Abstract
Background:
Bladder dysfunction can affect up to 75% of people with multiple sclerosis (MS) on several important life domains. It is a multifaceted problem that remains underdiagnosed by health-care professionals. The aims of this study were to understand the perceptions of Irish health-care professionals regarding bladder dysfunction and to explore current service provision for people with MS.
Methods:
Two focus groups, three dyadic interviews, and one semistructured interview with 14 health-care professionals lasting up to 90 minutes were audio-recorded. Participants included eight physiotherapists, two occupational therapists, three nurses, and one clinical case manager from acute and community settings.
Results:
Thematic analysis of transcripts yielded two key themes. The first theme involves the underlying beliefs of health-care professionals, their clinical practice, and experiential knowledge in the model of clinical practice development in relation to bladder management. The second theme addresses the pivotal points in this model where change can be implemented to optimize bladder management. The first element of change encompasses the interaction between clinical practice and experiential knowledge of health-care professionals. The second element of change incorporates how acknowledgment of individual beliefs of health-care professionals can further inform clinical practice and experiential knowledge.
Conclusions:
These findings suggest that health-care professionals need to be aware of their beliefs in relation to bladder dysfunction. Examining these beliefs may influence how people with MS access health service provision for this disabling symptom. This type of reflexive practice may facilitate changes to existing perceptions and reduce the reluctance to discuss bladder symptoms.
Bladder dysfunction affects approximately 75% of people with multiple sclerosis (MS)1 and is one of the most debilitating aspects of MS, affecting daily activities such as work, travel, sexual functioning, and social and leisure activities.2 Bladder symptoms that interfere with daily living activities are associated with an increased risk of falling in people with MS.3 Thus, when safety is of utmost concern for all, bladder dysfunction falls under the scope of practice of all health-care professionals.
Despite the high prevalence of bladder dysfunction in this population, many people avoid discussing their symptoms with health-care professionals.4 This reluctance to discuss bladder symptoms is a substantial barrier to management.5 It is common for people to develop strategies to self-manage their bladder symptoms instead of seeking care owing to the sensitive nature of the problem.6 The lack of professional guidance results in a trial and error approach.
There is a lack of awareness of bladder dysfunction among health-care professionals and care providers.7 Family physicians in Canada consider urinary incontinence a difficult problem to address and feel ill-prepared to manage it in older populations.8 Lack of confidence regarding management was reported due to concerns about the level of training and general embarrassment regarding urinary incontinence.8 Therefore, an in-depth exploration of the perceptions of health-care professionals is necessary to understand how bladder dysfunction is addressed in clinical practice.
Despite a lack of awareness of bladder dysfunction among health-care professionals, guidelines exist for the management of bladder dysfunction in MS.9,10 Asking about bladder dysfunction has become systematic in some MS clinics. However, it is not known to what extent current practice reflects the recommended guidelines. Findings from an Irish review of services for people with MS reported a lack of neurologists and MS nurses and limited access to both specialist and generalist neurorehabilitation services in the community.11Therefore, the aims of this study were to understand the perceptions of health-care professionals regarding bladder dysfunction and to explore current service provision for people with MS in the Republic of Ireland.
Methods
This qualitative study involved a combination of focus groups12 and dyadic13 and telephone interviews. Focus groups were deemed most appropriate; however, this was not possible due to a low response rate and a nationwide dispersal of participants. A variety of interview methods were used for logistical purposes and to accommodate health-care professionals given their work schedules.
Participants
A snowballing technique was used to recruit a purposive sample of Irish health-care professionals. A recruitment e-mail and an information letter were sent to the Multiple Sclerosis Society of Ireland, the Irish Society of Chartered Physiotherapists, Physiotherapists in Multiple Sclerosis, the Association of Occupational Therapists of Ireland, and the Irish Practice Nurses Association. Representatives acted as gatekeepers for participant recruitment, forwarding the recruitment e-mail and information letter to health-care professionals working with people with MS. Health-care professionals can elect to be on the e-mail list of the Multiple Sclerosis Society of Ireland. This allows regular two-way communication and updates on the role and work of the Multiple Sclerosis Society of Ireland to health-care professionals and people with MS nationally. Potential participants were invited to forward the recruitment e-mail and information letter to other health-care professionals in their network working with people with MS. The study inclusion criteria were as follows: older than 18 years, communicates effectively in English, encounters people with MS during clinical practice in any setting, and includes assessment of bladder dysfunction in their scope of practice. Because all levels of experience in the assessment and management of bladder dysfunction were sought, no participants were excluded based on expertise in bladder dysfunction.
Ethical approval was obtained from the University of Limerick Faculty of Education and Health Sciences Research Ethics Committee (Limerick, Ireland).
Data Collection
The interview guide was informed by a previous study exploring how bladder dysfunction interfered with quality of life for people with MS2 and by other service provision questionnaires.8,14,15 Open-ended questions that focused on participants' understanding of bladder dysfunction covered the topics of awareness, effect of symptoms on quality of life, symptom self-management, and current service provision.
All the interviews were audio-recorded and were moderated by the first author (CB); a notetaker recorded the main points and documented group dynamics and body language. Each interview concluded with a summary of the key points, and participants were able to make additional comments. Debriefing sessions between authors followed each data collection session. Key topics arising in early interviews were discussed in subsequent groups to allow for refinement of ongoing thematic analysis.
Data Analysis
Thematic analysis16 guided the analytic process. Reflexivity enhanced the transparency, accountability, and general trustworthiness of the study.17 This reflexive process involved detailed discussions among all the authors. These regular discussions disrupted preconceptions, thus enabling critical reflection. Field notes were used to document initial impressions during data collection and throughout the analytic process. Analytic memos were kept to achieve trustworthiness by clearly documenting the key decisions.
Thematic analysis involved an iterative process of engaging with the data.16 This process began with verbatim transcription of interviews, followed by close reading after documents were imported into NVivo10 (QSR International Inc, Burlington, MA). This qualitative data analysis software package aids the researcher in providing a transparent picture of the data while also providing an audit of the data analysis process as a whole.18 Initial codes were generated by drawing from key words and phrases in transcripts and field notes. Codes were gradually moved into clusters. Potential themes were checked across the coded extracts, and an initial diagram of the analysis was created. Tentative themes were examined to ensure that they described a coherent pattern. Clear definitions were then developed for each theme. The diagram (Figure 1) was adjusted to reflect these changes. Final definitions were developed for each category and theme.
Figure 1.
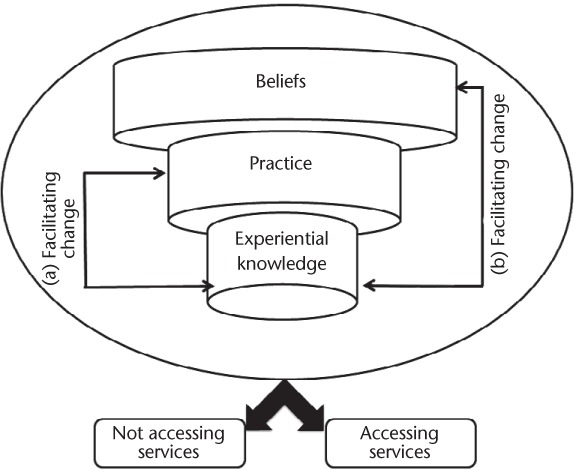
Model of clinical practice development in relation to bladder management
Results
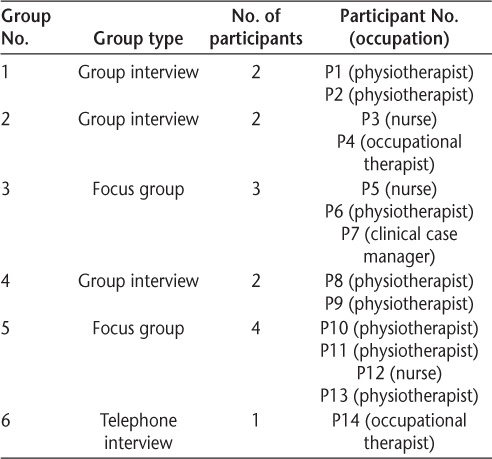
This study involved 14 health-care professionals, including physiotherapists (n = 8), occupational therapists (n = 2), nurses (n = 3), and clinical case managers (n = 1) from acute and community settings. All the participants were aged 25 to 65 years; 13 were women. Number of years qualified ranged from 5 to 32 years. Time working with people with MS ranged from 1 to 20 years (Table 1). There was a range of 5% to 100% of people with MS occupying participants' caseloads, with an average of 62%. Participants were asked before each interview to summarize their level of experience in bladder management. All three nurses had several years' experience in the management of bladder dysfunction in people with MS. One physiotherapist was a specialist in pelvic floor dysfunction for more than 20 years. The clinical case manager, two physiotherapists, and one occupational therapist were experienced in MS care and felt that they were clear about their role in bladder management. The remaining six participants were not confident with their approach to the management of this symptom. Two focus groups (n = 7), three dyadic interviews (n = 6), and one individual telephone interview were conducted (Table 2). The focus groups consisted of either 3 or 4 participants and lasted 95 and 75 minutes, respectively. The mean interview time of dyadic interviews was 70 minutes (range, 61–75 minutes), and the telephone interview lasted 54 minutes.
Table 1.
Participant demographic characteristics (N = 14)
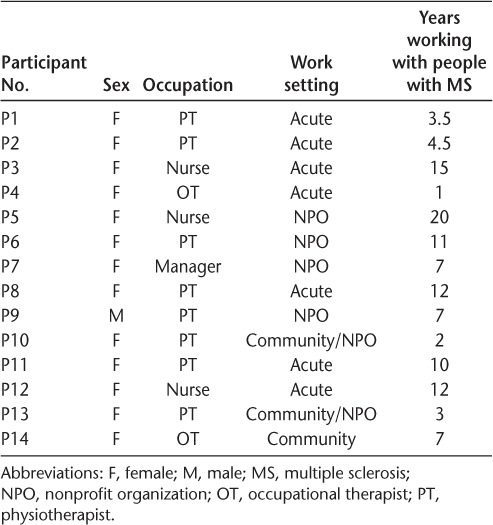
Table 2.
Group details
Analysis yielded two key themes: 1) a model of clinical practice development in relation to bladder management and 2) facilitating change to optimize access to services for people with MS. Figure 1 represents the interaction between these themes. Theme 1 is represented by the three cylinders labeled beliefs, practice, and experiential knowledge. The second theme is symbolized by the brackets named facilitating change on both sides of the model. Bracket “a” encompasses the interaction between clinical practice and experiential knowledge of health-care professionals. Bracket “b” incorporates how acknowledgment of individual beliefs can inform clinical practice and experiential knowledge. The arrows stemming from beneath the model indicate that implementing change within the model may influence whether people with MS access services.
Theme 1: Model of Clinical Practice Development in Relation to Bladder Management
Participants spoke about how their underlying beliefs regarding bladder dysfunction informed clinical practice, which in turn influenced their experiential knowledge. Participants discussed beliefs about time, priorities, responsibility, the privacy associated with the topic, and professional competence in relation to bladder management. Participants frequently reflected on the time demands associated with asking people with MS about bladder dysfunction: “If you ask that question [about bladder dysfunction] you need to give people time. Every question you ask is time related and people [health-care professionals] don't have time so they avoid the questions. But in the long term that's not effective” (nurse P5). This statement demonstrates the intense time demands that may result in some health-care professionals sidestepping issues related to incontinence. Beliefs about responsibility were also discussed: “Everyone tends to focus in on what they know, on what they are familiar with, on what they are good at. Maybe we are not really looking at the whole bigger picture. I suppose the doctors in clinic are probably the same. They zone in on really what they think they can work on and improve” (physiotherapist P1). The issue of responsibility among health-care professionals is centralized in this statement, with the participant mapping out her typical focus as a physiotherapist. If one does not recognize professional responsibility in bladder management, then it is unlikely to translate to practice. This focus not only potentially affects people with MS with bladder dysfunction and their quality of life but also limits opportunities for learning among health-care professionals. Physiotherapist P1 acknowledged that this narrow, discipline-specific focus may be problematic. Although in theory the person with MS is central to management, this is not evident in participants' perspectives about current service provision. Another physiotherapist identified how she came to realize her possible role in bladder management: “I would have always kind of thought it [incontinence] was a nurse thing that needs to be done. It was only when they [people with MS] started opening up a bit more that I kind of thought that maybe we could have more of a role in it” (physiotherapist P2). This statement captured a shift in thinking for this physiotherapist. People with MS disclosed their bladder symptoms, thus expanding her experiential knowledge and influencing her underlying beliefs about her responsibility as a health-care professional.
Beliefs held by participants regarding the sensitive nature of bladder dysfunction reinforced the reluctance to discuss the topic. For example, physiotherapist P10 found it difficult to ascertain whether the person might want to talk about bladder dysfunction: “Sometimes I do feel a little bit uncomfortable because a lot of these clients I would see every week and we would see for mobility problems. We would talk about a lot of things and then sometimes I'm like do they want to talk about this with me because they are going to continue seeing me afterwards and would they prefer if I didn't know this information” (physiotherapist P10).
This uncertainty contributed to inconsistency in practice. Onward referral seems to be reliant on how comfortable the person with MS is bringing up the issue of bladder dysfunction. This underlying belief of sensitivity informed how participants discussed bladder dysfunction and their choice of language. Physiotherapist P1 described how she asks about bladder dysfunction differently than about other symptoms. She said she asks directly “How is walking going now?” or “How are you getting on?” but would never ask “How's the bladder?” She suggested that one could not ask about bladder symptoms in the same way as other symptoms, which emphasized the influence of this belief on her clinical practice.
The final belief discussed by participants was connected to professional competence. One participant argued that health-care professionals had the necessary skills to discuss bladder dysfunction, including being open, active listening, problem solving, and using a person-centered approach to management: “I think as occupational therapists and as health-care professionals it is something we are very good at, we are active listeners, and we are problem solvers as well; we can look at things, you know, and we are very open about things” (occupational therapist P14). This participant claimed that health professional training includes all the elements needed to effectively address issues related to bladder dysfunction. However, she was concerned about health-care professionals who were unable to talk about bladder dysfunction: “If you're not able to do that then there is something wrong. If you feel that you haven't got the confidence to say ‘look I need help here’ you have to be able to go back and say, ‘Well why can't I ask? What is it? Why am I embarrassed? Why am I ashamed?’” (occupational therapist P14). This participant conveyed the importance of personal reflection in practice and being able to seek guidance when needed. Lack of expertise on the topic can reduce self-confidence. Bladder dysfunction is considered outside the scope of practice for many participants. They felt unable to offer any help for clients with bladder symptoms: “I would feel quite limited myself. I'm not trained in women's health or continence. I would feel that that would be a bit of a gap and we don't really have a very large women's health service here so there isn't really anybody directly I can really refer them to” (physiotherapist P2). This belief regarding individual ability in bladder management resulted in physiotherapist P2 avoiding this topic with patients.
This model of clinical practice development portrays the influence of the underlying beliefs of health-care professionals on clinical practice and their knowledge on bladder dysfunction. The model can have consequences for people with MS in terms of accessing services. The interaction among the elements of underlying beliefs, clinical practice, and experiential knowledge of health-care professionals can steer people with MS toward successful management of symptoms but may also inadvertently divert them from services altogether.
Theme 2: Facilitating Change to Optimize Access to Services for People with MS
This theme focuses on how change may be implemented within the model of clinical practice development to optimize bladder management. The first element of change (a) involves reflecting on clinical practice and experiential knowledge. This provided participants with new insights in terms of collecting a detailed history, asking about bladder dysfunction, methods of probing for more information, and providing a suitable physical environment for disclosure. The second element of change (b) relates back to the individual beliefs of participants in relation to bladder dysfunction and how this changed practice. In addition to the potential influence of these changes for people with MS accessing services, participants discussed their development as health-care professionals.
Many participants reflected on their clinical practice and offered examples of new knowledge gained through this process. Several participants suggested the need for a detailed history during subjective assessment: “It's getting the collateral [information] from the patient. I think that is crucial and getting that history and asking the question ‘have you this problem and that?’ Then it is amazing what comes out then” (nurse P12). Looking back, nurse P12 learned from clinical practice that a detailed history is imperative. Methods of asking about bladder dysfunction were also regarded as important among participants. Occupational therapist P14 recognized changes in daily routines as indications of bladder symptoms. She stressed that assessment is more than just asking questions and that it is also necessary to observe changes in daily functions and habits. Other participants also investigated changes in socializing activities. For example, physiotherapist P6 asked people “Are you going out on the bus trip today?” to see whether bladder dysfunction was limiting participation. This question emphasized the need to explore daily activities when assessing bladder dysfunction. Occupational therapist P14 also highlighted the importance of explaining why bladder dysfunction is relevant to the assessment and offering reassurance: “You say ‘right, ok you are not alone. You're not the first person this has happened to. You're not going to be the last person this happens to.’ Then once they are able to off-load, you can see there is a big change in the person. They kind of go ‘oh my God that's grand, that's OK’” (occupational therapist P14).
In-depth questioning and justification of why one is asking about these symptoms was suggested. Implementing these strategies contributes to experiential learning. Knowing when to probe for more information is an important skill for health-care professionals. Many participants emphasized the importance of probing: “I guess that's [probing] one way of making them aware—just asking them when assessing. So they are like ‘oh no problem with that’ then maybe when you keep asking . . . so it depends on the way you ask” (physiotherapist P10). This demonstrated how this participant used experiential knowledge, recognizing that probes are often needed when patients dismiss bladder symptoms after just one question. This captured her learning from clinical practice about the methods of asking about bladder dysfunction, which in turn influences the response of the person.
In addition to methods of questioning, the importance of creating a comfortable environment was discussed among participants. Physiotherapist P2 described how a crowded clinical environment can result in people withholding information: “I find that they are seen in clinic by the team and they could have four or five doctors in the room between medical students or registrars. Then you get a referral for them to be seen by physiotherapy and you bring them into a quiet gym and you see them one-on-one and they would tell you a lot of stuff then that they wouldn't have told the doctor. I might go back to the doctor and say ‘oh she's having a lot of sexual problems or she's having a lot of urinary problems’ and they wouldn't have heard of it” (physiotherapist P2). This participant raises the importance of the environment and how it can affect people disclosing their symptoms by comparing a one-to-one private session with a room full of health-care professionals.
Some participants took into account their personal beliefs and how this influenced their practice. Physiotherapist P13 reported that many of the people with MS she interacted with did not have bladder problems. Looking back, she suggested that this low prevalence may relate to her not asking enough questions on this topic: “That's why I feel with some patients they initially come in and do the assessment and they don't have any problems. I think it was partially as well my fault because I probably didn't ask them enough, most of my assessment is really physical . . . so maybe I did not give enough time to ask about the bladder so maybe it's them not wanting to disclose or me” (physiotherapist P13). This critical reflection, prompted by new ideas about bladder dysfunction, disrupted this participant's typical approach, creating a new perspective regarding initial assessment.
The first point of contact for care for the person with MS is the health-care professional. Each health-care professional has a specific set of beliefs about themselves and their profession. Findings from this study demonstrate the influence of underlying beliefs on clinical practice and the experiential knowledge of the health-care professional. These findings also display that these beliefs determine the pathway of the person seeking help. Thus, the importance of underlying beliefs of health-care professionals should not be underestimated in relation to bladder management.
Discussion
This is the first study attempting to understand the perceptions of health-care professionals concerning bladder dysfunction and to explore current service provision for people with MS in Ireland. The model of clinical practice development presented the interactions among underlying beliefs, practice, and experiential knowledge of health-care professionals. Findings suggest that implementing change within this model may optimize access to services for people with MS. The first element of change connects practice and experiential knowledge. This is an example of reflective practice.19 The second element of change focuses on understanding one's underlying beliefs and the influence of these beliefs on clinical practice and experiential knowledge. This is an example of reflexive practice.20 The terms reflective and reflexive practice are often used interchangeably in the literature21; however, this study offers a mechanism to explore the difference between them. Reflexive practice is central to research methods,22 but its value is not yet fully appreciated in the clinical setting. As health-care professionals, we need to consider the value of reflective and reflexive practice in optimizing service provision for people with MS with bladder dysfunction. The degree of experience in assessing and managing MS-related bladder dysfunction would influence the themes identified during the study and, therefore, the final conclusions. However, the nature of focus groups and dyadic interviews allowed the teasing out of ideas across participants of different disciplines with varying expertise, which reflects the clinical setting in which people with MS are seen.
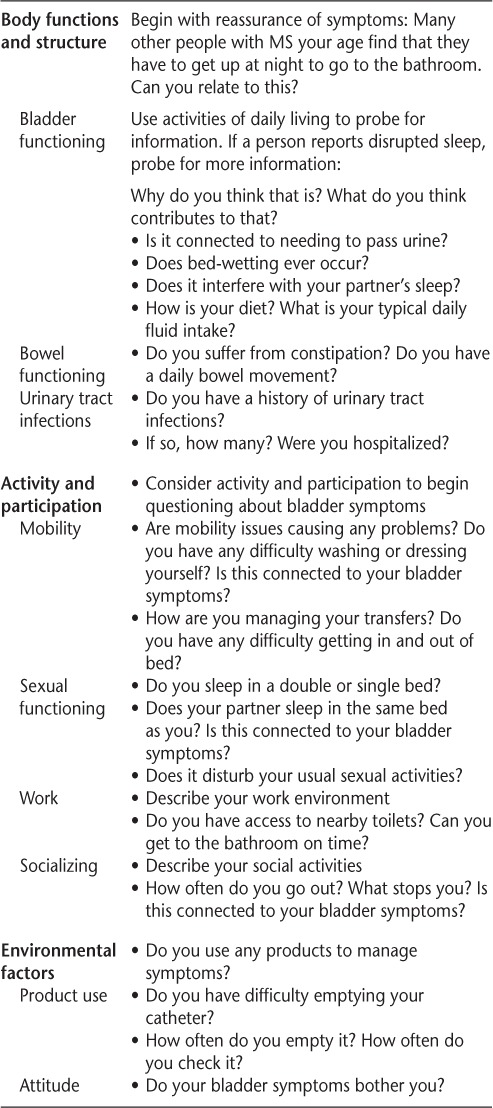
Reflective capacity is an essential characteristic of professional competence and is often prompted by complex clinical problems, which enables learning from experience.23 Participants in this study reflected on their practice, which allowed them to develop strategies to improve service provision for people with MS. They suggested ways in which to optimize discussion of bladder dysfunction during assessment. This involved collecting a detailed history, methods of asking, linking bladder questions to daily activities, probing for more information, and providing a suitable physical environment. Based on the reflections of participants, a set of practical recommendations is offered to address the difficulties clinicians face when subjectively assessing bladder dysfunction (Table 3). These recommendations aim to guide initial assessment and increase communication about bladder dysfunction. To centralize the person with MS, these recommendations are structured according to the International Classification of Functioning, Disability, and Health.24
Table 3.
Suggestions to guide subjective assessment
Reflexive practice involves finding strategies to question our own attitudes, thought processes, values, assumptions, prejudices, and habitual actions to strive to understand our complex roles in relation to others.20 Reflexivity demands more complex critical engagement than reflective practice in that the potential for understanding the countless ways in which one's own presence and perspective influence the knowledge and actions that are created is potentially more problematic than the simple searching for implicit theory.25 The core of the model of clinical practice development involves the underlying beliefs of health-care professionals. Addressing these beliefs creates an opportunity for health-care professionals to question their assumptions in relation to bladder management. It is necessary to engage in this type of reflexive practice in the clinical setting if attitudes toward bladder dysfunction are to be challenged.
Challenging beliefs is vital in a perceived silent condition such as bladder dysfunction. In this study, participants discussed their hesitancy in approaching the topic. This hesitancy is similar to that in other studies where health-care professionals are reluctant to discuss urinary conditions. Lack of training, lack of competency, lack of knowledge, and lack of time have been reported as barriers to successful management of bladder dysfunction across a range of health-care professionals.7,26 This study added that lack of privacy and uncertainty in relation to professional responsibility were barriers to the management of bladder dysfunction in an Irish context. No study to date has explored beliefs regarding the reluctance to discuss bladder dysfunction and whether this contributes to reduced discussion in clinical practice.
There were some limitations to this study. It is acknowledged that the sample size could be identified as a limitation. Multiple methods of recruitment were used over 6 months. The 14 participants represent diverse backgrounds in terms of clinical setting, discipline, and number of years of clinical experience and working with people with MS. Therefore, these 14 participants were a representative sample. There was a predominance of physiotherapists in the cohort and only three nurses. This may reflect the reduced number of nurses working with people with MS in Ireland. Although all health-care professionals were recruited similarly, the leading author is a physiotherapist and a member of the special interest group PIMS: Physiotherapists in Multiple Sclerosis. Members of this group are familiar with a strong research ethos from the MS research team in Ireland and, therefore, may have been more inclined to participate by knowing members of this research team and being familiar with how the data are used to influence policy and practice. Findings from a previous study exploring bladder dysfunction in people with MS2 were used to inform the interview schedule. This may potentially result in confirmation bias. However, the interview schedule offered a springboard for discussion among participants to initiate conversation on the topic and, therefore, did not influence the findings of this study.
This is the first in-depth exploration of the perceptions of health-care professionals concerning bladder dysfunction and service provision for people with MS in Ireland. The findings from this study suggest that health-care professionals may need to first consider their own underlying beliefs in relation to bladder dysfunction. Clinical reflection and reflexive practice are both vital for the development of services and may influence how people with MS access health service provision for this disabling symptom.
PracticePoints
Examining beliefs about bladder dysfunction is necessary to challenge existing perceptions and to address the reluctance to discuss bladder symptoms among health-care professionals.
Health-care professionals need to consider the value of reflective and reflexive practice in optimizing service provision for people with MS with bladder dysfunction.
Whereas clinical reflection can essentially disrupt clinical practice and create the possibility for change, reflexive practice may offer greater scope for change.
Acknowledgments
We thank all the study participants for sharing their time and knowledge with us; the Irish Society of Chartered Physiotherapists and the Association of Occupational Therapists of Ireland for recruitment support; and Blathin Casey for her assistance in notetaking during the focus group stage of data collection.
Financial Disclosures
The authors have no conflicts of interest to disclose.
Funding/Support
Ms. Browne is funded by the Irish Research Council (Government of Ireland Postgraduate Scholarship).
References
- 1. Nortvedt MW, Riise T, Frugaård J, . et al. Prevalence of bladder, bowel and sexual problems among multiple sclerosis patients two to five years after diagnosis. Mult Scler. 2007; 13: 106– 112. [DOI] [PubMed] [Google Scholar]
- 2. Browne C, Salmon N, Kehoe M.. Bladder dysfunction and quality of life for people with multiple sclerosis. Disabil Rehabil. 2015; 37: 2350– 2358. [DOI] [PubMed] [Google Scholar]
- 3. Finlayson M, Peterson EW, Cho CC.. Risk factors for falling among people aged 45 to 90 years with multiple sclerosis. Arch Phys Med Rehabil. 2006; 87: 1274– 1279. [DOI] [PubMed] [Google Scholar]
- 4. Koch T, Kralik D, Kelly S.. We just don't talk about it: men living with urinary incontinence and multiple sclerosis. Int J Nurs Pract. 2000; 6: 253– 260. [Google Scholar]
- 5. Wang C, Li J, Wan X, Wang X, Kane RL, Wang K.. Effects of stigma on Chinese women's attitudes towards seeking treatment for urinary incontinence. J Clin Nurs. 2015; 24: 1112– 1121. [DOI] [PubMed] [Google Scholar]
- 6. St John W, Wallis M, Griffiths S, McKenzie S.. Daily-living management of urinary incontinence: a synthesis of the literature. J Wound Ostomy Continence Nurs. 2010; 37: 80– 90. [DOI] [PubMed] [Google Scholar]
- 7. Swanson JG, Skelly J, Hutchison B, Kaczorowski J.. Urinary incontinence in Canada: national survey of family physicians' knowledge, attitudes, and practices. Can Fam Physician. 2002; 48: 86– 92. [PMC free article] [PubMed] [Google Scholar]
- 8. Nguyen K, Hunter KF, Wagg A.. Knowledge and understanding of urinary incontinence: survey of family practitioners in northern Alberta. Can Fam Phys. 2013; 59: e330– e337. [PMC free article] [PubMed] [Google Scholar]
- 9. Fowler CJ, Panicker JN, Drake M, . et al. A UK consensus on the management of the bladder in multiple sclerosis. J Neurol Neurosurg Psychiatry. 2009; 80: 470– 477. [DOI] [PubMed] [Google Scholar]
- 10. Pannek J, Blok B, Castro-Diaz D, . et al. Neurogenic lower urinary tract dysfunction. : Guidelines on Neuro-urology. Arnhem, the Netherlands: European Association of Urology; 2013. [Google Scholar]
- 11. Neurological Alliance of Ireland. . Summary Findings from First National Audit of Neurology Services in Ireland: Report on National Survey of Neurological Services. Dublin, Ireland: Neurological Alliance of Ireland; 2015. [Google Scholar]
- 12. Krueger RA, Casey MA.. Focus Groups: A Practical Guide for Applied Research. Thousand Oaks, CA: Sage Publications; 2009. [Google Scholar]
- 13. Morgan DL, Ataie J, Carder P, Hoffman K.. Introducing dyadic interviews as a method for collecting qualitative data. Qual Health Res. 2013; 23: 1276– 1284. [DOI] [PubMed] [Google Scholar]
- 14. Coote S, McKeown G, Shannon M.. A profiling study of people with multiple sclerosis who access physiotherapy services in Ireland. Int J MS Care. 2010; 12: 115– 121. [Google Scholar]
- 15. Wagg A. Treating overactive bladder in the elderly. Can Urol Assoc J. 2011; 5 suppl 2: S149– S151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Braun V, Clarke V.. Using thematic analysis in psychology. Qual Res Psychol. 2006; 3: 77– 101. [Google Scholar]
- 17. Finlay L, Gough B.. Reflexivity: A Practical Guide for Researchers in Health and Social Sciences. Hoboken, NJ: John Wiley & Sons; 2008. [Google Scholar]
- 18. Welsh E. Dealing with data: using NVivo in the qualitative data analysis process. Forum Qualitative Sozialforschung/Forum: Qualitative Social Research. 2002; 3: 26. [Google Scholar]
- 19. Finlay L. Reflecting on ‘Reflective practice.’ PBPL paper 52. http://www.sencer.net/Symposia/SSI2015/documents/Finlay-2008-Reflecting-on-reflective-practice-PBPL-paper-52.pdf. Published 2008. Accessed September 2015.
- 20. Bolton G. Reflective practice: an introduction. : Reflective Practice: Writing and Professional Development. Thousand Oaks, CA: Sage Publications; 2010. [Google Scholar]
- 21. D'Cruz H, Gillingham P, Melendez S.. Reflexivity, its meanings and relevance for social work: a critical review of the literature. Br J Soc Work. 2007; 37: 73– 90. [Google Scholar]
- 22. Alvesson M, Sköldberg K.. Reflexive Methodology: New Vistas for Qualitative Research. Thousand Oaks, CA: Sage Publications; 2009. [Google Scholar]
- 23. Mann K, Gordon J, MacLeod A.. Reflection and reflective practice in health professions education: a systematic review. Adv Health Sci Educ. 2009; 14: 595– 621. [DOI] [PubMed] [Google Scholar]
- 24. World Health Organization. . International Classification of Functioning, Disability and Health (ICF). Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 25. Fook J, White S, Gardner F.. Critical reflection: a review of contemporary literature and understandings. Crit Reflect Health Soc Care. 2006: 3– 20. [Google Scholar]
- 26. Teunissen D, van den Bosch W, van Weel C, Lagro-Janssen T.. Urinary incontinence in the elderly: attitudes and experiences of general practitioners: a focus group study. Scand J Prim Health Care. 2006; 24: 56– 61. [DOI] [PubMed] [Google Scholar]


