Abstract
Background
Craniofacial growth pattern has been correlated with variations in size of the upper airway spaces. The objective of this study was to evaluate the nasopharyngeal, oropharyngeal, and hypopharyngeal airway spaces variations according to the craniofacial growth pattern, by comparing brachyfacial, mesofacial, and dolichofacial in Angle Class I individuals.
Methods
To measure the spaces, 45 lateral teleradiographs were used and divided into 3 groups per the craniofacial growth pattern, determined by the Tweed cephalometry angular measurements: FMA and Y-axis. To evaluate the airways, sleep apnea cephalometry was used, containing 28 points that compose 14 factors. Three groups were compared relative to each of the 14 sleep apnea cephalometry measurements. Adherence test to the normal curve was performed. For the non-normally distributed data—measurement of the inferior pharyngeal space—the Kruskal-Wallis test was used for comparison between the groups. For the remaining data, the distribution was normal and ANOVA test was used.
Results
Statistically significant difference was verified among the groups for the measurement of the median posterior-palatal space, with the difference being pointed out by the post hoc test between the brachyfacial and dolichofacial groups. For the other measurements, there was no statistically significant difference.
Conclusions
It could be concluded that there was difference in the median posterior-palatal space measurement, in the oropharynx region, which was reduced for individuals with a dolichofacial pattern.
Keywords: Orthodontics, Cephalometry, Nasopharynx, Oropharynx, Hypopharynx, Facial types
Background
The upper airway is composed of the nasopharynx, oropharynx, and hypopharynx. Pharyngeal space size is determined primarily by the relative growth and size of the soft tissues surrounding the dentofacial skeleton [1, 2].
A normal upper airway improves nasal breathing and is considered important in the growth and development of craniofacial structures [1, 2].
An obstructive upper airway is present when obstructive processes of a morphological, physiological, or pathological nature occur, such as hypertrophy of adenoids and tonsils, chronic and allergic rhinitis, irritant environmental factors, infections, congenital nasal deformities, nasal traumas, polyps, and tumors cause functional imbalance and result in oral breathing patterns [3].
The upper airway dimensions may be influenced by the facial skeletal pattern, in which the relationship between the position of the maxilla and mandible in the anteroposterior direction has great influence on space [1].
There are studies in the literature about changes in the upper airways resulting from orthodontic treatment, orthognathic surgery or in individuals diagnosed with sleep apnea [4–7]; however, few studies have shown evidence of the airspace related to facial types and Angle Class I individuals, and this information is relevant to assist in orthodontic planning.
The aim of the present study was to evaluate the nasopharyngeal, oropharyngeal, and hypopharyngeal airway spaces in brachyfacial, mesofacial, and dolichofacial in Angle Class I individuals.
Methods
Sample characteristics and data collection
The sample size calculation for the difference between two measurements was made considering the test power of 80 and 95% confidence coefficient. The values with reference to the mean and standard deviation of the variable median posterior palatal space when compared with two independent groups, and the estimate of the minimum difference to be detected, required for the calculation, were retrieved from the previous results [8].
The sample was composed of 45 digital lateral head teleradiographs of adult individuals, with permanent dentition, skeletal Class I determined by Steiner’s variable ANB [8], mean SNA of 82.65° (standard deviation = 1.94), and SNB 81.11° (standard deviation 1.95).
Excluded from the study were teleradiographs lacking distinctness of structures in the image, previous history of palatine tonsil and/or pharyngeal tonsil surgeries, orthodontic treatment and/or orthognathic surgeries, volunteers submitted to extractions, or those with dental agenesis.
Teleradiographs were obtained by using the same equipment (Cranex D® Soredex Orion Corporation, Tuusula, Finland).
The cephalometric analyses were performed digitally by means of the Radiocef Studio 2 program (Radiomemory Ltda, MG, Brazil), using a resolution of 300 dpi for the teleradiographs [9]. For this purpose, the radiographs were digitized by a table scanner (Cranex D® Soredex Orion Corporation, Tuusula, Finland) [10], coupled to a transparency reader, using a resolution of 300 dpi, and saved in TIFF format (Tagged Image File Format) without compression.
The measurements were performed by a single, blinded, duly calibrated examiner. Intra-examiner reliability was tested by re-doing 30% of the cephalometric analyses. Five teleradiographs were randomly selected from each group, totaling 15 teleradiographs of patients whose sleep apnea cephalometries were repeated after 30 days.
The Tweed FMA [11] and Y-Axis measurements were used to select the facial type. Teleradiographs were randomly selected at a radiology center and classified according to the FMA and Y-axis, and all teleradiographs presented the same FMA measures and Y-axis classification. The FMA measurement corresponded to the angle between the mandibular plane (GoMe) and the Frankfort plane (PoOr), and its reference value was 25°. Values above 30° were considered a vertical growth trend (dolichofacial); below 20°, a horizontal trend (brachyfacial), and the Y-axis, also called the angle of facial growth, formed by the sella-gnathion line and the Frankfort horizontal plane intersection. The mean value was 59°. An increase in this value indicated a vertical growth trend, and a reduction, a horizontal growth trend [12].
Fifteen teleradiographs were selected of each craniofacial growth pattern, classified into mesofacial (5 males and 10 females, aged 16–31 years, mean age = 22.21), brachyfacial (8 males and 7 females, aged 17–34 years, mean age = 25.6), and dolichofacial patterns (11 male e 4 females, aged 16–31, mean age = 25.0). To evaluate the upper airways, sleep apnea cephalometry, validated for Brazilians [8], was used, containing 28 points that compose 14 factors (Figs. 1, 2, 3, 4, 5 and 6).
Fig. 1.
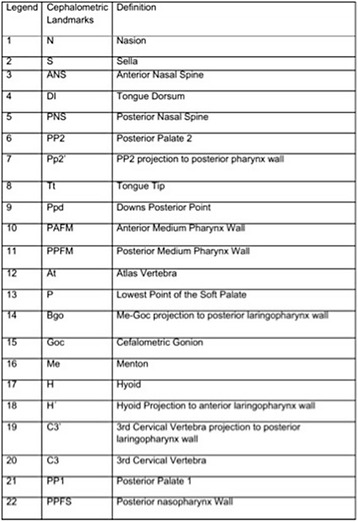
Factors for sleep apnea analysis
Fig. 2.
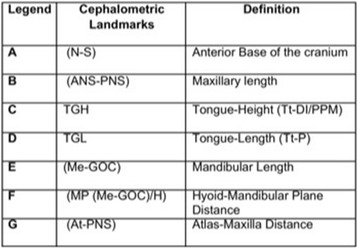
Legend, cephalometric landmarks, and definition for sleep apnea analysis
Fig. 3.
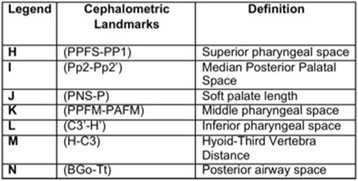
Legend, cephalometric landmarks, and definition
Fig. 4.
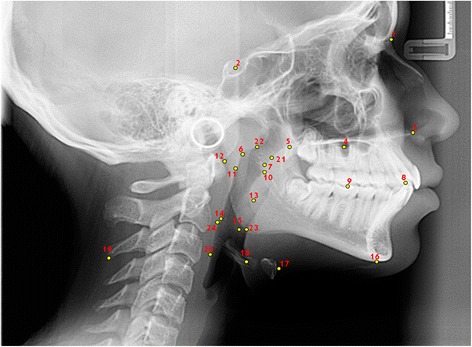
Cephalometric landmarks for sleep apnea analysis
Fig. 5.
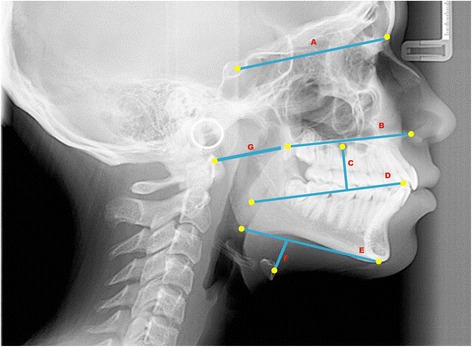
Cephalometric planes (cranial base, maxilla, mandibulla, nasopharynx and hyoid-mandibular plane distance)
Fig. 6.
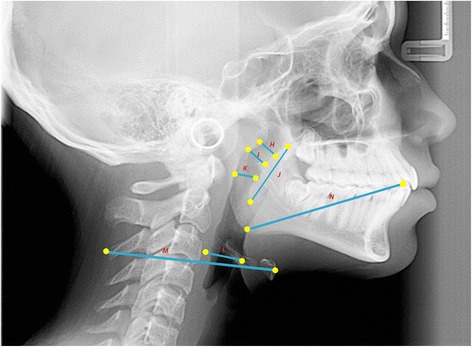
Cephalometric planes (oropharynx and laryngopharynx) for sleep apnea analysis
Statistical analysis
The groups were compared for each of the 14 factors. For the inferior airway space measurement that presented non normal distribution, the Kruskal-Wallis test was used for inter-group comparison. For the remaining data, whose distribution was normal, one-way ANOVA followed by complementary Tukey tests was used. The significance level was 5%.
Results
The Intraclass Correlation Coefficient (ICC) showed excellent replicability (0.9636).
In the comparison of the three groups for each of the 14 sleep apnea cephalometric measures, statistically significant difference was verified among the groups for the median posterior palatal space (p = 0.020), with the complementary Tukey test pointing out difference between the brachyfacial and dolichofacial groups.
When the measurements presented in Table 1 were analyzed, it was verified that the median posterior palatal measurement in the oropharyngeal region was lower for individuals with a dolichofacial (10.64 ± 1.83) pattern when compared with mesofacial (12.64 ± 2.30) and brachyfacial (12.91 ± 2.74) patterns.
Table 1.
Mean and standard deviation of the 14 factors of sleep apnea cephalometry and the respective p values of the comparison among the groups
| Measurements | Brachyfacial | Mesiofacial | Dolichofacial | p values | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Cranial base | |||||||
| Anterior base of the cranium (N-S) | 69.82 | 5.49 | 67.86 | 4.27 | 66.45 | 5.34 | 0.203 |
| Maxilla/mandibulla | |||||||
| Maxillary length (ANS-PNS) | 53.93 | 3.88 | 54.12 | 3.39 | 53.44 | 3.87 | 0.877 |
| Mandibular length (Me-Goc) | 70.74 | 6.27 | 72.01 | 6.50 | 70.96 | 3.38 | 0.803 |
| Nasopharynx | |||||||
| Atlas-maxilla distance (At-PNS) | 38.59 | 4.08 | 37.74 | 4.91 | 35.22 | 3.25 | 0.080 |
| Superior pharyngeal space (PPFS-PP1) | 15.8 | 2.27 | 13.68 | 2.53 | 14.09 | 6.42 | 0.352 |
| Oropharynx | |||||||
| Middle pharyngeal space (PPFM-PAFM) | 11.42 | 2.97 | 13.68 | 2.53 | 12.03 | 4.03 | 0.474 |
| TGL (tongue length) (Tt-P) | 71.51 | 4.59 | 69.41 | 6.58 | 67.95 | 5.43 | 0.186 |
| TGH (tongue height) (Tt-DI/P) | 23.85 | 5.27 | 22.3 | 3.45 | 20.70 | 3.43 | 0.129 |
| Median posterior palatal space (Pp2-Pp2’) | 12.91a | 2.74 | 12.64ab | 2.30 | 10.64b | 1.83 | 0.020* |
| Soft palate length (PNS-P) | 34.39 | 8.42 | 31.07 | 4.16 | 33.12 | 3.96 | 0.307 |
| Laryngopharynx | |||||||
| Inferior pharyngeal space (C3’-H’) | 16.83 | 5.33 | 14.00 | 4.79 | 12.79 | 4.72 | 0.063 |
| Posterior airway space (BGo-Tt) | 14.11 | 2.69 | 13.36 | 4.11 | 12.31 | 2.86 | 0.328 |
| Hyoid-third vertebra distance (H-C3) | 76.29 | 7.62 | 79.24 | 6.62 | 76.57 | 6.39 | 0.442 |
| Hyoid-mandibular plane distance (MP (Me-Goc)/H) | 18.95 | 4.37 | 15.97 | 4.97 | 18.74 | 5.53 | 0.201 |
Values marked by distinct letters are significantly different from each other Tukey test (p < 0.05)
For the other measurements, there was no statistically significant difference (p > 0.05). However, for the dolichofacial group, it was observed that on an average, numerically, the inferior pharyngeal space measurements (12.79 ± 4.72), atlas-maxilla distance (35.22 ± 3.25), and posterior airway space (12.31 ± 2.86) were shown to be smaller in comparison with those of the other facial types.
Discussion
The contribution of this study was to present the use of a cephalometric analysis, commonly used in orthodontics, with the aim of identifying anatomical changes in the upper airways, which may predispose to respiratory disorders.
Cephalometric performed by means of lateral teleradiography has been shown to be an important instrument in the multidisciplinary field for evaluating the upper airways [13, 14] because it is easily accessible and low cost, highly reproducible, and the individual is submitted to a low dose of radiation [4, 15]. Thus, innumerable studies have sought associations of the physical characteristics related to these airway spaces, as a way of predicting pathologies [13–20].
However, there are studies that use computed tomography for morphological evaluation of the airway spaces, particularly due to the possibility of measuring areas and volumes, which is impossible to do by means of other radiographic exams [21–23]. Therefore, the authors point out that one of the limitations of the present study refer to not measuring the airway volumes, due to the type of exam used for evaluation [24]. There was also difficulty in the methodologies with two-dimensional radiographs when performing superimposition of tracings [25]; however, in the present study, no superimpositions were made. Many studies have evaluated the airways by using lateral cephalograms and associated their dimensions with the vertical skeletal pattern of the face and facial morphology [1, 26, 27]. A recent longitudinal study also used lateral cephalometric radiographs for associating changes in the morphology of the nasopharyngeal space in different facial patterns [28], which did not make this method of evaluation unfeasible.
In this study, the authors opted to use the sleep apnea cephalometry instrument because it has been validated for Brazilians and presents standard values that may be used as reference [8].
The authors were able to identify reduction in the median posterior palatal space in individuals with a dolichofacial pattern. A previous study also observed changes in the dimensions of the upper airway related to the reduction in the medial posterior palatal space in individuals with the obstructive sleep apnea syndrome (OSAS) [8]. This measurement expresses the distance from the soft palate to the posterior wall of the pharynx and has a close relationship with the dimensions of the soft palate. The increased length of which was related to presence of OSAS in other researches [8, 29, 30] and the present study. The highest alteration values in upper airway dimensions in OSAS patients occur in the oropharynx [8] and were related to the reduction of the median posterior palatal space [31]. In individuals with a vertical pattern, the mandible is normally retracted and rotated downwards and backwards, thus diminishing the oropharyngeal space [26] Furthermore, the base of the tongue accompanies the direction of mandibular rotation, being positioned downward and backward, thus the soft palate is in a more retrusive position, diminishing the median posterior palatal space.
Some authors have pointed out that when the nasopharyngeal space was reduced, there would be a tendency towards neuromuscular adaptation, leading to vertical growth of the face that is associated with a dolichofacial pattern [14, 21]. However, in this study, no difference was found in the upper airway dimensions in the nasopharyngeal region in the studied volunteers with this facial type. This could be attributed to different sample characteristics in others studies in which the sample was composed of the youngest participants [1, 26]. This aged group could be more susceptible to narrower nasopharyngeal airway spaces due to adenotonsillar hypertrophy, for example [32, 33]. In addition, authors [1] compared Angle Classes I and II, differently from the present study, in which the sample was composed of only Class I patients.
Obstruction of the upper airways forces the patient to breathe through the mouth, and in addition to OSAS, these factors cause oral dysfunction, such as lip incompetence, low position of the tongue in the floor of the mouth, tongue thrust, and may lead to unbalanced muscle and function [32] disturbances in swallowing, mastication, speech [34], and stability of occlusion [35].
This study was performed using two-dimensional digital lateral cephalogram that is a limitation. Therefore, it is important to recognize that three-dimensional evaluation of the airways by means of cone-beam computed tomography, respecting legal and ethical aspects, due a higher dose of radiation, could be useful for improved assessment in further studies to minimize this limitation.
Conclusions
Under the conditions of this study and considering the results, the authors could conclude that there were no differences in nasopharyngeal and hypopharyngeal airway spaces in brachyfacial and mesofacial individuals. Oropharyngeal space reduction was observed in Angle Class I dolichofacial individuals, characterized by reduction in the median posterior palatal measurement.
Authors’ contributions
RS, VVD, GCV, and CCdM conceived and designed the experiments. RS, GCV, LACM, and JCS performed the experiment. GCV, CCdM, and VVD analyzed the data. RS, GCV, LACM, and JBS contributed material/analysis tools. RS, VVD, GCV, and CCdM wrote the manuscript. RS, VVD, GCV, LACM, and JCBS prepared the figures and tables. VVD, GCV, and CCdM reviewed drafts of the paper. All authors read and approved the final manuscript.
Ethics approval and consent to participate
This retrospective study was approved by the Research Ethics Committee of the institution at which the study was conducted (no. 33799614.1.0000.5385).
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Roselaine Sprenger, Email: rose_sprenger@hotmail.com.
Luciano Augusto Cano Martins, Email: luciano_cano@hotmail.com.
Júlio Cesar Bento dos Santos, Email: radius@nteecon.com.br.
Carolina Carmo de Menezes, Email: carol.menezes.odonto@gmail.com.
Giovana Cherubini Venezian, Email: giovanavenezian@hotmail.com.
Viviane Veroni Degan, Email: vvdegan@gmail.com.
References
- 1.Lopatienė K, Dabkutė A, Juškevičiūtė V. Vertical and sagittal morphology of the facial skeleton and the pharyngeal airway. Stomatologija. 2016;18(1):21–25. [PubMed] [Google Scholar]
- 2.Ghoneima A, Albarakati S, Jiang F, Kula K, Wasfy T. Computational fluid dynamics analysis of the upper airway after rapid maxillary expansion: a case report. Prog Orthod. 2015;16:10. doi: 10.1186/s40510-015-0085-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Claudino LV, Mattos CT, Ruellas AC, Sant’ Anna EF. Pharyngeal airway characterization in adolescents related to facial skeletal pattern: a preliminar study. Am J Orthod Dentofacial Orthop. 2013;143(6):799–809. doi: 10.1016/j.ajodo.2013.01.015. [DOI] [PubMed] [Google Scholar]
- 4.Borges PTM, Silva BM, Neto JMM, Borges NE, Li ML. Cephalometric and anthropometric data of obstructive apnea in different age groups. Braz J Otorhinolaryngol. 2015;81(1):79–84. doi: 10.1016/j.bjorl.2014.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gornic C, Nascimento PP, Melgaço CA, Ruellas ACO, Medeiros PJA, Sant’ Anna EF. Cephalometric analysis of the upper airways of Class III patients subjected to orthosurgical treatment. Dental Press J Orthod. 2011;16(5):82–88. doi: 10.1590/S2176-94512011000500013. [DOI] [Google Scholar]
- 6.Fernández-Ferrer L, Montiel-Company JM, Pinho T, Almerich-Silla JM, Bellot-Arcís C. Effects of mandibular setback surgery on upper airway dimensions and their influence on obstructive sleep apnoea—a systematic review. J Craniomaxillofac Surg. 2015;43(2):248–253. doi: 10.1016/j.jcms.2014.11.017. [DOI] [PubMed] [Google Scholar]
- 7.Koay WL, Yang Y, Tse CS, Gu M. Effects of two-phase treatment with the Herbst and preadjusted edgewise appliances on the upper airway dimensions. ScientificWorldJournal. 2016;2016:4697467. doi: 10.1155/2016/4697467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maschtakow PSL, Tanaka JLO, Rocha JC, Giannasi LC, de Moraes ML, Costa CB, Castilho JCM, de Moraes LC. Cephalometric analysis for the diagnosis of sleep apnea: a comparative study between reference values and measurements obtained for Brazilian subjects. Dental Press J Orthod. 2013;18(3):143–149. doi: 10.1590/S2176-94512013000300023. [DOI] [PubMed] [Google Scholar]
- 9.Steiner CC. The use of cephalometrics as an aid to planning and assessing orthodontic treatment. Am J Orthod. 1960;46:721–735. doi: 10.1016/0002-9416(60)90145-7. [DOI] [Google Scholar]
- 10.Cabral MBA, Freitas AC, Araújo TM, Pena N, Brandão Filho RA. Effects of chin advancement surgery in hyoid bone and tongue positions and in the dimension of the oropharynx. Dental Press J Orthod. 2013;18(5):64–69. doi: 10.1590/S2176-94512013000500012. [DOI] [PubMed] [Google Scholar]
- 11.Saghaie S, Ghaffari R. Effect of image compression of direct digital lateral cephalograms on the identification of cephalometric points. Dent Res J (Isfahan) 2014;11(1):27–31. [PMC free article] [PubMed] [Google Scholar]
- 12.Tweed CH. Was the development of the diagnostic facial triangle as an accurate analysis based on fact or fancy? Am J Orthod. 1962;48:823–840. doi: 10.1016/0002-9416(62)90002-7. [DOI] [PubMed] [Google Scholar]
- 13.Gungor AY, Turkkahraman H, Yilmaz HH, Yariktas M. Cephalometric comparison of obstructive sleep apnea patients and healthy controls. Eur J Dent. 2013;7(11):48–54. [PMC free article] [PubMed] [Google Scholar]
- 14.Ryu HH. The usefulness of cephalometric measurement as a diagnostic tool for obstructive sleep apnea syndrome: a retrospective study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;119(1):20–23. doi: 10.1016/j.oooo.2014.07.537. [DOI] [PubMed] [Google Scholar]
- 15.Kaur S, Rai S, Kaur M. Comparison of reliability of lateral cephalogram and computed tomography for assessment of airway space. Niger J Clin Pract. 2014;17(5):629–636. doi: 10.4103/1119-3077.141431. [DOI] [PubMed] [Google Scholar]
- 16.Silva NN, Lacerda RLW, Silva AWC, Ramos TB. Assessment of upper airways measurements in patients with mandibular skeletal Class II malocclusion. Dental Press J Orthod. 2015;20(5):86–93. doi: 10.1590/2177-6709.20.5.086-093.oar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Indriksone I, Jakobsone G. The upper airway dimensions in different sagittal craniofacial patterns: a systematic review. Stomatologija. 2014;16(3):109–117. [PubMed] [Google Scholar]
- 18.Tsunori M, Mashita M, Kasai K. Relationship between facial types and tooth and bone characteristics of the mandible obtained by CT scanning. Angle Orthod. 1998;68(6):557–562. doi: 10.1043/0003-3219(1998)068<0557:RBFTAT>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 19.Silva VG, Pinheiro LA, Silveira PL, Duarte AS, Faria AC, Carvalho EG, Zancanella E, Crespo AN. Correlation between cephalometric data and severity of sleep apnea. Braz J Otorhinolaryngol. 2014;80(3):191–195. doi: 10.1016/j.bjorl.2013.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cho HW, Kim IK, Cho HY, Seo JH, Lee DH, Park SH. Retrospective study of changes in pharyngeal airway space and position of hyoid bone after mandibular setback surgery by cephalometric analysis. Maxillofac Plast Reconstr Surg. 2015;37(1):38. doi: 10.1186/s40902-015-0039-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Celikoglu M, Bayram M, Sekerci AE, Buyuk SK, Toy E. Comparison of pharyngeal airway volume among different vertical skeletal patterns: a cone-beam computed tomography study. Angle Orthod. 2014;84(5):782–787. doi: 10.2319/101013-748.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang T, Yang Z, Yang F, Zhang M, Zhao J, Chen J, Li Y. A three dimensional study of upper airway in adult skeletal Class II patients with different vertical growth patterns. Plos One. 2014;9(4):e95544. doi: 10.1371/journal.pone.0095544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dalmau E, Zamora N, Tarazona B, Gandia JL, Paredes V. A comparative study of the pharyngeal airway space, measured with cone beam computed tomography, between patients with different craniofacial morphologies. J Craniomaxillofac Surg. 2015;43(8):1438–1446. doi: 10.1016/j.jcms.2015.06.016. [DOI] [PubMed] [Google Scholar]
- 24.Aboudara C, Nielsen I, Huang JC, Maki K, Miller AJ, Hatcher D. Comparison of airway space with conventional lateral headfilms and 3-dimensional reconstruction from cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2009;135(4):468–479. doi: 10.1016/j.ajodo.2007.04.043. [DOI] [PubMed] [Google Scholar]
- 25.Lowe AA, Santamaria JD, Fleetham JA, Price C. Facial morphology and obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 1986;90(6):484–491. doi: 10.1016/0889-5406(86)90108-3. [DOI] [PubMed] [Google Scholar]
- 26.Ucar FI, Uysal T. Orofacial airway dimensions in subjects with Class I malocclusion and different growth patterns. Angle Orthodontist. 2011;81(3):460–468. doi: 10.2319/091910-545.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Armalaite J, Lopatiene K. Lateral teleradiography of the head as a diagnostic tool used to predict obstructive sleep apnea. Dentomaxillofac Radiol. 2016;45(1):20150085. doi: 10.1259/dmfr.20150085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Park JE, Gray S, Bennani H, Antoun JS, Farella M. Morphometric growth changes of the nasopharyngeal space in subjects with different vertical craniofacial features. Am J Orthod Dentofacial Orthop. 2016;150(3):451–458. doi: 10.1016/j.ajodo.2016.02.021. [DOI] [PubMed] [Google Scholar]
- 29.Tangugsorn V, Krogstad O, Espeland L, Lyberg T. Obstructive sleep apnoea: multiple comparisons of cephalometric variables of obese and non-obese patients. J Craniomaxillofac Surg. 2000;28(4):204–212. doi: 10.1054/jcms.2000.0147. [DOI] [PubMed] [Google Scholar]
- 30.Strauss RA, Burgoyne CC. Diagnostic imaging and sleep medicine. Dent Clin North Am. 2008;52(4):891–915. doi: 10.1016/j.cden.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 31.Battagel JM, L’Estrange PR, Nolan P, Harkness B. The role of lateral cephalometric radiography and fluoroscopy in assessing mandibular advancement in sleep-related disorders. Eur J Orthod. 1998;20(2):121–132. doi: 10.1093/ejo/20.2.121. [DOI] [PubMed] [Google Scholar]
- 32.Grippaudo C, Paolantonio EG, Antonini G, Saulle R, La Torre G, Deli R. Association between oral habits, mouth breathing and malocclusion. Acta Otorhinolaryngol Ital. 2016;36(5):386–394. doi: 10.14639/0392-100X-770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Valera FC, Travitzki LV, Mattar SE, et al. Muscular, functional and orthodontic changes in preschool children with enlarged adenoids and tonsils. J Pediatr Otorhinolaryngol. 2003;67:761–770. doi: 10.1016/S0165-5876(03)00095-8. [DOI] [PubMed] [Google Scholar]
- 34.Pereira SRA, Bakor SL, Weckx LLM. Adenotonsillectomy in facial growing patients: spontaneous dental effects. Braz J Otorhinolaryngol. 2011;77(5):600–604. doi: 10.1590/S1808-86942011000500011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Knösel M, Nüser C, Jung K, Helms HJ, Engelke W, Sandoval P. Interaction between deglutition, tongue posture, and malocclusion: a comparison of intraoral compartment formation in subjects with neutral occlusion or different types of malocclusion. Angle Orthod. 2016;86(5):697–705. doi: 10.2319/101615-699.1. [DOI] [PMC free article] [PubMed] [Google Scholar]


