Abstract
Objective
Recent changes in DSM criteria require new documentation of the prevalence and developmental sequences of cannabis use disorder. Our goal was to study the early course of DSM-5 cannabis use disorder (CUD) and its overlap with DSM-IV and consumption constructs in a community-representative sample with American Indians.
Method
Data came from the prospective-longitudinal, population-based Great Smoky Mountains Study in North Carolina (N = 1,420, including n = 349 American Indians). Cannabis use and disorder were assessed during yearly interviews from ages 9 to 16, and again at ages 19, 21, 26, and 30 (up to 11 assessments per participant between 1993 and 2015).
Results
By age 30, approximately 70% of participants had used cannabis, 34% had used daily, and 18% had met criteria for DSM-5 CUD. Approximately 1 in 4 cannabis users met criteria for CUD at some point. Those who met criteria initiated use over two years earlier (at age 13.3) compared to other users. Despite higher risks due to increased poverty, American Indians’ patterns of use were similar to the rest of the sample. Concordance between DSM-5 CUD and DSM-IV abuse/dependence was substantial, but was even higher between DSM-5 CUD and daily use.
Conclusion
It was common to have either used cannabis daily or to have met criteria for DSM-5 CUD by adulthood. DSM-5 CUD was an improvement over DSM-IV diagnostic constructs by raising the threshold for diagnosis.
Keywords: American Indian, cannabis use, cannabis use disorder, epidemiology, adolescence
INTRODUCTION
As efforts to legalize and decriminalize cannabis use are growing, cannabis involvement is increasingly viewed as harmless by youth (e.g., 1, 2). At the same time, criteria for problematic cannabis use were changed with the 2013 transition to DSM-5, and critical pieces of information about cannabis disorder and use are currently missing. These include basic epidemiological documentation of DSM-5 cannabis use disorder (CUD) prevalence and the overlap with DSM-IV diagnostic constructs and frequent-use measures up to age 30.
Several diagnostic changes were implemented with the transition to DSM-5. First, abuse and dependence were combined into a single CUD category. Second, a criterion related to cannabis-related legal problems was removed. This change may reduce racial/ethnic differences in areas in which there are disparities in legal or police contact. Third, a criterion related to craving/withdrawal was included. Finally, the threshold to diagnose was increased from ≥ 1 criterion to ≥ 2 criteria.3, 4 This last change was implemented to address concerns that the threshold for DSM-IV abuse disorder was too low and potentially allowed for transient substance problems to be considered diagnostic. These changes in diagnostic criteria could impact the overall prevalence of CUD and also who (e.g., in terms of frequency of use) is likely to be diagnosed.
The aim of this analysis is to use a community-representative, longitudinal sample of children to study DSM-5 CUD from ages 9 to 30. This includes looking at the point prevalence of cannabis use at different ages as well as assessing the cumulative prevalence of CUD by age 30. Next, we examine the overlap between DSM-5 CUD with DSM-IV constructs and different frequency measures of cannabis use (e.g., weekly, daily). One goal is to understand whether the DSM changes accomplished what was intended; another is to determine how well frequency of cannabis use tracks DSM-5 CUD for clinical diagnostic purposes.
American Indians are one of the most understudied segments of the population. The longitudinal course of substance use is rarely documented among American Indian youth; this gap in research exists, in part, because of a lack of long-term longitudinal studies among this group.5,6 On average, substance use among American Indians begins earlier than among other races/ethnicities, involves heavier use, and increases more steeply.7,8 Notably, considerable tribal and regional variation in use exists. With respect to cannabis use specifically, cross-sectional studies—primarily from the Western United States—reported that early marijuana use among American Indian youth was common.9 In one tribe, >50% of youth had used marijuana by age 13.9 Reasons cited for high cannabis use in this group include cultural/historical traditions, easier access to cannabis than to alcohol on some reservations,9 and, importantly, demographic hardship— including poverty—endured by many American Indians (e.g., 9, 10). The current study examines cannabis use and disorder among American Indian youth from the Cherokee Nation tribe in western North Carolina and local residents, who are primarily non-Hispanic whites.
In addition to race/ethnic differences, sex differences in cannabis use and disorder are known to exist in adolescence and young adulthood.11–16 More information is needed about when such sex differences emerge, and whether sex differences take a similar developmental course in American Indian youth compared to other racial/ethnic groups.
METHOD
Participants
The Great Smoky Mountains Study (GSMS) is a prospective, longitudinal study of the development of psychiatric disorders and need for mental health services in rural and urban youth.17–19 Three cohorts of children aged 9, 11, and 13 years at intake were recruited from 11 counties in western North Carolina in 1993. The GSMS design and sampling procedures are described elsewhere.17,19 Briefly, a two-stage sampling design was employed, which oversampled for American Indians, who only make up 3% of the area population but 25% of the study sample. Accordingly, all participants were given a weight inversely proportional to their probability of selection to create a representative sample of western North Carolina. Of all participants recruited, 80% (N=1,420) agreed to participate. Of the 1,420 participants, 51.1% were female (unweighted n=630), 6.9% were non-Hispanic African-American (n=88), and 3.7% were American Indian (n=349). Throughout the results section, comparisons are made between the American Indian subsample and the other participants. The latter group was labeled “non-Indian” and consisted mainly of non-Hispanic whites and the small proportion of non-Hispanic African Americans.
Annual assessments were completed on the 1,420 children until age 16 and then again at ages 19, 21, 25, and 30 for a total of 11,084 assessments. The maximum possible number of interviews per participant is 8 (oldest cohort), 10 (middle cohort), and 11 (youngest cohort). The mean number of interviews to date is 7.7 (SD 2.3). Across all waves, 82.1% of all possible interviews were completed, ranging from 74% – 94% at any particular wave.
Procedures
The parent (biological mother for 83% of interviews) and participant were interviewed by trained interviewers separately until the participant was 16; thereafter, only participants were interviewed. Before the interviews began, both the parent and child signed informed consent forms approved by the Duke University Medical Center Institutional Review Board. Each parent and child received an honorarium for their participation.
Assessment
All variables were assessed using the Child and Adolescent Psychiatric Assessment (CAPA) until age 16, and its upward extension, the Young Adult Psychiatric Assessment (YAPA) thereafter.20, 21 These structured interviews were coded by a trained interviewer, and each interview was subsequently checked by a supervisor. A detailed glossary provides the operational rules for each item assessed. In addition to the cannabis-related variables described below, the interview collected information on sex, race/ethnicity, and variables needed to calculate poverty status according to the federal guidelines for the year in which the assessment took place.
Cannabis Involvement
For the current analysis, the focus was on cannabis involvement, including DSM-5 CUD, DSM-IV abuse, DSM-IV dependence, and non-diagnostic frequency measures for daily, weekly, or any cannabis use. The substance use module of the CAPA/YAPA assesses cannabis use, abuse, addiction, and disorder. The phenomenology of cannabis use was assessed via age-of-onset, frequency of use, symptoms of DSM-IV abuse and dependence, DSM-5 CUD, and associated features of problematic use. These include: use of cannabis to improve mood, narrowed substance use repertoire, use first thing in the morning, blackouts, and cannabis-related criminality. Although DSM-5 CUD symptoms of craving and withdrawal were not part of DSM-IV abuse or dependence diagnostic criteria, these data have been collected since the start of the GSMS study in 1993. The time frame for determining the presence of diagnostic items (both DSM-IV and DSM-5) was the three months immediately prior to the interview to minimize recall biases. Assessment of cannabis use and frequency of use included assessments of three-month primary periods for each interview, cumulatively across all interviews (i.e., across 8, 10, and 11 interviews for the oldest, middle, and youngest cohorts, respectively), and an ever/lifetime status.
The structure of the CAPA/YAPA substance use section consists of a preliminary section covering the use of specific substances, followed by a detailed section on symptoms and impairment, asked only if use is reported. Scoring algorithms written in SAS generate variables indicative of symptoms for DSM-IV abuse and dependence diagnoses and DSM-5 CUD. In a two-week test retest study to determine the reliability of participant reporting, the intraclass correlation coefficient (ICC) for the number of substance abuse/dependence symptoms was .98.22
Analytic Strategy
Sampling weights were applied to account for differential probability of selection and to ensure that the results represent unbiased estimates for the original population from which the sample was drawn. All reported prevalence estimates are weighted, and all sample sizes are unweighted. In addition, sandwich-type variance corrections23 were applied to adjust for the parameter and variance effects induced by the sampling stratification. Weighted regression analyses were completed using PROC GENMOD in SAS 9.4.24
RESULTS
3-Month Point Prevalence of Cannabis Involvement
Figures 1A–E show age-related patterns from ages 9 to 30 for 3-month cannabis-related disorders and daily, weekly, and any cannabis use for non-Indian and Indian females and males. These figures illustrate rapid increases from preadolescence to late adolescence, peaking at ages 19–21, and subsequent declines in the mid-20s that remain stable (i.e., slower declines or no change) to age 30. These age-related prevalence patterns were consistent with a cubic age effect for all frequency levels of cannabis involvement. The percentage of participants meeting DSM-5 CUD criteria (Figure 1a) was similar to that of participants meeting either DSM-IV cannabis abuse or dependence disorders (Figure 1b) and slightly higher than that of participants reporting daily use in a three-month primary period (Figure 1c) from 9–30 years old.
Figure 1.
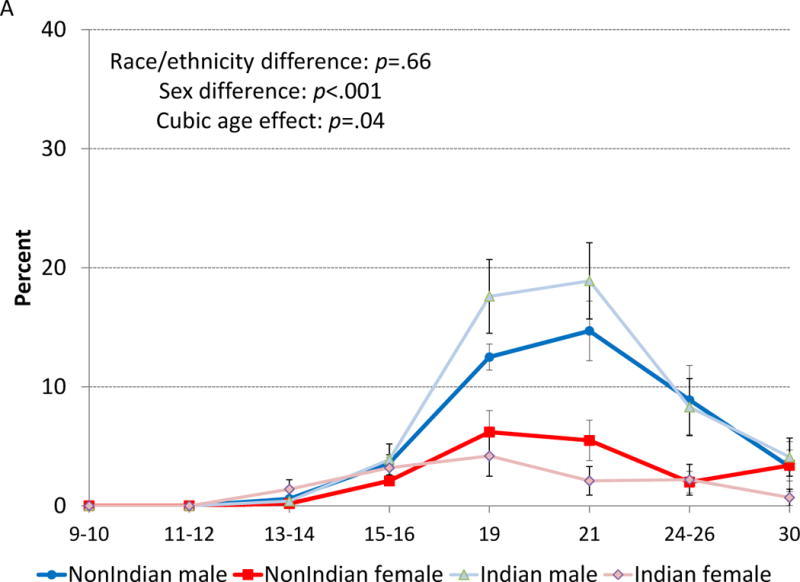
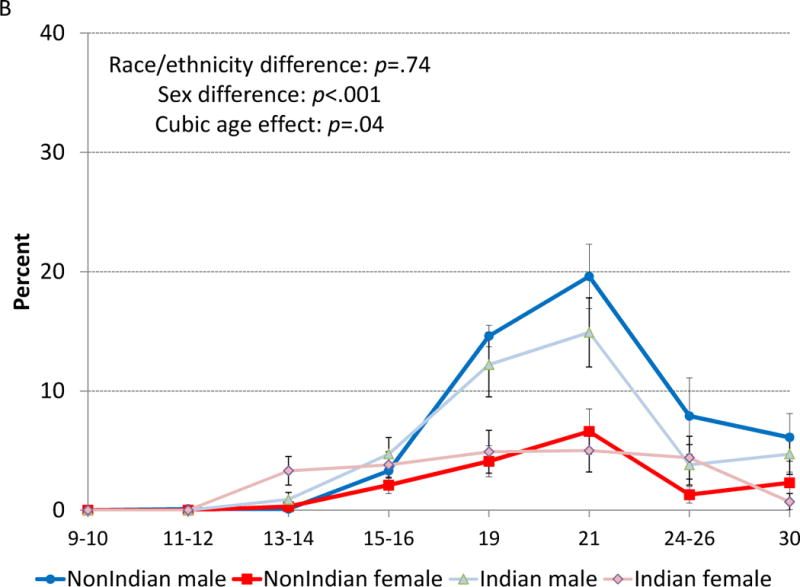
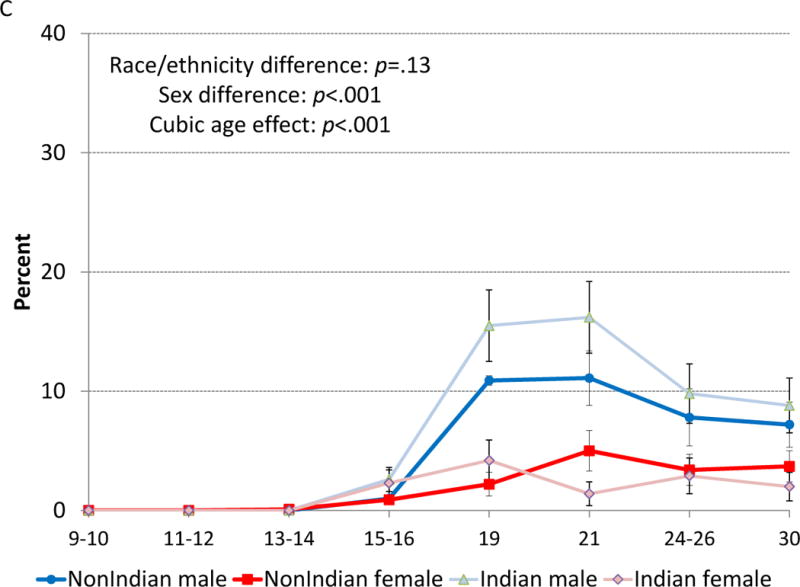
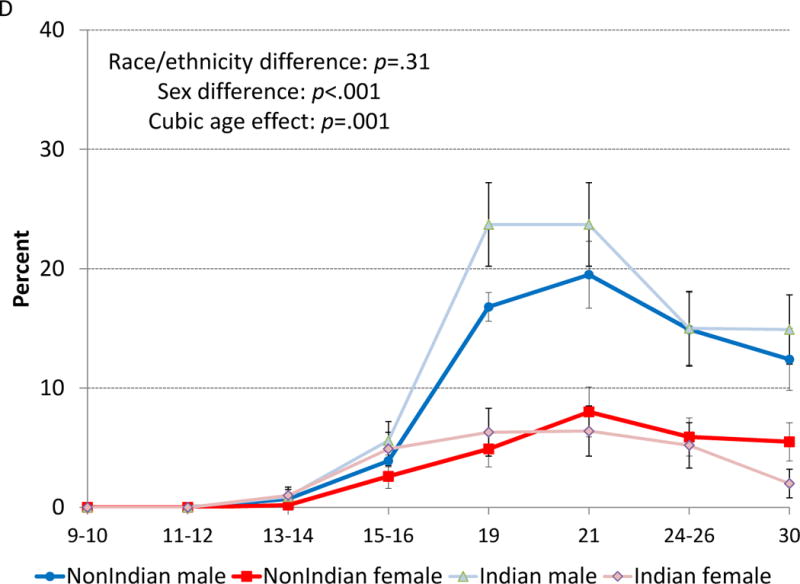
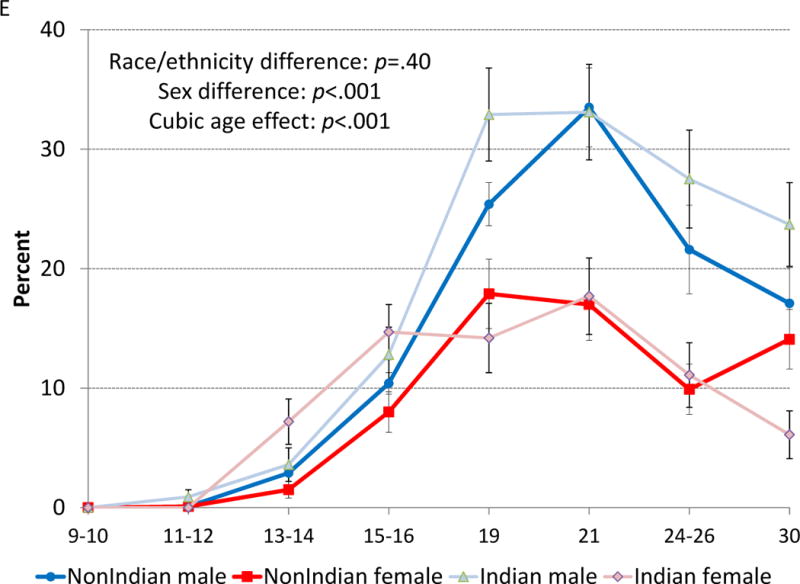
Three-month prevalence estimates for a) DSM-5 cannabis use disorder (CUD), b) DSM-IV abuse or dependence, c) daily cannabis use, d) weekly cannabis use, and e) any cannabis use from ages 9 to 30 by sex and Indian/non-Indian status.
An approximate 2-to-1 sex ratio was observed across all frequency levels of cannabis involvement during peak use periods at 19–21 years. For example, daily use (Figure 1c) peaked at approximately 10–15% for males and up to 5% for females. Weekly use (Figure 1d) peaked near 20% for males and just below 10% for females. Finally, any use in the past three months (Figure 1e) peaked at over 30% for males and over 15% for females. There was some evidence that the observed age-related patterns differed by sex and age by sex interactions in the trend range (p<.10). Among females only, the cubic age effect was significant (p<.05) for DSM-5 CUD, DSM-IV abuse/dependence, weekly use, and any use, while daily use showed no age-related effect.
There were no consistent significant differences in overall levels or developmental trends of cannabis involvement by Indian/non-Indian status. Only at very specific ages did American Indians report slightly higher cannabis involvement (ps < .05). For instance, at age 19, American Indian males had the highest any use, weekly use, daily use, and DSM-5 CUD, and at ages 13–14 American Indian females reported the most any use and DSM-IV cannabis abuse/dependence. In turn, at age 30, American Indian females had the lowest levels of involvement for weekly and any cannabis use.
Cumulative Prevalence Across Childhood and Early Adulthood
Given the potentially harmful effects of cannabis exposure during the first few decades of life, an important public health question is just how many participants have reported cannabis involvement cumulatively—at some point from childhood to early adulthood. By age 30, 18% of study participants had met criteria for DSM-5 CUD and 21% for DSM-IV cannabis abuse/dependence (Table 1). Males had higher cumulative prevalence estimates than females for both DSM-IV and DSM-5 disorders. Race/ethnic differences in cumulative diagnostic prevalence estimates did not emerge. When the ever/lifetime variables were aggregated into cumulative lifetime prevalence variables, the data indicated that by age 30, one in three participants had used cannabis daily at some point; almost half had a period of weekly use; and over 7 in 10 participants had used cannabis (i.e., any use). Overlaying the cumulative ever/lifetime involvement data and cumulative diagnostic data suggested that 25% of participants who reported ever using cannabis met criteria for DSM-5 CUD.
Table 1.
Cumulative Prevalence Estimates of Cannabis Disorder and Frequency of Use by Age 30
| Overall | Non-Indians | Indians | Sex Differences | Race/Ethnicity Differences | |||
|---|---|---|---|---|---|---|---|
| Female | Male | Female | Male | ||||
| Total | N=1,420 | n=464 | n=607 | n=166 | n=183 | ||
| % (n) | % (n) | % (n) | % (n) | % (n) | p | p | |
| Cumulative Diagnoses – 3-Month Timeframe | |||||||
| 3-month DSM-5 CUD | 17.9 (269) | 12.3 (60) | 23.2 (138) | 11.5 (19) | 28.4 (52) | .002 | .39 |
| 3-month DSM-IV abuse/dependence | 20.5 (290) | 12.1 (66) | 28.5 (150) | 16.3 (27) | 25.7 (47) | <.001 | .86 |
| Cumulative Use – Ever Time Frame | |||||||
| Ever daily use | 34.4 (548) | 23.8 (119) | 43.9 (277) | 35.5 (59) | 50.8 (93) | <.001 | .006 |
| Ever weekly use | 47.9 (714) | 40.3 (184) | 54.6 (337) | 45.2 (75) | 64.5 (118) | .001 | .03 |
| Ever any use | 71.5 (1038) | 68.7 (327) | 73.8 (442) | 75.9 (126) | 78.1 (143) | .22 | .07 |
Note: Bolded values are significant at p <.05. CUD = cannabis use disorder.
Males reported more frequent involvement than females across all use variables (e.g., daily, weekly) except any use. With respect to race/ethnic differences, American Indians reported more cumulative and ever/lifetime “daily use” and also more ever/lifetime “weekly use” but not cumulative “any use” or “ever weekly use.” Table S1, available online, provides cumulative prevalence estimates for all categories of cannabis involvement up to age 16 when high levels of involvement were much less common.
Ages-of-Onset
Median ages-of-onset were derived from the ever/lifetime variables (except for DSM diagnoses, which were assessed using the three-month time frame only). The median age-of-onset for cannabis-related disorders was around age 19 (Table 2; Figure S1, available online). For the non-diagnostic use variables, at least one in four users initiated use by age 16 or earlier according to interquartile ranges. Significant sex differences existed for both the diagnostic and non-diagnostic variables, with males typically displaying earlier onsets than females. Race/ethnic differences did not emerge for the diagnostic age-of-onset data, but they did emerge for all frequency of use data, with American Indians typically initiating use at earlier ages than non- Indians (noted higher cumulative rates by age 16 in Table S1, available online).
Table 2.
Age-of-Onsets for Cannabis Disorder and Use Among Young People Who Have Ever Used Cannabis
| Overall | Non-Indians | Indians | Sex Differences | Race/Ethnicity Differences | |||
|---|---|---|---|---|---|---|---|
| Female | Male | Female | Male | ||||
| M (IQR) | M (IQR) | M (IQR) | M (IQR) | M (IQR) | p | p | |
| DSM-5 CUD | 19.3 (18.9–21.3) |
19.0 (16.1–21.4) |
19.5 (18.9–21.3) |
19.1 (15.1–20.9) |
19.4 (19.0–21.6) |
.001 | .37 |
| DSM-IV abuse or dependence | 19.6 (18.9–21.6) |
19.2 (16.1–21.3) |
20.1 (18.9–21.7) |
16.1 (14.6–20.8) |
19.8 (16.9–21.5) |
<.001 | .79 |
| Daily use | 16.6 (15.5–18.8) |
16.5 (15.5–19.5) |
16.6 (15.5–18.6) |
17.0 (15.5–18.6) |
16.0 (15.0–18.0) |
<.001 | .003 |
| Weekly use | 16.1 (14.5–18.0) |
16.5 (15.0–18.0) |
16.0 (14.5–17.6) |
16.0 (14.5–18.0) |
15.5 (14.0–18.0) |
<.001 | .02 |
| Any use | 15.0 (13.3–17.0) |
15.5 (13.9–17.5) |
14.6 (12.5–16.4) |
14.9 (13.0–16.4) |
14.0 (12.0–16.0) |
.02 | .009 |
Note: Bolded values are significant at p <.05. CUD = cannabis use disorder; IQR = interquartile range difference between the 25th and 75th quartiles.
Age-of-onset data was also used to understand progression to high-frequency use. These analyses revealed that those who met criteria for DSM-5 CUD initiated cannabis use earlier than those who never met full CUD criteria (median of 13.3 vs. 15.5 years, p <.001). Similarly, youth who reported daily use at some point by age 30 had a significantly younger age-of-onset of cannabis use compared to their peers who reported any use but never daily use (median of 14.0 vs. 16.3 years, p <.001).
DSM-5 and DSM-IV Overlap
Figure 2a shows the levels of co-occurrence for participants who met criteria for either DSM-5 CUD or DSM-IV cannabis disorder (abuse or dependence) at any given assessment and also cumulatively by age 30. The overlap was high and statistically significant (any given assessment: OR=52.0, 95% CI, 34.9–77.6, p <.001 or κ= 0.49; cumulatively: OR=19.2, 95% CI, 11.0–44.6, p <.001 or κ= 0.55). At any given wave, nearly half of the participants who met criteria for a cannabis disorder according to one of the DSM diagnostic guidelines failed to meet criteria for the other. Figure 2b shows the overlap between specific DSM-IV disorders and DSM- 5 CUD at any given wave. Overall, approximately a third of participants met criteria for a diagnosis of DSM-IV abuse/dependence, DSM-5 CUD, or both. The high overlap was primarily due to DSM-IV abuse, as there were no cases of DSM-IV dependence that failed to meet criteria for DSM-5 CUD. This raises the question of who is meeting criteria for DSM-5 CUD but did not meet criteria for either DSM-IV disorder. Participants meeting criteria for DSM-5 CUD only reported no DSM-IV abuse symptoms (by definition) but did report a mean of 1.7 dependence symptoms (SD=0.54). (This compared to a mean of 2.1 symptoms [SD=0.87] for cases that overlapped.) Thus, in this sample, DSM-5 CUD identified subthreshold DSM-IV dependence cases with no abuse symptoms. These cases, also known as diagnostic orphans, were previously undiagnosed.
Figure 2.
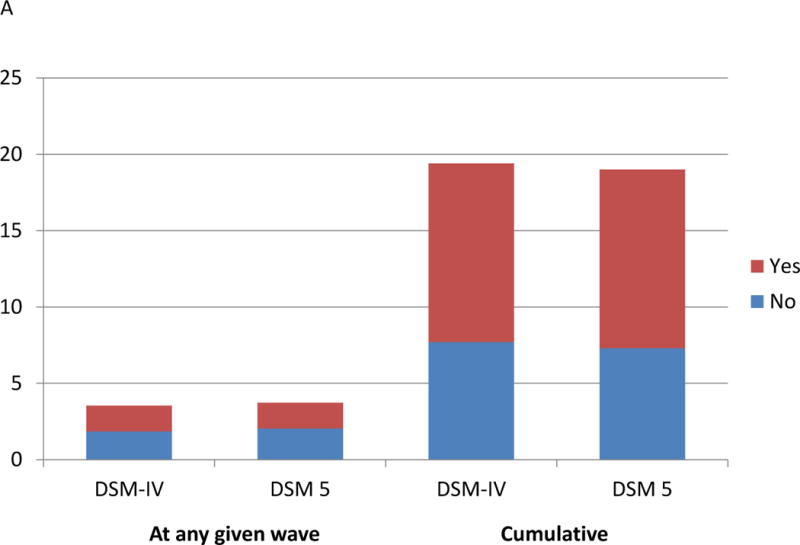
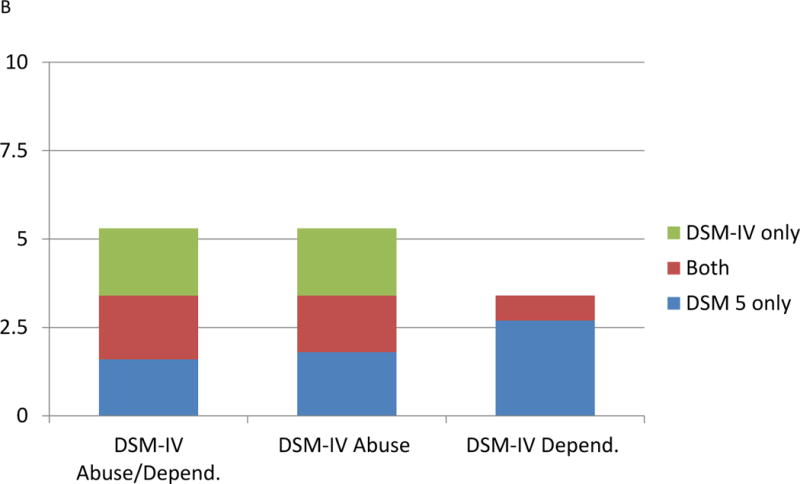
Co-occurrence of DSM-5 cannabis disorder a) with DSM-IV status at any given assessment and cumulatively and b) with specific DSM-IV cannabis disorder at a given assessment.
DSM-5 Cannabis Use Disorder and Frequent Cannabis Use
Finally, we examined overlap between DSM-5 CUD and frequent (i.e., daily) cannabis use. Figure 3a shows the levels of co-occurrence for those reporting either daily cannabis use or CUD at any given assessment and also cumulatively by age 30. The overlap was much greater than expected by chance (any given assessment: OR=151.0, 95% CI, 91.1–250.4, p <.001 or κ= 0.64; cumulatively: OR=95.3, 95% CI, 46.3–195.7, p <.001 or κ= 0.73). While DSM-5 CUD without daily use occurred some of the time, daily cannabis use without also meeting criteria for CUD was very rare. Figure 3b shows the cumulative overlap by the number of individual assessments at which an individual met criteria for CUD or reported daily cannabis use. As expected, the more often an individual reported daily use, the more likely s/he was to also report DSM-5 CUD and vice versa. A comparison of those who met criteria for DSM-5 CUD but never reported using cannabis daily with those who reported CUD and daily use showed significant differences on 2 of the 11 symptoms of CUD: time spent obtaining/using/recovering and craving. Individuals who reported daily use and met CUD diagnosis had significantly higher endorsement levels for both symptoms than those with CUD only (time spent: 96.4% vs. 61.6%, p <.001; craving: 70.2% vs. 11.6%, p <.001).
Figure 3.
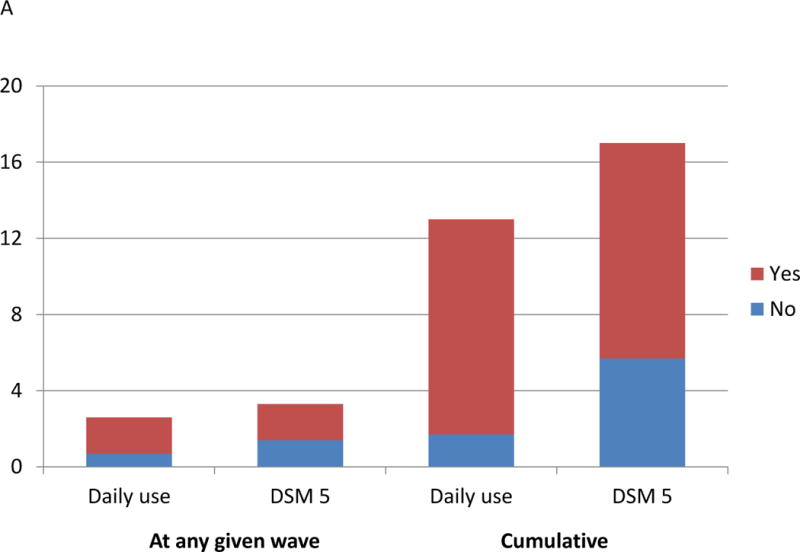
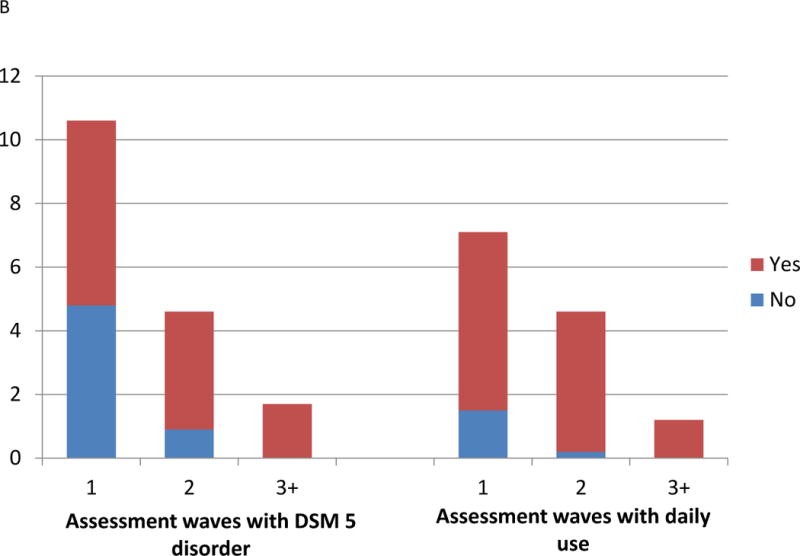
Co-occurrence of DSM-5 cannabis use disorder a) and daily cannabis use at any given assessment and cumulatively and b) with daily cannabis use cumulatively by the number of assessments with reported disorder or daily use.
DISCUSSION
Using the GSMS sample to assess participants from 9–30 years of age, we observed that levels of cannabis involvement were constantly changing, with steep increases across adolescence to a peak in early adulthood followed by decreases and subsequent plateaus to the early 30s. The findings are consistent with previous cross-sectional and shorter-term longitudinal studies of cannabis use.25–27 By age 30, approximately 70% of all participants had used cannabis at some point, over 30% had used cannabis daily, and 18% had met criteria for DSM-5 CUD based on cumulative prevalence estimates. This cumulative prevalence was higher than the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) III total lifetime estimate of 6.3% on average and 11% for ages 18–29.28 NESARC’s lower estimate is likely due to the cross-sectional, single-wave design with retrospective lifetime reports. Such designs tend to significantly underestimate the prevalence of mental health and substance disorders (e.g.,29,30)
Moreover, the observed GSMS cumulative prevalence estimate of DSM-5 CUD by age 30 is likely to be an underestimate, too. Our study assessed CUD in the 3 months immediately preceding each interview. Consequently, the assessments covered at most approximately two years and 9 months (11 assessments × 3 months) of our participants’ lives spanning a 21-year period. In addition, cannabis use had not been decriminalized or legalized in North Carolina during the study period, which may have resulted in under-reporting. Thus, the “true” prevalence of DSM-5 CUD by age 30 likely exceeds the observed 20%. This projection is also supported by our cumulative ever/lifetime variables for use that found that 1 in 4 individuals who had ever used cannabis by age 30 (70% of sample) also met criteria for DSM-5 CUD.
DSM-5 Comparison to DSM-IV and Frequency of Use Measures
Consistent with previous studies conducted among adults, the prevalence of CUD did not change dramatically when comparing DSM-5 and DSM-IV diagnoses.31, 32 The overlap in cases was substantial but not complete, below 50% at any given assessment. Inconsistencies in diagnoses were attributable to the addition of criteria in DSM-5 but also to the new minimum diagnostic threshold that falls between that of DSM-IV abuse and dependence. Consequently, only a subset of participants with DSM-5 CUD would meet full criteria for DSM-IV dependence. And, many participants with DSM-IV abuse would fail to meet minimum criteria for DSM-5 CUD. Importantly, the new DSM-5 CUD criteria cover DSM-IV diagnostic orphans, participants who were subthreshold for dependence but did not display abuse symptoms.32 As such, the changes to the DSM appear to have met the intended goals of raising the minimum threshold for having a cannabis disorder and covering prior diagnostic orphans.
At the same time, it is noteworthy that the overlap of DSM-5 was greater with a simple measure of daily cannabis use than with the DSM-IV constructs. Combined with prior findings, this study supports inclusion of frequency of use measures to future DSM criteria for CUD.33 Finally, additional work must be done on how this revised DSM construct relates to other psychiatric disorders over time (i.e., which disorders or comorbidities best predict DSM-5 CUD and vice versa).
Sex and Race Differences in Cannabis Involvement
Our findings suggest that overall levels of cannabis use and disorder were higher in males than in females, as has been shown in other studies.12,14–16 It is important to note, however, that the overall age-related pattern of steep increases in adolescence, peaks in young adulthood, and decreases/plateaus to age 30 did not differ by sex, suggesting similar developmental patterns despite underlying sex differences in overall levels.
There were no consistent race/ethnic differences in the point prevalence of 3-month use, DSM disorders, or the overall age-related trends in cannabis use. (The exceptions, Indian females in early adolescence and Indian males at age 19, were observed early in development.) The lack of race/ethnic differences is noteworthy because American Indians were exposed to substantially higher rates of poverty in our sample, and this risk factor is typically linked to substance use and disorders.5, 6 Resilience in our American Indian study population has been reported previously (to ages 19 and 21) and is, in part, attributable to income supplements received by American Indian families and their community following casino openings in the late 1990s.34 These findings are also consistent with correlational studies reporting that differences in substance use between American Indian and white participants are no longer significant when adjusting for annual family income and education level (and also sex, age, urbanicity, and region).26 There may be additional explanations for the late adolescent declines in use. Whitebeck et al. reported similar declines in late adolescents’ substance use in an indigenous sample that did not experience an income shock.35 As in their study, it is possible that cultural changes to promote greater resilience within the tribe could have contributed to the decline in cannabis use in late adolescence.
However, by age 30, our study identified higher cumulative ever/lifetime estimates in weekly and daily use among American Indians. These differences were likely due to an earlier age-of-onset of cannabis use among American Indian youth compared to their non-Indian neighbors. For example, by age 16, 38% of American Indian females and 28% of American Indian males had reported lifetime use compared to 15% and 23% of non-Indian females and males, respectively. High prevalence and “reverse” sex differences in early cannabis use would be consistent with previous work on American Indians.36, 37 Early onset and frequent use often predict subsequent problematic use,38 thus our lack of race/ethnic differences in 3-month use and CUD across ages is especially notable. Previous studies have reported faster increases in cannabis use among American Indians, which we did not find.7, 8 The geographic integration and social, educational, and economic opportunities available to American Indian adolescents in our study could have shielded them from an escalation of use.
The prospective, longitudinal cohort design is both a strength and a weakness. On the one hand, this design allowed us to examine age-related changes in the prevalence of cannabis disorder and frequency of use in the same group of individuals over time. On the other hand, policies and attitudes toward cannabis use have changed dramatically from 1993 to 2015, as did the chemical composition of cannabis products used across this period. Consequently, the age- related changes observed here may not generalize to other historical times, cohorts, and places. Nevertheless, our overall prevalence estimates (e.g., of DSM-IV diagnostic constructs) were remarkably similar to those from other studies from around the globe. In addition, the sample is only representative of the community from which it was drawn. Consequently, it is not representative of the US population in that American Indians are overrepresented and African Americans and Latinos underrepresented. It is also important to note that the Indian tribe studied here is distinctive in terms of its history and economics and social circumstances, and our findings are not meant to be representative of other tribes. Nevertheless, heterogeneity among Indian tribes should not be a barrier to research on this disadvantaged group, and our findings may inform expectations for other groups with similar characteristics.
This analysis has implications for a research agenda for DSM-5 CUD. First, given that close to 1 in 5 individuals met criteria for this disorder by age 30 and 1 in 3 reported daily use, it is imperative for additional work to test causal links between early life course cannabis involvement and later morbidities. This would prioritize longitudinal studies with detailed baseline data (particularly health measures) and adequate controls (e.g., sibling analysis, twin designs) as well as natural experiments that capitalize on the differences in legal restrictions regarding cannabis use across states and countries. Second, our age-related findings suggest that a joint consideration of late adolescence (as the period of highest first use) and the late 20s (as a key period of potential desistance from use) should be a priority for cannabis use researchers. A shift to analyses of developmental trajectories of age-at-initiation, duration of use, and desistance from use could be especially beneficial to understand precursors, correlates, and outcomes. Future studies of early risk factors for cannabis involvement should take into account these developmental findings to better understand what predicts cannabis use that persists into adulthood.
Our findings suggest that DSM-5 CUD is an improvement over DSM-IV diagnostic constructs by both raising the threshold for diagnosis and including important additional criteria while also eliminating some DSM-IV diagnostic orphans. Our findings also indicate that a simple heuristic for clinicians to assess risk for DSM-5 CUD is to ask about frequency of use. If daily use is reported, then DSM-5 CUD is likely.
Supplementary Material
Figure S1. Age of onset survival curves for cannabis involvement variables. Note: CUD = cannabis use disorder.
Acknowledgments
The work presented here was supported by the National Institute of Mental Health (MH63970, MH63671, MH48085, and MH094605), the National Institute on Drug Abuse (DA/MH11301, DA036523, and DA023026), and the William T. Grant Foundation.
Dr. Copeland had full access to all the data in the study, performed all statistical analyses, and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors would like to thank the participants of the Great Smoky Mountains Study and their families for their longstanding involvement in this study.
Disclosure: Dr. Copeland has received research support from the National Institute of Mental Health and the National Institute on Drug Abuse. Dr. Hill has received research support from the National Institute on Drug Abuse. Dr. Costello has received research support from the National Institute of Mental Health and the National Institute on Drug Abuse. She is co-author of the following assessment tools: Child and Adolescent Psychiatric Assessment (CAPA), Young Adult Psychiatric Assessment (YAPA), Child and Adolescent Impact Assessment (CAIA), Child and Adolescent Services Assessment (CASA), and Mood and Feelings Questionnaire (MFQ). No personal income is derived from any of these measures. Dr. Shanahan has received research support from the National Institute on Drug Abuse and the National Institute of Child Health and Development.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
This article is discussed in an editorial by Drs. Nancy Whitesell and Carol Kaufman on page xx.
Supplemental material cited in this article is available online.
Contributor Information
Drs. William E. Copeland, Duke University, Durham, NC.
Sherika Hill, Duke University, Durham, NC.
E. Jane Costello, Duke University, Durham, NC.
Dr. Lilly Shanahan, University of North Carolina, Chapel Hill.
References
- 1.Arria AM, Caldeira KM, Bugbee BA, Vincent KB, O’Grady KE. Marijuana use trajectories during college predict health outcomes nine years post-matriculation. Drug Alcohol Depend. 2016;159:158–165. doi: 10.1016/j.drugalcdep.2015.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, Miech RA. Monitoring the future: national survey results on drug use, 1975–2013. I. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2015. (Secondary school students). [Google Scholar]
- 3.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th. Washington, DC: APA; 2013. (DSM-V) [Google Scholar]
- 4.Hasin DS, O’Brien CP, Auriacombe M, et al. DSM-5 criteria for substance use disorders: Recommendations and rationale. Am J Psychiatry. 2013;170:834–851. doi: 10.1176/appi.ajp.2013.12060782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Etz KE, Arroyo JA, Crump AD, Rosa CL, Scott MS. Advancing American Indian and Alaska Native substance abuse research: Current science and future directions. Am J Drug Alcohol Abuse. 2012;38:372–375. doi: 10.3109/00952990.2012.712173. [DOI] [PubMed] [Google Scholar]
- 6.Volkow ND, Warren KR. Advancing American Indian/Alaska Native substance abuse research. Am J Drug Alcohol Abuse. 2012;38:371. doi: 10.3109/00952990.2012.712174. [DOI] [PubMed] [Google Scholar]
- 7.Miller KA, Beauvais F, Burnside M, Jumper-Thurman P. A comparison of American Indian and non-Indian fourth to sixth graders’ rates of drug use. J Ethn Subst Abuse. 2008;7:258–67. doi: 10.1080/15332640802313239. [DOI] [PubMed] [Google Scholar]
- 8.Whitbeck LB, Yu M, Johnson KD, Hoyt DR, Walls ML. Diagnostic prevalence rates from early to mid-adolescence among indigenous adolescents: First results from a longitudinal study. J Am Acad Child Adolesc Psychiatry. 2008;47:890–900. doi: 10.1097/CHI.0b013e3181799609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Whitesell NR, Kaufman CE, Keane EM, Crow CB, Shangreau C, Mitchell CM. Patterns of substance use initiation among young adolescents in a Northern Plains American Indian tribe. Am J Drug Alcohol Abuse. 2012;38:383–388. doi: 10.3109/00952990.2012.694525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Whitesell NR, Beals J, Mitchell CM, et al. Marijuana initiation in 2 American Indian reservation communities: Comparison with a national sample. Am J Public Health. 2007;97:1311–1318. doi: 10.2105/AJPH.2005.071266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brook JS, Kessler RC, Cohen P. The onset of marijuana use from preadolescence and early adolescence to young adulthood. Dev Psychopathol. 1999;11:901–914. doi: 10.1017/s0954579499002370. [DOI] [PubMed] [Google Scholar]
- 12.Perkonigg A, Goodwin RD, Fiedler A, et al. The natural course of cannabis use, abuse and dependence during the first decades of life. Addiction. 2008;103:439–449. doi: 10.1111/j.1360-0443.2007.02064.x. discussic 450–431. [DOI] [PubMed] [Google Scholar]
- 13.Kandel DB, Chen K. Types of marijuana users by longitudinal course. J Stud Alcohol. 2000;61:367–378. doi: 10.15288/jsa.2000.61.367. [DOI] [PubMed] [Google Scholar]
- 14.Poulton R, Moffitt TE, Harrington H, Milne BJ, Caspi A. Persistence and perceived consequences of cannabis use and dependence among young adults: implications for policy. New Zeal Med J. 2001;114:544–547. [PubMed] [Google Scholar]
- 15.Coffey C, Carlin JB, Lynskey MT, Li N, Patton GC. Adolescent precursors of cannabis dependence: findings from the Victorian Adolescent Health Cohort Study. Br J Psychiatry. 2003;182:330–336. doi: 10.1192/bjp.182.4.330. [DOI] [PubMed] [Google Scholar]
- 16.Griffith-Lendering MF, Wigman JT, Prince van Leeuwen A, et al. Cannabis use and vulnerability for psychosis in early adolescence–a TRAILS study. Addiction. 2012;108:733–740. doi: 10.1111/add.12050. [DOI] [PubMed] [Google Scholar]
- 17.Costello EJ, Angold A, Burns B, et al. The Great Smoky Mountains Study of Youth: Goals, designs, methods, and the prevalence of DSM-III-R disorders. Arch Gen Psychiatry. 1996;53:1129–1136. doi: 10.1001/archpsyc.1996.01830120067012. [DOI] [PubMed] [Google Scholar]
- 18.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry. 2003;60:837–44. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- 19.Copeland WE, Angold A, Shanahan L, Costello EJ. Longitudinal patterns of anxiety from childhood to adulthood: The Great Smoky Mountains Study. J Am Acad Child Adolesc Psychiatry. 2014;53:21–33. doi: 10.1016/j.jaac.2013.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Angold A, Costello E. The Child and Adolescent Psychiatric Assessment (CAPA) J Am Acad Child Adolesc Psychiatry. 2000;39:39–48. doi: 10.1097/00004583-200001000-00015. [DOI] [PubMed] [Google Scholar]
- 21.Angold A, Cox A, Prendergast M, et al. The Young Adult Psychiatric Assessment (YAPA) Durham, NC: Duke University Medical Center; 1999. Structures Interview. [Google Scholar]
- 22.Angold A, Costello EJ. A test-retest reliability study of child-reported psychiatric symptoms and diagnoses using the Child and Adolescent Psychiatric Assessment (CAPA-C) Psychological Medicine. 1995;25:755–762. doi: 10.1017/s0033291700034991. [DOI] [PubMed] [Google Scholar]
- 23.Pickles A, Dunn G, Vazquez-Barquero J. Screening for stratification in two-phase (‘two- stage’) epidemiological surveys. Statistical Methods in Medical Research. 1995;4:73–89. doi: 10.1177/096228029500400106. [DOI] [PubMed] [Google Scholar]
- 24.SAS/STAT® Software: Version 9.2 [computer program] Cary, NC: SAS Institute, Inc; 2008. [Google Scholar]
- 25.Substance Abuse and Mental Health Services Administration. Results from the 2011 National Survey on Drug Use and Health: Summary of National Findings NSDUH Series H-44. Rockville, MD: SAMHSA; 2012. (HHS Publication No. (SMA 12-4713)). [Google Scholar]
- 26.Grant BF, Goldstein RB, Saha TD, et al. Epidemiology of DSM-5 alcohol use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA psychiatry. 2015;72:757–766. doi: 10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Farmer RF, Kosty DB, Seeley JR, et al. Natural course of cannabis use disorders. Psychol Med. 2015;45:63–72. doi: 10.1017/S003329171400107X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hasin DS, Kerridge BT, Saha TD, et al. Prevalence and correlates of DSM-5 cannabis use disorder, 2012–2013: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Am J Psychiatry. 2016;173:588–99. doi: 10.1176/appi.ajp.2015.15070907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moffitt TE, Caspi A, Taylor A, et al. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychol Med. 2010;40:899–909. doi: 10.1017/S0033291709991036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Compton WM, Gfroerer J, Conway KP, Finger MS. Unemployment and substance outcomes in the United States 2002–2010. Drug Alcohol Depend. 2014;142:350–353. doi: 10.1016/j.drugalcdep.2014.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peer K, Rennert L, Lynch KG, Farrer L, Gelernter J, Kranzler HR. Prevalence of DSM- IV and DSM-5 alcohol, cocaine, opioid, and cannabis use disorders in a largely substance dependent sample. Drug Alcohol Depend. 2013;127:215–219. doi: 10.1016/j.drugalcdep.2012.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Compton WM, Dawson DA, Goldstein RB, Grant BF. Crosswalk between DSM-IV dependence and DSM-5 substance use disorders for opioids, cannabis, cocaine and alcohol. Drug Alcohol Depend. 2013;132:387–390. doi: 10.1016/j.drugalcdep.2013.02.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Compton WM, Saha TD, Conway KP, Grant BF. The role of cannabis use within a dimensional approach to cannabis use disorders. Drug Alcohol Depend. 2009;100:221–7. doi: 10.1016/j.drugalcdep.2008.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Costello EJ, Erkanli A, Copeland WE, Angold A. Association of family income supplements in adolescence with development of psychiatric and substance use disorders in adulthood among an American Indian population. Jama. 2010;303:1954–1960. doi: 10.1001/jama.2010.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Whitbeck LB, Sittner Hartshorn KJ, Crawford DM, Walls ML, Gentzler KC, Hoyt DR. Mental and substance use disorders from early adolescence to young adulthood among indigenous young people: final diagnostic results from an 8-year panel study. Soc Psychiatry Psychiatr Epidemiol. 2014;49:961–973. doi: 10.1007/s00127-014-0825-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wu LT, Woody GE, Yang C, Pan JJ, Blazer DG. Racial/ethnic variations in substance- related disorders among adolescents in the United States. Arch Gen Psychiatry. 2011;68:1176–85. doi: 10.1001/archgenpsychiatry.2011.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chen P, Jacobson KC. Developmental trajectories of substance use from early adolescence to young adulthood: Gender and racial/ethnic differences. J Adolesc Health. 2012;50:154–163. doi: 10.1016/j.jadohealth.2011.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Swift W, Coffey C, Carlin JB, Degenhardt L, Patton GC. Adolescent cannabis users at 24 years: Trajectories to regular weekly use and dependence in young adulthood. Addiction. 2008;103:1361–1370. doi: 10.1111/j.1360-0443.2008.02246.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Age of onset survival curves for cannabis involvement variables. Note: CUD = cannabis use disorder.


