Abstract
Purpose: Transgender women have consistently reported elevated rates of lifetime physical and sexual abuse. This study examined the associations between reported physical and/or sexual abuse and symptoms of psychological and emotional distress among a sample of urban, high-risk transgender women.
Methods: From June 2005 through July 2012, 99 transgender women enrolled in a Comprehensive Risk Counseling and Services program in Hollywood, CA. Seemingly unrelated regression equations (SURE) were used to simultaneously regress psychiatric symptom reports on participant sociodemographic characteristics and self-reported history of physical/sexual abuse.
Results: Participants were African American/Black (33.3%), Caucasian/White (28.3%), or Hispanic/Latina (24.2%). Average age was 35 years (standard deviation [SD] = 9), and 37.4% of participants self-reported an HIV-positive status. Most (84.9%) participants reported experiencing physical or sexual abuse at some point in their lifetime, and symptoms of psychological and emotional distress (as measured by the Brief Symptom Inventory) among those who reported abuse were more severe than those observed in cisgender psychiatric in-patient populations. After controlling for participant sociodemographics, prior experience of physical and/or sexual abuse was associated with significantly increased psychological and emotional distress across all measured symptom domains except psychoticism [χ2(9) = 17.56; p < 0.05].
Conclusion: Given these associations as well as the high prevalence of physical and/or sexual abuse among transgender women, mental health professionals and social service providers working with this population should be sensitive to the abuse history and mental health needs of the transgender women with whom they work.
Keywords: : mental health, physical abuse, sexual abuse, suicide, transgender women
Introduction
Transgender women (hereafter “trans women”) are estimated to comprise approximately 0.1%–0.5% of the overall U.S. population1; however, trans women are at a far greater risk for experiencing physical or sexual abuse, and/or psychological distress when compared with other adult populations.2–4 Over the past decade, survey-based research with trans women has found reported rates of physical abuse ranging from 39% to 47%,2,4–6 and sexual abuse rates ranging from 50% to 59%.4,7
The observed mental health correlates of such physical and sexual abuse among communities of trans women are pronounced. Studies published in the past 5 years report a significant association between incidents of self-reported physical and sexual abuse and a lifetime prevalence of suicidal behaviors.2 A recently completed 3-year prospective study of trans women demonstrated similar results, with significant associations between physical gender abuse and major depressive symptoms.8 Another study of 135 trans women found that those who reported interpersonal trauma and discriminatory life events were 29.9% more likely to engage in self-injurious behavior, and 34.8% had attempted suicide.9 These findings, though not denoting causal relationships, demonstrate consistent statistical correlation between experienced physical and/or sexual abuse and negative psychological outcomes among trans women.
Research has further demonstrated that the experience of abuse (physical and sexual) has been associated with increased odds of developing severe mental illness, with considerable emphasis on symptoms of trauma and/or Post Traumatic Stress Disorder (PTSD).10–12 Furthermore, the experience of abuse during childhood has been significantly and positively associated with both psychiatric diagnoses and symptoms, such as PTSD, depression, Generalized Anxiety Disorder, and perceived stress among sexual minority groups.13,14 Research in the past decade has highlighted the increased risk of sexual minority groups to experience childhood abuse, possibly leading to a higher prevalence of mental illness within the adult population.13,14 Early studies on trans women demonstrated that distinct from sexual minority groups, the prevalence of reported physical and sexual abuse is endemic among trans women.2,4–6
Potential mental health outcomes other than depression and suicidality associated with past abuse have been largely overlooked. Specifically, research on trauma symptomology and its impact on the overall functioning of trans women have yet to be investigated. The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) provides a model for trauma, including symptom criteria such as experiencing an event that was perceived as life threatening to the self or others, intrusive symptoms (e.g., intrusive memories/thoughts, flashbacks, nightmares, panic attacks), avoidance, negative alterations in mood and cognition, and change in physiological arousal.15 Within the existing research of trans women's health, trauma-specific symptomology has largely been neglected in favor of depressive symptomology and suicidal ideation, particularly in relation to experienced abuse.
Given the persistent and pervasive rates of physical and/or sexual abuse among samples of trans women, and the lack of a granular understanding of how abuse affects mental health in this population beyond observed increases in suicidal ideation and depression, this study had three goals. The first was to report the severity of a broad range of psychological and emotional symptom domains in a sample of high-risk, urban trans women. The second was to test the association between the severity of these psychological and emotional distress symptoms and prior physical or sexual abuse. The last goal was to compare the severity of psychological and emotional distress among abused and non-abused trans women in this sample with the severity of symptom complaints observed among cisgender male and cisgender female psychiatric in-patient and non-patient samples to contextualize the relative severity of negative mental health symptoms experienced by this sample.
Methods
Participants
From June 2005 through July 2012, participants were recruited from a community-based, low-intensity, health education/risk reduction HIV prevention program serving high-risk trans women in the Hollywood area of Los Angeles County. Potential participants were eligible for the health education/risk reduction HIV prevention program if they self-reported identifying as a trans woman, regardless of her stage of gender transition. Potential participants were recruited to the health education/risk reduction program through street- and venue-based outreach. Outreach procedures have been reported elsewhere.16–18 All participants enrolled in the low-intensity health education/risk reduction HIV program who requested a higher level of intervention services were referred to the Comprehensive Risk Counseling and Services (CRCS) program. However, in addition to being within the eligible target population, that is, a self-reported trans woman, potential participants for the CRCS program must also self-report multiple, complex needs and be at risk for infection or transmission of HIV. Thus, the analytic sample (i.e., those enrolled in the CRCS program; N = 99) comprised trans women who were at an extremely high risk for HIV infection/transmission.
Procedure
After a written informed consent and an intake screening to assess risk behaviors and needs, a comprehensive baseline assessment was conducted to assess sociodemographic characteristics, physical and mental health history, levels of psychological and emotional distress, and acuity level. Participants received $5 on completion of the baseline comprehensive assessment during program enrollment. After completing baseline assessments, participants met with the counselor to assess areas of behavioral change and to create a participant-centered prevention plan. Participants were compensated with a $10 incentive per session, up to a maximum of five sessions, and a $5 bonus after achieving their first identified behavioral change goal. Participants also received incentives for completing a 30-, 60-, and 90-day post-intervention follow-up evaluation ($5, $15, and $10, respectively). The maximum that participants could earn was $90. All incentives were provided in gift certificates, and no cash was transmitted. All program materials, including the consent form, program protocol, and data assessment forms for both the health education/risk reduction program and the CRCS program, were approved by the funding agency; Institutional Review Board approval was not required.
Measures
Program Admissions Assessment Form. This seven-page measure, designed by the senior author, collects information describing participant sociodemographic characteristics, sexual risk behaviors, healthcare, and transgender-specific healthcare (e.g., hormone use or misuse). The Program Admissions Assessment is a standard-type programmatic intake assessment and, therefore, does not derive from a theoretical base or have existing scores.
Brief Symptom Inventory
The Brief Symptom Inventory (BSI) is a self-report symptom scale that is a shortened version of the Symptom Checklist-90 (SCL-90-R).19,20 Reliability scores for the BSI are consistently high and range from 0.75 (psychoticism) to 0.89 (depression) on the individual subscales21; both criterion and convergent validity have also been established by using the SCL-90-R and the Minnesota Multiphasic Personality Inventory.19,21 The BSI was administered as an indicator of state psychological (including psychosis) and emotional functioning. Established samples of BSI symptom complaints from adult psychiatric in-patient and non-patient cisgender males and females19 provide comparative baselines against which scores from the current study are compared.
Addiction Severity Index
The Addiction Severity Index (ASI) is a standardized clinical interview that gathers participants' demographic and sociodemographic data and determines addiction-related problem severity.22 The ASI asks respondents: (1) “Did anyone abuse you physically (including causing you physical harm)?” and (2) “Did anyone abuse you sexually (including forced sexual advances/acts)?” These items were combined to determine prior abuse (i.e., a “yes” response to either question was coded “1,” otherwise “0”). As an assessment, the ASI has excellent inter-rater and test-retest reliability as well as discriminant and concurrent validity.23
Statistical analyses
Counts and their corresponding percentages are provided for all nominal variables, whereas means and standard deviations (SDs) are provided for all continuous variables. Tests of association across a lifetime history of both physical and sexual abuse were carried out by using chi-square tests, where appropriate, and Fisher's Exact tests, where necessary. Multivariable associations between symptoms of psychological distress and abuse history while controlling for participant sociodemographics were carried out by using seemingly unrelated regression equations (SURE). This analytical technique is preferred to nine discrete hypothesis tests that are carried out via recursive ordinary least-squares regression as it allows all nine separate symptom domains to be simultaneously regressed on the statistical covariates at once. This simultaneously reduces the odds of a Type-I error due to iterative hypothesis testing, and it further allows for subsequent omnibus tests of significance of abuse history on symptom complaints. All analyses were carried out by using Stata V13 (StataCorp LLC, College Station, TX), and all significance tests were two tailed.
Results
Most participants identified as African American/Black (33.3%), Caucasian/White (28.3%), or Hispanic/Latina (24.2%). The mean age was 35.1 years (SD = 9.1); however, among the subset of trans women who reported prior abuse (n = 84/99; 84.9%), their mean age was significantly older than the mean age of the trans women who had not experienced prior abuse (35.9 years vs. 30.9 years; p ≤ 0.05). Slightly more than a third of the sample reported being HIV positive (37.4%), and nearly a third were currently homeless (30.3%). On average, the sample averaged less than 12 years of lifetime educational attainment (mean = 11.4; SD = 2.5).
At baseline, participants who had experienced prior physical or sexual abuse reported more severe symptom complaints across every measured symptom domain except hostility and psychoticism, both of which were also observed to be greater in the prior abuse group and were trending toward significance (both p ≤ 0.10). Compared with the trans women who reported no prior abuse, trans women who had reported abuse experienced on average more severe symptoms of somatization (0.32 vs. 0.81), obsessive compulsive disorder (0.59 vs. 1.35), interpersonal sensitivity (0.60 vs. 1.29), depression (0.61 vs. 1.27), anxiety (0.43 vs. 1.19), phobic anxiety (0.39 vs. 1.02), and paranoid ideation (0.64 vs. 1.50; all p ≤ 0.05) (Table 1).
Table 1.
Participants' Sociodemographics and Psychological/Emotional Distress by Prior Physical and/or Sexual Abuse (N = 99)
| Not abused (n = 15) | Abused (n = 84) | ||||
|---|---|---|---|---|---|
| n | % | n | % | Effect sizea | |
| Race/ethnicity | |||||
| Caucasian/White | 3 | 20.0 | 25 | 29.8 | ns |
| African American/Black | 6 | 40.0 | 27 | 32.1 | |
| Hispanic/Latina | 3 | 20.0 | 21 | 25.0 | |
| Multiracial/other | 3 | 20.0 | 11 | 13.1 | |
| Age (mean, SD) | |||||
| Years | 30.9 | 6.9 | 35.9 | 9.3 | −0.56* |
| Educational attainment (mean, SD) | |||||
| Years | 12.1 | 1.3 | 11.3 | 2.6 | ns |
| HIV status | |||||
| HIV positive | 4 | 26.7 | 33 | 39.3 | ns |
| Homelessness | |||||
| Currently living on the streets | 4 | 26.7 | 26 | 31.0 | ns |
| Psychological/emotional distress symptoms (current)b | Mean | SD | Mean | SD | |
| Somatization | 0.32 | 0.56 | 0.81 | 0.87 | −0.59* |
| Obsessive compulsive disorder | 0.59 | 0.59 | 1.35 | 1.12 | −0.73** |
| Interpersonal sensitivity | 0.60 | 0.87 | 1.29 | 1.06 | −0.68* |
| Depression | 0.61 | 0.91 | 1.27 | 1.10 | −0.62* |
| Anxiety | 0.43 | 0.64 | 1.19 | 1.08 | −0.75** |
| Hostility | 0.49 | 0.79 | 0.89 | 0.88 | −0.47† |
| Phobic anxiety | 0.39 | 0.50 | 1.02 | 1.10 | −0.62* |
| Paranoid ideation | 0.64 | 0.71 | 1.50 | 1.04 | −0.88** |
| Psychoticism | 0.53 | 0.80 | 1.02 | 1.00 | −0.51† |
Cohen's d for uneven groups.
As measured by the Brief Symptom Inventory.
≤0.10; *p ≤ 0.05; **p ≤ 0.01; two tailed.
ns, Not significant; SD, standard deviation.
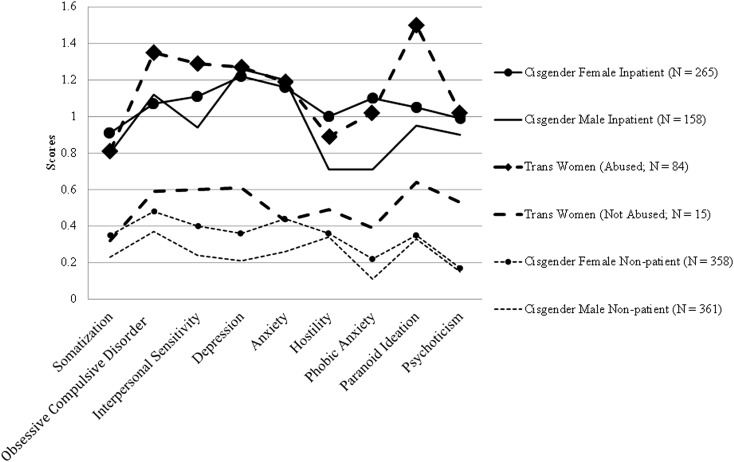
Using t-tests to compare the severity of psychological and emotional distress of this sample of trans women against samples of cisgender males and cisgender females,19 trans women who had experienced prior abuse reported significantly (p < 0.0001) higher levels of symptom severity across all measured symptom domains of the BSI relative to cisgender male or cisgender female non-patient populations, and significantly (p < 0.05) higher levels of symptom severity on the interpersonal sensitivity, phobic anxiety, and paranoid ideation domains relative to the cisgender male psychiatric in-patient and/or cisgender female psychiatric in-patient populations. Though the small number of trans women who did not experience prior abuse (n = 15) prevents accurate statistical contrasts with cisgender populations, Figure 1 demonstrates that the trans women who were not abused reported levels of symptom severity situated between cisgender male and female in-patient and non-patient populations.
FIG. 1.
Symptoms of psychological and emotional distress among high-risk urban transgender women compared with adult cisgender male and cisgender female psychiatric in-patient and non-patient samples. Average scores for each symptom category assessed by the Brief Symptom Inventory comparing high-risk urban trans women who have self-reported physical and/or sexual abuse (big dash with square) or have not self-reported any abuse (big dash) with adult psychiatric in-patient cisgender males (solid line), adult non-patient cisgender males (small dash), adult psychiatric in-patient cisgender females (solid line with circles), and adult non-patient cisgender females (small dash with circles).
As demonstrated in Table 2, when controlling for participant sociodemographics through multivariable analyses, bivariate patterns remain stable or are strengthened. The lifetime experience of physical and/or sexual abuse was associated with significantly more severe symptoms of (in increasing magnitude of estimated effect): somatization (b = 0.43), hostility (b = 0.47), depression (b = 0.61), obsessive compulsive disorder (b = 0.68), interpersonal sensitivity (b = 0.71), phobic anxiety (b = 0.75), anxiety (b = 0.87), and paranoid ideation (0.91; all p ≤ 0.05). The effect of prior abuse on the severity of psychoticism symptoms was also positive and trending toward significance (b = 0.46; p = 0.09). The SURE omnibus test of significance for the effects of prior experience of abuse on psychological symptom complaints while controlling for participant sociodemographics revealed that prior experience of abuse was significantly related to severity of psychological symptom complaints [χ2(9) = 17.56; p = 0.04].
Table 2.
Associations Between Symptoms of Psychological/Emotional Distress and Physical/Sexual Abuse (N = 99)
| Somatization | Obsessive compulsive disorder | Interpersonal sensitivity | Depression | Anxiety | Hostility | Phobic anxiety | Paranoid ideation | Psychoticism | |
|---|---|---|---|---|---|---|---|---|---|
| b (95% CI) | b (95% CI) | b (95% CI) | b (95% CI) | b (95% CI) | b (95% CI) | b (95% CI) | b (95% CI) | b (95% CI) | |
| Physical and/or sexual abuse (lifetime) | 0.43* (0.00–0.86) | 0.68* (0.12–1.25) | 0.71** (0.16–1.27) | 0.61* (0.02–1.19) | 0.87** (0.32–1.42) | 0.47* (0.01–0.93) | 0.75** (0.21–1.29) | 0.91*** (0.37–1.45) | 0.46† ([−0.07] −0.99) |
≤0.10; *p ≤ 0.05; **p ≤ 0.01; ***p ≤ 0.001; all significance tests two-tailed.
Statistical controls: race/ethnicity, age, educational attainment, HIV status, homelessness.
Omnibus test of significance (i.e., b = 0 across all symptom domains): χ2(9) = 17.56; p < 0.05.
CI, confidence interval.
Discussion
This sample of high-risk trans women was predominantly non-White, reported limited educational attainment, and included significant numbers of people experiencing homelessness and/or who were HIV positive. The severity of psychological and emotional distress observed was high relative to standardized cisgender populations, particularly for those trans women who reported prior experience of physical and/or sexual abuse (84.9% of participants). The results suggest that the experience of physical and/or sexual abuse among high-risk trans women is associated with increased psychological and emotional distress on all measured symptom domains of the BSI. Particularly strong positive associations were found between physical and/or sexual abuse and symptoms of paranoid ideation, phobic anxiety, obsessive compulsive disorder, interpersonal sensitivity, and anxiety; in each case, trans women who had experienced prior abuse exhibited symptoms that were equal to, or significantly more severe than, those observed in cisgender psychiatric in-patient populations.
Though data were not obtained to assess for trauma-specific symptom presentation, the symptom domains with the strongest associations to lifetime prevalence of physical and/or sexual abuse have historically been correlated with trauma.15 Avoidance symptoms that are common to trauma-related disorders may also be reflected in the elevated symptoms scores of phobic anxiety and anxiety, in general. This study demonstrates the distinct relationship between past abuse and a broad array of symptom complaints, including current trauma symptom presentation. This presents direction for future psychological research pertaining to how trans women who have experienced physical and/or sexual abuse cope with additional symptoms of psychological distress beyond depression and/or suicidal ideation.
The results presented on the negative psychological states and the presence of abuse histories highlight the capacity for resilience and vulnerability of this population of high-risk, urban trans women. Many trans women, such as those described in this study, struggle with severe mental illness and symptoms of emotional distress that often go largely untreated due to barriers in accessing mental health treatment.24–26 The capacity of trans women to overcome these negative psychological symptoms that are linked to trauma histories and to utilize both adaptive (social support, meditation) and maladaptive (substance use, hormone misuse) coping strategies to survive defines resiliency and determination. Future investigation should examine resiliency and the coping strategies utilized in the frequent absence of mental health support and/or hospitalization, as these strategies may be useful in informing culturally competent and effective clinical treatment and intervention.
Limitations
The limitations of this study are based in its cross-sectional design with self-report measures. Participants' life events and current symptoms were not verified by using other sources of information. In addition, these results represented a single moment in time. The sample consisted of a subgroup of high-risk trans women in Hollywood, California. Cultural attitudes and norms in trans women populations in other urban areas may be different and lead to different outcomes. Furthermore, the data from in-patient and non-patient cisgender males and cisgender females were derived from established populations published alongside the BSI, intended only for the contextualization of symptom severity. Consequently, there are no sociodemographic or risk behavior characteristics from these samples that could be used in comparison with the sample in this study. Thus, the results from this study must be interpreted in light of these limitations.
Conclusion
Given these findings, mental health professionals and social service providers working with high-risk trans women or similar populations should be particularly aware of the likelihood of strong negative psychological impact related to reported histories of abuse, specifically as these impact trans women's behaviors in seeking primary care, clinical, and legal resources. Histories of abuse within gender minority, sexual minority, and nonsexual minority groups have been positively associated with various negative mental health outcomes, including increased suicidal ideation, suicide attempts, and depressive symptoms.2,9,10,27 The disproportionately high prevalence of physical and/or sexual abuse within trans women populations calls for interventions that explore the sources of resilience. Similarly, discussions on how to reduce the structural barriers that inhibit trans women from seeking medical and/or mental health treatment require further exploration. Future research should move toward intervention development, as psychological and emotional distress among high-risk, urban trans women remains high. Intervention development should focus on relieving clinical distress more effectively and work on improving overall functionality.
Acknowledgments
This study was supported by the Los Angeles County, Department of Public Health, Division of HIV and STD Programs (formerly Office of AIDS Programs and Policy) contract Nos. H700861 and PH001053. C.J.R. acknowledges additional support from the National Institute of Mental Health (P30 MH58107). The authors assert that all work was carried out in accordance with the Declaration of Helsinki.
Disclaimer
An earlier version of this article was presented at the annual meeting of the Transgender Health Summit, Oakland, California, April 2015 and the American Psychological Association, Washington, DC, August 2014.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Bingham T, Carlos-Henderson J: Los Angeles County Transgender Population Estimates, 2012. Los Angeles, CA: Los Angeles County Department of Public Health Division of HIV and STD Programs, 2012 [Google Scholar]
- 2.Testa RJ, Sciacca LM, Wang F, et al. : Effects of violence on transgender people. Profess Psychol Res Pract 2012;43:452–459 [Google Scholar]
- 3.Nemoto T, Bödeker B, Iwamoto M: Social support, exposure to violence and transphobia, and correlates of depression among male-to-female transgender women with a history of sex work. Am J Public Health 2011;101:1980–1988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clements-Nolle K, Marx R, Katz M: Attempted suicide among transgender persons: The influence of gender-based discrimination and victimization. J Homosex 2006;51:53–69 [DOI] [PubMed] [Google Scholar]
- 5.Xavier JM, Bobbin M, Singer B, Budd E: A needs assessment of transgendered people of color living in Washington, DC. Int J Transgend 2005;8:31–47 [Google Scholar]
- 6.Reback CJ, Simon P: The Los Angeles transgender health study: Creating a research and community collaboration. In: Preventing AIDS: Community-Science Collaborations. Edited by Bowser B, Mishra S, Reback CJ, Lemp G. New York: The Haworth Press, 2004, pp 115–131 [Google Scholar]
- 7.Garofalo R, Deleon J, Osmer E, et al. : Overlooked, misunderstood and at-risk: Exploring the lives and HIV risk of ethnic minority male-to-female transgender youth. J Adolesc Health 2006;38:230–236 [DOI] [PubMed] [Google Scholar]
- 8.Nuttbrock L, Bockting W, Rosenblum A, et al. : Gender abuse and major depression among transgender women: A prospective study of vulnerability and resilience. Am J Public Health 2014;104:2191–2198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.House AS, Van Horn E, Coppeans C, Stepleman LM: Interpersonal trauma and discriminatory events as predictors of suicidal and nonsuicidal self-injury in gay, lesbian, bisexual, and transgender persons. Traumatology 2011;17:75–85 [Google Scholar]
- 10.Springer KW, Sheridan J, Kuo D, Carnes M: Long-term physical and mental health consequences of childhood physical abuse: Results from a large population-based sample of men and women. Child Abuse Negl 2007;31:517–530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Katon W, Sullivan M, Walker E: Medical symptoms without identified pathology: Relationship to psychiatric disorders, childhood and adult trauma, and personality traits. Ann Intern Med 2001;134(Pt 2):917–925 [DOI] [PubMed] [Google Scholar]
- 12.Kendler KS, Bulik CM, Silberg J, et al. : Childhood sexual abuse and adult psychiatric and substance use disorders in women: An epidemiological and cotwin control analysis. Arch Gen Psychiatry 2000;57:953–959 [DOI] [PubMed] [Google Scholar]
- 13.Friedman MS, Marshal MP, Stall R, et al. : Gay-related development, early abuse and adult health outcomes among gay males. AIDS Behav 2008;12:891–902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Balsam KF, Lehavot K, Beadnell B, Circo E: Childhood abuse and mental health indicators among ethnically diverse lesbian, gay, and bisexual adults. J Consult Clin Psychol 2010;78:459–468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). Arlington, VA: American Psychiatric Association Publishing, 2013 [Google Scholar]
- 16.Bowers JR, Branson CM, Fletcher J, Reback CJ: Differences in substance use and sexual partnering between men who have sex with men, men who have sex with men and women and transgender women. Cult Health Sex 2011;13:629–642 [DOI] [PubMed] [Google Scholar]
- 17.Reback CJ, Fletcher JB, Shoptaw S, Grella CE: Methamphetamine and other substance use trends among street-recruited men who have sex with men, from 2008 to 2011. Drug Alcohol Depend 2013;133:262–265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reback CJ, Shoptaw S, Grella CE: Methamphetamine use trends among street-recruited gay and bisexual males, from 1999 to 2007. J Urban Health 2008;85:874–879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Derogatis LR, Melisaratos N: The Brief Symptom Inventory: An introductory report. Psychol Med 1983;13:595–605 [PubMed] [Google Scholar]
- 20.Derogatis LR: The SCL-90 Manual I: Scoring, Administration and Procedures for the SCL-90. Baltimore, MD: Clinical Psychometrics Research, 1977 [Google Scholar]
- 21.Boulet J, Boss MW: Reliability and validity of the Brief Symptom Inventory. Psychol Assess J Consult Clin Psychol 1991;3:433–437 [Google Scholar]
- 22.McLellan AT, Luborsky L, Cacciola J, et al. : New data from the Addiction Severity Index. Reliability and validity in three centers. J Nerv Mental Dis 1985;173:412–423 [DOI] [PubMed] [Google Scholar]
- 23.McLellan AT, Kushner H, Metzger D, et al. : The fifth edition of the Addiction Severity Index. J Subst Abuse Treat 1992;9:199–213 [DOI] [PubMed] [Google Scholar]
- 24.Shipherd JC, Green KE, Abramovitz S: Transgender clients: Identifying and minimizing barriers to mental health treatment. J Gay Lesbian Mental Health 2010;14:94–108 [Google Scholar]
- 25.Sanchez NF, Sanchez JP, Danoff A: Health care utilization, barriers to care, and hormone usage among male-to-female transgender persons in New York City. Am J Public Health 2009;99:713–719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clements-Nolle K, Marx R, Guzman R, Katz M: HIV prevalence, risk behaviors, health care use, and mental health status of transgender persons: Implications for public health intervention. Am J Public Health 2001;91:915–921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nuttbrock L, Hwahng S, Bockting W, et al. : Psychiatric impact of gender-related abuse across the life course of male-to-female transgender persons. J Sex Res 2010;47:12–23 [DOI] [PubMed] [Google Scholar]