Abstract
Objective:
The objective of this study is to evaluate the fracture resistance of newer restorative materials that could serve as an alternate to crown coverage.
Materials and Methods:
Forty extracted human mandibular molar teeth were selected for this study and were divided into four groups (n = 10). All the teeth in the experimental groups (Group 2–4) were subjected to access cavity preparation with roughly 1.5 mm of tooth structure remaining throughout the circumference. Group 1: Intact teeth used as control. Group 2: Access cavities reinforced with biodentine. Group 3: Inner circumference of access cavities reinforced with polyethylene fiber and nano-hybrid composite. Group 4: Access cavities were reinforced with fiber reinforced composite. All the teeth were subjected to fracture resistance using universal testing machine.
Results:
The results of the study were evaluated statistically using one-way ANOVA and Tukey post hoc test. Group 2 demonstrated the least mean values of fracture resistance and was significantly different from the control and other experimental groups. Statistically significant difference among Groups 1, 3, and 4 was not found.
Conclusion:
Within the limitation of this in vitro study, it can be concluded that fiber reinforced composite and polyethylene fibers with nanohybrid composite could serve as an alternate to crown coverage.
Keywords: Biodentine, fiber reinforced composite, nanohybrid composite, polyethylene fibers
INTRODUCTION
The restoration of endodontically treated teeth is one of the topics studied extensively and is controversial in dentistry. Diverse opinions remain about clinical procedures and materials to be used to restore these teeth, once fractures occur. Fractures are more common in pulpless teeth than teeth with vital pulps although some authors have related a little difference at the fracture incidence between nonendodontically treated versus endodontically treated teeth in Chinese patients.[1] Studies have proposed that because of loss of water and collagen cross-linking the dentin in endodontically treated teeth is substantially different and also is supposed to be more brittle than in vital teeth.[2] Previous studies compared the physical and mechanical properties of dentine specimens and concluded that neither dehydration nor endodontic treatment affected the properties of dentin.[3]
Restoration of endodontically treated teeth is common procedure in everyday clinical practice. Even though extensive research has been done on this subject, it has been difficult to arrive at a particular solution as to what type of restorative procedure gives the greatest success.[4] Whether full cast crowns, especially in posterior teeth, are indeed compulsory or not after endodontic treatment has been a subject of debate for some time now. Although crown restoration has been suggested as a means to strengthen a tooth after endodontic treatment, tooth fractures have been unavoidable despite the crown placement.[5] Hence, an in vitro study was carried out to determine whether advanced restorative materials would be an alternate to crown coverage. The present study compares the resistance to fracture of endodontically treated mandibular molars with extensive access cavity preparations restored with three different restorative materials.
MATERIALS AND METHODS
Forty intact noncarious mandibular molars which were extracted due to periodontal reasons were collected for this in vitro study. To rule out any defective teeth they were examined under an operating microscope (Global Surgical Corporation, Saint Louis, USA) at ×12.8 magnifications and only sound teeth without any fracture lines or cracks were selected for the study. The teeth were stored in physiological saline until the study was done. To achieve standardization and to minimize the influence of variations in size and shape on the results, the teeth were selected based on their mesiodistal (10.5 ± 1 mm) and buccolingual (9.5 ± 1 mm) dimensions and randomly distributed into four groups of ten teeth each.
Group 1: The teeth in this group were not subjected to either access cavity preparation or biomechanical preparation and were used as control.
All the teeth in the experimental groups (Group 2–4) were subjected to access cavity preparation with roughly 1.5 mm of tooth structure remaining throughout the circumference [Figure 1a]. This preparation was done to simulate access preparations in teeth with extensive occlusal caries. The canals of all the experimental teeth were prepared to a size F1 ProTaper Rotary (Dentsply, Mumbai, India) and were obturated with the respective ProTaper gutta-percha (Dentsply, Mumbai, India) and AH Plus (DeTrey, Switzerland) sealer. In Group 2, the access cavities were restored with biodentine as postobturation restoration. In Group 3, the access cavities were conditioned with 37% phosphoric acid (3M ESPE, Bangalore, India) and bonding agent applied (Adper, 3M ESPE, Bangalore, India) and cured according to manufacturer's instruction. A strip of premeasured polyethylene fiber (Ribbond, Seattle, WA, USA) was placed against the entire inner circumference of the remaining weakened tooth structure with the help of a thin layer of flowable posterior composite (G-ænial Universal Flo, GC India) [Figure 1b]. Later, the entire access cavity was filled with nanohybrid composite (Nexcomp, METABIOMED, Chungbuk, Korea South) [Figure 1c]. In Group 4, the same protocol of etching and bonding was performed as that of Group 3, but the access cavity was restored with fiber reinforced posterior composite material (everX Posterior, Dentsply, Mumbai, India) as base and occlusal 1 mm layer of Filtek Z350 XT (3M ESPE, Bangalore, India) was placed to achieve better finishing and polishing to simulate the clinical situation. Each tooth was coated with a layer of polyvinyl siloxane impression material (EXAFLEX, GC America Inc., USA) and was embedded in a block of self-curing acrylic resin (Tempron, GC India) with the long axis of the tooth perpendicular to the base of the block. All the teeth were stored in an incubator at 37°C and 100% humidity until subjected to fracture resistance. Static fracture resistance testing was performed using a universal testing machine (Instron India Pvt Ltd., Chennai). A 5 mm diameter round tip stainless steel metal rod was positioned parallel to the long axis of the teeth and centered over the teeth until the bar just slightly contacted the occlusal surface. Compressive loading of the teeth was performed at a crosshead speed of 1 mm/min, and the force necessary to fracture each tooth was recorded in Newton's. The results of the study were evaluated statistically using SPSS 11.5 statistical software (SPSS Corp., Chicago, IL, USA). One-way ANOVA and Tukey post hoc test were applied. P values were computed and compared with statistical significance at the level of 0.05.
Figure 1.
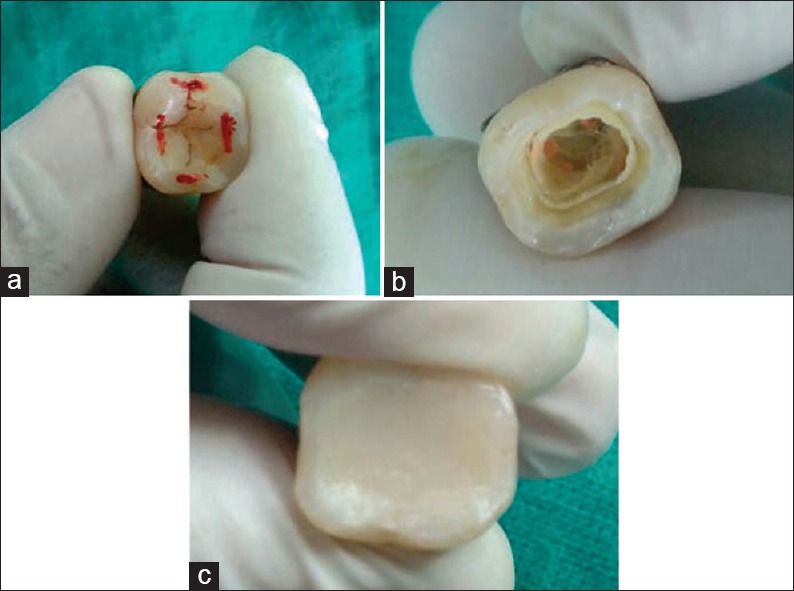
(a) Marking extent of access cavity, (b) reinforcing access cavity with premeasured polyethylene fiber, (c) access restored with nano hybrid composite
RESULTS
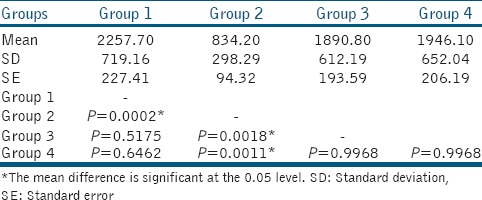
The mean of the fracture resistance values and the standard deviation for each group are presented in Table 1. The mean fracture resistance value of Group 4 was slightly higher than the mean value of Group 3. The mean value of fracture resistance of Group 1 (intact teeth specimens) was higher than the other groups. Group 2 demonstrated the least mean value of fracture resistance and was significantly different from the control and other experimental groups. A significant difference between Groups 1, 3, and 4 was not found.
Table 1.
Comparison of fracture resistance among experimental groups
DISCUSSION
The remaining coronal tooth structure and functional requirement are crucial in deciding the type of restorative material and the technique to restore endodontically treated teeth are.[6] The decrease in fracture resistance of all occlusal cavity preparations in proportion to the width of the preparation has been established in restorative dentistry.[7] Similar concept was later suggested to endodontics, stating that the cuspal deflection was proportionally greater with the increase in cavity size and was greatest in the presence of an endodontic cavity.[8]
In recent years, Clark and Khademi[9] have described a modified endodontic cavity concept with minimal tooth structure removal intended to improve fracture resistance of root-filled teeth. Our study had a methodology of large access cavity preparation simulating a clinical condition of extensive caries.
Earlier, the methodology adopted in restoring an endodontically treated was based on experimental exercise, the results of which were not always predictable.[10] The structural integrity of teeth in nonvital and root canal treated teeth is lost, which may contribute to tooth fracture.[11] The largest reduction in the tooth stiffness results from additional preparation, especially the loss of marginal ridges.[12]
A retrospective cohort study by Nagasiri and Chitmongkolsuk indicated that endodontically treated molars that are intact (except for the access opening) could be restored successfully using composite restorations.[13] Another study compared the clinical success of 1273 endodontically treated anterior teeth with a follow-up of 25 years. It was concluded that coronal coverage crowns did not significantly improve the fracture resistance.[14]
A finite element analysis study was conducted by Zelic et al. to determine weakening of the tooth regarding extent of cavity preparation. They concluded that access cavity preparation had the greatest influence on tooth strength while canal enlargement did not contribute to this process significantly.[15]
The present study was designed to evaluate whether an alternate to crown coverage can be considered in strengthening an endodontically treated tooth mimicking an extensive loss of crown structure due to caries. Considering the functionary requirement and placement of the tooth in the arch, mandibular molars were selected for this in vitro study.[16]
The remaining dentin thickness offers a sound base required for tooth restoration. Its structural strength depends on the quality and integrity of its anatomic form, hence the key problem is the decreased quantity of sound dentin remaining to retain and support the restoration.[1] Therefore, selecting an appropriate restorative material and technique to compensate for the loss of coronal tooth structure is fundamental to restorative success.
In this study, the strength of the teeth was reduced significantly after access cavity preparation, as shown in previous studies.[6,12] Therefore, reinforcement of the access cavity with a restorative material is necessary to support the remaining tooth structure.
Biodentine was one of postendodontic restorative material chosen as it is considered a dentine substitute. It sets within 12 min, which facilitates its use in immediate crown restoration. Its properties such as elastic modulus, compressive strength and micro hardness is very similar to that of natural dentin. It exhibits good bacterial tight seal with the margins of the tooth structure.[17] Furthermore, in a study by Koubi et al.,[18] Biodentine was used as a posterior restoration and revealed satisfactory surface properties such as good marginal adaptation until 6 months and later covered by a surface layer of composite. The statistical results of the study demonstrated lower fracture resistance than the control and experimental groups, but the mean value was at par with the bite force values as demonstrated by Regalo et al.[19]
In the present study, it was assumed that placing a strip of 3 mm Ribbond fiber against the inner circumference of the experimental teeth (Group 3) would increase the fracture resistance. This was conceived on the concept that the presence of polyethylene network would create a change in the stress dynamics at the restoration/adhesive resin interface. The higher modulus of elasticity and lower flexural modulus of the polyethylene fiber might have a modifying effect on how the interfacial stresses are developed along the restoration/tooth interface.[20] The experimental Group 3 demonstrated fracture resistance which was very close to the control group (intact teeth). The nanohybrid composite material used in the study has been reported to have less polymerization shrinkage, good compressive, and flexure properties.[21]
The experimental teeth in Group 4 were restored with FRC as base and covered with 1 mm layer of Z 350 nanocomposite. The mean values of fracture resistance were slightly less than that of control and marginally greater than the Group 3, although statistically there was no significant difference found.
The results achieved can be associated with previous studies which concluded that the volume fraction or thickness of short fiber composite could contribute to the crack propagation and load-bearing capacity.[22] These innovative materials and techniques enable the clinician to approach old problems from a different perspective and thereby achieve unique and innovative solutions.
Although there is inadequate evidence to support or negate the effectiveness of conventional fillings over crowns for the restoration of root filled teeth, clinicians should continue to base decisions on how to restore such teeth on their own clinical experience as well as the preferences of their patients. The most important aspect regarding the choice of restoration depends immensely on the amount of remaining tooth which may influence long-term survival and cost.[23]
CONCLUSION
Within the limitations of this in vitro study, it can be concluded that both FRC and polyethylene fibers (Ribbond) could be considered as an alternate to crown coverage, considering the insignificant difference in the values of fracture resistance when compared to that of natural tooth.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Assif D, Gorfil C. Biomechanical considerations in restoring endodontically treated teeth. J Prosthet Dent. 1994;71:565–7. doi: 10.1016/0022-3913(94)90438-3. [DOI] [PubMed] [Google Scholar]
- 2.Carter JM, Sorensen SE, Johnson RR, Teitelbaum RL, Levine MS. Punch shear testing of extracted vital and endodontically treated teeth. J Biomech. 1983;16:841–8. doi: 10.1016/0021-9290(83)90008-8. [DOI] [PubMed] [Google Scholar]
- 3.Sedgley CM, Messer HH. Are endodontically treated teeth more brittle? J Endod. 1992;18:332–5. doi: 10.1016/S0099-2399(06)80483-8. [DOI] [PubMed] [Google Scholar]
- 4.Llena-Puy MC, Forner-Navarro L, Barbero-Navarro I. Vertical root fracture in endodontically treated teeth: A review of 25 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:553–5. doi: 10.1067/moe.2001.117262. [DOI] [PubMed] [Google Scholar]
- 5.Eckerbom M, Magnusson T, Martinsson T. Reasons for and incidence of tooth mortality in a Swedish population. Endod Dent Traumatol. 1992;8:230–4. doi: 10.1111/j.1600-9657.1992.tb00249.x. [DOI] [PubMed] [Google Scholar]
- 6.Türp JC, Heydecke G, Krastl G, Pontius O, Antes G, Zitzmann NU. Restoring the fractured root-canal-treated maxillary lateral incisor: In search of an evidence-based approach. Quintessence Int. 2007;38:179–91. [PubMed] [Google Scholar]
- 7.Mondelli J, Steagall L, Ishikiriama A, de Lima Navarro MF, Soares FB. Fracture strength of human teeth with cavity preparations. J Prosthet Dent. 1980;43:419–22. doi: 10.1016/0022-3913(80)90213-9. [DOI] [PubMed] [Google Scholar]
- 8.Panitvisai P, Messer HH. Cuspal deflection in molars in relation to endodontic and restorative procedures. J Endod. 1995;21:57–61. doi: 10.1016/s0099-2399(06)81095-2. [DOI] [PubMed] [Google Scholar]
- 9.Clark D, Khademi J. Modern molar endodontic access and directed dentin conservation. Dent Clin North Am. 2010;54:249–73. doi: 10.1016/j.cden.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 10.Smith CT, Schuman N. Restoration of endodontically treated teeth: A guide for the restorative dentist. Quintessence Int. 1997;28:457–62. [PubMed] [Google Scholar]
- 11.Randow K, Glantz PO. On cantilever loading of vital and non-vital teeth. An experimental clinical study. Acta Odontol Scand. 1986;44:271–7. doi: 10.3109/00016358609004733. [DOI] [PubMed] [Google Scholar]
- 12.Larson TD, Douglas WH, Geistfeld RE. Effect of prepared cavities on the strength of teeth. Oper Dent. 1981;6:2–5. [PubMed] [Google Scholar]
- 13.Nagasiri R, Chitmongkolsuk S. Long-term survival of endodontically treated molars without crown coverage: A retrospective cohort study. J Prosthet Dent. 2005;93:164–70. doi: 10.1016/j.prosdent.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 14.Sorensen JA, Martinoff JT. Intracoronal reinforcement and coronal coverage: A study of endodontically treated teeth. J Prosthet Dent. 1984;51:780–4. doi: 10.1016/0022-3913(84)90376-7. [DOI] [PubMed] [Google Scholar]
- 15.Zelic K, Vukicevic A, Jovicic G, Aleksandrovic S, Filipovic N, Djuric M, et al. Mechanical weakening of devitalized teeth: Three-dimensional finite element analysis and prediction of tooth fracture. Int Endod J. 2015;48:850–63. doi: 10.1111/iej.12381. [DOI] [PubMed] [Google Scholar]
- 16.Chan CP, Lin CP, Tseng SC, Jeng JH. Vertical root fracture in endodontically versus nonendodontically treated teeth: A survey of 315 cases in Chinese patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:504–7. doi: 10.1016/s1079-2104(99)70252-0. [DOI] [PubMed] [Google Scholar]
- 17.Camilleri J. Investigation of Biodentine as dentine replacement material. J Dent. 2013;41:600–10. doi: 10.1016/j.jdent.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 18.Koubi G, Colon P, Franquin JC, Hartmann A, Richard G, Faure MO, et al. Clinical evaluation of the performance and safety of a new dentine substitute, Biodentine, in the restoration of posterior teeth – A prospective study. Clin Oral Investig. 2013;17:243–9. doi: 10.1007/s00784-012-0701-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Regalo SC, Santos CM, Vitti M, Regalo CA, de Vasconcelos PB, Mestriner W, Jr, et al. Evaluation of molar and incisor bite force in indigenous compared with white population in Brazil. Arch Oral Biol. 2008;53:282–6. doi: 10.1016/j.archoralbio.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 20.Rudo DN, Karbhari VM. Physical behaviors of fiber reinforcement as applied to tooth stabilization. Dent Clin North Am. 1999;43:7–35, v. [PubMed] [Google Scholar]
- 21. [Last accessed on 2015 Dec 18]. Available from: http://www.meta.biomed.com/eng/cnt/prod/prod020101.html?uid=33&cateID=2 .
- 22.Garoushi S, Säilynoja E, Vallittu PK, Lassila L. Physical properties and depth of cure of a new short fiber reinforced composite. Dent Mater. 2013;29:835–41. doi: 10.1016/j.dental.2013.04.016. [DOI] [PubMed] [Google Scholar]
- 23.Fedorowicz Z, Carter B, de Souza RF, Chaves CA, Nasser M, Sequeira-Byron P. Single crowns versus conventional fillings for the restoration of root filled teeth. Cochrane Database Syst Rev. 2012;16:CD009109. doi: 10.1002/14651858.CD009109.pub2. [DOI] [PubMed] [Google Scholar]


