Abstract
Background
Surgery on the lower impacted third molar usually involves trauma in the highly vascularized loose connective tissue area, leading to inflammatory sequelae including postoperative pain, swelling, and general oral dysfunction during the immediate post-operative phase. This study aimed to investigate the effectiveness of preoperative injection of a single dose of 8 mg dexamethasone for postoperative pain control in lower third molar surgery.
Methods
A controlled, randomized, split-mouth, prospective study involving lower third molar surgery was performed in 31 patients. The randomized sampling group was preoperatively injected, after local anesthesia, with a single dose of dexamethasone (8 mg in 2 ml) through the pterygomandibular space; 2 ml of normal saline (with no dexamethasone) was injected as a placebo.
Results
The pain VAS score was significantly different on the day of the operation compared to the first post-operative day (P = 0.00 and 0.01, respectively), but it was not significantly different on the third and seventh postoperative day between the control and study groups. There was a significant reduction in swelling on the second postoperative day, and a difference between the second postoperative day and baseline value in the study group (P < 0.05). Trismus was highly significantly different on the second postoperative day and between baseline and second postoperative day between the groups (P = 0.04 and 0.02, respectively). Descriptive statistics and independent-samples t- test were used to assess the significance of differences.
Conclusions
Injection of 8 mg dexamethasone into the pterygomandibular space effectively reduced the postoperative pain and other postoperative sequalae.
Keywords: Dexamethasone injection, Impacted tooth, Lower third molar surgery, Postoperative pain, Postoperative sequelae, Pterygomandibular space, Single dose
INTRODUCTION
Lower third molar removal is a common oral surgical practice performed by oral and maxillofacial surgeons [1]. The procedure can cause trauma to the highly vascularized loose connective tissue area, and may cause acute inflammation with intense discomfort, as well as pain during the immediate post-operative phase [2]. Postoperative pain is a subjective sensation, and depends on various factors such as patient age, sex, anxiety, and surgical difficulty [3]. The pterygomandibular space is highly vascular with loose areolar tissue, and is one of the spaces related to the lower third molar region. Trismus is one of the clinical symptoms of pterygomandibular space infection [4,5]. With good surgical technique, gentle manipulation of the tissue and analgesic administration after surgery can reduce postoperative side effects, although pain is not controlled completely in most cases [6,1].
Corticosteroids have potent anti-inflammatory activity, and have been used at different dosages and through various routes of administration to lessen the inflammatory effects of third molar surgical removal [3,7].
Glucocorticoids act at every step in the inflammatory process to decrease circulating lymphocytes, inhibit capillary dilatation and fibroblast proliferation, and alter prostaglandins and leukotrienes synthesis. As the suppression of these factors exerts a profound effect on tissue inflammation, corticosteroids are used in surgical procedures to reduce the acute inflammatory conditions that occur postoperatively [8]. Acute inflammation induced by tissue damage plays a major role in development of postoperative pain. Moreover, locally applied glucocorticoids have a direct inhibitory effect on signal transmission in nociceptive C-fibers and ectopic neuroma discharge in injured nerves [9].
By virtue of its potential anti-inflammatory effects, dexamethasone is useful in lowering pain, and is currently the most powerful anti-inflammatory drug, with a long half-life. Dexamethasone is considered safe for periods shorter than two weeks even in amounts above physiological doses [6,10,11,12]. Previous studies have shown that the perioperative use of corticosteroids reduces postoperative discomfort after removal of impacted mandibular third molars [12,13].
The effectiveness of dexamethasone on postoperative pain, swelling, and trismus seems to depend on the dose of the drug. Dionne et al. [14] found that administration of 4 mg of dexamethasone via the intravenous route one hour before the operation, in conjunction with administration of 4 mg of the drug via the oral route 12 hours after third molar surgery exerts a sufficient inhibitory effect on prostaglandin E2 (PGE2), and can in turn curtail the induction of analgesia.
The study showed that dexamethasone injection before the operation may not be required in all lower third molar surgeries, but is indicated for difficult cases [11,15]. Longer operations are typically associated with more pain, and the intensity of pain may increase with the difficulty of the operation [3].
The postoperative experience of pain depends on the degree of surgical trauma suffered, requirement for bone tissue removal, and the extension of the periosteum. The role of corticosteroids in preventing postoperative pain is controversial. Corticosteroids are employed particularly after surgery to limit the accumulation of inflammatory mediators and reduce fluid transudation and edema [3,13,16].
A previous study noted that the swelling made the tissue tense and caused intense pain that was decreased when dexamethasone was used to reduce the facial swelling [17]. Another study also described trismus as a direct result of postoperative swelling that causes compression of the nervous structures [18].
The rate of absorption of a drug largely depends on the blood flow in the area of administration [19]. The pterygomandibular space is a highly vascular and loose areolar tissue space adjacent to the operation area. Therefore, we chose this space as the site of drug injection in order to get better absorption.
The aim of this study was to investigate the efficacy of a single dose of 8 mg dexamethasone, injected preoperatively into the pterygomandibular space, for the control of postoperative pain and other sequalae in lower third molar surgery.
MATERIALS AND METHODS
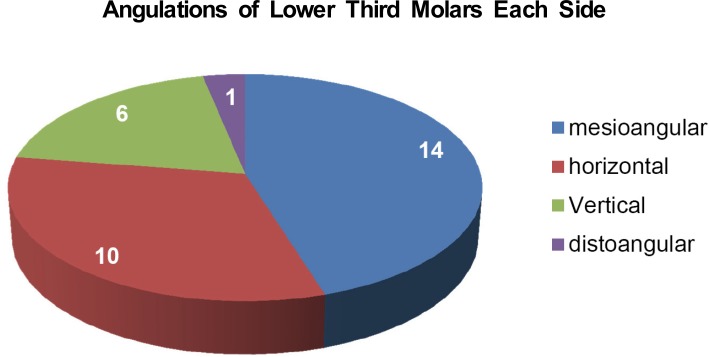
A controlled randomized, prospective, split-mouth study was done at the Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Mahidol University, and approved by The Mahidol University Institutional Review Board (MU-IRB), with COA No. MU-DT/PY-IRB 2016/021.2303. This study involved 62 lower third molar operations in 31 patients, performed under local anesthesia (Table 1 and Fig. 1). The difficulty of lower third molar surgery was evaluated according to the Pell-Gregory classification [20].
Table 1. Type of lower third molar in the patients of this study.
| Position Class | A | B | C | Total (%) |
|---|---|---|---|---|
| I | 3 | 9 | - | 12 (38.71) |
| II | 1 | 15 | 3 | 19 (61.29) |
| III | - | - | - | - |
| Total (%) | 4 (12.90) | 24 (77.42) | 3 (9.68) | 31 (100) |
Fig. 1. The angulations of lower third molars in this study.
The patients had similarly bilateral lower third molar, so we randomly divided each side into two groups. Thus, the study group received 8 mg of dexamethasone (4 mg/ml in 2 ml), injected preoperatively through the pterygomandibular space after local anesthesia, whereas the control group received 2 ml of normal saline, also injected preoperatively through the pterygomandibular space after local anesthesia.
Of the 31 patients who participated in this study, 11 were male (22 operations: 35.48%), 20 were female (40 operations: 64.51%) with mean age 22 (age range 16 to 32) years. The patients were blinded to the use of dexamethasone, and all procedures were performed by the same surgeon.
The standard surgical technique of lower third molars surgery was done under local anesthesia with 4% articaine hydrochloride with 1:100,000 epinephrine for inferior alveolar nerve block and long buccal nerve block. All the patients received amoxicillin (500 mg) at intervals of 8 hours for 7 days, and acetaminophen (500 mg) for pain every 6 hours as needed.
1. Pain evaluation
For pain evaluation, all patients were given a form to record visual analog scale (VAS) scores and the number of analgesic drugs taken. VAS scores were collected on the day of operation, and on the first, third and seventh day after surgery. The number of drug tablets taken was collected every day starting from the day of operation.
2. Postoperative sequalae
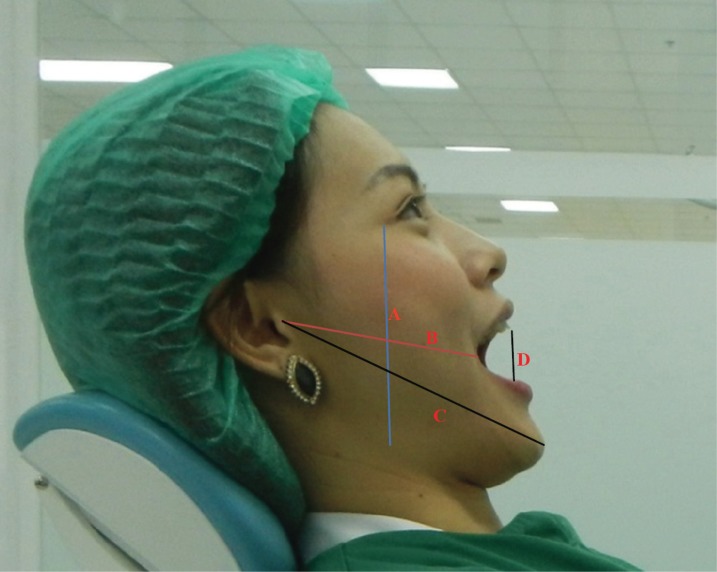
Facial swelling and trismus measurements were done prior to the operation and on the second and seventh days after surgery. Three measurements for gonion angle-lateral canthal of the eye (Fig. 2A), tragus-commissure of the mouth (Fig. 2B), and tragus-pogonium (Fig. 2C) were taken to assess facial swelling. We evaluated trismus by maximum inter-incisal distance (MID) (Fig. 2D), which is the distance between the upper and lower incisal edge of central incisors (Fig. 2).
Fig. 2. Facial swelling and trismus measurements. A: Gonion angle-lateral canthal of eye; B: Tragus-commissure of mouth; C: Tragus-pogonium; D: Maximum inter-incisal distance (MID).
The data were coded and entered into the Microsoft excel spreadsheet. The Statistical Package for the Social Sciences (SPSS version 22, SPSS Inc., USA) was used to calculate the significance of differences between the study and placebo groups. Descriptive statistical parameters (mean, standard deviation, and independent-samples t-test) were used to assess the significance of difference. P < 0.05 was considered significant.
RESULTS
A total of 62 lower third molar removals involving 31 operations in the dexamethasone group and control non-dexamethasone group were performed. Operation times were 22.8 min for the dexamethasone group and 21.5 min for the control (non-dexamethasone) group. There was no significant difference (P-value 0.3) in operation times between both groups.
There was no postoperative infection. Only a case of lower lip paresthesia was found in the dexamethasone group, but it resolved two weeks after the operation. No other complications were found in both control and study groups.
Pain VAS scores were significantly different on operation day and after the first day of the operation (P = 0.00 and 0.01, respectively), but there was no significant difference in VAS scores control and study groups on the third and seventh day after surgery. However, the use of analgesic drugs for pain was significantly different between control and study groups during the first 3 days after surgery. In this study, we considered a pain VAS score of 20 mm as representing a turning point for transforming mild pain. The number of day required for transforming mild pain was significantly different between the two groups (Table 2).
Table 2. Measurements of pain (VAS and number of analgesic taken) in study groups.
| Evaluation day | Study group (SD) | Control group (SD) | P-value | |
|---|---|---|---|---|
| Pain VAS scores | Operation day | 25.3 (23.1) | 51.5 (29.1) | 0.00* |
| First postop day | 18.6 (17.2) | 35.39 (24.89) | 0.01* | |
| Third postop day | 14.2 (17.3) | 23.3 (24.6) | 0.1 | |
| Seventh postop day | 4.71 (11.43) | 11.47 (17.20) | 0.07 | |
| P-value | 0.00* | 0.00* | ||
| Day of reaching mild pain (20 mm) | 1.8 (2.6) | 3.8 (2.8) | 0.01* | |
| Number | First postop day | 1.9 (1.3) | 2.9 (1.7) | 0.01* |
| Analgesic taken | Second postop day | 2.0 (1.7) | 3.5 (1.8) | 0.01* |
| Third postop day | 1.3 (1.5) | 2.7 (2.2) | 0.01* | |
| P-value | 0.93 | 0.01* | ||
There was significant reduction in the magnitude of swelling on the second postoperative day. There was also a difference on second postoperative day and baseline in the study group compared with control group (Table 3). On the second day after the operation, differences in the measurements of trismus were highly significant between control and study groups (P = 0.04 and 0.02, respectively) (Table 4).
Table 3. Measurements of swelling and differences from preoperative day in study groups.
| Position measurement | Evaluation day | Study group (SD) | Control group (SD) | P-value |
|---|---|---|---|---|
| Gn-Lc | Preoperative day (baseline) | 111.8 (6.4) | 111.6 (7.9) | 0.88 |
| Second postop day | 115.4 (6.4) | 119.6 (6.7) | 0.01* | |
| Seventh postop day | 112.8 (6.0) | 114.8 (6.3) | 0.20 | |
| P-value | 0.00* | 0.00* | ||
| Differences | ||||
| Second postop day to Preoperative day | 3.6 (3.2) | 8.0 (6.3) | 0.00* | |
| Seventh postop day to Preoperative day | 0.9 (1.7) | 3.3 (4.6) | 0.01* | |
| Tr-Com | Preoperative day (baseline) | 116.9 (5.7) | 117.6 (6.6) | 0.7 |
| Second postop day | 120.9 (5.4) | 124.6 (6.8) | 0.0* | |
| Seventh postop day | 118.9 (4.9) | 119.7 (6.8) | 0.6 | |
| P-value | 0.32 | 0.00* | ||
| Differences | ||||
| Second postop day to Preoperative day | 3.9 (3.7) | 6.6 (4.6) | 0.02* | |
| Seventh postop day to Preoperative day | 1.9 (3.3) | 2.1 (3.2) | 0.88 | |
| Tr-Pog | Preoperative day (baseline) | 152.0 (10.3) | 151.2 (12.7) | 0.77 |
| Second postop day | 155.8 (10.3) | 159.1 (10.2) | 0.22 | |
| Seventh postop day | 153.3 (9.9) | 153.9 (10.4) | 0.81 | |
| P-value | 0.04* | 0.02* | ||
| Differences | ||||
| Second postop day to Preoperative day | 3.8 (2.7) | 7.9 (9.3) | 0.02* | |
| Seventh postop day to Preoperative day | 1.3 (1.7) | 2.8 (9.4) | 0.39 |
Gn-Lc = goial angle-lateral canthal of eye, Tr-Com = tragus-commissure of mouth, Tr-Pog = Tragus-Pogonion
Table 4. Measurements of trismus and differences frompre-operative day in the study groups.
| MID | Study group (SD) | Control group (SD) | P-value |
|---|---|---|---|
| Preoperative day (baseline) | 43.9 (5.9) | 43.4 (5.9) | 0.70 |
| Second postop day | 33.2 (8.9) | 28.3 (9.4) | 0.04* |
| Seventh postop day | 40.4 (8.1) | 38.8 (8.6) | 0.44 |
| P-value | 0000.28 | 0.04* | |
| Differences of MID | |||
| Preoperative to Second postop day | 10.8 (6.6) | 15.0 (7.2) | 0.02* |
| Preoperative to Seventh postop day | 3.5 (5.5) | 4.6 (4.9) | 0.42 |
MID: maximum inter-incisal distances.
DISCUSSION
By virtue of its potential anti-inflammatory effects, dexamethasone is useful for lowering pain and is currently used in surgical procedures to reduce the acute inflammatory conditions that occur postoperatively [8]. Acute inflammation induced by tissue damage plays a major role in development of postoperative pain [9]. Dexamethasone has a long half-life, and is the most powerful anti-inflammatory drug whose administration is considered safe for periods shorter than two weeks [6,10,11,12]. Previous studies have shown that the perioperative use of corticosteroids reduces postoperative discomfort after removal of impacted mandibular third molars [12,13].
In this study, we found that preoperative injection of 8 mg of dexamethasone into the pterygomandibular space after local anesthesia resulted in a significant reduction of postoperative pain compared to control, non-dexamethasone study.
Increase in operation time is typically associated with more pain, and the difficulty of the operation may increase pain [3]. The operation times in this study were not significantly different between both groups because of the type of impacted lower third molar, and the bilateral split-mouth study design whereby the same position was used, and the same operator performed surgery for all cases.
In this study, there was only one case of lower lip paresthesia in the test group, which was attributed to the deep position of the impacted lower third molar and surgical trauma; however, it was resolved within the second week after the operation.
Dionne et al. [14] found that administration of 4 mg of dexamethasone via the intravenous route one hour before the operation, in conjunction with administration of 4 mg of the drug via the oral route 12 hours after third molar surgery, could relieve the induction of analgesia. In this study, we used 8 mg of dexamethasone injection pre-operation.
This study required bone removal in all the cases, and tooth separation in some cases; therefore, overall the study can be characterized as being associated with only moderate technical difficulties.
The pterygomandibular space is a highly vascular and loose areolar tissue space adjacent to the operation area. We therefore chose this space as the site of drug injection in order to get better absorption. The injection technique used in this study was similar to the inferior alveolar nerve block, which is routinely used in dental practice.
Depending on the degree of surgical trauma suffered, the requirement for bone tissue removal and the extension of the periosteum reduced the postoperative pain. In this study, the mean value of pain VAS scores was lower in the study group compared with the control group at all postoperative evaluations. The role of corticosteroids in preventing postoperative pain is controversial.
Corticosteroids are employed particularly after surgery to limit the accumulation of inflammatory mediators and reduce fluid transudation and edema [3,13,16]. In this study, the mean values for postoperative swelling were significantly lower in the study group compared to control group, especially on the second day after surgery. The mean difference in swelling on the second postoperative day versus the pre-operation baseline swelling was also significantly lower in the study group. A previous study stated that the swelling made the tissue tense and caused intense pain that was reduced when dexamethasone was used to decrease facial swelling [17].
Another study also reported that trismus may be a direct consequence of postoperative swelling that then compresses the nervous structures [18]. In that study, better results were obtained in the trismus group compared to the control group, especially on the second postoperative day, and no difference in the mean value before operation and on the second day after surgery (P = 0.04 and 0.02, respectively). Therefore, trismus seemed to follow the postoperative swelling.
In our study, significantly reduced pain scores were noted in the study group on the first postoperative day and on the second postoperative day (P-values of 0.00 and 0.01), respectively. Fewer analgesic drugs were consumed, and the mild pain score (20 mm) was reached faster in the dexamethasone group of this study. Others have reported significant pain reduction in 4-6 hours postoperatively, but not later [21,22]. However, some studies have reported a reduction in pain 6 hours after extraction and during the subsequent 3 days [12,23]. Therefore, this may be the reason for the significant reduction in pain on the operative day and on the second postoperative day. Others have also stated reported that steroids can reduce the effect of analgesics taken after surgical removal of the lower third molar [11,24], consistent with our findings. However, others have found the anti-analgesic effect of corticosteroids to lack statistical significance (P > 0.05), despite a reduction in postoperative pain [14,21]. Furthermore, some studies have suggested that the possibility that corticosteroid treatment can increase patient reaction to pain, secondary to a suppression of endorphin β levels [3]. Nevertheless, many studies have reported statistically significant analgesic action with simultaneous corticosteroid use [21,25,26].
A number of authors have reported a statistically significant reduction (P < 0.05) in pain after the postoperative administration of corticosteroids [22,27]. De Oliveria Jr et al. [28] suggested that preoperative administration of the drug provides a greater effect on postoperative pain. In the current study, dexamethasone was injected after local anesthesia but before the operation in order to get the maximum benefit from an early onset of drug action.
In conclusion, a single dose injection of 8 mg of dexamethasone into the pterygomandibular space was effective at reducing postoperative pain. Injection into this pterygomandibular space is convenient and is familiar to dental practitioners. Because the pterygomandibular space comprises loose areolar tissue, has high vascularity, and is adjacent to the operation area, injection of the drug into this space after local anesthesia ensures better absorption of the drug and is associated with no pain to patients. Preoperative injection of dexamethasone has better results than postoperative injection because of the fast onset of drug action. Therefore, we propose that dexamethasone injection, unless contraindicated, is the drug of choice for pain control during surgical removal of the lower third molar.
Acknowledgements
The authors would like to thank the staff and dental assistants in the Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Mahidol University.
Footnotes
Funding: Mahidol University Fund
Ethics Approval: This study was approved by The Mahidol University Institutional Review Board (MU-IRB) with COA No. MU-DT/PY-IRB 2016/021.2303.
References
- 1.Susarla SM, Blaeser BF, Magalnick D. Third molar surgery and associated complications. Oral Maxillofac Surg Clin North Am. 2003;15:177–186. doi: 10.1016/S1042-3699(02)00102-4. [DOI] [PubMed] [Google Scholar]
- 2.Majid OW, Mahmood WK. Use of dexamethasone to minimise post-operative sequelae after third molar surgery: comparison of five different routes of administration. Oral Surg. 2013;6:200–208. [Google Scholar]
- 3.Ata-Ali J, Ata-Ali F, Peñarrocha-Oltra D, Peñarrocha M. Corticosteroids use in controlling pain, swelling and trismus after lower third molar surgery. J Clin Exp Dent. 2011;3:e469–e475. [Google Scholar]
- 4.Antunes AA, Avelar RL, Martins Neto EC, Frota R, Dias E. Effect of two routes of administration of dexamethasone on pain, edema, and trismus in impacted lower third molar surgery. Oral Maxillofac Surg. 2011;15:217–223. doi: 10.1007/s10006-011-0290-9. [DOI] [PubMed] [Google Scholar]
- 5.Khoury JN, Mihailidis S, Ghabriel M, Townsend G. Applied anatomy of the pterygomandibular space: improving the success of inferior alveolar nerve blocks. Aust Dent J. 2011;56:112–121. doi: 10.1111/j.1834-7819.2011.01312.x. [DOI] [PubMed] [Google Scholar]
- 6.Mohtadi A, Nesioonpour S, Salari A, Akhondzadeh R, Masood Rad B, Aslani SM. The effect of single-dose administration of dexamethasone on postoperative pain in patients undergoing laparoscopic cholecystectomy. Anesth Pain Med. 2014;4:e17872. doi: 10.5812/aapm.17872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gozali P, Kiattavornchareon S, Wu M, Wongsirichat N, Suphangul S. Betamethasone and methylprednisolone usage in lower third molar surgery: Review literature. M Dent J. 2015;35:273–280. [Google Scholar]
- 8.Vyas N, Agarwal S, Shah N, Patel D, Aapaliya P. Effect of single dose intramuscular methylprednisolone injection into the masseter muscle on the surgical extraction of impacted lower third molars: a randomized controlled trial. Kathmandu Univ Med J (KUMJ) 2014;12:4–8. doi: 10.3126/kumj.v12i1.13625. [DOI] [PubMed] [Google Scholar]
- 9.Holte K, Kehlet H. Perioperative single dose glucocorticoid administration: Pathophysiologic effects and clinical implications. J Am Coll Surg. 2002;195:694–712. doi: 10.1016/s1072-7515(02)01491-6. [DOI] [PubMed] [Google Scholar]
- 10.Blondeau F, Daniel NG. Extraction of impacted mandibular third molars: postoperative complications and their risk factors. J Can Dent Assoc. 2007;73:325. [PubMed] [Google Scholar]
- 11.Esen E, Tasar F, Akhan O. Determination of the anti-inflammatory effects of methylprednisolone on the sequelae of third molar surgery. J Oral Maxillofac Surg. 1999;57:1201–1206. doi: 10.1016/s0278-2391(99)90486-x. [DOI] [PubMed] [Google Scholar]
- 12.Montgomery MT, Hogg JP, Roberts DL, Redding SW. The use of glucocorticosteroids to lessen the inflammatory sequelae following third molar surgery. J Oral Maxillofac Surg. 1990;48:179–187. doi: 10.1016/s0278-2391(10)80207-1. [DOI] [PubMed] [Google Scholar]
- 13.Alexander RE, Throndson RR. A review of perioperative corticosteroid use in dentoalveolar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:406–415. doi: 10.1067/moe.2000.109778. [DOI] [PubMed] [Google Scholar]
- 14.Dionne RA, Gordon SM, Rowan J, Kent A, Brahim JS. Dexamethasone suppresses peripheral prostanoid levels without analgesia in a clinical model of acute inflammation. J Oral Maxillofac Surg. 2003;61:997–1003. doi: 10.1016/s0278-2391(03)00310-0. [DOI] [PubMed] [Google Scholar]
- 15.Capuzzi P, Montebugnoli L, Vaccaro MA. Extraction of impacted third molars.A longitudinal prospective study on factors that affect postoperative recovery. Oral Surg Oral Med Oral Pathol. 1994;77:341–343. doi: 10.1016/0030-4220(94)90194-5. [DOI] [PubMed] [Google Scholar]
- 16.Wakeling HG, Barry PC, Butler PJ. Postoperative analgesia in dental day case surgery. A comparison between Feldene "melt" (Piroxicam) and diclofenac suppositories. Anaesthesia. 1996;51:784–786. doi: 10.1111/j.1365-2044.1996.tb07898.x. [DOI] [PubMed] [Google Scholar]
- 17.Laureano Filho JR, Maurette PE, Allais M, Cotinho M, Fernandes C. Clinical comparative study of the effectiveness of two dosages of Dexamethasone to control postoperative Clinical swelling, trismus and pain after the surgical extraction of mandibular impacted third molars. Med Oral Patol Oral Cir Bucal. 2008;13:E129–E132. [PubMed] [Google Scholar]
- 18.Klongnoi B, Kaewpradub P, Boonsiriseth K, Wongsirichat N. Effect of single dose preoperative intramuscular dexamethasone injection on lower impacted third molar surgery. Int J Oral Maxillofac Surg. 2012;41:376–379. doi: 10.1016/j.ijom.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 19.Kim K, Brar P, Jakubowski J, Kaltman S, Lopez E. The use of corticosteroids and nonsteroidal anti-inflammatory medication for the management of pain and inflammation after third molar surgery: a review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:630–640. doi: 10.1016/j.tripleo.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 20.Latt MM, Chewpreecha P, Wongsirichat N. Prediction of difficulty in impacted lower third molar extraction: Review literature. M Dent J. 2015;35:281–290. [Google Scholar]
- 21.Üstün Y, Erdogan Ö, Esen E, Karsli ED. Comparison of the effects of 2 doses of methylprednisolone on pain, swelling and trismus after third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:535–539. doi: 10.1016/S1079210403004645. [DOI] [PubMed] [Google Scholar]
- 22.Mico-Llorens JM, Satorres-Nieto M, Gargallo-Albiol J, ArnabatDomınguez J, Berini-Aytes L, Gay-Escoda C. Efficacy of methylprednisolone in controlling complications after impacted lower third molar surgical extraction. Eur J Clin Pharmacol. 2006;62:693–698. doi: 10.1007/s00228-006-0164-5. [DOI] [PubMed] [Google Scholar]
- 23.Baxendale BR, Vater M, Lavery KM. Dexamethasone reduces pain and swelling following extraction of third molar teeth. Anaesthesia. 1993;48:961–964. doi: 10.1111/j.1365-2044.1993.tb07474.x. [DOI] [PubMed] [Google Scholar]
- 24.Vegas-Bustamante E, Mico-Llorens J, Gargallo-Albiol J, Satorres-Nieto M, Berini-Aytes L, Gay-Escoda C. Efficacy of methylprednisolone injected into the masseter muscle following the surgical extraction of impacted lower third molars. Int J Oral Maxillofac Surg. 2008;37:260–263. doi: 10.1016/j.ijom.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 25.Gersema L, Baker K. Use of corticosteroids in oral surgery. J Oral Maxillofac Surg. 1992;50:270–277. doi: 10.1016/0278-2391(92)90325-t. [DOI] [PubMed] [Google Scholar]
- 26.Zandi M. Comparison of corticosteroids and rubber drain for reduction of sequelae after third molar surgery. Oral Maxillofac Surg. 2008;12:29–33. doi: 10.1007/s10006-008-0096-6. [DOI] [PubMed] [Google Scholar]
- 27.Buyukkurt MC, Gungormus M, Kaya O. The effect of a single dose prednisolone with and without diclofenac on pain, trismus, and swelling after removal of mandibular third molars. J Oral Maxillofac Surg. 2006;64:1761–1766. doi: 10.1016/j.joms.2005.11.107. [DOI] [PubMed] [Google Scholar]
- 28.De Oliveira GS, Jr, Almeida MD, Benzon HT, McCarthy RJ. Perioperative Single Dose Systemic Dexamethasone for Postoperative Pain. Anesthesiology. 2011;115:575–588. doi: 10.1097/ALN.0b013e31822a24c2. [DOI] [PubMed] [Google Scholar]