Abstract
Aim:
The aim of this study was to evaluate the fracture resistance of simulated immature teeth, when the root canals were completely filled either with mineral trioxide aggregate (MTA) or Biodentine, comparing with that of roots filled with apexification procedure.
Materials and Methods:
Sixty mandibular premolar teeth with single, straight canals decoronated at cementoenamel junction were divided into five groups (n = 12 each). Group 1 samples served as negative control and remaining four groups root samples were shaped and cleaned using ProTaper rotary files. To simulate immature roots, a #5 Peeso reamer was passed beyond the apex so that apices were enlarged to a diameter of 1.5 mm. Group 2 and 4 samples were filled with 5 mm of MTA or Biodentine apical plug and backfilling with gutta-percha using AH Plus sealer. Group 3 and 5 root samples were completely obturated with MTA and Biodentine, respectively. All the teeth were loaded vertically until fracture, using the universal testing machine.
Statistical Analysis:
Forces at which fracture of the roots occurred were subjected to statistical analysis using SPSS/PC version 2 software, and the results were analyzed with the one-way analysis of variance and Newman–Keuls multiple post hoc test.
Results:
Complete root canal obturation with MTA or Biodentine has shown significantly higher fracture resistance (P < 0.05) when compared to apexification with MTA or Biodentine.
Conclusion:
Obturation of the root canals with bioactive materials has shown highest fracture resistance when compared to apexification groups.
Keywords: Apexification, biodentine, mineral trioxide aggregate, universal testing machine, vertical root fracture
INTRODUCTION
Dental impact injuries most often occur in children, between the ages of 8 and 12 years, where the teeth are still in the process of maturing. These injuries often lead to pulpal necrosis, which usually results in the cessation of root formation in developing roots, producing immature root apex.[1] Pulpal necrosis of an immature tooth will necessitate endodontic treatment, which can pose both endodontic and restorative challenges, because of incomplete closure of the apex and thin dentinal walls. In open-apex roots, due to large apical diameter and smaller coronal canal diameter, debridement of the root canal becomes difficult. Lack of apical stop makes working length determination and obturation difficult, and also the thin root canal walls are always prone to fracture. It has been pointed out that endodontically treated immature teeth have a relatively high (>60%) incidence of cervical root fractures, either spontaneously or due to minor impacts. The thinner the root dentin, the more likely is the tooth to fracture. These fractures lead to postendodontic tooth repairs and extractions.[2]
Management of open apices in pulpless immature teeth has historically been accomplished through apexification, using long-term calcium hydroxide (Ca[OH]2), to induce calcific bridge formation at the apex with success rate ranging from 79% to 96%.[3] It was demonstrated that the long-term use of Ca (OH)2 (up to 18 months) may weaken the dentin and thus making the roots more susceptible to fracture.[1] Other alternatives to Ca (OH)2 have been proposed, the most promising being recently developed calcium silicate-based materials, such as mineral trioxide aggregate (MTA) and Biodentine. These root-end repair materials have been claimed to be biocompatible, capable of stimulating biomineralization, and offer a superior seal with better bond strength.[4]
MTA has shown promising results as an apical barrier with open apex when compared to Ca (OH)2, and it favored the occurrence of apexification and periapical healing.[5] Biodentine is a silicate-based biologically active cement which has dentin-like mechanical properties and designed as a “dentin replacement” material. This material is actually formulated using the MTA-based cement technology while improving its physical and mechanical properties.[6] It has been reported that Biodentine as an apical plug and backfilling the canal with fiber post provided better fracture resistance of simulated immature teeth.[7]
Establishment of a proper fracture resistance to the root dentin, when obturated with different obturating materials, is an important key point for clinical success. Based on these considerations, the aim of this in vitro study was to compare and evaluate the influence of MTA and Biodentine as obturating materials on the fracture resistance of immature teeth. The null hypothesis was that there will be no difference between the tested materials in providing the fracture resistance of immature teeth.
MATERIALS AND METHODS
Sixty noncarious, single-rooted mandibular premolar teeth, with approximately similar buccolingual and mesiodistal dimensions, were selected for the study. After extraction, all the collected teeth were immersed in 5% sodium hypochlorite (NaOCl) solution for 2 h, for surface disinfection and dissolution of the superficial soft tissue. Preoperative radiographs and surgical loupes (STAC Clip-On Loupe, SC250, Canada) at ×3.5 magnification were used to ensure that the collected teeth did not have root caries or restorations, open apices, calcifications, fractures, or craze lines. Then, each experimental tooth was decoronated at 1 mm coronal to the cementoenamel junction (CEJ), using a flexible diamond disk (Novo Dental Products, Mumbai, India) in a slow-speed handpiece, under a copious amount of water coolant. The root of each tooth was standardized to a length of 12 mm as measured from the apex to the facial CEJ.
Grouping method
The sixty experimental root samples were randomly divided into five groups:
Group 1 (n = 12): Sound teeth with no root canal treatment (negative control)
Group 2 (n = 12): MTA apical plug and backfilling with gutta-percha
Group 3 (n = 12): Filling of root canal system completely with MTA
Group 4 (n = 12): Biodentine apical plug, and backfilling with gutta-percha
Group 5 (n = 12): Root canals completely filled with Biodentine.
Cleaning and shaping of the root canals
For all the test root samples, coronal access was prepared using #245 bur in a high-speed handpiece, and the canal patency was checked by inserting endodontic explorer DG-16 and #10 K-file (Dentsply Maillefer, Switzerland). The working length was determined and cleaning and shaping of the root canals were completed with ProTaper rotary Ni-Ti files (Dentsply Maillefer, Switzerland) upto F3 (#30/09) at a speed of 300 rpm using an Endo-Mate Endo Motor System (NSK NAKANISHI INC. Kanuma-Shi, Tochigi, Japan). The canals were irrigated with 2 ml of 3% NaOCl, after each instrumentation, using 27-gauge side vented needle and syringe.
To simulate immature roots with open apexes, #1–5 Peeso reamers were used. A #5 Peeso reamer was passed beyond the apex so that apices were enlarged to a diameter of 1.5 mm. Following cleaning and shaping, all the root canals were irrigated with 5 ml of normal saline. Before the obturation, the root canals in all the root samples were irrigated with 17% ethylenediamine tetraacetic acid (EDTA) (Canalarge, Ammdent, Mohali, India) for 1 min to remove the smear layer. A final flush was done with 5 ml of normal saline and excess moisture from the canals was removed with sterile absorbent points.
Obturation of the root canals
In Group 2 root samples, ProRoot MTA (Dentsply Tulsa, Germany) mix was placed into the canal with MTA messing gun and advanced apically with endodontic pluggers of different sizes 9/11, 5/7, 1/3 (Dentsply Maillefer, Germany), and 5 mm thickness of the apical plug was maintained. After 24 h, remaining part of the root canals was obturated with F3 master gutta-percha point and AH Plus sealer. In Group 3 samples, 5 mm of MTA apical barrier was placed and then the remaining canal was filled with MTA up to 1 mm short of CEJ. In Group 4 root samples, an apical plug of 5 mm with Biodentine and backfilling with gutta-percha and AH Plus sealer was done. In Group 5, Biodentine apical plug was prepared, and immediately, remaining coronal part of the canal was filled with Biodentine. For all the experimental root samples, postobturation radiographs were taken in both labiolingual and mesiodistal directions, to ensure homogeneous, adequate root filling without voids. The filled roots were stored in an incubator for 1 month at 37°C and 100% relative humidity, to allow the obturating materials to set completely.
To stimulate periodontal ligament lining the root surfaces, utility wax was liquefied at a temperature of 70°C and applied on the roots with a paint brush up to 2 mm below CEJ, until a homogeneous wax thickness of 0.3 mm was obtained. The specimens were then embedded in metal matrices containing autopolymerizing acrylic resin. After curing, the specimens were removed from the matrices and wax was detached from the root surface and from the space created in the acrylic resin. Later, polyether elastomeric material (AD-Sil, prime Dental products pvt. LTD, Thane, India) was manipulated and inserted into this space. The specimens were repositioned in acrylic resin blocks, and the excess polyether was removed using a scalpel.
Fracture resistance evaluation
Fracture resistance was evaluated using the universal testing machine. A cylindrical ball indenter of 2.2 mm diameter, with a sharpened conical tip, was attached to the upper part of the universal testing machine to apply force to the root causing vertical root fracture. The root was centered under the plunger on the lower platen, and the plunger was driven downward exactly along the long axis of the root. A vertical load was applied at a crosshead speed of 0.5 mm/min until the root fractured. The maximum load at the time of fracture recorded in Newtons was then converted into ^Mega pascals (MPA) using the formula:
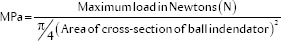
Where π = 3.14 (constant value).
Statistical analysis
All the collected data of forces at which fracture of teeth occurred in MPa were subjected to statistical analysis using SPSS/PC version 20 software (IBM). A one-way analysis of variance was used to compare the forces at which the fracture of roots obturated with different materials occurred. Pair-wise comparison of five groups was performed by Newman–Keuls multiple post hoc procedure. Statistical analysis was performed at 95% level of confidence.
RESULTS
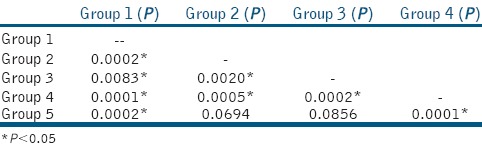
The mean fracture resistance value was higher in Group 1 (control group, without instrumentation) when compared to experimental groups with statistically significant difference (P < 0.05) [Table 1]. In experimental groups, the mean fracture resistance value was higher in Group 3 (root canals completely obturated with MTA) when compared to Group 5 (root canals obturated completely with Biodentine) with no statistically significant difference between them, P > 0.05 [Table 2]. Significantly lower mean fracture resistance value was observed for Group 4 (Biodentine apexification group).
Table 1.
Group statistics :-Mean, Standard Deviation, Standard Error and Coefficient of Variation of fracture resistance values in MPa for the experimental and control groups
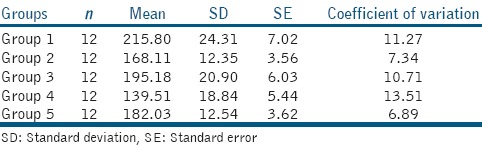
Table 2.
Pair wise comparisons of five groups (1, 2, 3, 4, 5) with respect to fracture resistance (Mpa) by Newman-Keuls multiple posthoc procedure
DISCUSSION
The open apex typically occurs when the pulp undergoes necrosis as a result of caries or trauma, before root growth and development are complete. It can also occasionally form in a mature apex as a result of extensive apical resorption due to orthodontic treatment, periapical pathosis, over instrumentation during conventional root canal therapy or root end resection during periradicular surgery.
When restoring immature teeth, single-visit apexification using an MTA barrier offers several advantages over conventional apexification. These include fewer appointments for the patient and development of an immediate apical seal and less potential to weaken the tooth structure compared with long-term Ca (OH)2. MTA offers a biologically active substrate for bone cells and stimulates interleukin production because of its alkaline pH and calcium ion release and initiates the calcific bridge formation within the first postoperative week.[5] However, apexification with MTA has several disadvantages such as difficult handling characteristics, prolonged setting time, potential coronal discoloration, and less compressive strength when compared to dentine and Biodentine.[7]
During apexification procedure, the most common disadvantage when gutta-percha is used as a backfilling material is microleakage.[8] Research indicated that no known method with various techniques of cold or warm compaction of gutta-percha can predictably produce a coronal bacterial-tight seal, when the material is exposed to microorganisms and their by-products.[9] Thus, the current trend in endodontic research is to explore various alternatives to gutta-percha as obturating material.
Studies revealed that MTA apexification and backfilling with gutta-percha will have less fracture resistance than MTA apexification and backfilling with different types of prefabricated intracanal metal posts or fiber posts.[10,11] One study stated that there is no statistical difference between MTA apexification with gutta-percha backfilling and complete root canal obturation with MTA.[12] Considering these varied results, the present study compared the complete root canal obturation using Biodentine or MTA. Mandibular premolars were used which has a circular cross-section in the mid to apical region that would result in uniform distribution of load to fracture. They also simulate the clinical situation better, where chewing forces are maximum.
Removal or retention of smear layer before canal obturation still remains controversial. Some studies stated that smear layer might act as a coupling agent enhancing MTA bonding to root dentin.[13] However, recent studies stated that the removal of smear layer must be done with 17% EDTA to improve the sealing ability of MTA.[14] Hence, in the present study, 17% EDTA was used to remove the smear layer before obturating the canals. To simulate the periodontal ligament, polyether impression material was used as it prevents stress concentration in one particular region and transfers the stresses produced by load application all over the root surface.[15]
The mean bond strength values were higher for control group when compared to the experimental groups with a statistical difference. Contrary to these findings, few studies concluded that control group exhibits less fracture resistance than the canals completely obturated with MTA.[5,16] Furthermore, it appears that long-term (tested for 1 year period) placement of MTA in the canal system not only provides increased resistance to fracture but also increases the strength of the tooth with time. Researchers postulated that MTA might prevent the destruction of collagen by inducing the expression of a tissue inhibition of metalloproteinase-2 (TIMP-2) in the dentin matrix. According to histological analysis, expression of collagen type I, matrix metalloproteinase (MMP)-2, -14, and TIMP-2 on the dentin were noticed in MTA-treated teeth. TIMP-2 prevented the organic matrix from degradation caused by MMP-2, -14.[13] Therefore, Hatibovic-Kofman et al.[17] stated that the reason for high fracture resistance of dentin at long-term MTA placement might lie in the inhibitor activities of TIMP-2 and reduced expression of MMP-2, -14 in the dentine matrix.
The mean fracture resistance values were higher for root canals obturated completely with MTA when compared to Biodentine, but the difference was not statistically significant. This finding was in accordance with the results of the study conducted by Elnaghy and Elsaka.[18] Biodentine has high compressive strength, reduced setting time (9–12 min), and less solubility and better handling characteristics when compared to MTA. A specific feature of Biodentine is its capacity to continue improving the compressive strength with time over several days. It reaches up to 300 MPa after 1 month, which is almost equal to that of the compressive strength of natural dentin (297 MPa).[19]
A finite element analysis study showed that the materials with similar elastic modulus to dentin could reinforce the weak roots. This hypothesis can explain the failure of gutta-percha to reinforce immature roots. The elastic modulus of Portland cements is around 15–30 GPa and dentin which is about 14–18.6 GPa and for Biodentine is 22.0 GPa, and thus, the reinforcing effect of MTA and Biodentine may be explained by their similar elastic modulus to dentin.[16] The mean fracture resistance values were higher for MTA apexification group when compared to Biodentine apexification group, and the difference between them is statistically significant. This can be attributed to the superior sealing ability of MTA when compared to Biodentine.
The present mechanical testing was performed with greater effort to simulate the exact clinical conditions and to achieve standardization. However, in vitro conditions do not completely reflect in vivo conditions. The teeth used in the present study may simulate the shape of immature teeth but may not simulate the tissue composition and physical properties exactly. The ability of these materials to reinforce the immature teeth should be evaluated clinically in future.
CONCLUSION
Complete obturation of the root canals with bioactive materials (MTA/Biodentine) has improved the fracture resistance of immature teeth when compared to apexification groups. Further in vivo and in vitro studies are necessary to support the efficacy of MTA and Biodentine as a root canal filling materials.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Andreasen JO, Farik B, Munksgaard EC. Long-term calcium hydroxide as a root canal dressing may increase risk of root fracture. Dent Traumatol. 2002;18:134–7. doi: 10.1034/j.1600-9657.2002.00097.x. [DOI] [PubMed] [Google Scholar]
- 2.Peroz I, Dent M, Blankenstein F, Lang KP, Nauman M. Restoring endodontically treated teeth with posts and cores – A review. Quintessence Int. 2005;36:737–46. [PubMed] [Google Scholar]
- 3.Damle SG, Bhattal H, Loomba A. Apexification of anterior teeth: A comparative evaluation of mineral trioxide aggregate and calcium hydroxide paste. J Clin Pediatr Dent. 2012;36:263–8. [PubMed] [Google Scholar]
- 4.Felippe WT, Felippe MC, Rocha MJ. The effect of mineral trioxide aggregate on the apexification and periapical healing of teeth with incomplete root formation. Int Endod J. 2006;39:2–9. doi: 10.1111/j.1365-2591.2005.01037.x. [DOI] [PubMed] [Google Scholar]
- 5.Andreasen JO, Munksgaard EC, Bakland LK. Comparison of fracture resistance in root canals of immature sheep teeth after filling with calcium hydroxide or MTA. Dent Traumatol. 2006;22:154–6. doi: 10.1111/j.1600-9657.2006.00419.x. [DOI] [PubMed] [Google Scholar]
- 6.Malkondu Ö, Karapinar Kazandag M, Kazazoglu E. A review on biodentine, a contemporary dentine replacement and repair material. Biomed Res Int 2014. 2014:160951. doi: 10.1155/2014/160951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Topçuoglu HS, Kesim B, Düzgün S, Tuncay Ö, Demirbuga S, Topçuoglu G. The effect of various backfilling techniques on the fracture resistance of simulated immature teeth performed apical plug with Biodentine. Int J Paediatr Dent. 2015;25:248–54. doi: 10.1111/ipd.12137. [DOI] [PubMed] [Google Scholar]
- 8.Fransen JN, He J, Glickman GN, Rios A, Shulman JD, Honeyman A. Comparative assessment of ActiV GP/glass ionomer sealer, Resilon/Epiphany, and gutta-percha/AH plus obturation: A bacterial leakage study. J Endod. 2008;34:725–7. doi: 10.1016/j.joen.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 9.Siqueira JF, Jr, Rôças IN, Favieri A, Abad EC, Castro AJ, Gahyva SM. Bacterial leakage in coronally unsealed root canals obturated with 3 different techniques. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:647–50. doi: 10.1067/moe.2000.110412. [DOI] [PubMed] [Google Scholar]
- 10.Tanalp J, Dikbas I, Malkondu O, Ersev H, Güngör T, Bayirli G. Comparison of the fracture resistance of simulated immature permanent teeth using various canal filling materials and fiber posts. Dent Traumatol. 2012;28:457–64. doi: 10.1111/j.1600-9657.2011.01098.x. [DOI] [PubMed] [Google Scholar]
- 11.Dikbas I, Tanalp J, Koksal T, Yalniz A, Güngör T. Investigation of the effect of different prefabricated intracanal posts on fracture resistance of simulated immature teeth. Dent Traumatol. 2014;30:49–54. doi: 10.1111/edt.12034. [DOI] [PubMed] [Google Scholar]
- 12.Bortoluzzi EA, Souza EM, Reis JM, Esberard RM, Tanomaru-Filho M. Fracture strength of bovine incisors after intra-radicular treatment with MTA in an experimental immature tooth model. Int Endod J. 2007;40:684–91. doi: 10.1111/j.1365-2591.2007.01266.x. [DOI] [PubMed] [Google Scholar]
- 13.Bogen G, Kuttler S. Mineral trioxide aggregate obturation: A review and case series. J Endod. 2009;35:777–90. doi: 10.1016/j.joen.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 14.Pace R, Giuliani V, Nieri M, Di Nasso L, Pagavino G. Mineral trioxide aggregate as apical plug in teeth with necrotic pulp and immature apices: A 10-year case series. J Endod. 2014;40:1250–4. doi: 10.1016/j.joen.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 15.Soares CJ, Pizi EC, Fonseca RB, Martins LR. Influence of root embedment material and periodontal ligament simulation on fracture resistance tests. Braz Oral Res. 2005;19:11–6. doi: 10.1590/s1806-83242005000100003. [DOI] [PubMed] [Google Scholar]
- 16.Milani AS, Rahimi S, Borna Z, Jafarabadi MA, Bahari M, Deljavan AS. Fracture resistance of immature teeth filled with mineral trioxide aggregate or calcium-enriched mixture cement: An ex vivo study. Dent Res J (Isfahan) 2012;9:299–304. [PMC free article] [PubMed] [Google Scholar]
- 17.Hatibovic-Kofman S, Raimundo L, Zheng L, Chong L, Friedman M, Andreasen JO. Fracture resistance and histological findings of immature teeth treated with mineral trioxide aggregate. Dent Traumatol. 2008;24:272–6. doi: 10.1111/j.1600-9657.2007.00541.x. [DOI] [PubMed] [Google Scholar]
- 18.Elnaghy AM, Elsaka SE. Fracture resistance of simulated immature teeth filled with biodentine and white mineral trioxide aggregate – An in vitro study. Dent Traumatol. 2015;15:32–5. doi: 10.1111/edt.12224. [DOI] [PubMed] [Google Scholar]
- 19.Vipin A, Vineeta N, Namrata S, Pooja A. Bioactive dentin replacement. J Dent and Med Sci. 2013;12:51–7. [Google Scholar]


