Abstract
Background: There is little research comparing dermatologist and patient satisfaction with in-person, store-and-forward, and live interactive examinations.
Objective: To compare satisfaction with in-person examinations to store-and-forward and live interactive consultations having two types of video.
Methods: A controlled study was conducted where patients referred for dermatology consultations were examined in-person, by video, and by store-and-forward methods. Video changed between compressed and uncompressed on alternate clinics. Patients and dermatologists rated encounters after each examination. Dermatologists doing store-and-forward evaluations rated the quality of information provided. After experiencing all methods patients ranked their preferences. Dermatologists ranked their preferences at the end of the study.
Results: In-person examinations were preferred by both patients and dermatologists. Overall, satisfaction with teledermatology was still high. Patients were evenly divided in preferring store-and-forward workups or live interactive video. Dermatologists were also divided on store-and-forward and uncompressed video, but tended toward the latter. Compressed video was the least preferred method among dermatologists.
Limitations: Dermatology residents took store-and-forward photos and their quality was likely superior to those normally taken in practice.
Conclusions: Patients and dermatologists prefer in-person examinations and diverge on preferring store-and-forward and live interactive when video is not compressed. The amount of video compression that can be applied without noticeable image degradation is a question for future research.
Keywords: : teledermatology, telemedicine, satisfaction, preferences
Background
Live interactive teledermatology uses videoconferencing for synchronous examination, while store-and-forward involves sending photographs and histories to consulting dermatologists for later asynchronous evaluation.1–9 General telemedicine research reviews, including teledermatology1,2 and reviews specifically focused on teledermatology,3–9 tend to emphasize clinical decision-making, but some address satisfaction.4,5,7 Many satisfaction reports are anecdotal.4,7 Whited7 summarized the satisfaction findings of studies before 200610–20 almost all of which were cited in the other satisfaction reviews. Overall, patients were satisfied with teledermatology. Their primary misgivings for store-and-forward teledermatology were lack of interaction with a specialist, long waiting times for results, and sometimes absence of follow-up. Patients felt that real-time live interactive consultations were similar to in-person, but sensed discomfort at possibly being recorded and they missed the lack of “hands on” evaluation. There was less information about dermatologists' satisfaction other than that there were no reported image quality issues and that they had more confidence in face-to-face clinical examinations.
Studies subsequent to Whited's 2006 review indicate that patients' positive perceptions of teledermatology improved after using the service, although the number who felt they needed an in-person consult after exposure also increased.21 Other studies found that 93%,22 91%,23 90.5%,24 82.9%,25 58%,26 and 50%27 of patients were satisfied. Studies have shown that patients value teledermatology as quicker and less costly,24 believe it similar to face to face,23 have social and religious objections to it in some cultures,28 and high satisfaction rates over time.29 In one study, patients suspecting cancer or who were older preferred traditional examinations. Those under 56 were more likely to use teledermatology than those over, although the difference was not significant (p = 0.06).30 Studies also indicate satisfaction rates of 74% for dermatologists25 and 71% and 91% for primary care providers and imaging technicians.31 Still, many dermatologists prefer examinations in-person.11,12,30 Teledermatology satisfaction studies assessing a tryout of a pilot program or an ongoing existing service usually report higher levels of satisfaction,15,16,19,21–23,25–27,31 while those directly comparing face-to-face consultations with remote methods have more varied results.10–12,17,29,30
Materials and Methods
This study was a quasi-randomized control trial, in that clinics were scheduled whenever the number of dermatology referral patients volunteering for the study exceeded 10. Patients were compensated for time and travel. The study's 210 patients were evaluated thrice; in-person, by high definition live interactive video that was either compressed lower resolution or uncompressed higher resolution, or by store-and-forward methods with pictures and histories taken for later evaluation. Uncompressed video was 1,920 by 1,080 pixels transmitted at almost 1.5 gigabits per second, while compressed video used the H.264 compression standard and was 1,280 by 720 pixels transmitted at about 2 megabits per second (Mbps). Each videoconferencing system was installed in a clinic examination room and had pan, tilt, and zoom cameras that could be remotely controlled from a teledermatology consultation room outside the examination area. Uncompressed video was transmitted over dedicated lines, while compressed video used the clinic's existing network. Store-and-forward workups followed a protocol having a standardized form for history taking and required a minimum of three 10-megapixel JPEG images taken with a Canon G12 camera (3,648 × 2,736 pixel 24-bit color with a 1 to 5 compression ratio), each including a ruler and color wheel. The store-and-forward and video teledermatology implementations met or exceeded relevant guidelines published by the American Telemedicine Association.32 Not all guidelines applied, such as payment or providing store-and-forward results, since consultations were free and in-person examinations were used to manage patients.
Type of video alternated between clinics. The order that patients experienced the three methods rotated between clinics as did the 10 second- and third-year dermatology residents assigned each method. An attending board certified dermatologist, however, always saw patients in-person along with a resident assigned that method. Method order was recorded for analysis to control for sequence effects. Diagnostic concordance was measured, as well as satisfaction (reported in a separate publication33) and rotating residents controlled for variations in expertise and ensured each would examine approximately the same number of patients.
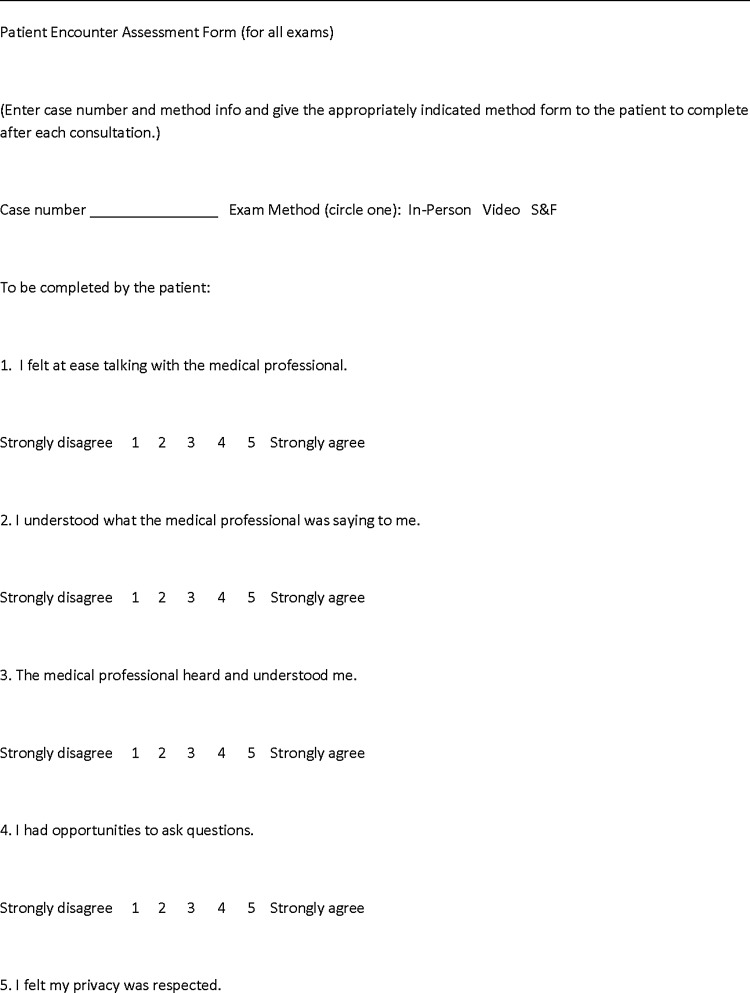
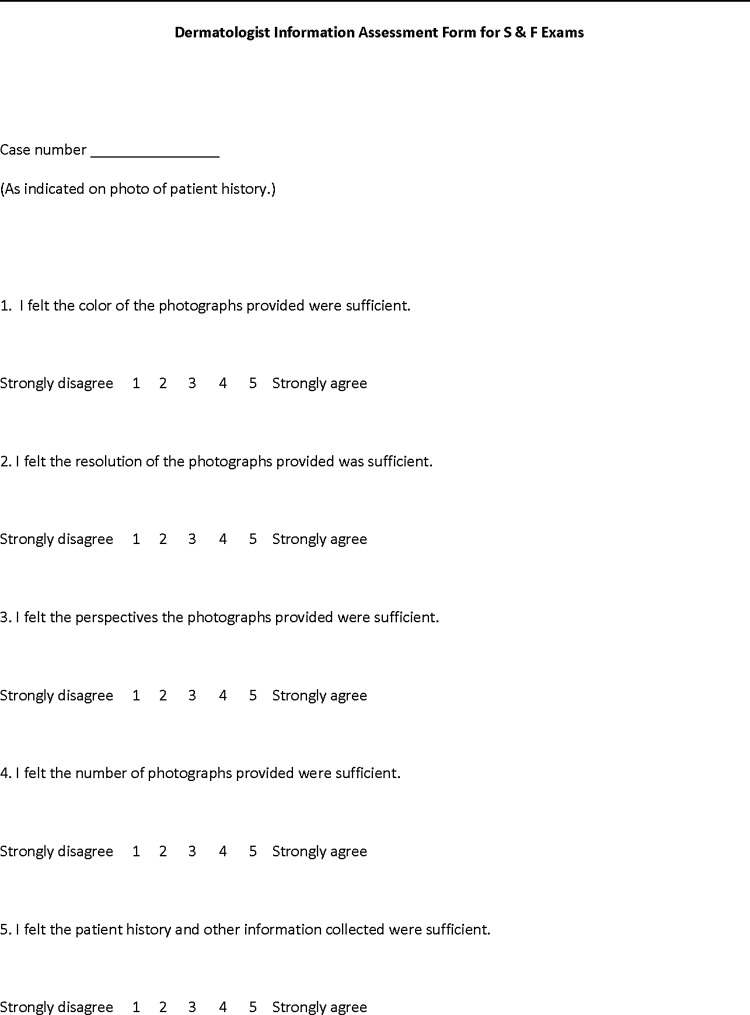
After each in-person and video examination, patients and dermatologists rated quality of the encounter using a 10 item 5-point Likert scale adapted from a study of video medical interpretation (Fig. 1).34 Questions were identical, with slight wording changes to reflect the perspective of the person completing the scale. For example, patients responded to the statement “I think my privacy was respected” and dermatologists responded to the statement “I think the patient's privacy was respected.” Patients also completed this scale after their store-and-forward workup, but dermatologists evaluating patients by this method completed a different 10 item 5-point Likert scale rating the quality of information provided (Fig. 2). Patients also rank ordered their preferences for each method after completing all examinations and provided reasons for their ranking. Since the patients only experienced one kind of video in their live interactive encounter, no distinction between compressed and uncompressed was made in their rankings. Dermatologists were interviewed at the conclusion of the study and were asked to rank methods that did account for the two types of video, since they had used both. The study was approved by the Institutional Review Boards of the Medical University of South Carolina and the National Institutes of Health.
Fig. 1.
Patient encounter assessment form.
Fig. 2.
Dermatologist information assessment form for store-and-forward consultations.
A mean score was calculated for scales having at least nine items completed. Cronbach's alpha was computed for each scale to assess internal reliability, and means and standard deviations of all scale scores were calculated. Since the scale means tended to be skewed and non-normal, the nonparametric Wilcoxon Signed Rank test for related groups using exact procedures was used to test for differences between group means. A two-tailed alpha of 0.05 was used for testing, and all tests were done with the SPSS statistical package.
Results
Patient and dermatologist encounter and information rating means, standard deviations, and significance levels are presented in Table 1. Median ratings and interquartile ranges are also shown. Mean and median ratings are relatively high for all methods, but there were still significant differences because the within-subject testing used in the design of this study tends to be more powerful for detecting differences than between-subjects testing. Patient satisfaction with live interactive video examinations (both higher resolution uncompressed and lower resolution compressed) was significantly lower than for store-and-forward workups and in-person examinations, while their ratings of store-and-forward and in-person examinations were not significantly different. In contrast, dermatologists' satisfaction ratings of all remote methods were significantly lower than in-person encounters. Their satisfaction ratings of compressed lower resolution live interactive examinations were significantly lower than those for store-and-forward workups which were rated significantly lower than examinations having uncompressed higher resolution video. Ratings also were analyzed by treatment order. Sequence affected ratings, but independent of the method. The first treatment experienced, regardless of method, tended to be rated lower.
Table 1.
Mean Satisfaction Scores Stratified by Diagnosis Method and by Patient or Dermatologist (Higher Numbers Indicate Greater Satisfaction; 5-Point Likert Scale 1–5)
| PATIENTa | DERMATOLOGISTb | |
|---|---|---|
| MEAN (SD), N | MEAN (SD), N | |
| MEDIAN (IQR) | MEDIAN (IQR) | |
| Compressed video | 4.66 (0.80), 112 | 4.53 (0.47), 112 |
| 5.00 (0.30) | 4.65 (0.80) | |
| Uncompressed video | 4.68 (0.73), 97 | 4.87 (0.24), 98 |
| 5.00 (0.35) | 5.00 (0.20) | |
| Store-and-forward | 4.74 (0.86), 209 | 4.48 (0.78), 212 |
| 5.00 (0.00) | 5.00 (0.90) | |
| In-person | 4.75 (0.81), 206 | 5.00 (0.03), 211 |
| 5.00 (0.00) | 5.00 (0.00) |
Significant differences (Wilcoxon signed rank test) in patient ratings between methods: Compressed and Uncompressed Video rated significantly lower than Store and Forward (Compressed p = 0.0008; Uncompressed p = 0.0006). Compressed and Uncompressed Video rated significantly lower than In-Person (Compressed p = 0.0001; Uncompressed p = 0.004). There were no significant differences between patient ratings of Store-and-Forward and In-Person.
Significant differences (Wilcoxon signed rank test) in dermatologist ratings between methods: All remote methods were rated significantly lower than In-Person (Compressed Video p = 0.000001, Uncompressed Video p = 0.00002, and Store-and-Forward p = 0.000001). Compressed Video and Store-and-Forward were rated significantly lower than Uncompressed Video (Compressed p = 0.000002; Store-and-Forward p < 0.000001). There were no significant differences between dermatologists' ratings of Uncompressed Video and Store-and-Forward.
Cronbach's alphas for rating forms used in patient store-and-forward workups, video, and in-person examinations are 0.99, 0.96, and 0.98. Alphas for dermatologist ratings of store-and-forward information, video, and in-person examinations are 0.96, 0.93, and 0.64. The alpha value for the in-person scale completed by dermatologists was lower because some items were excluded that lacked variance, since they had the same value for every respondent. Overall, the satisfaction scales were highly reliable.
Patient rankings of in-person examinations versus live interactive and store-and-forward methods are shown in Table 2. There is an overwhelming preference for in-person consultations, although about 14% preferred remote methods. Comments recorded on forms ranking remote methods better than in-person indicated that these patients felt the examinations were more private or might be more convenient. Patients rating in-person first were almost equally divided in making video or store-and-forward their second choice. Patients indicating store-and-forward as second choice often mentioned having someone physically present and being able to see what the resident was photographing. Patients choosing video second often mentioned having immediate diagnostic feedback and the ability to interact and ask questions. The mean patient rank order was significantly higher for in-person than remote methods, and remote method rankings were not significantly different from each other.
Table 2.
Number and Mean of Patient Rankings of In-Person and Teledermatology Methods
| DIAGNOSIS METHOD | |||
|---|---|---|---|
| RANK | IN-PERSON | VIDEO | STORE-AND-FORWARD |
| 1st | 173 | 16 | 12 |
| 2nd | 18 | 89 | 94 |
| 3rd | 10 | 96 | 95 |
| Mean (SD) | 1.19 (0.50) | 2.41a (0.60) | 2.40a (0.63) |
Significantly (p < 0.001) lower preference ranking than the In-Person method, Wilcoxon signed rank tests, exact method.
All dermatologists ranked in-person examinations as most preferable (Table 3), indicating the ability to palpate and touch and the flexibility in conducting examinations while more naturally interacting with patients as primary reasons. When asked about their preferences for video, each made a distinction between compressed and uncompressed and uniformly ranked live interactive lower resolution compressed video as significantly least preferable. Some indicated they could not see how reliable diagnoses could be made with this technology. Dermatologists tended to rank uncompressed video higher than store-and-forward methods, but not significantly. Those preferring live interactive higher resolution uncompressed video mentioned image quality, being able to interact with patients, and being able to control the camera to get different views or examine other areas as reasons. All dermatologists, even those preferring store-and-forward, indicated that uncompressed video quality was the best they had seen and some deemed it equal or better than in-person in cases where there is a need to zoom in close without violating a patient's personal space. Dermatologists preferring store-and-forward based their rankings on efficiency and image quality. They could make diagnoses faster with the photographs and histories supplied.
Table 3.
Number and Mean of Dermatologist Rankings of In-Person and Teledermatology Methods
| DIAGNOSTIC METHOD | ||||
|---|---|---|---|---|
| RANK | IN-PERSON | UNCOMPRESSED VIDEO | STORE-AND-FORWARD | COMPRESSED VIDEO |
| 1st | 11 | |||
| 2nd | 8 | 3 | ||
| 3rd | 3 | 8 | ||
| 4th | 11 | |||
| Mean (SD) | 1.0 (0)a | 2.27 (0.47) | 2.72 (0.47)a | 4.0 (0)a |
Significantly higher mean ranking for In-Person than any remote method (p = 0.001), significantly higher preference ranking for Store-and-forward versus Compressed Video (p = 0.001), no significant preference differences between Store-and-forward and Uncompressed Video (p = 0.227), Wilcoxon signed rank test, exact method.
Discussion
Patients were generally more satisfied with their store-and-forward workups than dermatologists were with the information provided, and patients rated this experience similarly to in-person. One reason may be that patients rated remote methods higher than they otherwise would because they knew they would be seen in-person. Another reason might be that patients felt the methods were similar because of the physical presence of a resident. Given that patients still rated live interactive video significantly lower, the latter reason is more likely. Dermatologists tended to be less satisfied with remote methods than patients. They were much more critical of store-and-forward than patients, especially in clinics using uncompressed video.
Dermatologists rated uncompressed video encounters most satisfactory of all remote methods. One reason why dermatologist rated uncompressed video higher was that they experienced video that was both compressed and uncompressed, while patients were only exposed to one type. The way video examinations were conducted also may have affected patient ratings. When video examinations were given in the study, patients were brought into an examination room, introduced to the dermatologist on screen, and were left alone. In contrast, a resident was present taking pictures and histories throughout the store-and-forward workup. During video examinations, patients could see the camera move, but were uncertain what the dermatologist was seeing. These concerns could be ameliorated in the future by having someone remain with the patient and activating a picture-in-picture capability so patients can see where the camera is pointing.
There were differences in the way satisfaction was assessed in this study versus previous ones. Only two of the previous teleconsultation studies directly compared patient preferences for in-person and live interactive examinations by exposing patients to both methods10,12 as in this study. In one study,10 patients were asked to respond to hypothetical comparison statements (e.g., teleconsultation can reduce time or teleconsultations are as good as going to clinics), instead of asking questions about general encounter attributes as was done in this study. The other study12 asked about encounter attributes, but patients had to indicate whether in-person or video consultations were better, worse, or about the same. In this study, patients and dermatologists agreed or disagreed with encounter quality statements in relation to each treatment just experienced and both had to rank order methods. It is in the rankings, not the ratings, that patient preferences for in-person examinations become apparent, their likings of store-and-forward and live interactive methods become more even, and their method choices conform more to those of dermatologists when dermatologists' distinctions between compressed and uncompressed live interactive methods are taken into account.
Conclusions
Patient and dermatologist ratings of in-person and teleconsultations in this study generally agree with previous research. Patients rated store-and-forward workups and in-person examinations about the same, but not video, while dermatologists rated in-person encounters significantly higher than remote methods. They were concerned about the limitations of compressed high definition video, even though the compression and data transmission rate were likely superior to the standard definition video used in most prior live interactive research. It is only in asking patients to make a forced choice between methods that this study clearly shows patient, as well as dermatologist, preferences for and satisfaction with in-person consultations, and greater alignment between dermatologists' and patients' choice of live interactive and store-and-forward methods. One limitation of this study was the use of residents, although the cases presented in the study were typical of other clinics and not particularly difficult for residents in their second and third years. Another limitation is the use of dermatology residents to take store-and-forward images and histories. This may have resulted in collecting higher quality information than if the data were obtained by nondermatologists. There were extreme differences in image quality in the two types of video used because a high degree of compression was applied in relation to uncompressed. A question for future research is how much compression can be applied before dermatologists notice differences in image quality.
Acknowledgments
The authors thank participating residents Vivian Beyer, Kathryn Dempsey, Brad Greenhaw, Francesa Lewis, Nick Papajohn, Adam Perry, Adam Sperduto, Roger Sullivan, Julie Swick, and Brent Taylor. This study was supported by NIH Research Contracts HHSN276201100424P, HHSN276201100588P, and the NIH Intramural Research Program. The study was approved by the Institutional Review Boards of the Medical University of South Carolina and the National Institutes of Health.
Disclosure Statement
No competing financial interests exist.
References
- 1.Hersch W, Wallace J, Patterson P, Shapiro S, Kraemer D, Eilers G, Chan B, Greenlick M, Helfand M. Telemedicine for the Medicare population. Evidence reports/technology assessments, No. 24. Rockville, MD: Agency for Healthcare Research and Quality, 2001: Report No. 01-E012 [Google Scholar]
- 2.Hersch W, Hickam D, Severance S, Dana T, Krages K, Helfand M. Telemedicine for the Medicare population: Update. Evidence reports/technology assessments, No. 131. Rockville, MD: Agency for Healthcare Research and Quality, 2006: Report No. 06-E007 [PMC free article] [PubMed] [Google Scholar]
- 3.Eminovic N, de Keizer N, Bindels P, Hasman A. Maturity of teledermatology evaluation research: A systematic review. Br J Dermatol 2007;156:412–419 [DOI] [PubMed] [Google Scholar]
- 4.Johnson M, Armstrong A. Technologies in dermatology: Teledermatology review. G Ital Dermatol Venereol 2011;146:143–153 [PubMed] [Google Scholar]
- 5.Romero G, Garrido J, Garcia-Arpa M. Telemedicine and teledermatology (I): Concepts and applications. Actas Dermosifiliogr 2008;99:506–522 [PubMed] [Google Scholar]
- 6.Romero G, Cortina P, Vera E. Telemedicine and teledermatology (II): Current state of research on dermatology teleconsultations. Actas Dermosifiliogr 2008;99:586–597 [PubMed] [Google Scholar]
- 7.Whited J. Teledermatology research review. Int J Derm 2006;45:220–229 [DOI] [PubMed] [Google Scholar]
- 8.Levin Y, Warshaw E. Teledermatology: A review of reliability and accuracy of diagnosis and management. Dermatol Clin 2009;27:163–176 [DOI] [PubMed] [Google Scholar]
- 9.Warshaw E, Hillman Y, Greer N, Hagel E, MacDonald R, Rutks I, Wilt T. Teledermatology for diagnosis and management of skin conditions: A systematic review. J Am Acad Dermatol 2011;64:759–772 [DOI] [PubMed] [Google Scholar]
- 10.Gilmour E, Campbell SM, Loane MA, Esmail A, Griffiths CEM, Roland MO, Parry EJ, Corbett RO, Eedy D, Gore HE, Mathews C, Steel K, Wootton R. Comparison of teleconsultations and face-to-face consultations: Preliminary results of a United Kingdom multicenter teledermatology study. Br J Dermatol 1998;139:81–87 [DOI] [PubMed] [Google Scholar]
- 11.Lowitt MH, Kessler II, Kaufman CL, Hooper FJ, Siegel E, Burnett JW. Teledermatology and in-person examinations: A comparison of patient and physician perceptions and diagnostic agreement. Arch Dermatol 1998;134:471–476 [DOI] [PubMed] [Google Scholar]
- 12.Nordal EJ, Moseng D, Kvammen B, Lochen ML. A comparative study of teleconsultations versus face-to-face consultations. J Telemed Telecare 2001;7:257–265 [DOI] [PubMed] [Google Scholar]
- 13.Weinstock MA, Nguyen FQ, Risica PM. Patient and provider satisfaction with teledermatology. J Am Acad Dermatol 2002;47:68–72 [DOI] [PubMed] [Google Scholar]
- 14.Pak HS, Welch M, Poropatich R. Web-based teledermatology consult system: Preliminary results from the first 100 cases. Stud Health Technol Inform 1999;64:179–184 [PubMed] [Google Scholar]
- 15.Kvedar JC, Menn ER, Baradagunta S, Smulders-Meyer O, Gonzalez E. Teledermatology in a capitated delivery system using distributed information architecture: Design and development. Telemed J 1999;5:357–366 [DOI] [PubMed] [Google Scholar]
- 16.van den Akker ThW, Reker CHM, Knol A, Post J, Wilbrink J, van der Veen JPW. Teledermatology as a tool for communication between general practitioners and dermatologists. J Telemed Telecare 2001;7:193–198 [DOI] [PubMed] [Google Scholar]
- 17.Williams TL, May CR, Esmail A, Griffiths CEM, Shaw NT, Fitzgerald D, Stewart E, Mould M, Morgan M, Pickup L, Kelly S. Patient satisfaction with teledermatology is related to perceived quality of life. Br J Dermatol 2001;145:911–917 [DOI] [PubMed] [Google Scholar]
- 18.Reid DS, Weaver LE, Sargeant JM, Allen MJ, Mason WF, Klotz PJ, Langille DB. Telemedicine in Nova Scotia: Report of a pilot study. Telemed J 1998;4:249–258 [DOI] [PubMed] [Google Scholar]
- 19.Loane MA, Bloomer SE, Corbett R, Eedy DJ, Gore HE, Mathews C, Steele K, Wootton R. Patient satisfaction with realtime teledermatology in Northern Ireland. J Telemed Telecare 1998;4:36–40 [DOI] [PubMed] [Google Scholar]
- 20.Jone DH, Crichton C, Macdonald A, Potts S, Sime D, Toms J, McKinlay J. Teledermatology in the highlands of Scotland. J Telemed Telecare 1996;2 Suppl 1:7–9 [DOI] [PubMed] [Google Scholar]
- 21.Eminovic E, Witkamp L, de Keizer NF, Wyatt JC. Patient perceptions about a novel form of patient-assisted teledermatology. Arch Dermatol 2006;142;647–651 [DOI] [PubMed] [Google Scholar]
- 22.Livingston J, Solomon J. An assessment of the cost effectiveness, safety of referral and patient satisfaction of a general practice teledermatology service. London J Prim Care 2015;7:31–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Azfar RS, Weinberg JL, Cavric G, Lee-Keltner IA, Bilker WB, Gefland JM, Kovarik C. HIV-positive patients in Botswana state that mobile teledermatology is an acceptable method for receiving dermatology care. J Telemed Telecare 2011;17:338–340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Al Quran HA, Khader YS, Ellauzi ZM, Shdaifat A. Effect of real-time teledermatology on diagnosis, treatment and clinical improvement. J Telemed Telecare 2015;21:93–99 [DOI] [PubMed] [Google Scholar]
- 25.Fruhauf J, Schwantzer G, Ambrose-Rudolph CM, Weger W, Ahlgrimm-Siess V, Salmhofer W, Hofmann-Wellenhof R. A pilot study on the acceptance of mobile teledermatology for the home monitoring of high-need patients with psoriasis. Australas J Dermatol 2012;55:41–46 [DOI] [PubMed] [Google Scholar]
- 26.Ebner C, Wurm EMT, Binder B, Kittler H, Lozzi GP, Massone C, Gabler G, Hofmann-Wellenhof R, Soyer HP. Mobile teledermatology: A feasibility study of 58 subjects. J Telemed Telecare 2008;14:2–7 [DOI] [PubMed] [Google Scholar]
- 27.Fruhauf J, Krock S, Quehenberger F, Kopera D, Fink-Puches R, Komericki P, Pucher S, Arzberger E, Hofmann-Wellenhof R. Mobile teledermatology helping patients control high-need acne: A randomized control trial. J Euro Acad Dermatol Venereo 2015;29:919–924 [DOI] [PubMed] [Google Scholar]
- 28.Kaliyadan F, Amin TT, Kuruvilla J, Al Bu Ali WH. Mobile teledermatology—patient satisfaction, diagnostic and management concordance, and factors affecting patient refusal to participate in Saudi Arabia. J Telemed Telecare 2013;19:315–319 [DOI] [PubMed] [Google Scholar]
- 29.Hsueh MT, Eastman K, McFarland LV, Raugi GJ, Reiber GE. Teledermatology patient satisfaction in the Pacific Northwest. Telemed J E Health 2011;18:377–381 [DOI] [PubMed] [Google Scholar]
- 30.Mofid M, Nesbitt T, Knuttel R. The other side of teledermatology: Patient preferences. J Telemed Telecare 2007;13:246–250 [DOI] [PubMed] [Google Scholar]
- 31.McFarland LV, Raugi G, Reiber GE. Primary care provider and imaging technician satisfaction with a teledermatology project in rural Veterans Health Administration clinics. Telemed J E Health 2012;19:815–825 [DOI] [PubMed] [Google Scholar]
- 32.Teledermatology Practice Guidelines Work Group. Practice guidelines for teledermatology. Washington, DC: American Telemedicine Association, 2016 [Google Scholar]
- 33.Marchell R, Locatis C, Burges G, Maisiak R, Liu W, Ackerman M. Comparing high definition live-interactive and store-and-forward consultations to in-person examinations. Telemed J E Health 2016. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Locatis C, Williamson D, Gould-Kabler C, Zone-Smith L, Detzler I, Roberson J, Maisiak R, and Ackerman M. Comparing in-person, video, and telephonic medical interpretation. J Gen Intern Med 2010;25:345–350 [DOI] [PMC free article] [PubMed] [Google Scholar]