Abstract
Background
The ideal alternative airway device should be intuitive to use, yielding proficiency after only a few trials. The Clarus Video System (CVS) is a novel optical stylet with a semi-rigid tip; however, the learning curve and associated orodental trauma are poorly understood.
Methods
Two novice practitioners with no CVS experience performed 30 intubations each. Each trial was divided into learning (first 10 intubations) and standard phases (remaining 20 intubations). Total time to achieve successful intubation, number of intubation attempts, ease of use, and orodental trauma were recorded.
Results
Intubation was successful in all patients. In 51 patients (85%), intubation was accomplished in the first attempt. Nine patients required two or three intubation attempts; six were with the first 10 patients. Learning and standard phases differed significantly in terms of success at first attempt, number of attempts, and intubation time (70% vs. 93%, 1.4 ± 0.7 vs. 1.1 ± 0.3, and 71.4 ± 92.3 s vs. 24.6 ± 21.9 s, respectively). The first five patients required longer intubation times than the subsequent five patients (106.8 ± 120.3 s vs. 36.0 ± 26.8 s); however, the number of attempts was similar. Sequential subgroups of five patients in the standard phase did not differ in the number of attempts or intubation time. Dental trauma, lip laceration, or mucosal bleeding were absent.
Conclusions
Ten intubations are sufficient to learn CVS utilization properly without causing any orodental trauma. A relatively small number of experiences are required in the learning curve compared with other devices.
Keywords: Education, Intubation, Learning curve, Orodental trauma
INTRODUCTION
An essential aspect of critical care is the ability to secure the airways of different types of patients. Sometimes practitioners encounter patients who require an alternative airway device rather than a conventional laryngoscope. Successful intubation in these patients depends on the selection of the most appropriate airway device and the practitioner's ability to use the device properly. In the last few decades, many alternative airway devices have been developed. Most practitioners are unlikely to become proficient in all of these devices given the time constraints. Since the degree of training and familiarity with the device is important for successful airway management, the ideal alternative airway device should be intuitive to use, therefore allowing the practitioner to gain expertise after only a few trials [1,2]. The Clarus Video System (CVS; Clarus Medical, Minneapolis, MN, USA) is a recently introduced optical stylet that is equipped with a semi-rigid tip and an on-board monitor. Owing to its distinctive semi-rigid tip, it does not require alignment of the oral-pharyngealtracheal axes or neck extension. Several studies have shown that it is effective in both normal and difficult airway situations [3,4,5,6], and that it is useful in various clinical settings [5,7,8,9]. Although the CVS has the potential to be an ideal alternative airway device, the learning curve is not clear. Therefore, the aim of this study was to evaluate the CVS learning curve of inexperienced practitioners.
METHODS
Our Institutional Review Board approved this study and written informed consent was obtained from each participating patient. All consecutive patients between the ages of 21 and 65 years who had an American Society of Anesthesiology Physical Status of I or II, and who were scheduled for elective surgery that required tracheal intubation between May 2012 and July 2012, were included in this study. Patients with a known history of difficult intubation, a small mouth (< 3.5 cm when open), a Mallampati score of ≥ 3, a body mass index of > 30, and/or an increased risk of gastric aspiration were excluded.
Two novice practitioners (A and B) performed the endotracheal intubations. Neither had any previous experience in CVS or other types of alternative airway device utilization, although both had at least 1 year of experience in anesthesia.
Standard monitoring techniques, including electrocardiography, non-invasive blood pressure, and pulse oximetry, were applied. Prior to inducing anesthesia, the Mallampati score, maximal inter-incisor distance, and thyromental distance were assessed with the patient in the sitting position, with the mouth opened as wide as possible, and the neck extended. Following preoxygenation with 100% oxygen for 3 min, anesthesia was induced with propofol 2 mg/kg and sevoflurane 4 vol%. After securing adequate mask ventilation, rocuronium 0.6 mg/kg was administered intravenously. Full neuromuscular blockage was confirmed with a nerve stimulator by train-of-four. Endotracheal intubation was attempted using the CVS with a preloaded endotracheal tube (7.5 mm internal diameter for women and 8.0 mm internal diameter for men). The chin-and-tongue lift maneuver by the operator was allowed during the procedure [6]. External airway manipulation, such as the backward, upward, and right-sided pressure maneuvers, or the modified jaw thrust maneuver by an assistant, was not permitted [10]. When the tip of the CVS was inserted into the mouth and once the epiglottis was visible, the tip was threaded under the epiglottis. The tip of the CVS was carefully advanced into the glottic aperture with direct visualization of the vocal cords, after which the operator slid the endotracheal tube into the trachea. The intubation time was defined as the time from opening the patient's mouth to the time the position of the endotracheal tube was confirmed by capnography. Three intubation attempts were allowed for each patient. An attempt was stopped if the intubation time exceeded 3 min or if arterial desaturation (SpO2 < 90%) developed before intubation could be accomplished. When an intubation attempt failed, the airway was managed with an appropriate method by an attending anesthesiologist and the reason for the failure was noted. The time required for intermittent mask ventilation between the individual attempts was subtracted from the total time. Total time to successful intubation, the number of intubation attempts, the ease of use in each step of the intubation, and adverse events were recorded. The intubation steps comprised: insertion in the oropharynx, visualization of the epiglottis, placement of the stylet under the epiglottis, identification of the vocal cords, advancement into the glottis aperture, and maneuverability of the tracheal tube. The ease of use was classified as excellent, good, fair, or poor. Airway complications such as dental trauma, lip laceration, and mucosal bleeding, and equipment malfunction were also recorded. The study protocol was divided into the learning phase (the first 10 patients for each practitioner) and the standard phase (the remaining 20 patients for each practitioner). The learning and standard phases were further subdivided into six subphases (L1-2 and S1-4, respectively), each of which comprised five patients. All data were presented as mean ± SD (range) or numbers. Normal distribution was assessed by using the Kolmogorov-Smirnov test. To test differences between patient groups, t-test, Mann-Whitney U test, and Kruskal-Wallis test with post-hoc analysis with Bonferroni correction were used, as appropriate. To compare patient groups in terms of success rate at the first attempt, Fisher's exact test or the Chi-squared test was utilized. All statistical data were analyzed using the Statistical Package for Social Sciences 20.0 (IBM Corp., Armonk, NY, USA). P-values < 0.05 were considered statistically significant.
RESULTS
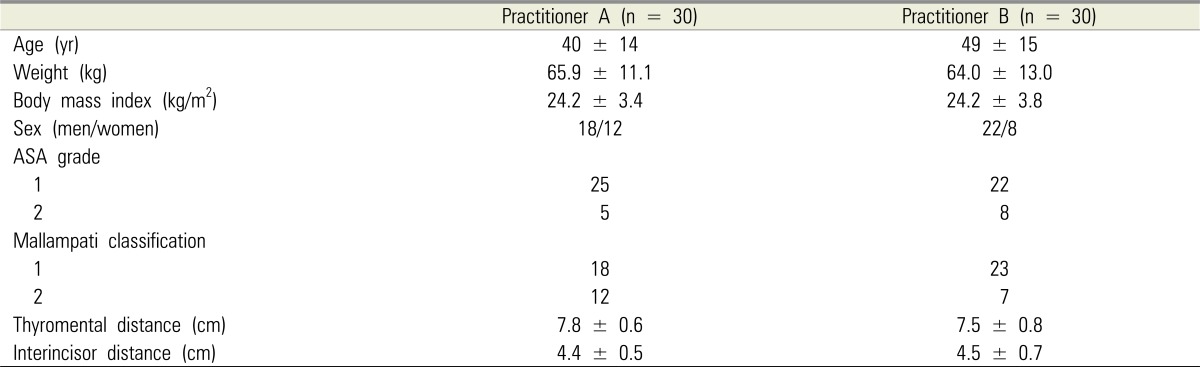
In total 60 patients were enrolled in this study. The demographic and clinical characteristics of the patients are presented in Table 1.
Table 1. Demographic characteristics of patients enrolled in the study.
Values are mean ± SD or number.
ASA, American Society of Anesthesiologists.
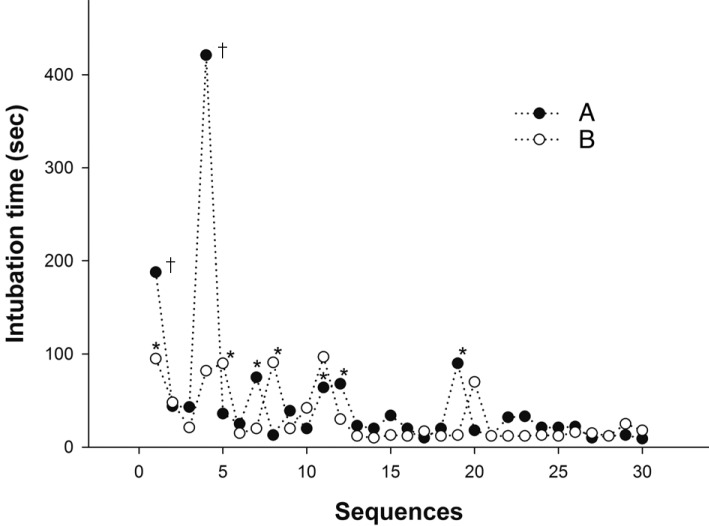
The two practitioners performed 30 endotracheal intubations each. Intubation was successful in all patients. In 51 patients, the intubation was accomplished on the first attempt. Seven patients required two intubation attempts (A = 4, B = 3), and two patients required three intubation attempts (A = 2, B = 0). The total time to intubate was not significantly different between the two practitioners in both learning and standard phases. Figure 1 shows the sequence of intubation time and the number of attempts by each practitioner as experience increased.
Fig. 1. Intubation times and number of attempts using Clarus Video System by two novice practitioners (A and B). *Two attempts required to intubate, †Intubation failed within two attempts.
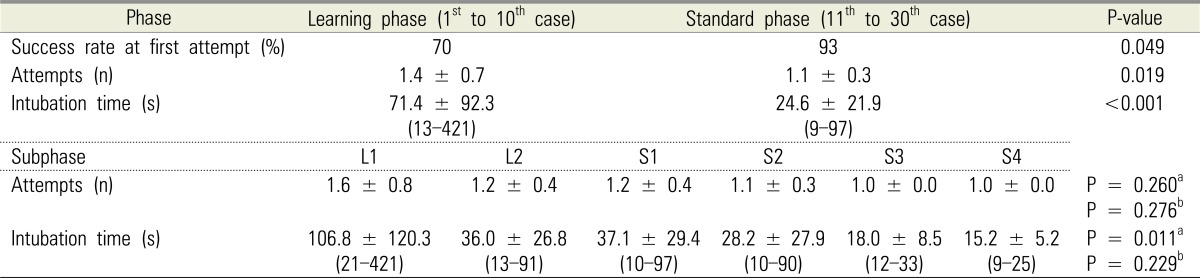
The learning phase and standard phase differed significantly in terms of success rate at first attempt, number of total attempts, and intubation time (P = 0.049, 0.019, and < 0.001, respectively, Table 2). In the learning phase, intubation time took significantly longer in subphase L1 than that in subphase L2 (P = 0.011). Number of attempts did not differ between the L1 and L2 subphases. Among the four subphases of the standard phase, no statistically significant differences were found with regard to the number of attempts and intubation time.
Table 2. Comparison of success rate at first attempt, total number of intubation attempts, and intubation time between learning and standard phases.
Values are mean ± SD (range).
aComparison between L1 and L2; bComparisons between S1, S2, S3, and S4.
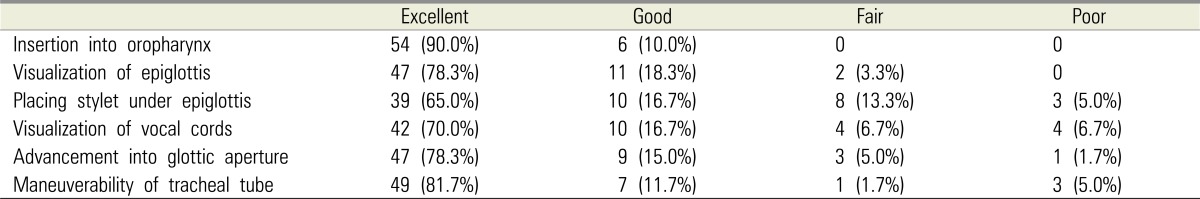
Ease of intubation at each step of the procedure is summarized in Table 3. The reasons for failure at the first or second attempt comprised secretions preventing a view of the glottic aperture (n = 5), failure in maneuverability of the tracheal tube (n = 3), failure to advance the tracheal tube into the glottis aperture (n = 1), difficulty in visualization of the epiglottis (n = 1), and fogged lens (n = 1).
Table 3. Subjective assessment of intubation conditions (n = 60).
Values are numbers (%).
There was no cases of dental trauma, lip laceration, or mucosal bleeding recorded for any of the enrolled patients. Furthermore, no episodes of desaturation or esophageal intubation occurred during the procedures.
DISCUSSION
The results of our study demonstrate that only 10 experiences of intubation are sufficient as a learning process for the proper use of the CVS. Success rate at first attempt, intubation time, and number of attempts significantly improved after 10 experiences of intubation. Our results suggest that the CVS requires a relatively smaller number of experiences as a learning curve for inexperienced trainees compared with other alternative airway devices.
Although numerous alternative airway devices have been introduced, considerable training is imperative for proper utilization. Fiberoptic bronchoscopy, the current gold standard for difficult airway management, requires a considerable amount of training and skill to perform [11]. The learning curve for fiberoptic bronchoscope intubation in normal airways has been reported to be approximately 40 intubations [12]. Furthermore, the mean intubation time associated with fiberoptic bronchoscopy after proficiency has been achieved is between 50 and 120 s [13,14,15]. The utilization of the video laryngoscope is easier to learn than the fiberoptic bronchoscope due to its similarities with the conventional laryngoscope [16]. However, bulky blades of video laryngoscopes may hamper maneuverability in patients with limited mouth opening [17,18]. Bonfils fiberscope is a rigid optical stylet with a fixed tip angle of 40° [19]. Several studies suggest that 20 intubations provide sufficient experience for clinical use of Bonfils fiberscope in normal airways [19,20]. After becoming proficient in the use of the Bonfils fiberscope, the mean intubation time is between 30 and 80 s [19,20,21,22]. However, the fixed angle of the tip could make it difficult to negotiate the oralpharyngeal-tracheal axes [6,23].
The CVS is an evolved form of optical stylet because it is equipped with a semi-rigid malleable tip and an embedded monitor. Unlike the fixed tip of the Bonfils fiberscope, it has an adjustable tip angle. This may help to increase the chance of successful intubation [6]. Our study showed that only 10 experiences were needed to gain proficiency in use of the CVS and the mean intubation time with the CVS after the tenth intubation was just 24.6 s. These values are considerable shorter than those of alternative airway devices. These results agree with those of previous studies that demonstrated a relatively short intubation time with the CVS, that this device is easy to use, and that it is associated with a high intubation success rate in various airway situations, including difficult airways and intubations for one-lung ventilation [5,6,7,8,9].
Of the 60 consecutive patients in this study, nine required two or more intubation attempts. Six of those nine patients were in the learning phase. Most of the failures were easily corrected during subsequent attempts. Secretions were reported as the main cause of failed intubation. Several other studies also found that a key limiting factor in the performance of successful intubation is view impairment due to excessive secretion and tissue contact [19,23]. Subjective assessment of the handling of the CVS showed that the most difficult step was placing the stylet under the epiglottis. When there was insufficient retropharyngeal space, we used the chin-and-tongue lift maneuver to lift the epiglottis above the posterior pharyngeal wall. If this maneuver failed to resolve the problem, we could have employed the backward, upward, and right-sided pressure maneuver, or the modified jaw thrust maneuver by an assistant [6]; however, neither of these maneuvers were permitted in our study protocol. Our study had several limitations. First, we only enrolled two practitioners. Although the findings of this study are apparent, potential bias could have occurred due to this small number of practitioners. Second, the two practitioners in this study had been trained for at least 1 year in the use of the direct laryngoscope and were familiar with airway anatomy. Therefore, our findings cannot be extrapolated to physicians or paramedical personnel lacking training in the anatomy of the oral airways. Third, we did not evaluate patients with an expected or simulated difficult airway. Therefore, our results cannot be applied to this subgroup of patients. Further studies are required to evaluate the learning curve of the CVS in patients with difficult airways.
CONCLUSIONS
In conclusion, we found that 10 intubation experiences were sufficient to learn the proper use of the CVS without resulting in orodental trauma. The fast learning curve associated with the CVS and its usefulness in various airway situations suggest that its clinical role in airway management may increase in the future.
References
- 1.Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013;118:251–270. doi: 10.1097/ALN.0b013e31827773b2. [DOI] [PubMed] [Google Scholar]
- 2.Rai MR, Dering A, Verghese C. The Glidescope system: a clinical assessment of performance. Anaesthesia. 2005;60:60–64. doi: 10.1111/j.1365-2044.2004.04013.x. [DOI] [PubMed] [Google Scholar]
- 3.Kim JK, Kim JA, Kim CS, Ahn HJ, Yang MK, Choi SJ. Comparison of tracheal intubation with the Airway Scope or Clarus Video System in patients with cervicalcollars. Anaesthesia. 2011;66:694–698. doi: 10.1111/j.1365-2044.2011.06762.x. [DOI] [PubMed] [Google Scholar]
- 4.Yang M, Kim JA, Ahn HJ, Choi JW, Kim DK, Cho EA. Double-lumen tube tracheal intubation using a rigid video-stylet: a randomized controlled comparison with the Macintosh laryngoscope. Br J Anaesth. 2013;111:990–995. doi: 10.1093/bja/aet281. [DOI] [PubMed] [Google Scholar]
- 5.Cheng WC, Lan CH, Lai HY. The Clarus Video System (Trachway) intubating stylet for awake intubation. Anaesthesia. 2011;66:1178–1180. doi: 10.1111/j.1365-2044.2011.06948.x. [DOI] [PubMed] [Google Scholar]
- 6.Lee AR, Yang S, Shin YH, Kim JA, Chung IS, Cho HS, et al. A comparison of the BURP and conventional and modified jaw thrust manoeuvres for orotracheal intubation using the Clarus Video System. Anaesthesia. 2013;68:931–937. doi: 10.1111/anae.12282. [DOI] [PubMed] [Google Scholar]
- 7.Costa F, Mattei A, Massimiliano C, Cataldo R, Agro FE. The Clarus Video System as a useful diagnostic tool. Anaesthesia. 2011;66:135–136. doi: 10.1111/j.1365-2044.2010.06590.x. [DOI] [PubMed] [Google Scholar]
- 8.Gaszynski T, Gaszynska E. The Clarus Video System stylet for awake intubation in a very difficult urgent intubation. Anaesthesiol Intensive Ther. 2013;45:153–154. doi: 10.5603/AIT.2013.0032. [DOI] [PubMed] [Google Scholar]
- 9.Seo H, Lee G, Ha SI, Song JG. An awake double lumen endotracheal tube intubation using the Clarus Video System in a patient with an epiglottic cyst: a case report. Korean J Anesthesiol. 2014;66:157–159. doi: 10.4097/kjae.2014.66.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kitagawa H, Yamazaki T, Imashuku Y. The "jaw thrust" maneuver rather than the "BURP" maneuver improves the glottic view for Pentax-AWS assisted tracheal intubation in a patient with a laryngeal aperture. Can J Anaesth. 2010;57:517–518. doi: 10.1007/s12630-010-9283-7. [DOI] [PubMed] [Google Scholar]
- 11.Mihai R, Blair E, Kay H, Cook TM. A quantitative review and meta-analysis of performance of non-standard laryngoscopes and rigid fibreoptic intubation aids. Anaesthesia. 2008;63:745–760. doi: 10.1111/j.1365-2044.2008.05489.x. [DOI] [PubMed] [Google Scholar]
- 12.Dalal PG, Dalal GB, Pott L, Bezinover D, Prozesky J, Bosseau Murray W. Learning curves of novice anesthesiology residents performing simulated fibreoptic upper airway endoscopy. Can J Anaesth. 2011;58:802–809. doi: 10.1007/s12630-011-9542-2. [DOI] [PubMed] [Google Scholar]
- 13.Cole AF, Mallon JS, Rolbin SH, Ananthanarayan C. Fiberoptic intubation using anesthetized, paralyzed, apneic patients. Results of a resident training program. Anesthesiology. 1996;84:1101–1106. doi: 10.1097/00000542-199605000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Erb T, Hampl KF, Schurch M, Kern CG, Marsch SC. Teaching the use of fiberoptic intubation in anesthetized, spontaneously breathing patients. Anesth Analg. 1999;89:1292–1295. [PubMed] [Google Scholar]
- 15.Aqil M. A study of stress response to endotracheal intubation comparing glidescope and flexible fiberoptic bronchoscope. Pak J Med Sci. 2014;30:1001–1006. doi: 10.12669/pjms.305.4788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paolini JB, Donati F, Drolet P. Review article: video-laryngoscopy: another tool for difficult intubation or a new paradigm in airway management? Can J Anaesth. 2013;60:184–191. doi: 10.1007/s12630-012-9859-5. [DOI] [PubMed] [Google Scholar]
- 17.Maruyama K, Yamada T, Kawakami R, Kamata T, Yokochi M, Hara K. Upper cervical spine movement during intubation: fluoroscopic comparison of the AirWay Scope, McCoy laryngoscope, and Macintosh laryngoscope. Br J Anaesth. 2008;100:120–124. doi: 10.1093/bja/aem313. [DOI] [PubMed] [Google Scholar]
- 18.Taylor AM, Peck M, Launcelott S, Hung OR, Law JA, MacQuarrie K, et al. The McGrath(R) Series 5 videolaryngoscope vs the Macintosh laryngoscope: a randomised, controlled trial in patients with a simulated difficult airway. Anaesthesia. 2013;68:142–147. doi: 10.1111/anae.12075. [DOI] [PubMed] [Google Scholar]
- 19.Thong SY, Wong TG. Clinical uses of the Bonfils Retromolar Intubation Fiberscope: a review. Anesth Analg. 2012;115:855–866. doi: 10.1213/ANE.0b013e318265bae2. [DOI] [PubMed] [Google Scholar]
- 20.Corbanese U, Morossi M. The Bonfils intubation fibrescope: clinical evaluation and consideration of the learning curve. Eur J Anaesthesiol. 2009;26:622–624. doi: 10.1097/EJA.0b013e328328f572. [DOI] [PubMed] [Google Scholar]
- 21.Wong P. Intubation times for using the Bonfils intubation fibrescope. Br J Anaesth. 2003;91:757, author reply -8. [PubMed] [Google Scholar]
- 22.Halligan M, Charters P. A clinical evaluation of the Bonfils Intubation Fibrescope. Anaesthesia. 2003;58:1087–1091. doi: 10.1046/j.1365-2044.2003.03407.x. [DOI] [PubMed] [Google Scholar]
- 23.Liem EB, Bjoraker DG, Gravenstein D. New options for airway management: intubating fibreoptic stylets. Br J Anaesth. 2003;91:408–418. doi: 10.1093/bja/aeg011. [DOI] [PubMed] [Google Scholar]