time or average sleep duration from several time points to predict subsequent body mass (Agras et al., 2004, Landhuis et al., 2008, Lumeng et al., 2007, Magee and Hale, 2012, Patel and Hu, 2008, Reilly et al., 2005, Snell et al., 2007, Suglia et al., 2014, Taveras et al., 2008), which obscures heterogeneity in sleep duration over time. As a result, longitudinal studies find inverse associations between sleep duration and body mass among adolescents and young adults (Lumeng et al., 2007), although that association is not significant in several studies (Snell et al., 2007, Suglia et al., 2014). We know of only one paper that specifically considers cumulative exposure to short sleep. Touchette and colleagues (2008) find that 5% of children in a representative sample from Québec province, Canada are persistent short sleepers between the ages of 5 months and 6 years of age; those children have higher odds of overweight and obesity at age 6 than intermittent short sleepers. We extend prior research by examining cumulative exposure to short sleep through adolescence and early adulthood.
Our second aim is to explore how various measures of cumulative exposure to short sleep duration are associated with body mass outcomes. Standards that distinguish adequate sleep from short sleep among adolescents and young adults are insufficiently informed by a robust evidence base. Longitudinal studies of children and adolescents that assess sleep duration with single continuous (Agras et al., 2004, Lumeng et al., 2007) or categorical measures (Reilly et al., 2005, Snell et al., 2007, Suglia et al., 2014), offer little consensus about how much sleep is necessary at different ages to help prevent weight gain and obesity. Indeed, Matricciani and colleagues assert, “sleep recommendations are still being issued in the acknowledged absence of meaningful evidence (Matricciani et al., 2012:553).”
We compare multiple standards for adequate sleep. First, we consider the National Sleep Foundation’s (NSF) recommendations of at least 9 hours of sleep for those aged 6–13, at least 8 hours of sleep for those aged 14–17, and at least 7 hours of sleep for those aged 18–25 (Hirshkowitz et al., 2015). NSF standards derive from expert panels’ reviews of the literature but have not been validated in longitudinal studies of body mass. Second, we consider a 7-hour threshold for adequate sleep. Many studies of adults define short sleep as less than 7-hours per night (Cappuccio et al., 2008, Chaput et al., 2008). The NSF report provides a rationale for using the 7-hour standard among youth by cautioning that the harm associated with sleeping fewer than 7 hours among children aged 6–17 outweighs any benefits, and is “not recommended” (Hirshkowitz et al., 2015). Finally, we consider measures derived from age- and sex-specific distributions of sleep duration in the National Longitudinal Study of Adolescent to Adult Health (Add Health)—a nationally representative cohort.
DATA AND METHODS
We employ prospective cohort data from all four waves of Add Health, collected in 1994–1995 (Wave 1, mean age=15.9), 1996 (Wave 2, mean age=16.9), 2001–2002 (Wave 3, mean age=22.3), and 2008–2009 (Wave 4, mean age=28.8). In Wave 1, Add Health conducted brief interviews with a nationally representative sample of over 90,000 students enrolled in grades 7 through 12 in United States schools, and then selected a much smaller subsample for detailed longitudinal follow-up (Chantala, 2006). Add Health conducts physical examinations of adolescents, as well as in-home surveys with parents and adolescents on topics including health, academics, romantic and friend relationships, employment, and family formation. Our analyses focus on the 14,800 young adults aged 24.3 to 34.7 years who were interviewed in Wave 4, and their data from prior survey waves. The response rate for eligible respondents was over 77% in each wave, but retention was temporarily reduced by the intentional exclusion of high school seniors in Wave 1 from Wave 2. Wave 4 data were re-weighted to be nationally representative of the population of adults in 2008–2009 who were enrolled in grades 7–12 during 1994–1995 (Wave 1) (Chantala, 2006).
Outcome Variables
Outcome variables are measured in Wave 4 (Entzel et al., 2009). BMI is calculated from measured heights and weights, and is dichotomized as obese (kg/m2 ≥ 30) and non-obese (kg/m2 < 30). Waist circumference is measured at the superior border of the iliac crest, and is dichotomized as those who are at or above the 75th percentile, by gender, and those who are below the 75th percentile. We estimate the 75th percentile of waist circumference separately for Asians and non-Asians (Grundy et al., 2005). Models that predict waist circumference also adjust for height at Wave 4. We dichotomize the body mass measures because we sought body mass thresholds that have established associations with adverse outcomes.
Cumulative Short Sleep Duration
Sleep duration is self-reported. In Waves 1 and 2, respondents report their usual sleep duration in hours. In Waves 3 and 4, respondents report the hour and minute they usually go to sleep and then awake on (a) days that they attend work or school-related activities (“weekdays”), and (b) days that they do not have to wake up at a certain time (“weekends”). We multiply sleep hours on weekdays by 5/7 and on weekends by 2/7, and then add the resulting figures to create a daily weighted average of usual sleep hours. Wave 3 and 4 data yield negative sleep hours or implausibly high sleep hours (e.g., 16+ hours) for 3% and 5% of respondents, respectively. Most misreports occur among respondents who report “12” as the hour of waking or sleep onset, suggesting that they confused 12am and 12pm. By correcting these misreports, we obtain similar correlations in sleep hours across each pair of consecutive waves.
We create the following measures of cumulative exposure to short sleep duration from usual sleep hours in each wave:
NSF Standard
Respondents receive a 0 in each wave if they meet the NSF age-specific standard for adequate sleep (at least 9 hours for those aged 6–13, at least 8 hours for those aged 14–17, and at least 7 hours for those aged 18–25), and a 1 otherwise (Hirshkowitz et al., 2015). Summing across waves provides a count of the number of waves in which respondents fail to meet the NSF standard for adequate sleep.
7-hour Standard
Respondents receive a 0 in each wave if they sleep 7 or more hours, and a 1 otherwise. Summing the four items provides a count of the number of waves in which respondents fail to sleep at least 7 hours.
Distribution-Based Measures
We use standardized residuals to indicate how much less a given respondent sleeps compared to the average for age- and sex-specific peers, based on the distribution of sleep hours in the Add Health data. We begin by estimating a hierarchical linear model (with wave-specific observations nested within respondents) that predicts average sleep duration with age, sex, and the wave of observation. We include quadratic splines for age, with knots at ages 15, 20, and 25 in the best-fitting model (Marsh and Cormier, 2002), and include interactions between sex and the age variables. Our model, shown in Appendix A, finds that residual variability in usual sleep duration increases from ages 11–14 to ages 19–22, and then declines through ages 31–34. Ancillary analyses found that sex differences in residual variability were trivial in magnitude and were, thus, excluded from our final models.
We square the within-individual and between-individual (by age) residual standard deviations, sum them, and take the square root to calculate a standard deviation (SD) for sleep duration, conditional on the variables included in the model (e.g., conditional SD for ages ). Then we sum the within-individual and between-individual residuals and divide them by the age-specific conditional standard deviations to create a standardized residual (Snijders and Bosker, 2011). A standardized residual of −1 indicates that a respondent’s usual sleep duration is one standard deviation below peers of the same age and sex.
We use the age- and sex-specific standardized residuals to consider the −0.25 SD, −0.50 SD, −0.75 SD, and −1.00 SD standards. In each wave, we create four dichotomous variables (one for each standard) that equal 1 if the residuals are −0.25 or smaller, −0.50 or smaller, −0.75 or smaller, or −1.00 or smaller, respectively. The dichotomous variables equal 0 if respondents have residuals that are above the threshold for a given standard in a given wave. Summing the dichotomous variables creates a count of the number of waves that respondents fail to meet a given standard for adequate sleep.
Confounders
Numerous variables are associated with sleep duration, but the causal ordering of those variables is unclear (Krueger and Friedman, 2009). Thus, we focus on confounders that are most clearly exogenous. All models adjust for demographic variables. Age in years in Wave 4 is coded continuously. We do not find evidence of a nonlinear association between age and body mass for the ages examined. Sex is coded dichotomously. Race/Ethnicity is coded categorically as non-Hispanic white, non-Hispanic black, Hispanic, Asian, Native American, and other.
Subsequent models adjust for additional potential confounders. Nativity is coded dichotomously as U.S. versus foreign born. Among women, a categorical variable indicates those who were never pregnant, previously pregnant, or currently pregnant at Wave 4. Models that exclude women who are currently pregnant are virtually identical to those shown herein. Years of education among mothers and fathers are measured continuously and range from 0 (never attended school) to 18 (any post-baccalaureate education). Total family income in 1994 is measured continuously; we add one and take the natural log to account for the diminishing association between income and health as income increases (Krueger and Burgard, 2011). Parental marital status at Wave 1 is coded categorically as never married, married, or previously married. Dichotomous variables indicate whether mothers or fathers ever smoked cigarettes (“Has your [mother/father] ever smoked cigarettes?”) or were obese (“Respondent’s [mother/father] has obesity?”) at Wave 1. Like other proxy reports, adolescent reports of mothers’ and fathers’ smoking and obesity may be measured with error and, thus, might incompletely account for confounding of the association between cumulative exposure to short sleep and body mass outcomes. We use information about biological parents where available; otherwise we use information about the current mother or father figure in the household.
Sensitivity analyses exclude adolescents who are obese at baseline. Obesity in Wave 1 is determined by comparing BMI to age- and sex-specific standards provided by the Centers for Disease Control and Prevention (Kuczmarski et al., 2002). To correct potential biases in self-reported heights and weights in Wave 1, we employ Wave 2 data that include both self-reported and measured heights and weights, use linear regression to predict differences between self-reported and measured items by age, race/ethnicity, and sex, and adjust our Wave 1 measures accordingly.
Analyses
When arraying our data such that there is a row for each respondent in our analyses, and a column for each variable, just 5.2% of the cells have missing values. Despite this small percentage of missing data, listwise deletion of missing data would result in the exclusion of over one-third of our sample because many respondents are missing on just one of the numerous variables in our analyses. Respondents may have missing data due to wave non-response (i.e., non-participation in a given wave of the study) or item non-response (i.e., refusal to respond to an item when respondents participated in a given wave). All of the respondents in our analyses participated in both Wave 1 and Wave 4. Thus, in terms of wave non-response, 100% of eligible respondents participated in at least two waves, 94% of eligible respondents participated in three waves, and 63.7% of eligible respondents participated in all four waves. Item non-response is rare for our key variables. In Wave 4, just 0.5% of respondents are missing on sleep duration, 0.1% are missing on BMI, and 1% are missing on waist circumference.
We use multiple imputation to preserve our sample size and to reduce the potential for biased estimates due to missing data. Multiple imputation fills in each piece of missing data with multiple values that are drawn from a distribution of likely values. Multiple imputation methods assume that data are missing at random (MAR), conditional on observed covariates. In contrast, the listwise deletion of missing values relies on a less plausible assumption that data are missing completely at random (MCAR), unconditional on observed covariates (Little and Rubin, 2002). The MAR assumption is most plausible when numerous variables are included in the imputation model. We include over 60 variables in our imputation model (including sleep and body mass variables, as well as variables associated with sleep and body mass) to provide information about the likely distribution of missing values (Moons et al., 2006). We create 100 imputations using chained equations methods. Because all respondents in our study are interviewed in at least two waves, we use both cross-sectional and longitudinal variation to impute sleep duration within individuals and over time. Simulation studies show that multiple imputation results in less biased results than listwise deletion of missing data (Lee and Carlin, 2010). In our data, estimates that use multiple imputation rather than listwise deletion provide similar point estimates but narrower confidence intervals due to enhanced statistical power.
We use multivariate logistic regression models to estimate associations between measures of cumulative short sleep duration and the Wave 4 measures of obesity and elevated waist circumference. We pool males and females in all models—although average sleep duration varies by sex, we found no sex differences in the association between cumulative exposure to short sleep and obesity or waist circumference. We use Taylor-series expansion to obtain robust standard errors, given the complex sampling frame employed by Add Health (Korn and Graubard, 1999). We use Stata software for all analyses (StataCorp, 2013).
Ethics Committee Approval
Staff at the University of North Carolina at Chapel Hill received Institutional Review Board (IRB) approval for the Add Health data collection and attained consent from survey respondents. The IRB at the University of Colorado Denver | Anschutz Medical Campus further approved our use of the de-identified version of the Add Health data for the current project.
RESULTS
Table 1 presents age- and sex-specific average sleep durations in Add Health, as well as the distribution-based thresholds for short sleep (derived from the model in Appendix A). Average sleep duration among females declines from 9.3 hours at age 11 to 7.7 hours by age 18, hovers around 7.7 hours between ages 18 and 28, and then declines to 7.3 hours by age 34. Compared to females, males have slightly longer sleep durations before age 18, and have somewhat shorter sleep durations after age 19.
Table 1.
Mean sleep duration and distribution-based thresholds for short sleep, by age and sex, Add Health.a
| Age | Females
|
Males
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Distribution-based thresholds
|
Mean | Distribution-based thresholds
|
|||||||
| −0.25 SD | −0.50 SD | −0.75 SD | −1.00 SD | −0.25 SD | −0.50 SD | −0.75 SD | −1.00 SD | |||
| 11 | 9.3 | 9.0 | 8.6 | 8.3 | 8.0 | 9.4 | 9.1 | 8.8 | 8.5 | 8.2 |
| 12 | 9.0 | 8.7 | 8.4 | 8.1 | 7.7 | 9.2 | 8.9 | 8.5 | 8.2 | 7.9 |
| 13 | 8.7 | 8.4 | 8.1 | 7.8 | 7.5 | 8.9 | 8.6 | 8.3 | 8.0 | 7.6 |
| 14 | 8.5 | 8.2 | 7.8 | 7.5 | 7.2 | 8.6 | 8.3 | 8.0 | 7.7 | 7.4 |
| 15 | 8.2 | 7.9 | 7.5 | 7.2 | 6.8 | 8.4 | 8.0 | 7.7 | 7.3 | 7.0 |
| 16 | 8.0 | 7.6 | 7.3 | 6.9 | 6.6 | 8.1 | 7.8 | 7.4 | 7.1 | 6.8 |
| 17 | 7.8 | 7.4 | 7.1 | 6.8 | 6.4 | 7.9 | 7.6 | 7.2 | 6.9 | 6.5 |
| 18 | 7.7 | 7.3 | 7.0 | 6.6 | 6.3 | 7.7 | 7.4 | 7.0 | 6.7 | 6.3 |
| 19 | 7.6 | 7.3 | 6.9 | 6.5 | 6.2 | 7.6 | 7.2 | 6.8 | 6.5 | 6.1 |
| 20 | 7.6 | 7.3 | 6.9 | 6.5 | 6.2 | 7.4 | 7.1 | 6.7 | 6.4 | 6.0 |
| 21 | 7.7 | 7.3 | 6.9 | 6.6 | 6.2 | 7.3 | 7.0 | 6.6 | 6.3 | 5.9 |
| 22 | 7.7 | 7.3 | 6.9 | 6.6 | 6.2 | 7.3 | 6.9 | 6.5 | 6.2 | 5.8 |
| 23 | 7.7 | 7.3 | 7.0 | 6.6 | 6.3 | 7.2 | 6.9 | 6.5 | 6.2 | 5.8 |
| 24 | 7.7 | 7.3 | 7.0 | 6.6 | 6.3 | 7.2 | 6.8 | 6.5 | 6.1 | 5.8 |
| 25 | 7.7 | 7.3 | 7.0 | 6.6 | 6.2 | 7.2 | 6.9 | 6.5 | 6.1 | 5.8 |
| 26 | 7.6 | 7.3 | 6.9 | 6.6 | 6.2 | 7.2 | 6.9 | 6.5 | 6.2 | 5.8 |
| 27 | 7.6 | 7.3 | 7.0 | 6.7 | 6.3 | 7.2 | 6.9 | 6.6 | 6.3 | 5.9 |
| 28 | 7.6 | 7.3 | 6.9 | 6.6 | 6.3 | 7.2 | 6.9 | 6.6 | 6.2 | 5.9 |
| 29 | 7.5 | 7.2 | 6.9 | 6.6 | 6.3 | 7.2 | 6.8 | 6.5 | 6.2 | 5.9 |
| 30 | 7.5 | 7.2 | 6.9 | 6.6 | 6.2 | 7.1 | 6.8 | 6.5 | 6.2 | 5.9 |
| 31 | 7.5 | 7.1 | 6.8 | 6.5 | 6.2 | 7.1 | 6.8 | 6.4 | 6.1 | 5.8 |
| 32 | 7.4 | 7.1 | 6.8 | 6.5 | 6.2 | 7.0 | 6.7 | 6.4 | 6.1 | 5.8 |
| 33 | 7.4 | 7.1 | 6.8 | 6.4 | 6.1 | 6.9 | 6.6 | 6.3 | 6.0 | 5.7 |
| 34 | 7.3 | 7.0 | 6.7 | 6.4 | 6.1 | 6.8 | 6.5 | 6.2 | 5.9 | 5.6 |
Derived from the model shown in Appendix A
Table 2 shows that by Wave 4, only one-third of respondents are normal weight and slightly more than one-third of respondents are obese. By definition, about one-quarter of respondents have waist circumferences at or above the 75th percentile. Few respondents have short sleep durations in all four waves. About 3% of respondents report short sleep in all four waves according to the NSF standard, 5% report short sleep in all four waves according to the −0.25 SD standard, and less than 2% report short sleep in all four waves according to the 7-hour and −0.75 SD standards. Further, few respondents meet standards for adequate sleep hours in all four waves. Just 28% of respondents meet the NSF standard in all four waves and 45% meet the 7-hour standard in all four waves. A majority of respondents (62%) report adequate sleep in every wave only when considering the −1.00 SD standard.
Table 2.
Means (standard deviations) and percentage distributions of study variables, Add Health.a
| Body mass variables | Number of waves respondents failed to meet a given standard for adequate sleep: | ||
| Wave 4 BMI, % | |||
| Normal weight | 33.6 | Below NSF standard, % | |
| Overweight | 29.7 | 0 waves | 27.6 |
| Obese | 36.8 | 1 wave | 33.1 |
| Wave 1 BMI, %b | 2 waves | 25.6 | |
| Normal weight | 72.6 | 3 waves | 10.8 |
| Overweight | 15.4 | 4 waves | 2.9 |
| Obese | 12.0 | Below 7-hour standard, % | |
| Waist circumference 75 percentile, % | 26.2 | 0 waves | 45.3 |
| Respondent confounders at Wave 4 | 1 wave | 31.9 | |
| Height, cm, mean | 170.7 (10.2) | 2 waves | 16.0 |
| 3 waves | 5.5 | ||
| Male, % | 50.7 | 4 waves | 1.4 |
| Age, mean | 28.8 (1.8) | Below −0.25 SD standard, % | |
| 0 waves | 23.0 | ||
| Race/Ethnicity, % | 1 wave | 30.4 | |
| Non-Hispanic White | 67.3 | 2 waves | 26.8 |
| Non-Hispanic Black | 15.8 | 3 waves | 14.8 |
| Hispanic | 12.0 | 4 waves | 4.9 |
| Asian | 3.2 | Below −0.50 SD standard, % | |
| Native American | 0.7 | 0 waves | 37.5 |
| Other | 1.0 | 1 wave | 32.6 |
| Foreign born, % | 5.3 | 2 waves | 19.9 |
| Pregnancy status at wave 4, % | 3 waves | 7.9 | |
| Never pregnant or male | 67.0 | 4 waves | 2.0 |
| Ever pregnant | 30.0 | Below −0.75 SD standard, % | |
| Currently pregnant | 3.0 | 0 waves | 49.3 |
| Parent confounders at Wave 1 | 1 wave | 30.4 | |
| Mother’s education, yrs, mean | 13.2 (2.5) | 2 waves | 14.6 |
| 3 waves | 4.8 | ||
| Father’s education, yrs, mean | 13.3 (2.6) | 4 waves | 1.0 |
| Below −1.00 SD standard, % | |||
| Family income, $, mean | 50,951 (74,391) | 0 waves | 62.1 |
| 1 wave | 26.2 | ||
| Parents marital status, % | 2 waves | 9.1 | |
| Never married | 4.9 | 3 waves | 2.3 |
| Married | 72.9 | 4 waves | 0.4 |
| Previously married | 22.2 | ||
| Mother ever smoked, % | 50.7 | ||
| Father ever smoked, % | 62.5 | ||
| Mother obese, % | 18.5 | ||
| Father obese, % | 10.6 | ||
| N (unweighted) | 14,800 | ||
Standard deviations are undefined when applying probability weights to survey data. For any given variable X, we approximate the standard deviation as: (mean (X2) - (mean (X))2)0.5.
BMI data from Wave 1 are based on self-reported height and weight, and are categorized based on CDC growth charts for 2000
Compare Measures of Short Sleep
Table 3 presents models for the odds of obesity (Models 1–2) and elevated waist circumference (Models 3–4). Each panel reports results for a different measure of short sleep. Each measure of cumulative exposure to short sleep has a graded association with the odds of being obese (Model 1) or of having an elevated waist circumference (Model 3) in Wave 4. The trend is statistically significant for each sleep measure, but those who are short-sleepers in one wave based on the NSF (Panel A) or −0.25 SD (Panel C) standards do not have significantly higher odds of elevated body mass than those who are not short sleepers in any wave.
Table 3.
Odds ratios and 95% Cis for obesity and elevated waist circumference, Add Health.a
| Obesity (kg/m2 ≥ 30.0)
|
Waist circ. ≥ 75th percentile
|
|||
|---|---|---|---|---|
| Model 1a | Model 2b | Model 3a | Model 4b | |
| Panel A: Below NSF standard
| ||||
| 0 waves | ref | ref | ref | ref |
| 1 wave | 1.02 (0.89,1.17) | 1.01 (0.87,1.16) | 1.07 (0.92,1.26) | 1.07 (0.89,1.27) |
| 2 waves | 1.17* (1.02,1.35) | 1.16 (1.00,1.36) | 1.18* (1.01,1.38) | 1.17 (0.97,1.41) |
| 3 waves | 1.21* (1.02,1.44) | 1.18 (0.96,1.43) | 1.18 (0.96,1.45) | 1.18 (0.92,1.51) |
| 4 waves | 1.52** (1.12,2.07) | 1.34 (0.95,1.88) | 1.61** (1.17,2.23) | 1.55* (1.04,2.30) |
| p for trend | 0.000 | 0.003 | 0.002 | 0.013 |
|
| ||||
| Panel B: Below 7-hour standard
| ||||
| 0 waves | ref | ref | ref | ref |
| 1 wave | 1.19** (1.05,1.35) | 1.17* (1.01,1.36) | 1.25** (1.08,1.44) | 1.23* (1.03,1.46) |
| 2 waves | 1.38*** (1.19,1.61) | 1.37*** (1.16,1.60) | 1.38*** (1.15,1.65) | 1.41** (1.13,1.75) |
| 3 waves | 1.40** (1.12,1.74) | 1.33* (1.03,1.73) | 1.43** (1.11,1.85) | 1.40* (1.03,1.90) |
| 4 waves | 1.78* (1.15,2.76) | 1.49 (0.90,2.46) | 1.75* (1.10,2.78) | 1.71 (0.97,3.01) |
| p for trend | 0.000 | 0.000 | 0.000 | 0.000 |
|
| ||||
| Panel C: Below −0.25 SD standard
| ||||
| 0 waves | ref | ref | ref | ref |
| 1 wave | 1.07 (0.92,1.25) | 1.07 (0.91,1.26) | 1.13 (0.95,1.35) | 1.14 (0.94,1.39) |
| 2 waves | 1.16* (1.01,1.34) | 1.17 (1.00,1.36) | 1.15 (0.97,1.37) | 1.12 (0.92,1.36) |
| 3 waves | 1.22* (1.04,1.44) | 1.19 (0.99,1.42) | 1.28** (1.08,1.52) | 1.27* (1.02,1.58) |
| 4 waves | 1.47** (1.16,1.85) | 1.40* (1.08,1.82) | 1.39* (1.07,1.82) | 1.38* (1.00,1.90) |
| p for trend | 0.000 | 0.001 | 0.001 | 0.014 |
|
| ||||
| Panel D: Below −0.50 SD standard
| ||||
| 0 waves | ref | ref | ref | ref |
| 1 wave | 1.19* (1.04,1.36) | 1.18* (1.02,1.36) | 1.24** (1.07,1.42) | 1.22* (1.03,1.43) |
| 2 waves | 1.24** (1.08,1.43) | 1.22* (1.05,1.42) | 1.29** (1.10,1.51) | 1.29** (1.07,1.56) |
| 3 waves | 1.35** (1.13,1.63) | 1.27* (1.03,1.57) | 1.36** (1.09,1.68) | 1.34* (1.03,1.74) |
| 4 waves | 1.55* (1.09,2.21) | 1.35 (0.92,2.00) | 1.56* (1.08,2.28) | 1.44 (0.91,2.29) |
| p for trend | 0.000 | 0.000 | 0.000 | 0.000 |
|
| ||||
| Panel E: Below −0.75 SD standard
| ||||
| 0 waves | ref | ref | ref | ref |
| 1 wave | 1.18** (1.05,1.33) | 1.17* (1.02,1.33) | 1.20* (1.04,1.37) | 1.18* (1.01,1.38) |
| 2 waves | 1.25** (1.08,1.46) | 1.24* (1.05,1.46) | 1.27** (1.06,1.51) | 1.32** (1.08,1.61) |
| 3 waves | 1.46** (1.16,1.83) | 1.36* (1.04,1.78) | 1.31* (1.02,1.68) | 1.26 (0.92,1.73) |
| 4 waves | 1.82* (1.06,3.13) | 1.43 (0.78,2.60) | 1.83* (1.07,3.14) | 1.69 (0.86,3.29) |
| p for trend | 0.000 | 0.000 | 0.000 | 0.000 |
|
| ||||
| Panel F: Below −1.00 SD standard
| ||||
| 0 waves | ref | ref | ref | ref |
| 1 wave | 1.25*** (1.11,1.41) | 1.22** (1.07,1.39) | 1.22** (1.07,1.39) | 1.19* (1.01,1.39) |
| 2 waves | 1.47*** (1.24,1.73) | 1.40*** (1.18,1.67) | 1.31** (1.08,1.59) | 1.35** (1.08,1.68) |
| 3 waves | 1.49* (1.07,2.08) | 1.15 (0.77,1.71) | 1.42* (1.03,1.96) | 1.14 (0.74,1.76) |
| 4 waves | 1.91 (0.82,4.44) | 1.63 (0.62,4.28) | 1.91 (0.79,4.61) | 1.63 (0.59,4.50) |
| p for trend | 0.000 | 0.000 | 0.000 | 0.001 |
Note:
p<0.001,
p<0.01,
p<0.05 (2-tailed test)
This model adjusts for age, sex, and race/ethnicity.
This model adjusts for age, sex, and race/ethnicity, and excludes those who were obese in Wave 1
Models 2 and 4 on Table 3 examine whether short sleep occurs prior to body mass outcomes by excluding respondents who were obese at Wave 1. Compared to the first model for each outcome, the odds ratios for the cumulative sleep variables are slightly attenuated, although two or three of the indicator variables remain significant for the 7-hour (Panel B), −0.50 SD (Panel D), and −0.75 SD (Panel E) standards.
Cumulative Exposure to Short Sleep and Body Mass
Table 4 shows models that predict the odds of obesity and elevated waist circumference with the NSF, 7-hour, −0.50 SD, and −0.75 SD standards, while adjusting for additional confounders. We exclude the −0.25 SD standard because it had the weakest association with the elevated body mass outcomes of all of the distribution-based measures, and we exclude the −1.00 SD standard because repeated exposure to extremely short sleep is rare (see Table 1). Each measure of cumulative exposure to short sleep has a graded association with the odds of obesity (Models 1 through 4) and elevated waist circumference (Models 5 through 8), although two or three of the indicators for the NSF and −0.75 SD standards fell from significance.
Table 4.
Odds ratios and 95% Cis for obesity and elevated waist circumference, Add Health.
| Obesity (kg/m2 ≥ 30.0)
|
Waist circumference above 75th percentile
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | Model 8 | |
|
|
|
|||||||
| NSF standard | 7-hour standard | −0.50 SD standard | −0.75 SD standard | NSF standard | 7-hour standard | −0.50 SD standard | −0.75 SD standard | |
| Below the specified sleep standard | ||||||||
| 0 waves | ref | ref | ref | ref | ref | ref | ref | ref |
| 1 wave | 1.02 (0.89,1.17) | 1.16* (1.02,1.33) | 1.18* (1.02,1.36) | 1.14* (1.01,1.30) | 1.07 (0.91,1.27) | 1.22* (1.05,1.42) | 1.23** (1.06,1.43) | 1.16* (1.00,1.33) |
| 2 waves | 1.16* (1.01,1.34) | 1.32*** (1.13,1.54) | 1.19* (1.03,1.37) | 1.19* (1.02 – 1.39) | 1.17 (0.99,1.38) | 1.31** (1.08 – 1.58) | 1.23* (1.04,1.46) | 1.20* (1.00,1.44) |
| 3 waves | 1.17 (0.98,1.39) | 1.29* (1.03,1.62) | 1.27* (1.05,1.54) | 1.36* (1.07,1.71) | 1.14 (0.92,1.41) | 1.32* (1.01,1.72) | 1.27* (1.01,1.60) | 1.2 (0.93,1.55) |
| 4 waves | 1.38* (1.02,1.85) | 1.55* (1.02,2.37) | 1.45* (1.03,2.04) | 1.59 (0.95,2.65) | 1.45* (1.07,1.96) | 1.49 (0.96,2.32) | 1.45* (1.02,2.06) | 1.56 (0.94,2.60) |
| Height in cm | 1.04*** (1.03,1.05) | 1.04*** (1.03,1.05) | 1.04*** (1.03,1.05) | 1.04*** (1.03,1.05) | ||||
| Male | 0.91 (0.73,1.12) | 0.89 (0.72,1.11) | 0.91 (0.74,1.12) | 0.91 (0.74,1.13) | 0.56*** (0.44,0.72) | 0.55*** (0.43,0.71) | 0.56*** (0.44,0.72) | 0.56*** (0.44,0.72) |
| Age | 1.03* (1.00,1.06) | 1.02 (0.99,1.05) | 1.03* (1.00,1.06) | 1.03 (1.00,1.06) | 1.03 (1.00,1.06) | 1.01 (0.98,1.05) | 1.03 (1.00,1.06) | 1.02 (0.99,1.06) |
| Race/ethnicity | ||||||||
| White | ref | ref | ref | ref | ref | ref | ref | ref |
| Black | 1.54*** (1.37,1.72) | 1.52*** (1.36,1.70) | 1.53*** (1.36,1.71) | 1.52*** (1.36,1.70) | 1.26** (1.10,1.44) | 1.24** (1.08,1.42) | 1.24** (1.09,1.43) | 1.25** (1.08,1.43) |
| Hispanic | 1.37** (1.11,1.69) | 1.37** (1.11,1.68) | 1.37** (1.11,1.69) | 1.36** (1.11,1.68) | 1.18 (0.95,1.45) | 1.17 (0.95,1.45) | 1.17 (0.95,1.45) | 1.17 (0.95,1.45) |
| Asian | 0.82 (0.53,1.26) | 0.82 (0.53,1.25) | 0.82 (0.53,1.26) | 0.82 (0.53,1.25) | 1.66* (1.03,2.68) | 1.66* (1.03,2.67) | 1.65* (1.02,2.68) | 1.67* (1.03,2.69) |
| Native American | 1.40 (0.62,3.15) | 1.38 (0.61,3.12) | 1.36 (0.60,3.07) | 1.38 (0.61,3.12) | 0.93 (0.39,2.23) | 0.92 (0.38,2.21) | 0.9 (0.37,2.18) | 0.92 (0.38,2.20) |
| Other | 0.76 (0.47,1.23) | 0.76 (0.47,1.23) | 0.76 (0.47,1.23) | 0.75 (0.47,1.22) | 0.61 (0.34,1.09) | 0.61 (0.34,1.08) | 0.61 (0.34,1.08) | 0.61 (0.34,1.08) |
| Foreign born (=1) | 0.70** (0.54,0.90) | 0.70** (0.54,0.91) | 0.70** (0.54,0.90) | 0.70** (0.55,0.91) | 0.75 (0.55,1.02) | 0.75 (0.55,1.03) | 0.75 (0.55,1.02) | 0.75 (0.55,1.03) |
| Never pregnant/male at Wave 4 | ref | ref | ref | ref | ref | ref | ref | ref |
| Ever pregnant | 1.00 (0.79,1.25) | 0.99 (0.79,1.25) | 0.99 (0.79,1.25) | 0.99 (0.79,1.25) | 0.91 (0.69,1.20) | 0.91 (0.69,1.19) | 0.91 (0.69,1.20) | 0.91 (0.69,1.19) |
| Currently pregnant | 1.42* (1.04,1.95) | 1.43* (1.04,1.95) | 1.43* (1.04,1.96) | 1.43* (1.04,1.95) | 1.96*** (1.37,2.81) | 1.97*** (1.38,2.82) | 1.97*** (1.38,2.82) | 1.96*** (1.37,2.80) |
| Mother’s education | 0.96*** (0.93,0.98) | 0.96*** (0.94,0.98) | 0.96*** (0.94,0.98) | 0.96*** (0.93,0.98) | 0.95*** (0.93,0.98) | 0.95*** (0.93,0.98) | 0.95*** (0.93,0.98) | 0.95*** (0.93,0.98) |
| Father’s education | 0.95*** (0.93,0.97) | 0.95*** (0.93,0.97) | 0.95*** (0.93,0.97) | 0.95*** (0.93,0.97) | 0.94*** (0.92,0.96) | 0.94*** (0.92,0.96) | 0.94*** (0.92,0.96) | 0.94*** (0.92,0.96) |
| Family income at Wave 1, ln | 0.98 (0.94,1.03) | 0.98 (0.93,1.03) | 0.98 (0.93,1.03) | 0.98 (0.93,1.03) | 0.97 (0.93,1.01) | 0.97 (0.93,1.01) | 0.97 (0.93,1.01) | 0.97 (0.93,1.01) |
| Parents’ marital status at Wave 1 | ||||||||
| Never married | ref | ref | ref | ref | ref | ref | ref | ref |
| Married | 0.89 (0.69,1.15) | 0.89 (0.70,1.15) | 0.89 (0.70,1.15) | 0.89 (0.70,1.15) | 0.84 (0.63,1.11) | 0.84 (0.63,1.11) | 0.84 (0.63,1.11) | 0.84 (0.63,1.11) |
| Previously married | 0.90 (0.72,1.12) | 0.9 (0.72,1.12) | 0.89 (0.72,1.11) | 0.9 (0.72,1.12) | 0.85 (0.65,1.12) | 0.85 (0.65,1.12) | 0.85 (0.64,1.11) | 0.85 (0.65,1.12) |
| Mother ever smoked (=1) | 1.20*** (1.08,1.33) | 1.19** (1.07,1.33) | 1.19** (1.07,1.33) | 1.19** (1.08,1.33) | 1.15* (1.02,1.29) | 1.14* (1.02,1.28) | 1.14* (1.02,1.28) | 1.15* (1.02,1.29) |
| Father ever smoked (=1) | 0.95 (0.85,1.07) | 0.95 (0.85,1.07) | 0.95 (0.85,1.07) | 0.95 (0.85,1.07) | 1.04 (0.92,1.19) | 1.04 (0.92,1.18) | 1.04 (0.92,1.18) | 1.04 (0.92,1.18) |
| Mother obese (=1) | 2.12*** (1.84,2.44) | 2.11*** (1.83,2.43) | 2.12*** (1.84,2.44) | 2.11*** (1.83,2.43) | 2.37*** (2.03,2.77) | 2.36*** (2.02,2.75) | 2.36*** (2.02,2.76) | 2.36*** (2.02,2.76) |
| Father obese (=1) | 1.98*** (1.68,2.32) | 1.97*** (1.68,2.31) | 1.98*** (1.68,2.32) | 1.97*** (1.68,2.32) | 1.97*** (1.66,2.34) | 1.97*** (1.66,2.33) | 1.98*** (1.67,2.34) | 1.97*** (1.66,2.33) |
| Constant | 0.74 (0.28,1.91) | 1.02 (0.39,2.65) | 0.72 (0.28,1.88) | 0.78 (0.30,2.02) | 0.00*** (0.00,0.00) | 0.00*** (0.00,0.01) | 0.00*** (0.00,0.00) | 0.00*** (0.00,0.00) |
Note:
p<0.001,
p<0.01,
p<0.05 (2-tailed test)
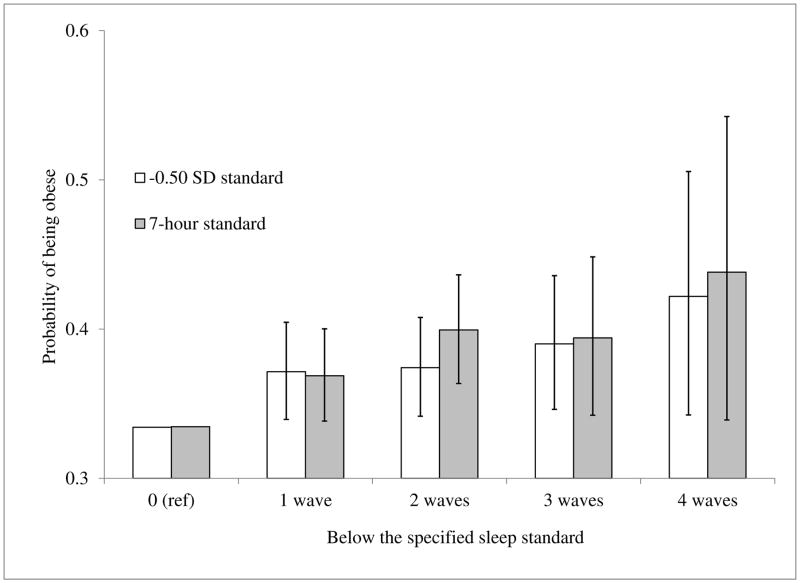
Figure 1 illustrates the dose-response association between the predicted probability of being obese and cumulative exposure to short sleep. We calculate the predicted probabilities from Model 2 (7-hour standard) and Model 3 (−0.50 SD standard) of Table 4, when the covariates are set to their mean values. Consistent with the results on Table 4, the association between cumulative exposure to short sleep and the probability of being obese is slightly stronger for the 7-hour standard than for the −0.50 SD standard, but the 95% confidence intervals are somewhat wider.
Figure 1.
Probability of being obese and cumulative exposure to short sleep (derived from Table 4)
DISCUSSION
The hypothesized hormonal (Hitze et al., 2008) and behavioral (Beebe et al., 2013, McKnight-Eily et al., 2011) mechanisms suggest that persistent exposures to short sleep will have stronger associations with body mass than short-term exposures. We find a dose-response association that is consistent with the hypothesis that sleep duration is causally associated with body mass, although we cannot rule out the possibility of unobserved confounders with observational data. After adjusting for numerous confounders, those who report short sleep in all four waves, as compared to those who do not report short sleep in any wave, have increased odds of obesity and elevated waist circumference that are comparable in magnitude to the odds ratio for obesity when comparing blacks to whites.
Two measures of short sleep perform similarly well. The 7-hour standard that is often used among adults (Cappuccio et al., 2008, Chaput et al., 2008) is also predictive of obesity and elevated waist circumference when applying that standard to adolescents. Although the 7-hour standard fails to consider the potential for changing sleep needs throughout adolescence and early adulthood, it is easy to use in clinical settings as a marker for obesity risk. Our findings affirm the NSF report, which asserts that sleeping fewer than 7 hours per night is particularly harmful for children aged 6 through 17 (Hirshkowitz et al., 2015). Failure to meet the −0.50 SD standard is also persistently associated with body mass outcomes in early adulthood, and reflects smoothly changing sleep needs throughout the ages examined.
Our distribution-based approach has limitations similar to other approaches that classify individuals based on the distribution of their peers (e.g., the CDC’s definition of overweight and obesity among children). In our case, definitions of “short sleep” are based on an empirical distribution, even though the average child may not be getting adequate sleep (Calamaro et al., 2009, Chen et al., 2008). Nevertheless, we tested various distribution-based thresholds and found that children who occasionally sleep −0.25 standard deviations or less than the average for their age and sex do not have consistently elevated body mass outcomes. Thus, adolescents and young adults who report the average sleep duration for their age and sex group, appear to have adequate sleep—at least in terms of body mass outcomes. Further, distribution-based methods provide a smoothly-changing set of values for adequate sleep, rather than the sharp changes at specific ages implied by the NSF standards (Hirshkowitz et al., 2015), which were only weakly associated with body mass outcomes.
The strengths of our study include the use of a large, nationally representative, 15-year prospective cohort of adolescents and young adults in the United States. Add Health provides repeated measures of sleep duration and objective measures of height and weight. Separate analyses (not shown) show similar results when adjusting for “current” sleep duration at Wave 4. Ancillary analyses (not shown) also find similar results when examining the waist-to-height ratio as an outcome. Our study is limited by relying on self-reported sleep duration. However, respondents with higher BMIs who are most likely to experience sleep apnea may be most likely to over-state their sleep durations (Weaver et al., 2004), which would tend to bias our results toward smaller associations.
In sum, cumulative exposure to short sleep appears to be an important risk factor for obesity and elevated waist circumference. The dose-response association between repeated (rather than on-time) exposures to short sleep duration provides evidence that is consistent with a causal association between sleep duration and body mass outcomes in adolescence and early adulthood. Our findings are particularly important given mixed results in existing longitudinal studies of adolescents (Lumeng et al., 2007, Snell et al., 2007, Suglia et al., 2014). Adolescence is a period marked by rapid changes in weight and sleep duration, which may presage adverse cardiovascular and metabolic outcomes throughout adulthood. Our findings strengthen the case for clinical, public health, and policy interventions that focus on ensuring adequate sleep throughout adolescence.
Supplementary Material
Acknowledgments
We acknowledge research support from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK grant R21DK08941), and administrative and computing support from the Eunice Kennedy Shriver National Institute of Child Health and Human Development-funded University of Colorado Population Center (grant R24 HD066613). We also acknowledge the researchers and funding agencies that provided the publicly available Add Health data: http://www.cpc.unc.edu/projects/addhealth We thank Jennifer Yland at Stony Brook University for her helpful comments on a previous draft of this paper.
Footnotes
Author Contributions: Krueger, Reither, Peppard, and Hale contributed to the conceptualization of the paper. Krueger led the data analysis and wrote the first draft of the manuscript. Reither, Peppard, and Hale provided critical comments on the data analysis. Krueger, Reither, Peppard, Burger, and Hale all provided critical and substantial revisions to the final manuscript, and approve the final document.
Conflicts of Interest and Source of Funding: The authors have no conflicts of interest to declare.
References
- Agras WS, Hammer LD, Mcnicholas F, Kraemer HC. Risk factors for childhood overweight: a prospective study from birth to 9.5 years. J Pediatr. 2004;145:20–25. doi: 10.1016/j.jpeds.2004.03.023. [DOI] [PubMed] [Google Scholar]
- Beebe DW, Simon S, Summer S, Hemmer S, Strotman D, Dolan LM. Dietary intake following experimentally restricted sleep in adolescents. Sleep. 2013;36:827–34. doi: 10.5665/sleep.2704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calamaro CJ, Mason TB, Ratcliffe SJ. Adolescents living the 24/7 lifestyle: effects of caffeine and technology on sleep duration and daytime functioning. Pediatrics. 2009;123:e1005–e10. doi: 10.1542/peds.2008-3641. [DOI] [PubMed] [Google Scholar]
- Cappuccio FP, Taggart FM, Kandala NB, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619–26. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chantala K. Guidelines for analyzing Add Health data. Carolina Population Center, University of North Carolina; Chapel Hill, Chapel Hill, NC: 2006. [Google Scholar]
- Chaput JP, Després JP, Bouchard C, Tremplay A. The association between sleep duration and weight gain in adults: a 6-year prospective study from the Quebec Family Study. Sleep Med Rev. 2008;31:517–23. doi: 10.1093/sleep/31.4.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X, Beydoun MA, Wang Y. Is Sleep Duration Associated With Childhood Obesity? A Systematic Review and Meta-analysis. Obesity. 2008;16:265–74. doi: 10.1038/oby.2007.63. [DOI] [PubMed] [Google Scholar]
- Entzel P, Whitsel EA, Richardson A, et al. Add Health Wave IV documentation: cardiovascular and anthropometric measures. Carolina Population Center, University of North Carolina; Chapel Hill, Chapel Hill, NC: 2009. [Google Scholar]
- Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, Blood Institute scientific statement. Circulation. 2005;112:2735–52. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health: Journal of the National Sleep Foundation. 2015;1:40–43. doi: 10.1016/j.sleh.2014.12.010. [DOI] [PubMed] [Google Scholar]
- Hitze B, Bosy-Westphal A, Bielfeldt F, et al. Determinants and impact of sleep duration in children and adolescents: data of the Kiel obesity prevention study. Eur J Clin Nutr. 2008;63:739–46. doi: 10.1038/ejcn.2008.41. [DOI] [PubMed] [Google Scholar]
- Javaheri S, Storfer-Isser A, Rosen CL, Redline S. Sleep quality and elevated blood pressure in adolescents. Circulation. 2008;118:1034–40. doi: 10.1161/CIRCULATIONAHA.108.766410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korn EL, Graubard BI. Analysis of health surveys. Wiley; New York: 1999. [Google Scholar]
- Krueger PM, Burgard SA. Work, occupation, income, and mortality. In: ROGERS RG, MCRIMMINS E, editors. International Handbood of Adult Mortality. Springer; New York: 2011. pp. 263–88. [Google Scholar]
- Krueger PM, Friedman EM. Sleep duration in the United States: a cross-sectional population based study. American Journal of Epidemiology. 2009;169:1052–63. doi: 10.1093/aje/kwp023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruger AK, Reither EN, Peppard PE, Krueger PM, Hale L. Do sleep-deprived adolescents make less-healthy food choices? British Journal of Nutrition. 2014;111:1898–904. doi: 10.1017/S0007114514000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: methods and development. National Center for Health Statistics: Vital and Health Statistics. 2002;11:1–190. [PubMed] [Google Scholar]
- Landhuis CE, Poulton R, Welch D, Hancox RJ. Childhood sleep time and long-term risk for obesity: a 32-year prospective birth cohort study. Pediatrics. 2008;122:955–60. doi: 10.1542/peds.2007-3521. [DOI] [PubMed] [Google Scholar]
- Larkin EK, Rosen CL, Kirchner L, et al. Variation of c-reactive protein levels in adolescents: association with sleep-disordered breathing and sleep duration. Circulation. 2005;111:1978–84. doi: 10.1161/01.CIR.0000161819.76138.5E. [DOI] [PubMed] [Google Scholar]
- Lee K, Carlin J. Multiple imputation of missing data: a fully conditional specification versus multivariate normal imputation. Am J Epidemiol. 2010;171:624–32. doi: 10.1093/aje/kwp425. [DOI] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. 2. Wiley; Hoboken, NJ: 2002. [Google Scholar]
- Lumeng JC, Somashekar D, Appugliese D, Kaciroti N, Corwyn RF, Bradley RH. Shorter sleep duration is associated with increased risk for being overweight at ages 9 to 12 years. Pediatrics. 2007;120:1020–29. doi: 10.1542/peds.2006-3295. [DOI] [PubMed] [Google Scholar]
- Magee L, Hale L. Longitudinal associations between sleep duration and subsequent weight gain: a systematic review. Sleep Med Rev. 2012;16:231–41. doi: 10.1016/j.smrv.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsh LC, Cormier DR. Spline regression models. Sage; Thousand Oaks, CA: 2002. [Google Scholar]
- Matricciani LA, Olds TS, Blunden S, Rigney G, Williams MT. Never enough sleep: a brief history of sleep recommendations for children. Pediatrics. 2012;129:548–56. doi: 10.1542/peds.2011-2039. [DOI] [PubMed] [Google Scholar]
- Mcknight-Eily LR, Eaton DK, Lowry R, Croft JB, Presley-Cantrell L, Perry GS. Relationship between hours of sleep and health-risk behaviors in US adolescent students. Preventive Medicine. 2011;54:271–73. doi: 10.1016/j.ypmed.2011.06.020. [DOI] [PubMed] [Google Scholar]
- Moons KGM, Donders RaRT, Stijnen T, Harrell FE., Jr Using the outcome for imputation of missing predictor values was preferred. Journal of Clinical Epidemiology. 2006;59:1092–101. doi: 10.1016/j.jclinepi.2006.01.009. [DOI] [PubMed] [Google Scholar]
- Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity. 2008;16:643–53. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel SR, Malhotra A, White DP, Gottlieb DJ, Hu FB. Association between reduced sleep and weight gain in women. Am J Epidemiol. 2006;164:947–55. doi: 10.1093/aje/kwj280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reilly JJ, Armstrong J, Dorosty AR, et al. Early life risk factors for obesity in childhood: cohort study. Br Med J. 2005;330:1–7. doi: 10.1136/bmj.38470.670903.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reither EN, Krueger PM, Hale L, Reiter E, Peppard PE. Ethnic variation in the association between sleep and body mass among U.S. adolescents. International Journal of Obesity. 2014;38:944–9. doi: 10.1038/ijo.2014.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snell EK, Adam EK, Duncan GJ. Sleep and the body mass index and overweight status of children and adolescents. Child Dev. 2007;78:309–23. doi: 10.1111/j.1467-8624.2007.00999.x. [DOI] [PubMed] [Google Scholar]
- Snijders TaB, Bosker RJ. Multilvel analysis: an introduction to basic and advanced multilevel modeling. Sage; Thousand Oaks, CA: 2011. [Google Scholar]
- Statacorp. Stata: release 13. Statistical software. StataCorp, LP; College Station, TX: 2013. [Google Scholar]
- Suglia SF, Kara S, Robinson WR. Sleep duration and obesity among adolescents transitioning to adulthood:do results differ by sex? J Pediatr. 2014 doi: 10.1016/j.jpeds.2014.06.052. Available online 25 July 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taheri S. The link between short sleep duration and obesity: we should recommend more sleep to prevent obesity. Archives of Disease in Childhood. 2006;91:881–84. doi: 10.1136/adc.2005.093013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS medicine. 2004;1:e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taveras EM, Rifas-Shiman SL, Oken E, Gunderson EP, Gillman MW. Short sleep duration in infancy and risk of childhood overweight. Archives of Pediatric and Adolescent Medicine. 2008;162:305–11. doi: 10.1001/archpedi.162.4.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Touchette E, Petit D, Tremblay RE, et al. Associations between sleep duration patterns and overweight/obesity at age 6. Sleep. 2008;31:1507–14. doi: 10.1093/sleep/31.11.1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver EM, Kapur V, Yueh B. Polysomnography vs self-reported measures in patients with sleep apnea. Archives of Otolaryngology-Head & Neck Surgery. 2004;130:453–58. doi: 10.1001/archotol.130.4.453. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.