Abstract
Factor XI deficiency (Hemophilia C) is a very rare autosomal recessive bleeding disorder. Patients with factor XI deficiency do not typically show any spontaneous bleeding or specific symptoms. Sometimes those who have this disorder are identified during special situations such as trauma or surgery. Orthognathic surgery is particularly associated with a high bleeding risk. Therefore, great care must be taken when treating patients with bleeding disorders such as factor XI deficiency. There are a few reports that address the management of patients with bleeding disorders during orthognathic surgery. The current report describes a patient with factor XI deficiency who underwent Le Fort I osteotomy together with bilateral sagittal split osteotomy. The patient's condition was assessed using both rotation thromboelastometry (ROTEM™) and noninvasive measurements of total hemoglobin (SpHb) using Masimo Radical 7 (Masimo Co. CA, USA).
Keywords: Continuous noninvasive hemoglobin monitoring, Factor XI deficiency, Orthognathic surgery, Rotation thromboelastometry
Factor XI deficiency is a very rare autosomal recessive bleeding disorder. In many cases, the disorder is identified after trauma or surgery because otherwise, patients do not experience any spontaneous bleeding or other specific symptoms [1,2,3]. Patients are particularly prone to bleeding during surgery or trauma which involves the oral mucosa, nose or genitourinary tract whose sites are rich in fibrinolytic activators [4,5,6]. Factor XI deficiency occurs in approximately 1:1,000,000 Ashkenazi Jews [3,7,8]. Orthognathic surgery is usually associated with a high bleeding risk in patients with factor XI deficiency. Therefore, great care must be taken when treating patients with such bleeding disorders.
Hemoglobin measurement in patients undergoing orthognathic surgery is one of the most significant examinations. Based upon patient's degree of anemia, anesthesiologists decide whether or not a blood transfusion is indicated. In the case of hemorrhagic diseases such as hemophilia, such decisions must be made with extra care. This might require frequent and repeated invasive blood sampling. However, it is disadvantageous because of the time commitment that it requires. Therefore, continuous monitoring is more useful in cases in which there is heavy bleeding such as during orthognathic surgery, or in patients with hemophilia who have a tendency to hemorrhage [9]. The Masimo Radical 7 is a noninvasive device capable of continuously measuring hemoglobin (SpHb). The usage of this device during surgery allows proper and timely treatment.
There are few reports that address the management of patients with bleeding disorders who are undergoing orthognathic surgery [10,11,12]. Here, we present effective perioperative management using the SpHb and rotation thromboelastometry (ROTEM™) during orthognathic surgery of patients with Factor XI deficiency.
CASE REPORT
A 25-year-old female patient (weight: 52 kg and height: 162 cm) with dentofacial anomalies having both anterior edge to edge bite relationship and facial asymmetry was scheduled to have Le Fort I osteotomy and bilateral sagittal split osteotomy (BSSRO) surgery under general anesthesia. The patient was also diagnosed with factor XI deficiency with an increased activated partial thromboplastin time (aPTT) of 87.5 seconds (normal: 26-35.3 seconds), and a factor XI activity of 5% (normal: 60-150%). Other laboratory values, including prothrombin time and international normalized ratio (PT INR) (1.06, normal: 0.8-1.2), and PT % (91.0%, normal: 80-120%) were within normal limits. The hemoglobin (Hb), hematocrit (Hct) and platelet counts were 12.8 g/dl (normal: 12-16 g/dl), 37.6 (normal: 36-48%), and 194,000/mm3, respectively. A chest radiograph, electrocardiogram (ECG), and other laboratory findings were unremarkable. The decision was made to operate on the patient using both the SpHb and rotation thromboelastometry for effective perioperative management.
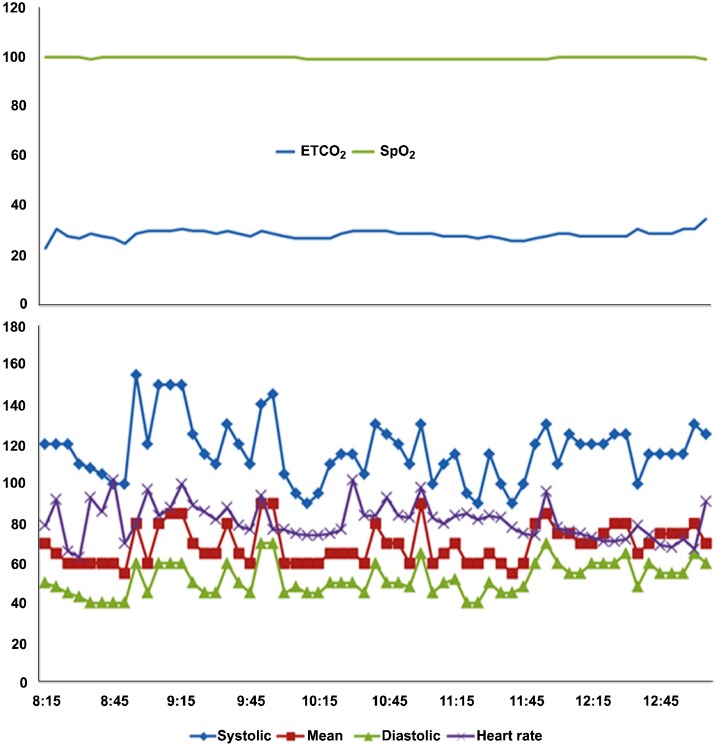
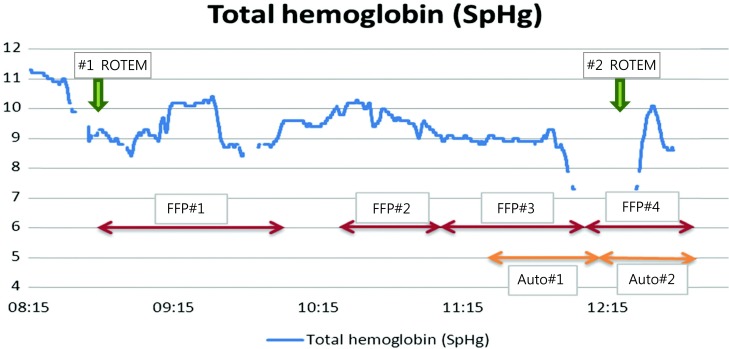
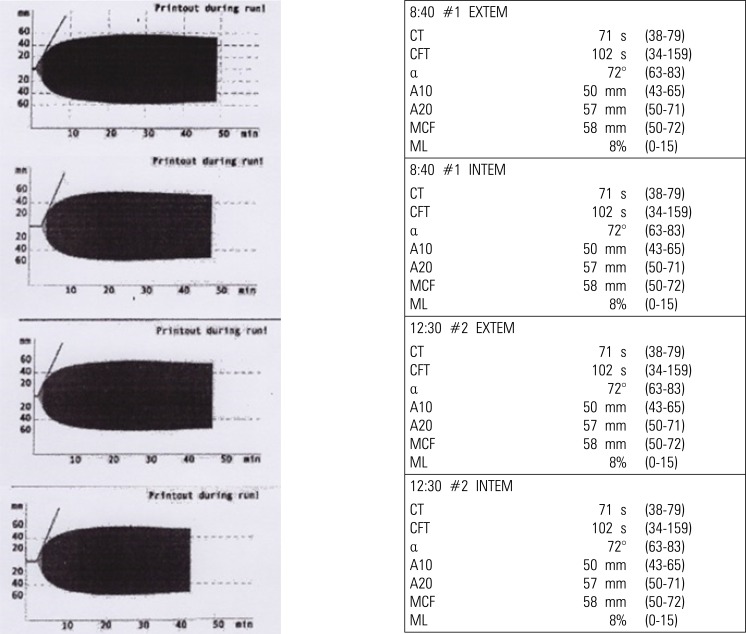
During surgery, the patient's ECG, noninvasive blood pressure, percutaneous oxygen saturation, temperature, and arterial line were actively monitored. Intravenous thiopental 175.0 mg was used to induce anesthesia. The patient was intubated nasally after the administration of cisatracurium 12.0 mg. Anesthesia was maintained with 5-6% desflurane, 50% nitrous oxide and oxygen. The patient's vital signs were stable throughout the procedure (Fig 1). The surgery time was total 250 minutes and the anesthesia time was 300 minutes. There was a total of 560 ml blood loss, and 500 ml of urine output. The patient's Hb levels were continuously checked through the SpHb values (Fig. 2). Four units of fresh frozen plasma (FFP) and two autologous units of blood (360 ml) were used during surgery based upon the continuously monitored blood levels of Hb. At the end of surgery, the patient's Hb was 8.1 g/dl and Hct was 27%. The patient was extubated with the removal of the endotracheal tube when she resumed spontaneous breathing but before she recovered consciousness. The patient was transferred to the recovery room. The ROTEM™ analysis showed normal variables in the extrinsically activated test (EXTEM) and intrinsically activated test (INTEM) (Fig. 3).
Fig. 1. Perioperative anesthetic monitoring of vital signs.
ETCO2: the level of carbon dioxide released at the end of expiration, SpO2: pulse oximetry oxygen saturation, systolic: systolic blood pressure, Mean: mean blood pressure, diastolic: diastolic blood pressure.
Fig. 2. Perioperative hemoglobin change. Total hemoglobin was continuously measured by the Masimo Radical-7.
FFP: Fresh Frozen Plasma, Auto: Autotransfusion, ROTEM: Rotation Thromboelastometry.
Fig. 3. Thromboelastograph curve. The curve demonstrates clot initiation, propagation, stabilization, and lysis.
CT: Clotting Time; CFT: Clot formation time; alpha: Alpha-angle; A10: Amplitude 10 min after CT; MCF: Maximum clot firmness; LI30; Lysis index 30 min after CT, ML; Maximum lysis.
After surgery but before the patient's discharge, her bleeding tendency was investigated using coagulation tests including aPTT. Seven days after surgery, aPTT was slightly elevated at 48.4 seconds. The patient was discharged without any complications.
DISCUSSION
Factor XI deficiency (hemophilia C) is a rare disease. As of 2005, there were only ten registered patients with factor XI deficiency in Korea, accounting for 0.5% of the population. This figure likely underestimates the true number of patients because those who with factor XI deficiencies are not diagnosed unless they experience trauma or undergo surgery. The recommended method for managing factor XI deficiency during surgery in which a large amount of bleeding is expected is with FFP transfusion [13,14]. An antifibrinolytic drug such as tranexamic acid has also been reported to be highly effective in reducing bleeding [1,3,15]. There is also literature suggesting that administering factor VII during surgery is successful, except that it also increases the risk of thrombosis [16,17,18].
The maxillofacial region is rich in vasculature. It is often difficult to control bleeding during orthognathic surgery and tends to be complicated by hemorrhage more often than do other types of surgery [19]. Prior studies have suggested that orthognathic surgery involves an average of 436.1 ml blood loss inside the oral cavity and takes an average of 196.9 minutes in operation time [20]. The amount of blood loss is directly related to the operation time and degree of intervention. The actual amount of bleeding often exceeds the expected amount; therefore, reserve blood should be prepared. Sometimes, even autologous transfusion becomes necessary.
A skilled surgical technique can significantly reduce blood loss. In addition, medications such as tranexamic acid and desmopressin can also be used [21]. In the present case, the patient lost 560.0 ml of blood during a 350-minutes operation. The patient was transfused with four units of FFP and two units of autologous blood. We also used tranexamic acid one day before surgery to prevent bleeding as much as possible.
Since orthognathic surgery is particularly associated with excess bleeding, the patient was carefully monitored throughout the procedure using both Masimo and ROTEM™. Masimo is a device capable of continuous, noninvasive hemoglobin monitoring. The device enables appropriate patient care and efficient monitoring so that clinical decisions can be made quickly, including those regarding transfusion [9]. Similarly, the ROTEM™ continuously monitors coagulation factors and provides quantitative parameters. This device provides information regarding clot stability, elasticity, formation time, and propagation. Using these data, one can predict when a transfusion may be required. The thromboelastometry curve before and after surgery is shown in Fig. 2. All figures including clotting time, and clot formation time were in the normal ranges. The curve also has a normal shape. INTEM is contact activation, and provides information similar to aPTT. EXTEM reflects tissue factor activation, providing information similar to PT [22].
ROTEM™ is especially useful during surgery of patients with bleeding disorders, because it produces results within ten minutes. In contrast, standard laboratory tests (PT, aPTT, fibrinogen concentration, platelet count) take much longer. Therefore, ROTEM™ allows providers to monitor the amount of clotting factor in hemophilia patients. In summary, this case describes orthognathic surgery conducted in a patient with Factor XI deficiency. The patient received preoperative tranexamic acids and monitored perioperatively with both the Masimo Radical 7 and ROTEM™, and later received FFP.
References
- 1.Bolton-Maggs PH, Young Wan-Yin B, McCraw AH, Slack J, Kernoff PB. Inheritance and bleeding in factor xi deficiency. Br J Haematol. 1988;69:521–528. doi: 10.1111/j.1365-2141.1988.tb02409.x. [DOI] [PubMed] [Google Scholar]
- 2.Salomon O, Steinberg DM, Seligshon U. Variable bleeding manifestations characterize different types of surgery in patients with severe factor xi deficiency enabling parsimonious use of replacement therapy. Haemophilia. 2006;12:490–493. doi: 10.1111/j.1365-2516.2006.01304.x. [DOI] [PubMed] [Google Scholar]
- 3.Seligsohn U. Factor xi deficiency in humans. J Thromb Haemost. 2009;(Suppl 1):84–87. doi: 10.1111/j.1538-7836.2009.03395.x. [DOI] [PubMed] [Google Scholar]
- 4.Bouma BN, Mosnier LO. Thrombin activatable fibrinolysis inhibitor (tafi) at the interface between coagulation and fibrinolysis. Pathophysiol Haemost Thromb. 2003;33:375–381. doi: 10.1159/000083832. [DOI] [PubMed] [Google Scholar]
- 5.Asakai R, Chung DW, Davie EW, Seligsohn U. Factor xi deficiency in ashkenazi jews in israel. N Engl J Med. 1991;325:153–158. doi: 10.1056/NEJM199107183250303. [DOI] [PubMed] [Google Scholar]
- 6.Dirkmann D, Hanke AA, Gorlinger K, Peters J. Perioperative use of modified thrombelastography in factor xi deficiency: A helpful method to assess drug effects. Acta Anaesthesiol Scand. 2007;51:640–643. doi: 10.1111/j.1399-6576.2007.01284.x. [DOI] [PubMed] [Google Scholar]
- 7.Peyvandi F, Lak M, Mannucci PM. Factor xi deficiency in iranians: Its clinical manifestations in comparison with those of classic hemophilia. Haematologica. 2002;87:512–514. [PubMed] [Google Scholar]
- 8.Shpilberg O, Peretz H, Zivelin A, Yatuv R, Chetrit A, Kulka T, et al. One of the two common mutations causing factor xi deficiency in ashkenazi jews (type ii) is also prevalent in iraqi jews, who represent the ancient gene pool of jews. Blood. 1995;85:429–432. [PubMed] [Google Scholar]
- 9.Kim SH, Choi JM, Kim HJ, Choi SS, Choi IC. Continuous noninvasive hemoglobin measurement is useful in patients undergoing double-jaw surgery. J Oral Maxillofac Surg. 2014;72:1813–1819. doi: 10.1016/j.joms.2014.03.011. [DOI] [PubMed] [Google Scholar]
- 10.Ilankovan V, Blesing NE, Moos KF, Davidson JF. Correction of facial deformities in patients with mild bleeding disorders: A report of three cases. Br J Oral Maxillofac Surg. 1990;28:398–400. doi: 10.1016/0266-4356(90)90038-m. [DOI] [PubMed] [Google Scholar]
- 11.Todd D, Galbraith D. Management of an orthognathic surgery patient with factor xi deficiency: Review and case report. J Oral Maxillofac Surg. 1993;51:417–420. doi: 10.1016/s0278-2391(10)80358-1. [DOI] [PubMed] [Google Scholar]
- 12.Abramowicz S, Staba SL, Dolwick MF, Chen DR. Orthognathic surgery in a patient with hemophilia a: Report of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:437–439. doi: 10.1016/j.tripleo.2007.07.041. [DOI] [PubMed] [Google Scholar]
- 13.Redondo M, Solenthaler M, Zeerleder S, Wuillemin WA. Isolated increased aPTT with anamnestic hemorrhagic diathesis--severe fxi deficiency. Ther Umsch. 1999;56:502–504. doi: 10.1024/0040-5930.56.9.502. [DOI] [PubMed] [Google Scholar]
- 14.Singh A, Harnett MJ, Connors JM, Camann WR. Factor xi deficiency and obstetrical anesthesia. Anesth Analg. 2009;108:1882–1885. doi: 10.1213/ane.0b013e3181a28715. [DOI] [PubMed] [Google Scholar]
- 15.Berliner S, Horowitz I, Martinowitz U, Brenner B, Seligsohn U. Dental surgery in patients with severe factor xi deficiency without plasma replacement. Blood Coagul Fibrinolysis. 1992;3:465–468. [PubMed] [Google Scholar]
- 16.Lawler P, White B, Pye S, Hermans C, Riddell A, Costello C, et al. Successful use of recombinant factor viia in a patient with inhibitor secondary to severe factor xi deficiency. Haemophilia. 2002;8:145–148. doi: 10.1046/j.1365-2516.2002.00590.x. [DOI] [PubMed] [Google Scholar]
- 17.Billon S, Le Niger C, Escoffre-Barbe M, Vicariot M, Abgrall JF. The use of recombinant factor viia (novoseven) in a patient with a factor xi deficiency and a circulating anticoagulant. Blood Coagul Fibrinolysis. 2001;12:551–553. doi: 10.1097/00001721-200110000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Bern MM, Sahud M, Zhukov O, Qu K, Mitchell W., Jr Treatment of factor xi inhibitor using recombinant activated factor viia. Haemophilia. 2005;11:20–25. doi: 10.1111/j.1365-2516.2005.01052.x. [DOI] [PubMed] [Google Scholar]
- 19.Faverani LP, Ramalho-Ferreira G, Fabris AL, Polo TO, Poli GH, Pastori CM, et al. Intraoperative blood loss and blood transfusion requirements in patients undergoing orthognathic surgery. Oral Maxillofac Surg. 2014;18:305–310. doi: 10.1007/s10006-013-0415-4. [DOI] [PubMed] [Google Scholar]
- 20.Pineiro-Aguilar A, Somoza-Martin M, Gandara-Rey JM, Garcia-Garcia A. Blood loss in orthognathic surgery: A systematic review. J Oral Maxillofac Surg. 2011;69:885–892. doi: 10.1016/j.joms.2010.07.019. [DOI] [PubMed] [Google Scholar]
- 21.Espahbod C, Veitz-Keenan A. Tranexamic acid reduces intraoperative blood loss in orthognathic surgery. Evid Based Dent. 2014;15:63. doi: 10.1038/sj.ebd.6401033. [DOI] [PubMed] [Google Scholar]
- 22.Whiting D, DiNardo JA. Teg and rotem: technology and clinical applications. Am J Hematol. 2014;89:228–232. doi: 10.1002/ajh.23599. [DOI] [PubMed] [Google Scholar]