Abstract
Background: The effectiveness of metered-dose inhalers (MDIs) in delivering medication to the lungs highly depends on its correct usage technique. Current guidelines state optimal technique for high lung deposition should include a slow inhalation (>5 seconds) at an inspiratory flow rate of 30 L/min and inhaler actuation at the start of inhalation. However, these recommendations were based on clinical studies using CFC (chlorofluorocarbon)-MDIs and in vitro studies of HFA (hydrofluoroalkane)-MDIs using idealized MDI techniques of uniform inhalation and actuation, disregarding the nonuniform techniques of actual patients.
Methods: To better understand the effects of time-varying MDI usage parameters on lung deposition of aerosol delivered by an HFA-MDI, we conducted an in vitro study modeled on real-life variable inspiratory flow and actuation techniques recorded from 15 subjects with asthma/chronic obstructive pulmonary disease (COPD). We developed a model representing the time-varying inspiratory flow waveforms and actuation timings based on 43 MDI techniques recorded from patients. Furthermore, we constructed an in vitro experimental setup using a mouth–throat cast, programmable MDI actuator, and breath simulator to evaluate lung deposition for the MDI techniques derived from our model.
Results: High inspiratory flow rates, 60–90 L/min, consistently resulted in high in vitro lung deposition (>40%) of aerosol (albuterol delivered from Ventolin HFA-MDI) compared to 30 L/min when MDI actuation occurred in the first half of inhalation. Also, positive coordination resulted in higher in vitro lung deposition compared with negative or zero coordination (actuating before or at the start of inspiration). Furthermore, variation in coordination affected lung deposition more significantly (23%) than flow rate or duration of inspiration (≤5%).
Conclusions: In an in vitro experimental model based on inhalation data from patients with asthma and COPD, we demonstrated that aerosol lung deposition emitted from Ventolin HFA-MDI is most optimal for MDI actuation in the first half of inspiration at high flow rates (60–90 L/min).
Keywords: : aerosol, asthma, COPD, inhaler technique, lung deposition, metered-dose inhaler
Introduction
Optimal delivery of inhaled medications to the lung is highly dependent on the accuracy of the technique using the inhaler device.(1–5) The metered-dose inhaler (MDI) is the most commonly used device that delivers a variety of rescue and maintenance medications for asthma and chronic obstructive pulmonary disease (COPD).(1,6) However, several studies have demonstrated that patients often commit various errors using such devices leading to wasted medication and thus, suboptimal control of their disease.(2–4)
Lung deposition of an aerosol delivered by an MDI may be dependent on all or a combination of the following five factors: (i) inspiratory flow rate, (ii) duration of inhalation, (iii) time of MDI actuation (time of actuating the MDI relative to the start of inspiration), (iv) duration of breath-hold after inhalation, and (v) fine fraction (the fraction of aerosol particles smaller than 5 μm in diameter).(5,7) The first four factors depend solely on the patient's technique of using MDIs, while the fifth factor, amount of fine fraction released from the MDI, depends on the design of the formulation and construction of the components of the MDI delivery device involved with the aerosol formation process, and not on the patient's MDI technique.(8) A high fine fraction results in higher deposition of medication in the lungs.(5) Thus, optimum lung deposition is achieved when the patient uses an MDI that releases a large fine fraction with the correct technique.(5)
The proper technique of using an MDI is based on the first four factors, inspiratory flow rate, duration of inhalation, time of MDI actuation and duration of breath-hold after inhalation, and is outlined by published GINA guidelines.(7) These guidelines are based on the results of numerous in vivo and in vitro studies previously conducted to quantify lung deposition of aerosol delivered by an MDI.(9–14)
For instance, in vivo studies by Newman et al. and Lawford and McKenzie during the 1980s using CFC (chlorofluorocarbon)-MDIs demonstrated that slow inspiration of duration greater than 4 seconds, and MDI actuation at the start of inhalation resulted in the most optimal lung deposition.(11–14) Furthermore, the effect of inspiratory flow rate was studied extensively for these CFC inhalers by Newman et al. in the 1990s, who demonstrated that higher lung deposition was achieved at low flow rates (∼28 L/min).(9,10) Based on those results, published guidelines for correct use of MDIs(7) currently recommend a low inspiratory flow rate of 30 L/min, long duration of inhalation of at least 5 seconds and MDI actuation at the start of inhalation, for optimal lung deposition.
However, since the early 2000s, the CFC MDIs have been discontinued due to their potential environmental hazards and were replaced with HFA (hydrofluoroalkane)-MDIs. The aerosol deposition characteristics for medication particles emitted from CFC MDIs are very different from that of HFA-MDIs due to the difference in fine fraction content of the two inhalers.(15–20) HFA-MDIs have a much higher fine fraction content than the CFC counterparts.(15–19)
The disparity in lung deposition is demonstrated in more recent in vivo studies by Usmani et al., Leach et al. and in vitro studies by Cheng et al. and Rahmatalla et al. using HFA-MDIs, which indicate that lung deposition increased with higher inspiratory flow rates, contrary to the lung deposition characteristics of CFC-MDIs.(15,17,18,20–22) In particular, Usmani et al. showed that for particles of diameter 1.5 μm, the lung deposition for fast inhalation was higher than that for slow inhalation.(18) However, as the particle size was increased from 1.5 to 6 μm, the lung deposition gradually decreased with increase in inspiratory flow rate.
Recent literature investigating the effects of duration of inhalation and MDI actuation timing for HFA-MDIs has been limited to in vitro studies using idealized techniques, having constant inspiratory flow rates, fixed duration of inhalation, and fixed actuation time(15,20–24); the idealized techniques do not represent actual patient's time-varying inhalation airflow profile and variable MDI actuation timings observed in a real-world setting. The correct HFA-MDI use technique in a real-world setting for both maximizing lung deposition and minimizing oropharyngeal deposition of medication is, therefore, unknown. The effect of the fourth factor, breath-hold after inhalation, has been well-documented through the above-mentioned in vivo studies.(9–14) Holding the breath for up to 10 seconds after inhalation minimizes any portion of the medication to be exhaled out of the lungs and is the recommended current guideline for MDI use.(5,7,25–27)
In this study, we developed a novel in vitro experimental setup to evaluate the lung deposition for time-varying realistic HFA-MDI techniques derived from techniques recorded from subjects with airway disease (asthma or COPD) using a placebo HFA-MDI in a clinic setting. We conducted the in vitro experiments to assess the effects of variation in the steps using the MDI (i–iii) listed in the beginning of this section: inspiratory flow rate, duration of inhalation, and time of MDI actuation on lung deposition of aerosol emitted from a albuterol HFA-MDI, Ventolin (GlaxoSmithKline, Research Triangle Park, NC).
Materials and Methods
This was a two-phase study. We first recorded the MDI technique of 15 subjects, 18–80 years old, with physician-diagnosed asthma or COPD using placebo HFA-MDI. The patients were seen in the Pulmonary Function Testing Laboratory at Ben Taub Hospital, Houston, Texas. We then conducted an in vitro lung deposition study, modeled on the recorded real-world HFA-MDI techniques. Both Baylor College of Medicine and Rice University institutional review boards approved the study and all subjects signed an informed consent form. The clinical study was registered at clinicaltrials.gov, with the registration number NCT02447575.
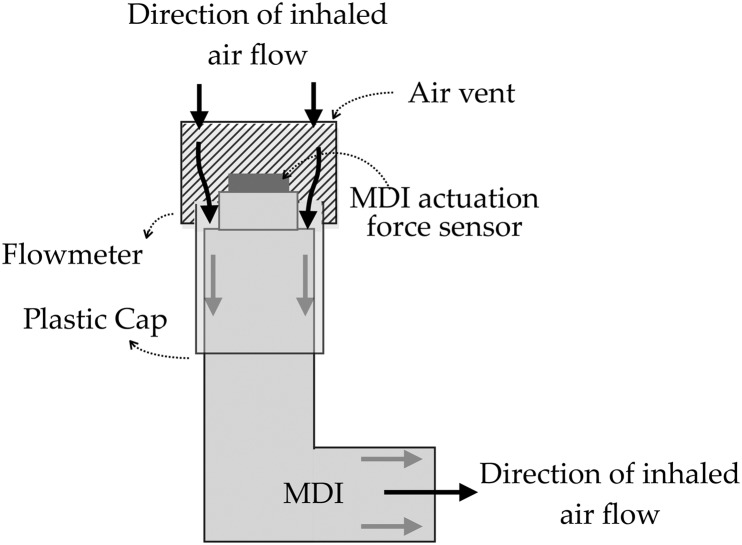
We used a calibrated turbine flow meter attached to a plastic cap with a force sensor, fitted tightly to a placebo HFA-MDI to measure the three factors, inspiratory flow rate as a function of time, duration of inhalation, and time of MDI actuation (Fig. 1). Out of the 15 subjects, 7 took more than one MDI puff with the attached cap, bringing the total number of techniques recorded to 43. The system added an average resistance of 30 Pa/(L·s), which did not interfere with inspiration through the MDI. However, the addition of the flow meter to the MDI may have added unfamiliarity to the subjects. Thus, before recording data, the subjects were instructed to actuate the MDI attached with the flow meter setup into the air (away from their mouth) to familiarize them with the system.
FIG. 1.
Schematic illustrates the MDI technique recording setup utilized in recording MDI techniques. The MDI is fitted with a plastic cap that connects to a calibrated flow meter. During inhalation through the MDI, the air flows in from the vent at the top of the flow meter and passes through the MDI as shown. The flow meter is also attached to a force sensor that synchronously detects and records the time of MDI actuation. The inhalation and actuation data are stored on the flow meter and are retrieved later on a PC. MDI, metered-dose inhaler; PC, personal computer.
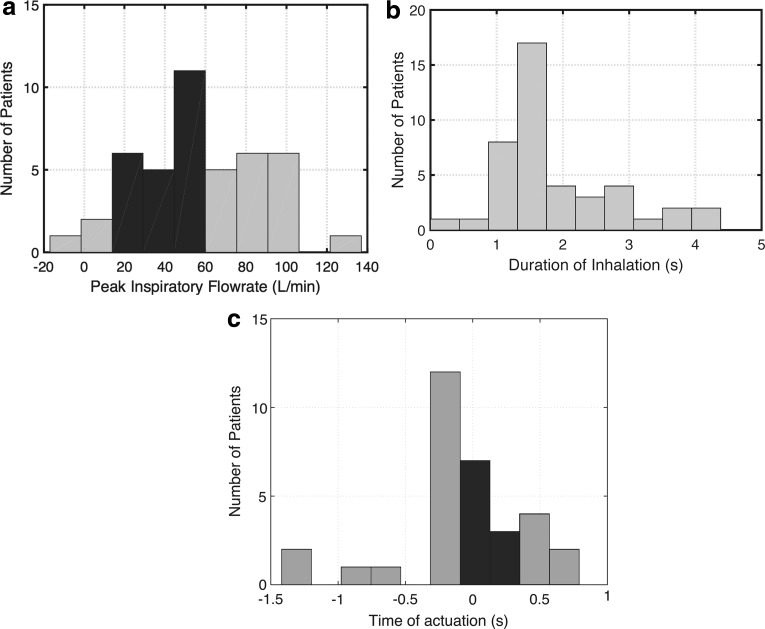
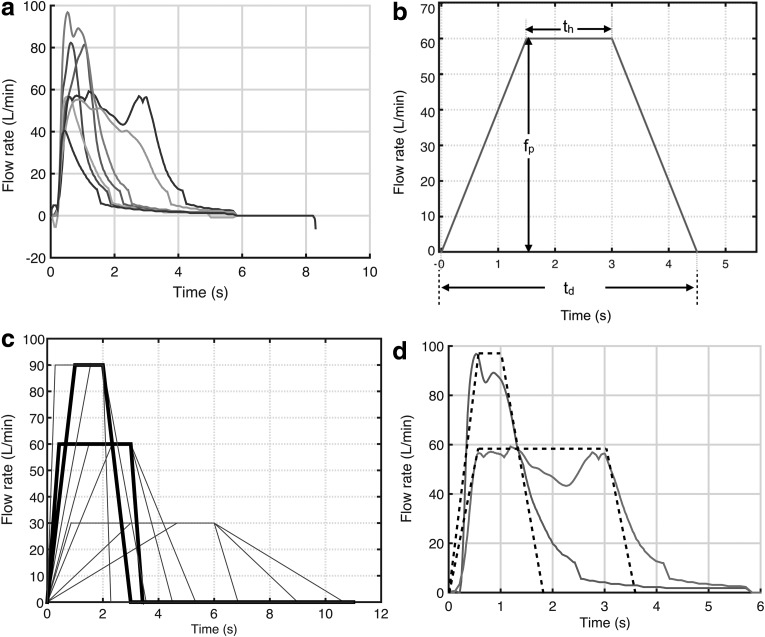
Figure 2 illustrates histograms of peak inspiratory flow rates (PIFRs), duration of inspiration, and time of actuation with respect to the start of inhalation, and Table 1 contains the summary statistics for recorded data. Data recorded illustrate significant variability in MDI use techniques among the test subjects and deviations from the current recommendations.(7) Figure 3a represents a subset of the recorded inhalation waveforms demonstrating variable PIFRs and durations of inhalation, thereby, confirming that actual MDI use is time-varying and not adequately approximated using idealized MDI techniques of constant inspiratory flow rates, duration, and MDI actuation. Figure 3b–d show the MDI technique model derived from the subject data.
FIG. 2.
Histogram of 43 MDI techniques collected from 15 subjects with asthma and COPD. Data collected consist of the inspiratory flow waveform and the time of MDI actuation. The distribution of three MDI technique steps of interest, (a) peak inspiratory flow rate, (b) duration of inhalation, and (c) time of actuation, is shown in (a–c), respectively. The black bars correspond to the correct technique as recommended by GINA guidelines, (a) peak flow rate between 30 and 60 L/min, (b) minimum inhalation of at least 5 seconds, and (c) time of actuation immediately after the start of inhalation (a positive value, 0–0.5 seconds). The gray bars correspond to the errors in MDI use, (a) peak inspiratory flow rate less than 30 L/min or greater than 60 L/min, (b) inhalation of less than 5 seconds, and (c) MDI actuation before the start of inhalation (a negative value) or late in the inhalation (a large positive value, greater than 0.5 seconds). COPD, chronic obstructive pulmonary disease.
Table 1.
Metered-Dose Inhaler Technique Data Recorded from 15 Subjects with Asthma and Chronic Obstructive Pulmonary Disease
| Peak inspiratory flow (L/min), fp | Duration of inhalation (seconds), td | Time of actuation (seconds), ta | |
|---|---|---|---|
| Mean (SD) | 57 (32) | 1.85 (0.93) | −0.05 (0.48) |
| Recommended guidelines | 30–60 | >5 | 0–0.5 |
| Percentage with Incorrect MDI uses | 60 | 100 | 79 |
MDI, metered-dose inhaler; SD, standard deviation.
FIG. 3.
The inspiratory flow waveforms recorded during MDI use by subjects with asthma and COPD, and the trapezoidal approximation to the waveforms are presented. (a) Shows a subset of the 43 waveforms collected from 15 subjects, representing the different inspiratory flow rates, duration of inhalation, and waveform shapes. (b) Shows the trapezoidal model for a particular 3 L flow waveform. Here, fp = 60 L/min (or 1 L/s), td = 4.5 seconds and th = 1.5 seconds. Thus the total inhalation volume is area of trapezoid = (1/2) fp (td + th) = 1/2 × 1 × (4.5 + 1.5) = 3 L. (c) Shows the different combinations of 3 L waveforms generated for fp = 30, 60, and 90 L/min and the ratio τ = 1.33, 3, and 8, corresponding to long, , and short duration of inhalation, respectively. As an example, a 90 L/min medium duration (τ = 3) and a 60 L/min short duration (τ = 1.33) are highlighted in bold. (d) Shows the trapezoidal approximation (dashed lines) for two of the waveforms recorded.
Data-driven MDI use technique model
We developed a data-driven model for MDI technique based on the usage data recorded from subjects with asthma and COPD. The model assumes a fixed inspiratory capacity (IC), that is, is the maximum volume of air that can be inspired from a resting respiratory level, of 3 L [IC ranges 2.5–3.5 L in adults(28)]. The main variables of MDI use examined in our model were (1) PIFR, (2) duration of inhalation, and (3) time of actuation, corresponding to the three out of five factors (i–iii), governing lung deposition. We defined a trapezoidal approximation to the patient inspiratory flow waveforms (Fig. 3a), accounting for the range of inhalation duration and PIFRs observed from our recorded waveforms shown in Figure 3b. The area under the flow-time curve represents the fixed volume (IC of 3 L); we derived the following model for inhalation during MDI use:
 |
where,
fp = PIFR
td = duration of inhalation = base 1 of trapezoid
th = hold time = duration that flow rate is held at fp = base 2 of trapezoid.
We also defined a third parameter, tr = rise-time, used in the later sections to define the time of MDI actuation. tr refers to the duration of time it takes for the flow rate to reach fp from 0 and vice versa (symmetrical waveform). Thus,
 |
The volume constraint Equation (1) is predicated on the assumption that the relationships between fp, td, and th are linearly dependent. We can further rewrite the equation as follows:
 |
where  is the ratio of the two durations corresponding to the bases of the trapezoid,
is the ratio of the two durations corresponding to the bases of the trapezoid,  .
.
We considered fp and  as two independent factors of MDI technique from our model; th is the dependent parameter. The ratio
as two independent factors of MDI technique from our model; th is the dependent parameter. The ratio  is a shape parameter, as it governs the profile of the trapezoid, ranging from 1 to ∞, from square (
is a shape parameter, as it governs the profile of the trapezoid, ranging from 1 to ∞, from square ( ) to triangular (
) to triangular ( ). Figure 3c demonstrates the range of flow waveforms generated based on the constraint Equation (3) by varying fp and
). Figure 3c demonstrates the range of flow waveforms generated based on the constraint Equation (3) by varying fp and  . A higher value of
. A higher value of  for a particular fp denoted longer inhalation duration (large td) with a small th, that is, a triangular trapezoid and vice versa.
for a particular fp denoted longer inhalation duration (large td) with a small th, that is, a triangular trapezoid and vice versa.
For example, a 3 L waveform associated with a given fp with high  required a long time to attain the peak flow, that is, a high rise-time, and resulted in a smaller average flow rate; and vice versa. Thus, the flow waveforms with a particular fp generated from the trapezoidal model had varying shapes (ranging from square to triangular) and varying average flow rates (ranging from low to high), due to the different tr and th governed by the value of
required a long time to attain the peak flow, that is, a high rise-time, and resulted in a smaller average flow rate; and vice versa. Thus, the flow waveforms with a particular fp generated from the trapezoidal model had varying shapes (ranging from square to triangular) and varying average flow rates (ranging from low to high), due to the different tr and th governed by the value of  . In our study, we varied the flow waveforms by choosing the factors fp in the range from 0 to 90 L/min, and the ratio τ = 1.33, 3, and 8, corresponding to a short, medium, and long duration of inhalation, respectively. Figure 3d illustrates how the flow waveforms generated from the trapezoidal waveforms fit inspiratory flow waveforms from actual patients.
. In our study, we varied the flow waveforms by choosing the factors fp in the range from 0 to 90 L/min, and the ratio τ = 1.33, 3, and 8, corresponding to a short, medium, and long duration of inhalation, respectively. Figure 3d illustrates how the flow waveforms generated from the trapezoidal waveforms fit inspiratory flow waveforms from actual patients.
The third independent parameter of MDI technique investigated was the time of MDI actuation, ta, which was the time of firing the MDI relative to the start of inhalation, also known as coordination. In this study,  conveyed that the inhaler was actuated at exactly the time instant when the patient started to inhale through the MDI; a negative ta conveyed that the inhaler was actuated before the start of inhalation; and a positive ta denoted that the inhaler was actuated after the start of inhalation. In this study, we investigated the effects of coordination on in vitro lung deposition by varying ta for −0.5, 0 seconds, +0.6 × tr,
conveyed that the inhaler was actuated at exactly the time instant when the patient started to inhale through the MDI; a negative ta conveyed that the inhaler was actuated before the start of inhalation; and a positive ta denoted that the inhaler was actuated after the start of inhalation. In this study, we investigated the effects of coordination on in vitro lung deposition by varying ta for −0.5, 0 seconds, +0.6 × tr,  , and
, and  . The three positive ta values are derived such that the MDI is actuated during the rising (
. The three positive ta values are derived such that the MDI is actuated during the rising ( ), constant (
), constant ( ), and falling edges (
), and falling edges ( ) of the trapezoid inspiratory waveform.
) of the trapezoid inspiratory waveform.
Note that the choice of values for fp,  , and ta were based on the data reported in previous literature on the range of PIFRs, duration of inhalation, and MDI actuation time,(24) and also on the 43 MDI usage techniques recorded from the 15 patients in our study, as shown in Table 1.
, and ta were based on the data reported in previous literature on the range of PIFRs, duration of inhalation, and MDI actuation time,(24) and also on the 43 MDI usage techniques recorded from the 15 patients in our study, as shown in Table 1.
In vitro experimental setup
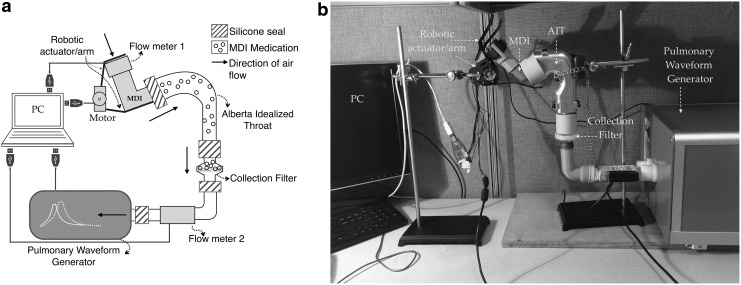
We constructed an in vitro lung deposition experimental setup to generate the time-varying MDI techniques based on fp,
 , and ta, and analyzed corresponding lung deposition (see Fig. 4a for a schematic diagram, Fig. 4b for photograph of the setup). A programmable robotic arm was built using Robotis' Dynamixel RX-64 servomotor (Trossen Robotics, Downers Grove, IL) to actuate the MDI at the predefined values of ta. We used albuterol sulfate Ventolin HFA-MDIs (GlaxoSmithKline) in our experiments, labeled to dispense 108 mcg of albuterol sulfate at every actuation.
, and ta, and analyzed corresponding lung deposition (see Fig. 4a for a schematic diagram, Fig. 4b for photograph of the setup). A programmable robotic arm was built using Robotis' Dynamixel RX-64 servomotor (Trossen Robotics, Downers Grove, IL) to actuate the MDI at the predefined values of ta. We used albuterol sulfate Ventolin HFA-MDIs (GlaxoSmithKline) in our experiments, labeled to dispense 108 mcg of albuterol sulfate at every actuation.
FIG. 4.
(a) Schematic to illustrate the in vitro experimental setup used in our work. A PC (personal computer) controls the motorized robotic MDI actuator, two flow meters, and the PWG. All the parts of the system are sealed using silicone connectors to minimize air leaks. The MDI is connected to the AIT, which represents the mouth–throat part of the body. The AIT is then connected to the collection filter, which acts as the lungs of the body. The different combinations of MDI techniques, inspiratory flow rates, duration of inhalations, and time of actuation are produced using the combination of the programmable PWG and motorized actuator. (b) Is a photograph of the actual setup used in the in vitro lung deposition experiments. AIT, Alberta Idealized Throat; PWG, pulmonary waveform generator.
The inhaler was fitted to the same turbine flow meter used to record the maneuvers by the study subjects (Fig. 1), and connected with the anatomically correct mouth–throat cast. The mouth–throat cast used was an adult Alberta Idealized Throat or AIT (manufactured by Copley Scientific Ltd., United Kingdom), the accuracy of which had been validated by previous studies.(15,21,22,24,29)
The AIT was connected to the collection filter, Respirgard 303 (manufactured by Vital Signs), representing in vitro lungs. The filter was connected through another flow meter, Thor SpiroTube (manufactured by THOR Research and Development, Hungary), to the ATS and ISO certified pulmonary waveform generator or PWG (manufactured by Piston Ltd., Hungary). The setup was sealed using silicone connectors to ensure the maximum leakage was below 0.15 L (5%). A PC (personal computer) controlled the robotic arm, the two flow meters, and the PWG to generate MDI use-cases, monitor the procedure, and record observations. We performed MDI techniques based on fp,
 , and ta, derived from our model [Eq. (3)], using the combination of PWG and a robotic arm in the experimental setup.
, and ta, derived from our model [Eq. (3)], using the combination of PWG and a robotic arm in the experimental setup.
Lung deposition testing was performed using AIT according to the guidelines provided by previous in vitro studies.(15,21,22,29) At the beginning of each experiment, we cleaned, dried, and coated the inner surfaces of the AIT with silicone release spray, Molykote 316 (manufactured by Dow Corning, Auburn, MI), to reduce aerosol particle bounce. For each MDI use-case, we repeated the experiment thrice (n = 3), including multiple MDI actuations and rinsing of each component to recover the deposited drug. The first 2 repetitions were conducted with 10 MDI actuations and the third with 15 actuations to reduce the dose-to-dose variability, as previous studies have shown that the amount of medication delivered by MDIs for each actuation is imprecise.(30) Furthermore, we employed a waiting period of 1 minute between actuations and vigorously shook the MDI 20 times before each actuation, as guided in previous studies.(31)
The total drug dispensed by the MDI comprises the amount of drug deposited in the MDI actuator mouthpiece, AIT, and collection filter. Thus the mass of the total drug delivered can be represented as follows:
 |
where,
mt is the mass of total delivered drug
 is the mass of drug deposited in the MDI actuator mouthpiece
is the mass of drug deposited in the MDI actuator mouthpiece
 is the mass of drug deposited in the AIT or the mouth–throat deposition
is the mass of drug deposited in the AIT or the mouth–throat deposition
 is the mass of the drug deposited in the filter or in vitro lung deposition.
is the mass of the drug deposited in the filter or in vitro lung deposition.
In this study, the mass of the drug deposited in the filter,  , is an approximation of the total lung deposition and fraction of medication exhaled into the air.
, is an approximation of the total lung deposition and fraction of medication exhaled into the air.
The percentage in vitro lung deposition is computed as follows:
 |
 |
where,
 |
 is the percentage in vitro lung deposition of Albuterol
is the percentage in vitro lung deposition of Albuterol
 is the percentage drug deposition in the MDI actuator mouthpiece
is the percentage drug deposition in the MDI actuator mouthpiece
 is the percentage drug deposition in the AIT
is the percentage drug deposition in the AIT
The mouthpiece, AIT, and filter were repeatedly rinsed with deionized water as outlined in previous studies(30) and the recovered solutions were analyzed using a UV spectrophotometer, Thermo Scientific™ GENESYS™ 10S UV-Vis Spectrophotometer, at 224 nm.
For our experiments, first fp was varied from 0 to 90 L/min in steps of 30, and td was varied as a short, medium, and long inhalation for the ratio  of 1.33, 3, and 8, respectively. ta was kept constant at
of 1.33, 3, and 8, respectively. ta was kept constant at  for all values of fp and
for all values of fp and  , that is, actuation in the rising edge of the waveform or the first half of the inspiration. Next, the 60 L/min long inhalation waveform (
, that is, actuation in the rising edge of the waveform or the first half of the inspiration. Next, the 60 L/min long inhalation waveform ( ) was selected and ta was varied for small intervals from 0.5 seconds before the start of inspiration (−0.5 seconds) to (
) was selected and ta was varied for small intervals from 0.5 seconds before the start of inspiration (−0.5 seconds) to ( ) (falling edge of the waveform at the end of inspiration), to study the effect of coordination on the in vitro lung deposition. The in vitro lung deposition data obtained were analyzed using one-way ANOVA and Tukey HSD for multiple comparisons at different fp,
) (falling edge of the waveform at the end of inspiration), to study the effect of coordination on the in vitro lung deposition. The in vitro lung deposition data obtained were analyzed using one-way ANOVA and Tukey HSD for multiple comparisons at different fp,  , and ta values, where a p-value <0.05 was considered to be statistically significant.
, and ta values, where a p-value <0.05 was considered to be statistically significant.
Results
The results are divided into two categories based on the inhalation variables fp,  , and coordination variable ta. The mean
, and coordination variable ta. The mean  for fp = 0 L/min was found to be 5.7% and considered the baseline condition, and was, as expected, associated with the lowest drug deposition. The baseline is of similar magnitude to previously reported results, for example, 7% deposition using CFC inhalers.(32,33)
for fp = 0 L/min was found to be 5.7% and considered the baseline condition, and was, as expected, associated with the lowest drug deposition. The baseline is of similar magnitude to previously reported results, for example, 7% deposition using CFC inhalers.(32,33)
The first category demonstrates the effect of inhalation waveform parameters, fp and  , on lung deposition. Table 2 lists the
, on lung deposition. Table 2 lists the  ,
,  , and
, and  for the MDI use-cases with different values of fp and
for the MDI use-cases with different values of fp and  (and corresponding td), at
(and corresponding td), at  . There were three repetitions (n = 3) of all MDI use-cases except for fp = 90 L/min and
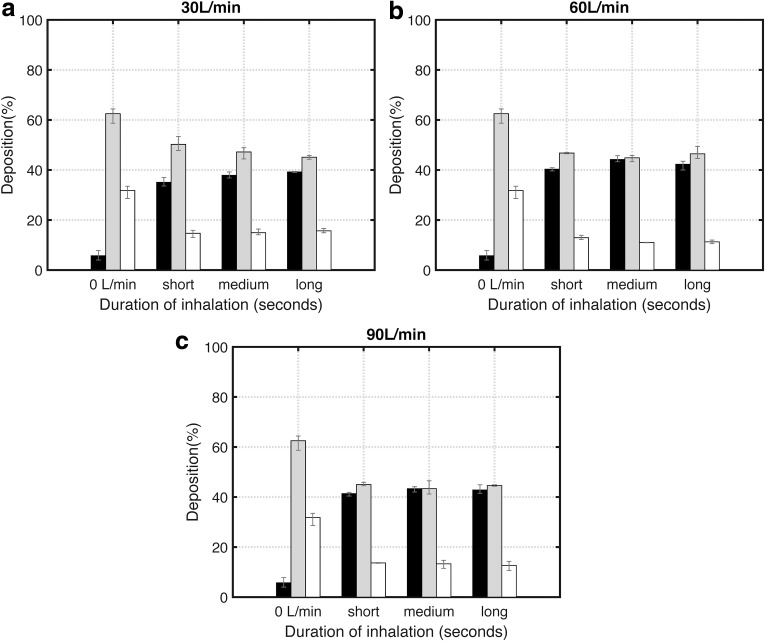
. There were three repetitions (n = 3) of all MDI use-cases except for fp = 90 L/min and  (n = 4). The results are further visualized graphically in Figure 5a–c, corresponding to the inspiratory flow rates 30, 60, and 90 L/min, respectively.
(n = 4). The results are further visualized graphically in Figure 5a–c, corresponding to the inspiratory flow rates 30, 60, and 90 L/min, respectively.
Table 2.
Percentage Lung Deposition for In Vitro Experiments for Variation in Inspiratory Parameters, Peak Inspiratory Flow Rate (fp) and Shape (τ), Where the Time of Actuation Is in the First Half of Inspiration, Set at ta = 0.6tr
| No. | Trial No. | PIFR (L/min), fp | Shape parameter, τ | Time duration (seconds), td | Time of actuation (seconds), ta | Percent MP deposition, pMP | Percent AIT deposition, pAIT | Percent in vitro lung deposition, pivL | Mean percent in vitro lung deposition, mean pivL |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 1 | 0 | 0 | 0 | 0 | 32.5 | 63.5 | 4 | 5.7 |
| 2 | 32.6 | 63.4 | 4 | ||||||
| 3 | 33.5 | 58.7 | 7.8 | ||||||
| 4a | 28.6 | 64.4 | 7 | ||||||
| 2 | 1 | 30 | 1.33 | 6.85 | 0.51 | 15.2 | 47.8 | 37 | 35.1 |
| 2 | 15.9 | 49.5 | 34.6 | ||||||
| 3 | 13 | 53.4 | 33.6 | ||||||
| 3 | 1 | 30 | 3 | 9 | 1.8 | 14.3 | 48.9 | 36.8 | 37.9 |
| 2 | 14.1 | 48.3 | 37.6 | ||||||
| 3 | 16.4 | 44.4 | 39.2 | ||||||
| 4 | 1 | 30 | 8 | 10.67 | 2.8 | 15.5 | 45.2 | 39.3 | 39.2 |
| 2 | 14.9 | 45.8 | 39.4 | ||||||
| 3 | 16.6 | 44.3 | 39 | ||||||
| 5 | 1 | 60 | 1.33 | 3.42 | 0.255 | 13.9 | 46.5 | 39.6 | 40.3 |
| 2 | 12.7 | 46.8 | 40.5 | ||||||
| 3 | 12.2 | 47 | 40.9 | ||||||
| 6 | 1 | 60 | 3 | 4.5 | 0.9 | 11.1 | 43.3 | 45.7 | 44.2 |
| 2 | 10.9 | 45.5 | 43.6 | ||||||
| 3 | 11 | 45.8 | 43.3 | ||||||
| 7 | 1 | 60 | 8 | 5.33 | 1.4 | 10.6 | 49.4 | 40 | 42.3 |
| 2 | 12 | 44.6 | 43.5 | ||||||
| 3 | 11.2 | 45.4 | 43.4 | ||||||
| 8 | 1 | 90 | 1.33 | 2.28 | 0.17 | 13.7 | 45.9 | 40.4 | 41.4 |
| 2 | 13.8 | 44.5 | 41.8 | ||||||
| 3 | 13.5 | 44.5 | 41.9 | ||||||
| 9 | 1 | 90 | 3 | 3 | 0.6 | 11.5 | 46.5 | 42 | 43.3 |
| 2 | 14.7 | 41.2 | 44.1 | ||||||
| 3 | 13.7 | 42.4 | 43.9 | ||||||
| 10 | 1 | 90 | 8 | 3.56 | 0.93 | 10.6 | 44.5 | 44.9 | 42.8 |
| 2 | 14.3 | 44.3 | 41.5 | ||||||
| 3 | 13 | 44.9 | 42 | ||||||
| 4a | 12.7 | 44.6 | 42.8 |
The trial numbers 1–2 correspond to experiments conducted with 10 doses and the number 3 corresponds to experiments repeated with 15 doses. The first row corresponds to baseline case of no flow rate.
Note that the fourth repetition for some of the experiments (with 10 doses) was carried out as we noticed a larger variation for that data point.
AIT, Alberta Idealized Throat; PIFR, peak inspiratory flow rate.
FIG. 5.
The percentage deposition in the in vitro lung (black bar), AIT (gray bar), and MDI mouthpiece (white bar) for the in vitro experiments are presented. The graph shows the results from experiments performed for inhalation (flow, duration)-dependent MDI techniques with MDI actuation fixed at the first half of inspiration. Each group of bars represents one MDI technique; the error bars show the range due to three repetitions of each experiment. The baseline result is shown in the beginning marked 0 L/min. The error margins for in vitro lung deposition ranged from ±0.2% to ±2.3%, average ±1.3%. Three flow rates, 30, 60, and 90 L/min, were used for each of the experiments. (a–c) Show the variation in lung deposition with shape ratio, τ (corresponding to the duration of inhalation), for the three different flow rates 30, 60, and 90 L/min, respectively. The short, medium, and long labels on the x-axis refer to τ equal to 1.33, 3, and 8, respectively. The inhalers were actuated at the beginning of the inhalation, ta = 0.6tr. We found that the mean in vitro lung deposition (black bar) is higher for 60–90 L/min than 30 L/min (p < 0.001), always greater than 40%. The maximum mean in vitro lung deposition was found to be 44.2% for the case of inspiration with PIFR 60 L/min and duration of 4.5 seconds. PIFR, peak inspiratory flow rate.
The results show that mean  was lowest for fp = 30 L/min, always below 40% for all values of
was lowest for fp = 30 L/min, always below 40% for all values of  . Furthermore, the mean
. Furthermore, the mean  for both fp = 60 L/min and 90 L/min was higher than 40% for all values of
for both fp = 60 L/min and 90 L/min was higher than 40% for all values of  (correspondingly, all values of td) and therefore, significantly higher than the mean
(correspondingly, all values of td) and therefore, significantly higher than the mean  for fp = 30 L/min (p < 0.001). The increase in mean
for fp = 30 L/min (p < 0.001). The increase in mean  for fp = 30 L/min to corresponding waveforms of fp = 60 − 90 L/min was found to be 5% (p < 0.001). There was no significant difference in
for fp = 30 L/min to corresponding waveforms of fp = 60 − 90 L/min was found to be 5% (p < 0.001). There was no significant difference in  for
for  and 90 L/min (p > 0.05). Furthermore, Figure 5a shows a steady increase in
and 90 L/min (p > 0.05). Furthermore, Figure 5a shows a steady increase in  for fp = 30 L/min with increasing
for fp = 30 L/min with increasing  (increase in the duration of inhalation). There was an increase of 3% in mean
(increase in the duration of inhalation). There was an increase of 3% in mean  for all flow rates due to an increase in
for all flow rates due to an increase in  from 1.33 to 3 and 8 (p < 0.05, n = 3). There was no significant effect on
from 1.33 to 3 and 8 (p < 0.05, n = 3). There was no significant effect on  for a change in
for a change in  from 3 to 8 (p > 0.05).
from 3 to 8 (p > 0.05).
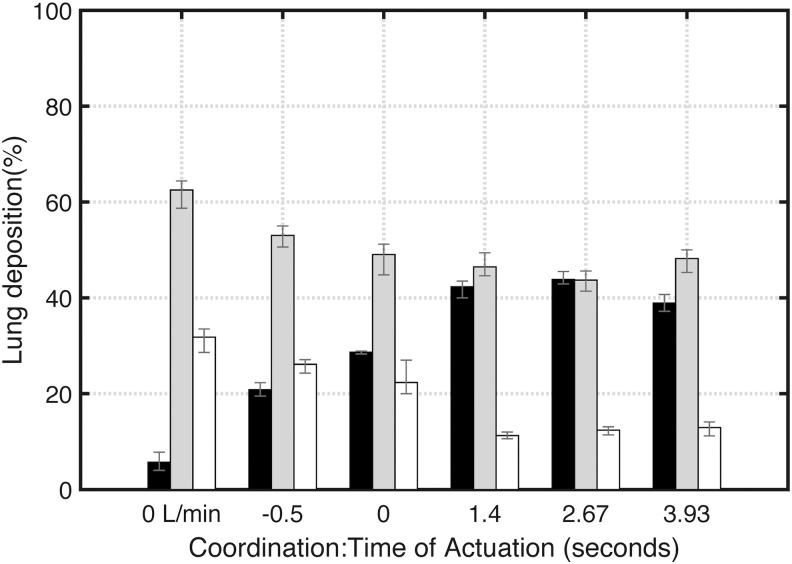
The next category of results demonstrates the effect of coordination, that is, ta, on lung deposition. As we obtained higher  for
for  and 90 L/min and
and 90 L/min and  and 8, we selected the inspiration waveform of fp = 60 L/min and
and 8, we selected the inspiration waveform of fp = 60 L/min and  (long duration of 5.33 seconds) to determine
(long duration of 5.33 seconds) to determine  for different values of ta. Table 3 illustrates the
for different values of ta. Table 3 illustrates the  ,
,  , and
, and  data collected for
data collected for  , 0 seconds, 0.6tr, 0.5td, and
, 0 seconds, 0.6tr, 0.5td, and  and the results are graphically shown in Figure 5c. There were three repetitions (n = 3) of all MDI use-cases. We found that the
and the results are graphically shown in Figure 5c. There were three repetitions (n = 3) of all MDI use-cases. We found that the  steadily increased with an increase in ta for
steadily increased with an increase in ta for  .
.
Table 3.
Percentage Lung Deposition for In Vitro Experiments with Actuation Time ta, Ranging from 0.5 Second Before Start of Inhalation (−0.5 seconds) to Falling Edge of the Waveform at the End of Inspiration (td − 0.6tr), for the Inspiratory Waveform with fp = 60 L/min and τ = 8 (or td = 5.33)
| No. | Trial No. | Time of actuation (seconds), ta | Percent MP deposition, pMP | Percent AIT deposition, pAIT | Percent in vitro lung deposition, pivL | Mean percent in vitro lung deposition, mean pivL |
|---|---|---|---|---|---|---|
| 1 | 1 | Baseline fp = 0 L/min, ta = 0 | 32.5 | 63.5 | 4 | 5.7 |
| 2 | 32.6 | 63.4 | 4 | |||
| 3 | 33.5 | 58.7 | 7.8 | |||
| 4 | 28.6 | 64.4 | 7 | |||
| 2 | 1 | −0.5 | 27.1 | 50.6 | 22.3 | 20.8 |
| 2 | 24.3 | 55 | 20.7 | |||
| 3 | 27 | 53.5 | 19.5 | |||
| 3 | 1 | 0 | 20 | 51.2 | 28.8 | 28.7 |
| 2 | 20 | 51.1 | 28.9 | |||
| 3 | 27 | 44.8 | 28.3 | |||
| 4 | 1 | 1.4 (0.6tr) | 10.6 | 49.4 | 40 | 42.3 |
| 2 | 12 | 44.6 | 43.5 | |||
| 3 | 11.2 | 45.4 | 43.4 | |||
| 5 | 1 | 2.67 (0.5td) | 12.7 | 44.1 | 43.1 | 43.8 |
| 2 | 11.4 | 45.6 | 42.9 | |||
| 3 | 13.1 | 41.4 | 45.5 | |||
| 6 | 1 | 3.93 (td − 0.6tr) | 13.5 | 49.3 | 37.2 | 38.9 |
| 2 | 11.2 | 50 | 38.8 | |||
| 3 | 14.1 | 45.3 | 40.7 |
The trial numbers 1–2 correspond to experiments conducted with 10 doses and the number 3 corresponds to experiments repeated with 15 doses.
Furthermore, the lung deposition value reached a plateau at the highest point in inspiratory flow rate, at  ; the increase in
; the increase in  from
from  to
to  was of 23% (p < 0.001). The
was of 23% (p < 0.001). The  for
for  was significantly less than
was significantly less than  for all other ta (p < 0.001); similarly, the
for all other ta (p < 0.001); similarly, the  for
for  was significantly less than
was significantly less than  for all positive ta (p < 0.001). There was no significant difference in
for all positive ta (p < 0.001). There was no significant difference in  for
for  and 0.5td. Furthermore,
and 0.5td. Furthermore,  for
for  was significantly smaller than
was significantly smaller than  for
for  and 0.5td (p < 0.01).
and 0.5td (p < 0.01).
Discussion
Our study results demonstrate that for a positive coordination in the first half of inspiration, a higher fp = 60 − 90 L/min yielded better lung deposition compared to lower fp = 30 L/min, independent of the duration of inspiration; the increase in mean  was found to be 5%. Thus, the positive effect of high PIFR on lung deposition of Albuterol from Ventolin HFA MDI observed in our in vitro experimentation is not only of opposite trend but also less critical (an increase of 5% only) from what has been reported in the past literature.(9–14)
was found to be 5%. Thus, the positive effect of high PIFR on lung deposition of Albuterol from Ventolin HFA MDI observed in our in vitro experimentation is not only of opposite trend but also less critical (an increase of 5% only) from what has been reported in the past literature.(9–14)
As mentioned earlier, a number of recent publications, particularly the work of Usmani et al., have suggested that the particle of smaller sizes (1.5 μm) delivered from various HFA inhalers have better lung deposition (4.6% increase) at high mean flow rates (67.1 ± 16.7 L/min) compared to low mean flow rates (30.8 ± 4.7 L/min).(15,17–20,34) However, for particles of 3 μm, the lung deposition at high mean flow rates decreased slightly (1.4% decrease) compared to low flow rates, decreasing more dramatically for larger particles of size 6 μm (24.7% decrease).(18)
Furthermore, Cheng et al. had demonstrated that, for the in vitro study using albuterol sulfate HFA MDI (Proventil) with a mass median aerodynamic diameter (MMAD) of 2.21 μm, the mouth–throat deposition decreased significantly on increasing flow rate from 30 to 90 L/min, consequently increasing the in vitro lung deposition.(20) A high oropharyngeal deposition at low flow rates was attributed to the higher speed of aerosol droplets compared to the inspiratory flow rate. Therefore, at higher inspiratory flow rates, a possibly more efficient momentum transfer occurred between the aerosol droplets and air flow, such that a larger fraction of aerosol droplets followed the air stream into the lungs, resulting in a lower mouth–throat deposition.
Furthermore, the authors also suggested that at higher flow rates, the evaporation of aerosol emitted from the MDI is more efficient in generating smaller droplets resulting in lower oropharyngeal deposition. In addition, the authors also stated that the impact force of the aerosol sprays from HFA MDIs are much smaller than CFC MDIs due to the smaller orifice diameters of HFA MDIs, which changes the plume characteristics (softer due to smaller aerosol velocities) and reduces oropharyngeal deposition.
Furthermore, Rahmatalla et al. also demonstrated that with Beclomethasone HFA MDI (QVAR), which has a high fine fraction close to 1 μm, the increased in vitro lung deposition at high flow rates was due to alternate mechanisms of aerosol deposition in addition to impaction; such as sedimentation and diffusion.(15) Hoye et al. also demonstrated that the MMAD of Ventolin Albuterol HFA MDIs was 2.07 μm.(19) Therefore, we conclude from our observed experimental results and past literature(15,17–20,34) that due to a combination of mechanisms governing the deposition of albuterol aerosol delivered by Ventolin HFA MDIs, having a small particle size (MMAD 2.07 μm) compared to CFC counterparts, the in vitro lung deposition is slightly higher for PIFRs in the range 60–90 L/min than low PIFRs.
A further extension of our work would be to measure particle size distribution using a cascade impactor for our dynamic trapezoidal inspiration waveforms to confirm higher fine fraction of aerosol delivered by HFA Albuterol MDI (Ventolin) and the corresponding dependency of PIFR on lung deposition obtained in our experiments.
Our results on the study of the effects of coordination on in vitro lung deposition demonstrated that the highest lung deposition occurred with positive coordination, especially actuation in the first half of the inspiratory waveform. The increase in  from
from  to
to  was 23%, suggesting that coordination was the most critical parameter in determining
was 23%, suggesting that coordination was the most critical parameter in determining  . Furthermore, compared to flow and duration parameters, a negative coordination caused the maximum loss in
. Furthermore, compared to flow and duration parameters, a negative coordination caused the maximum loss in  . As seen from the Figure 6, at negative and zero coordination, the mean
. As seen from the Figure 6, at negative and zero coordination, the mean  is much higher (almost double) than for positive coordination. Thus, when the MDI is actuated without any inspiratory flow rate, about 20%–32% of the medication is deposited in the plastic mouthpiece of the inhaler (compared to 12% for positive coordination), thereby reducing the amount of respirable aerosol medication. The baseline case of fp = 0 L/min, therefore, has the highest amount of
is much higher (almost double) than for positive coordination. Thus, when the MDI is actuated without any inspiratory flow rate, about 20%–32% of the medication is deposited in the plastic mouthpiece of the inhaler (compared to 12% for positive coordination), thereby reducing the amount of respirable aerosol medication. The baseline case of fp = 0 L/min, therefore, has the highest amount of  (32%) and
(32%) and  (62.5%) of all cases as there is no inspiratory flow rate even after MDI actuation.
(62.5%) of all cases as there is no inspiratory flow rate even after MDI actuation.
FIG. 6.
The percentage deposition in the in vitro lung (black bar), AIT (gray bar), and MDI mouthpiece (white bar) as a function of coordination or time of MDI actuation relative to the start of inspiration are presented. Each group of bars represents one MDI technique, the error bars show the range due to three repetitions of each experiment. The baseline result is shown in the beginning marked 0 L/min. The other bars correspond to the MDI technique of PIFR 60 L/min and duration 5.33 seconds, actuated at −0.5, 0 seconds, 0.6tr, 0.5td, and (td − 0.6tr). The error margins for in vitro lung deposition ranged from ±0.2% to ±2.3%, average ±1.3%. We found that the mean in vitro lung deposition is highest for actuation in the first half of inspiration, 43.8%, and lowest for negative coordination.
Note that for very late actuation, that is actuation in the second half of the inspiration with  , the presence of inspiration at the time of actuation ensured that the
, the presence of inspiration at the time of actuation ensured that the  is low (13%). However, due to the small volume of air inhaled coupled with a decreasing flow rate postactuation, the
is low (13%). However, due to the small volume of air inhaled coupled with a decreasing flow rate postactuation, the  (48%) increased and the
(48%) increased and the  (39%) decreased compared with actuation in the first half of inspiration (
(39%) decreased compared with actuation in the first half of inspiration ( ).
).
The two categories of results investigating the effect of PIFR (fp), duration of inspiration (td), defined in this study by the shape of inspiration waveform  , and coordination (ta) suggest that the optimal technique for maximizing the lung deposition of aerosol emitted from an HFA Ventolin MDI for 3 L IC is an inspiration with PIFR of 60–90 L/min of any duration in the range 2.28–5.33 seconds with a positive coordination in the first half of inspiration.
, and coordination (ta) suggest that the optimal technique for maximizing the lung deposition of aerosol emitted from an HFA Ventolin MDI for 3 L IC is an inspiration with PIFR of 60–90 L/min of any duration in the range 2.28–5.33 seconds with a positive coordination in the first half of inspiration.
Our study also has some limitations. As is the case with using simplified models to represent complex human maneuvers, our trapezoidal breathing model suffers from some disadvantages. The trapezoid model we developed has a symmetrical form, which is not the case for most inhalation curves recorded; see Figure 3a. The human inhalation waveforms have previously been approximated by asymmetric sinusoidal curves.(35,36) The asymmetric sinusoidal approximations yield waveforms much closer to actual breathing curves and hence may be a better choice for in vitro experimental procedures. However, because MDI actuation in the first half of the inhalation has the highest impact on lung deposition, we believe that the asymmetric trapezoidal waveforms may have similar lung deposition characteristics as that of symmetric trapezoidal waveforms, and thus is a valid first-order approximation.
Finally, the results obtained in our in vitro experimentation are an approximation to the actual in vivo lung deposition. Further investigation into this work would be to explore in vitro lung deposition using a more realistic lung model with lung airways of different sizes and in vivo lung deposition on human subjects, to explore the distribution of aerosol in different parts of the lung due to the variation in MDI technique.
In summary, in our in vitro experiment modeling of MDI technique based on the maneuvers recorded from subjects with asthma and COPD, we demonstrated that coordination of MDI actuation is the most important factor governing lung deposition of aerosol emitted by an Albuterol HFA-MDI (Ventolin). While higher inspiratory flow rates and increased duration of inspiration also yielded higher lung deposition, the increase was lower than the effect of coordination. Based on our results, the recommendation for optimal lung deposition for patients using an HFA containing MDI would be to inhale at high inspiratory flow rates, in the range from 60 to 90 L/min, and actuate the MDI in the first half of inspiration.
Acknowledgments
This study was supported by funding from National Institute of Health (Grant: NIH R41DA039450-01), provided by Cognita Labs LLC. The authors particularly thank Mr. Gaurav Patel for his knowledge, guidance, and expertise throughout the study. The authors also gratefully acknowledge Dr. Maura Puerto for her expert knowledge and guidance with the project and experimentation. The authors acknowledge Ms. June Chen for her contributions in the in vitro experimentation. The authors also greatly appreciate the help of Hadeel Abdulrazzaq, MD, and Caryn Pope, RCP, for overseeing the patient data collection at Ben Taub Hospital, Houston, Texas.
Author Disclosure Statement
Dr. Ashutosh Sabharwal is a Professor, Department of Electrical and Computer Engineering at Rice University, Houston, Texas. He is also a cofounder of Cognita Labs LLC. Ms. Rajoshi Biswas is a PhD candidate in the Department of Electrical and Computer Engineering at Rice University. She is also an employee of Cognita Labs LLC. Dr. Nicola Hanania is an Associate Professor, Baylor College of Medicine; Director, Airways Clinical Research Center, Houston, Texas. No competing financial interests exist.
References
- 1.Capstick TG, and Clifton IJ: Inhaler technique and training in people with chronic obstructive pulmonary disease and asthma. Expert Rev Respir Med. 2012;6:91–103 [DOI] [PubMed] [Google Scholar]
- 2.Rubin BK: What does it mean when a patient says, “My asthma medication is not working?” Chest. 2004;126:972–981 [DOI] [PubMed] [Google Scholar]
- 3.Roche N, Chrystyn H, Lavorini F, and Agusti A: Effectiveness of inhaler devices in adult asthma and COPD. EMJ Respir. 2013;1:64–71 [Google Scholar]
- 4.Melani AS, Bonavia M, Cilenti V, Cinti C, Lodi M, Martucci P, Serra M, Scichilone N, Sestini P, Aliani M, and Neri M: Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med. 2011;105:930–938 [DOI] [PubMed] [Google Scholar]
- 5.Laube BL, Janssens HM, De Jongh FHC, Devadason SG, Dhand R, Diot P, Everard ML, Horvath I, Navalesi P, Voshaar T, and Chrystyn H: What the pulmonary specialist should know about the new inhalation therapies. Eur Respir J. 2011;37:1308–1331 [DOI] [PubMed] [Google Scholar]
- 6.Bousquet J, and Khaltaev N: Global surveillance, prevention and control of chronic respiratory diseases: A comprehensive approach. World Health Organ. 2006;3:215–216 [Google Scholar]
- 7.Global Initiative for Asthma: Pocket Guide for Asthma Management and Prevention. Global Initiative for Asthma; p. 28, 2016 [Google Scholar]
- 8.Smith KJ, Chan HK, and Brown KF: Influence of flow rate on aerosol particle size distributions from pressurized and breath-actuated inhalers. J Aerosol Med. 1998;11:231–245 [DOI] [PubMed] [Google Scholar]
- 9.Pauwels R, Newman S, and Borgström L: Airway deposition and airway effects of antiasthma drugs delivered from metered-dose inhalers. Eur Respir J. 1997;10:2127–2138 [DOI] [PubMed] [Google Scholar]
- 10.Newman S, Steed K, Hooper G, Källén A, and Borgström L: Comparison of gamma scintigraphy and a pharmacokinetic technique for assessing pulmonary deposition of terbutaline sulphate delivered by pressurized metered dose inhaler. Pharma Res. 1995;12:231–236 [DOI] [PubMed] [Google Scholar]
- 11.Newman SP, Pavia D, and Clarke SW: Simple instructions for using pressurized aerosol bronchodilators. J R Soc Med 1980;73:776–779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Newman SP, Pavia D, and Clarke SW: How should a pressurized beta-adrenergic bronchodilator be inhaled? Eur J Respir Dis. 1981;62:3–21 [PubMed] [Google Scholar]
- 13.Newman SP, Pavia D, Garland N, and Clarke SW: Effects of various inhalation modes on the deposition of radioactive pressurized aerosols. Eur J Respir Dis Suppl. 1982;119:57–65 [PubMed] [Google Scholar]
- 14.Lawford P, and McKenzie D: Pressurized aerosol inhaler technique: How important are inhalation from residual volume, inspiratory flow rate and the time interval between puffs? Br J Dis Chest 1983;77:276–281 [PubMed] [Google Scholar]
- 15.Rahmatalla MF, Zuberbuhler PC, Lange CF, and Finlay WH: In vitro effect of a holding chamber on the mouth-throat deposition of QVAR (hydrofluoroalkane-beclomethasone dipropionate). J Aerosol Med. 2002;15:379–385 [DOI] [PubMed] [Google Scholar]
- 16.Lewis DA, Meakin BJ, and Brambilla G: New actuators versus old: Reasons and results for actuator modifications for HFA solution MDIs. Respir Drug Deliv. 2006;1:101–110 [Google Scholar]
- 17.Leach CL, Davidson PJ, and Boudreau RJ: Improved airway targeting with the CFC-free HFA-beclomethasone metered-dose inhaler compared with CFC-beclomethasone. Eur Respir J. 1998;12:1346–1353 [DOI] [PubMed] [Google Scholar]
- 18.Usmani OS, Biddiscombe MF, and Barnes PJ: Regional lung deposition and bronchodilator response as a function of beta2-agonist particle size. Am J Respir Crit Care Med. 2005;172:1497–1504 [DOI] [PubMed] [Google Scholar]
- 19.Hoye WL, Mogalian EM, and Myrdal Paul B: Effects of extreme temperatures on drug delivery of albuterol sulfate hydrofluoroalkane inhalation aerosols. Am J Health Syst Pharm. 2005;62:227. [DOI] [PubMed] [Google Scholar]
- 20.Cheng YS, Fu CS, Yazzie D, and Zhou Y: Respiratory deposition patterns of salbutamol pMDI with CFC and HFA-134a formulations in a human airway replica. J Aerosol Med. 2001;14:255–266 [DOI] [PubMed] [Google Scholar]
- 21.Ruzycki CA, Golshahi L, Vehring R, and Finlay WH: Comparison of in vitro deposition of pharmaceutical aerosols in an idealized child throat with in vivo deposition in the upper respiratory tract of children. Pharm Res. 2014;31:1525–1535 [DOI] [PubMed] [Google Scholar]
- 22.Zhang Y, Gilbertson K, and Finlay WH: In vivo-in vitro comparison of deposition in three mouth-throat models with Qvar and Turbuhaler inhalers. J Aerosol Med. 2007;20:227–235 [DOI] [PubMed] [Google Scholar]
- 23.Longest PW, Tian G, Li X, Son YJ, and Hindle M: Performance of combination drug and hygroscopic excipient submicrometer particles from a softmist inhaler in a characteristic model of the airways. Ann Biomed Eng. 2012;40:1–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Olsson B, Borgström L, Lundbäck H, and Svensson M: Validation of a general in vitro approach for prediction of total lung deposition in healthy adults for pharmaceutical inhalation products. J Aerosol Med Pulm. Drug Deliv. 2013;26:355–369 [DOI] [PubMed] [Google Scholar]
- 25.Inhaler Technique in Adults with Asthma or COPD. National Asthma Council; Australia: pp. 1–9, 2008 [Google Scholar]
- 26.Price D, Bosnic-Anticevich S, Briggs A, Chrystyn H, Rand C, Scheuch G, and Bousquet J: Inhaler competence in asthma: Common errors, barriers to use and recommended solutions. Respir Med. 2013;107:37–46 [DOI] [PubMed] [Google Scholar]
- 27.Giraud V, Allaert F-A, and Roche N: Inhaler technique and asthma: Feasability and acceptability of training by pharmacists. Respir Med. 2011;105:1815–1822 [DOI] [PubMed] [Google Scholar]
- 28.Ganong WF, and Barrett KE: Review of Medical Physiology. McGraw-Hill Medical, New York; 2005 [Google Scholar]
- 29.Shemirani FM, Hoe S, Lewis D, Church T, Vehring R, and Finlay WH: Investigation of the effect of ambient humidity on regional delivered dose with solution and suspension MDIs. J Aerosol Med Pulm Drug Deliv. 2012;26:215–222 [DOI] [PubMed] [Google Scholar]
- 30.Sprigge E, and Affairs P: Non uniform deposition of pMDI aerosol in a large volume spacer. 2014. (Doctoral dissertation, Carleton University Ottawa; ) [Google Scholar]
- 31.Hautmann J, Godoy SE, Marshik P, Chand R, Mcconville J, Krishna S, Krishna S, and Muttil P: Effect of time between actuation on the dose variability for three metered dose inhalers. Respir Drug Deliv Eur. 2013;2:429–434 [Google Scholar]
- 32.Newman SP, Weisz AW, Talaee N, and Clarke SW: Improvement of drug delivery with a breath actuated pressurised aerosol for patients with poor inhaler technique. Thorax. 1991;46:712–716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chrystyn H, and Price D: Not all asthma inhalers are the same: Factors to consider when prescribing an inhaler. Prim Care Respir J. 2009;18:243–249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Leach CL, Davidson PJ, Hasselquist BE, and Boudreau RJ: Influence of particle size and patient dosing technique on lung deposition of HFA-beclomethasone from a metered dose inhaler. J Aerosol Med. 2005;18:379–385 [DOI] [PubMed] [Google Scholar]
- 35.Delvadia RR, Longest PW, and Byron PR: Tests for aerosol deposition. I: Scaling a physical model of the upper airways to predict drug deposition variation in normal humans. J Aerosol Med Pulm Drug Deliv. 2012;25:32–40 [DOI] [PubMed] [Google Scholar]
- 36.Longest PW, Tian G, Walenga RL, and Hindle M: Comparing MDI and DPI aerosol deposition using in vitro experiments and a new stochastic individual path (SIP) model of the conducting airways. Pharm Res. 2012;29:1670–1688 [DOI] [PubMed] [Google Scholar]