Abstract
Atypical facial pain (AFP) is a type of facial pain which does not fulfill any other diagnosis. It has several features such as no objective signs, no obvious explanation of the cause and poor response to treatments. We report a case of a female patient with AFP on the left maxillary area. The pain was increased by cold innocuous stimulation and thermography showed that the temperature on the painful area was significantly decreased. The pain was successfully alleviated by stellate ganglion block (SGB). Therefore, SGB can be effectively used to treat AFP.
Keywords: Atypical facial pain, Stellate ganglion block, Thermography
Atypical facial pain (AFP) is continuous pain that does not have the property of cranial neuralgias and does not fulfill any other diagnosis. Several methods including medication, psychological and physical therapy, surgical procedure, and education are used to treat AFP. Among of these various therapeutic strategies, especially tricyclic antidepressant and anticonvulsant are widely used in the treatment of AFP. But these medications cannot completely eliminate AFP [1,2].
Sympathetic activity may generate pain under certain pathological conditions such as post-herpetic neuralgia, migraine, and complex regional pain syndromes [3,4,5]. Stellate ganglion block (SGB) is a selective sympathetic block that influences ipsilateral head, neck, and upper extremities. SGB increases the blood supply of head, neck, and upper extremities [6,7]. In addition, it has sedative effects and decreases the nociceptive response, subsequently resulting in pain relief [8,9].
We reported a case of a 51-year-old female patient presented with AFP, which was successfully alleviated by repeated SGB.
CASE REPORT
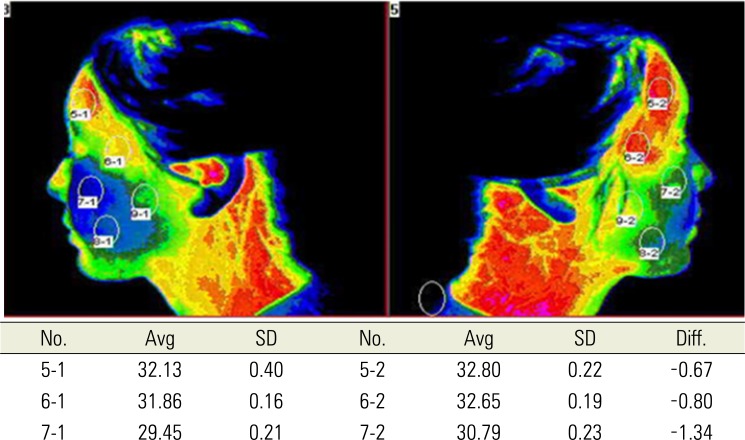
A 51-year-old female with four month history of a facial pain in left maxillary nerve innervated territory was referred to the department of anesthesiology and pain. There were not any initiating factors associated with this pain. She suffered from constant deep aching pain over the left maxillary area. Her pain intensity was 5-7 using visual analogue score (VAS: 0 = "no pain" and 10 = "worst pain imaginable"). There were no abnormalities in her imaging studies including X ray and MRI for head and face and blood laboratory examination such as erythrocyte sedimentation rate and C reactive protein. She was diagnosed with AFP syndrome by a dentist and tramadol 150 mg a day, imipramine 20 mg a day and pregabalin 300 mg a day were given. But these medications did not reduce the pain. Except her pain, physical examination showed no abnormal findings. The pain was increased by cold innocuous stimulation and we performed a thermograhic study on her face. The study revealed that the temperature was significantly lower in the left maxillary area than the right maxillary area (Fig. 1). Therefore, SGB was performed by injection of 6 ml of 1.5% lidocaine at the anterior aspect of the left 6th cervical transverse process. Two minutes after SGB ipsilateral Horner's syndrome developed and twenty minutes after SGB her pain intensity decreased to 1-2 on the VAS. We performed SGB 2-3 times a week. After the 12nd completion of SGB, her pain disappeared and she stopped medications. At 2 months follow-up, she continued to have no pain.
Fig. 1. Thermography showed that the temperature was significantly lower in the left maxillary area than the right maxillary area.
DISCUSSION
A diagnosis of AFP is made when patients present with symptoms that do not fulfill any criteria available. It has several features such as no objective signs, no obvious explanation of the cause and poor response to treatments. Psychogenic problems such as depression and anxiety were often associated with AFP. It is reported that AFP commonly occurs in middle aged or elderly females [10,11].
SGB is a selective sympathetic block that influences ipsilateral head, neck, and upper extremities. SGB help increase circulation and blood supply to the arm and are used to relieve vasospasm [12]. In addition, it has been used in treating various diseases such as post- herpetic neuralgia, migraine and complex regional pain syndromes [3,4,5]. Sympathetic activity may generate pain under certain pathological conditions. In sympathetically maintained pain cases, the receptors at the primary afferents can change and become sensitive to adrenergic substances such as norepinephrine [13,14]. It was reported that SGB is effective to reduce pain related to temporal arteritis and sympathetic maintained headache and orofacial pain [15,16]. Sympathetic block can improve blood flow by dilating vessels. In addition, sympathetic block may reduce pain by directly blocking afferent nociceptive signal traveling via sympathetic pathways [17]. Chronic stimulation of nociceptive system may lead to a demyelination and axonal dysfunction in addition to an overactivation of central sensory transmission. This could result in atypical chronic pain instead of a typical neuralgia [18]. Recently it was reported that SGB has selective effects in animal and human study. The sedative effects of SGB can be one of therapeutic actions for treating various pain disorders [8,9].
In this case, the pain is increased by cold innocuous stimulation and thermography showed that the temperature on the painful area was significantly decreased. And SGB successfully alleviated the atypical facial pain involving maxillary nerve territories.
In conclusion, SGB can be effectively used to treat AFP. Further research is needed to define its role in managing chronic pain conditions like AFP.
References
- 1.Sommer C. Patient careers. Facial pain and neuralgias. Schmerz. 2004;18:385–391. doi: 10.1007/s00482-004-0343-1. [DOI] [PubMed] [Google Scholar]
- 2.Sardella A, Demarosi F, Barbieri C, Lodi G. An up-to-date view on persistent idiopathic facial pain. Minerva Stomatol. 2009;58:289–299. [PubMed] [Google Scholar]
- 3.Currey TA, Dalsania J. Treatment for herpes zoster ophthalmicus: stellate ganglion block as a treatment for acute pain and prevention of postherpetic neuralgia. Ann Ophthalmol. 1991;23:188–189. [PubMed] [Google Scholar]
- 4.Ullrich J. Stellate ganglion block under EEG control in the treatment of complicated cervical migraine. J Neurol. 1975;209:301–306. doi: 10.1007/BF00314370. [DOI] [PubMed] [Google Scholar]
- 5.Owen-Falkenberg A, Olsen KS. Continuous stellate ganglion blockade for reflex sympathetic dystrophy. Anesth Analg. 1992;75:1041–1042. doi: 10.1213/00000539-199212000-00032. [DOI] [PubMed] [Google Scholar]
- 6.Wang QX, Wang XY, Fu NA, Liu JY, Yao SL. Stellate ganglion block inhibits formalin-induced nociceptive responses: mechanism of action. Eur J Anaesthesiol. 2005;22:913–918. doi: 10.1017/S0265021505001559. [DOI] [PubMed] [Google Scholar]
- 7.Salvaggio I, Adducci E, Dell'Aquila L, Rinaldi S, Marini M, Zappia L, et al. Facial pain: a possible therapy with stellate ganglion block. Pain Med. 2008;9:958–962. doi: 10.1111/j.1526-4637.2008.00515.x. [DOI] [PubMed] [Google Scholar]
- 8.Jeong S, Jeon Y, Yeo J, Baek W. The effects of stellate ganglion block on the electroencephalogram in rats. J Anesth. 2014;28:601–605. doi: 10.1007/s00540-013-1780-8. [DOI] [PubMed] [Google Scholar]
- 9.Yeo J, Jeon Y. Effects of stellate ganglion block on sedation as assessed by bispectral index in normal healthy volunteers. Pain Physician. 2015;18:173–178. [PubMed] [Google Scholar]
- 10.Madland G, Feinmann C. Chronic facial pain: a multidisciplinary problem. J Neurol Neurosurg Psychiatry. 2001;71:716–719. doi: 10.1136/jnnp.71.6.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hentschel K, Capobianco DJ, Dodick DW. Facial pain. Neurologist. 2005;11:244–249. doi: 10.1097/01.nrl.0000164816.56936.71. [DOI] [PubMed] [Google Scholar]
- 12.Bindra A, Prabhakar H, Singh GP. Stellate ganglion block for relieving vasospasms after coil embolization of basilar tip aneurysms. J Neurosurg Anesthesiol. 2011;4:379. doi: 10.1097/ANA.0b013e31823122e1. [DOI] [PubMed] [Google Scholar]
- 13.Rubin G, Kaspi T, Rappaport ZH, Cohen S, Ravikovitch M, Lomazov P, et al. Adrenosensitivity of injured afferent neurons does not require the presence of postganglionic sympathetic terminals. Pain. 1997;72:183–191. doi: 10.1016/s0304-3959(97)00036-5. [DOI] [PubMed] [Google Scholar]
- 14.Pertovaara A. Noradrenergic pain modulation. Prog Neurobiol. 2006;80:53–83. doi: 10.1016/j.pneurobio.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 15.Noma N, Kamo H, Nakaya Y, Dezawa K, Young A, Khan J, et al. Stellate ganglion block as an early intervention in sympathetically maintained headache and orofacial pain caused by temporal arteritis. Pain Med. 2013;14:392–397. doi: 10.1111/pme.12040. [DOI] [PubMed] [Google Scholar]
- 16.Jeon Y, Kim JH. Treatment of atypical facial pain with stellate ganglion block. J Korean Dent Soc Anesthesiol. 2014;14:173–175. [Google Scholar]
- 17.Meng ID, Cao L. From migraine to chronic daily headache: The biological basis of headache transformation. Headache. 2007;47:1251–1258. doi: 10.1111/j.1526-4610.2007.00907.x. [DOI] [PubMed] [Google Scholar]
- 18.Obermann M, Yoon MS, Ese D, Maschke M, Kaube H, Diener HC, et al. Impaired trigeminal nociceptive processing in patients with trigeminal neuralgia. Neurology. 2007;69:835–841. doi: 10.1212/01.wnl.0000269670.30045.6b. [DOI] [PubMed] [Google Scholar]