Abstract
Slit ventricle syndrome (SVS) is a well-known chronic complication of ventriculoperitoneal shunt (VPS) placement. In this report, we describe a unique anatomical change that we observed on the magnetic resonance (MR) images of the brain acquired from a patient with SVS. The patient was a 40-year-old woman who had undergone VPS placement at 3 months of age. A computed tomography scan of her brain revealed a slit-like ventricle. In addition, an MR image of her brain revealed upward ballooning of the third ventricle floor, which returned to normal after a lumbar puncture. This anatomical change resulted from the pressure gradient between the intra- and extraventricular spaces. We believe our findings will further our understanding of the pathogenesis of SVS. Moreover, we hope our findings will help clinicians to select endoscopic third ventriculostomy as the primary surgical approach in patients with this particular SVS pathogenesis in order to avoid complications.
Keywords: Slit ventricle syndrome, magnetic resonance imaging, endoscopic third ventriculostomy
Introduction
Slit ventricle syndrome (SVS) is a chronic complication of ventriculoperitoneal shunt (VPS) placement that occurs years (mean 6.5 years) after the initial shunt operation, which is usually performed during childhood.1 SVS is characterized by a small slit-like ventricle, slow refilling of the shunt reservoir, and the presence of chronic, intermittent headaches.2 Various pathogeneses, subclassifications, and treatment strategies for SVS have been reported, but a consensus among clinicians remains elusive.2–7 Likewise, several surgical procedures for treating SVS have been described, but no versatile and standard procedure currently exists, hence the process of selecting the appropriate procedure can be daunting.5,6,8–11 In order for clinicians to select the appropriate surgery, more information about the brain anatomy in patients with SVS is needed; however, few reports have described the magnetic resonance (MR) imaging findings of these patients. Therefore, here we report on a patient with SVS whose MR image revealed unique upward ballooning of the third ventricle floor (TVF).
Case report
The patient was a 40-year-old woman who had undergone VPS placement at 3 months of age. However, the details of her medical history at that time, including the cause of her hydrocephalus, were unclear. She presented with intermittent headaches, nausea, and muscae volitantes, and thus visited our department. On the day of her first visit, a computed tomography (CT) scan of her brain revealed a slit-like ventricle (Figure 1(a)). Bilateral papilledema was observed during the fundus examination and the opening pressure of the lumbar puncture (LP) was 32 mmH2O. Based on these findings, we diagnosed her with SVS; then, one month after the appearance of her initial symptoms, revision of the peritoneal tube was performed to confirm the patency of the shunt system and to insert a programmable valve with an anti-siphon system.
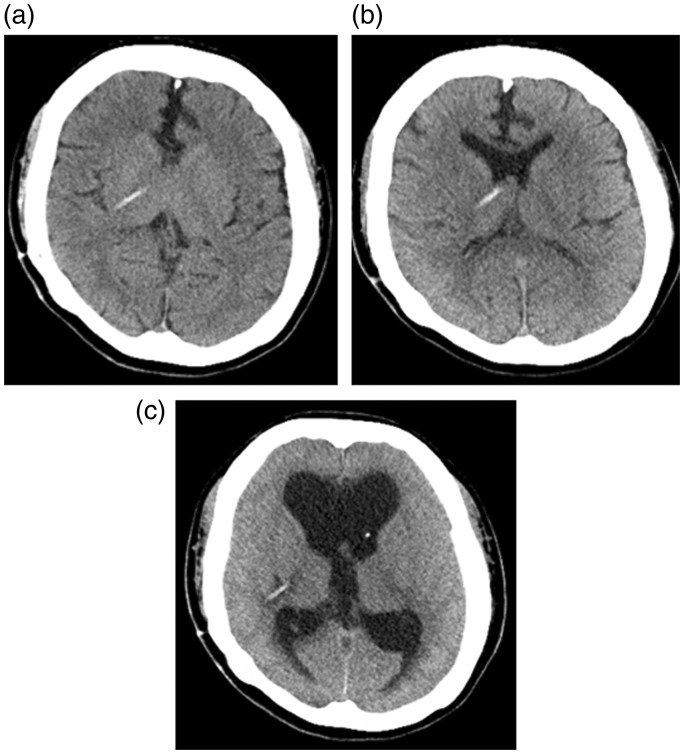
Figure 1.
Computed tomography images of the patient’s brain. (a) Image acquired when the patient was symptomatic revealed a slit-like ventricle. (b) During continuous lumbar drainage, the ventricle was dilated, and the patient’s symptoms improved. (c) After lumboperitoneal shunt placement, her level of consciousness deteriorated. The computed tomography scan revealed over-dilation of the ventricular system and disappearance of the subarachnoid space.
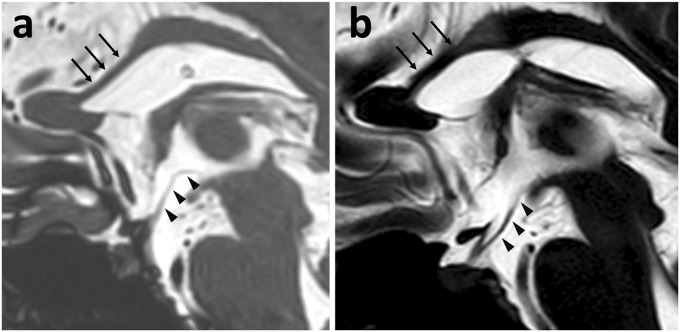
Although her symptoms disappeared postoperatively, the same symptoms recurred three months after the operation. An MR image of the brain revealed a slit-like ventricle, upward ballooning of the TVF, and downward displacement of the body of the corpus callosum (Figure 2(a)). The opening pressure of the LP was >35 mmH2O, and her symptoms improved after the LP. MR imaging of the brain that was performed immediately after the LP revealed a normal TVF and corpus callosum (Figure 2(b)). Unfortunately, her symptoms returned by the next day. Continuous lumbar drainage progressively improved her symptoms, and a CT scan of her brain revealed a dilated ventricle rather than a slit-like ventricle (Figure 1(b)).
Figure 2.
Magnetic resonance cisternography images of the patient’s brain. (a) A sagittal magnetic resonance cisternography image, which was acquired when the patient was symptomatic, revealed upward ballooning of the third ventricle floor (TVF) (arrow heads) and downward displacement of the corpus callosum (arrows). (b) After performing a lumbar puncture, the TVF and corpus callosum returned to normal.
Four months after the shunt revision, we inserted a lumboperitoneal shunt (LPS) with a programmable valve into the patient and adjusted it to the lowest level. Her symptoms improved postoperatively; however, her level of consciousness deteriorated two days after the operation. Another CT scan of her brain revealed dilation of the ventricular system and disappearance of the subarachnoid space. This finding indicated overdrainage of the cerebrospinal fluid in the extraventricular space (Figure 1(c)). Thus, we immediately adjusted the programmable valve of the LPS to the highest level and performed endoscopic third ventriculostomy (ETV) from the right anterior horn. The opening pressure of the first puncture was ∼15 mmH2O. During the operation, we found that the aqueduct was obstructed with a membranous structure and that the old ventricular tube was partially obstructed. A stoma was created using an expander balloon (Phycon, Fuji Systems Corporation, Tokyo, Japan) under a flexible video-scope guide, and the prepontine cistern was confirmed through the stoma. As the TVF was loose and fluctuated unstably, we placed the ventricle tube of the Ommaya reservoir, which contained additional side holes, in the stoma as a stent to maintain permanent patency.
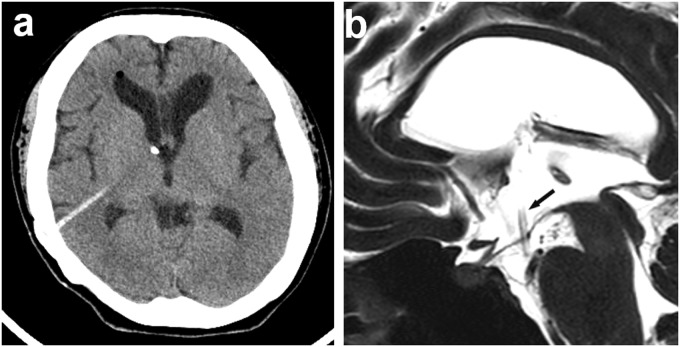
Postoperative CT and MR images of the patient’s brain revealed that the size of the ventricle had returned to normal; the TVF and corpus callosum had also returned to normal (Figure 3(a) and (b)). Importantly, the patient’s level of consciousness improved and her symptoms disappeared. Finally, she was discharged with no new neurological deficits. Informed consent for the details of her case to be reported was obtained from the patient.
Figure 3.
Images acquired from the patient after endoscopic third ventriculostomy (ETV). (a) Computed tomography image showing that the dilated ventricular system returned to normal after ETV; moreover, her consciousness level improved. (b) Sagittal magnetic resonance cisternography image acquired after ETV reveals the ventricular tube of the Ommaya reservoir, which was placed at the prepontine cistern through a stoma (arrow), and shows that the TVF and corpus callosum had returned to normal.
Discussion
A variety of surgical procedures for treating SVS (e.g. shunt revision, cranial expansion, LPS and ETV) have been reported.5,6,8–11 However, there is no standard procedure, and clinicians should select the type of surgery based on the pathogenesis of the SVS in each patient in order to ensure complete recovery.
Here, we hypothesized that the pathogenesis of the SVS in our patient was related to secondary obstruction of the aqueduct and increased pressure in the extraventricular space, which promoted the discharge of cerebrospinal fluid from the intraventricular space through the VPS, resulting in a slit-like ventricle and intermittent obstruction of the ventricular tube. In this situation, the pressure in the extraventricular space was higher than that in the intraventricular space, that is, a pressure gradient among the intra- and extraventricular spaces developed, which produced upward ballooning of the TVF. When aqueductal stenosis or obstruction without dilation of the ventricular system occurs, as was the case in our patient with SVS, it can be difficult to prove whether patency of the aqueduct is being maintained based on MR imaging findings unless the obstruction can be directly visualized on the images. Additionally, since the initial shunt operation is often performed years before the occurrence of SVS, the cause of the original hydrocephalus that required the shunt operation may be unknown. Therefore, identifying upward ballooning of the TVF on MR images is clinically important as an indirect indicator of aqueductal stenosis or obstruction.
Upward ballooning of the TVF was clearly visible on sagittal and coronal MR cisternography images. In addition to upward ballooning of the TVF, MR imaging of the brain revealed downward displacement of the body of the corpus callosum. After treatment, however, the corpus callosum returned to normal. Although the callosal displacement might have been the result of existing partial thinning of the patient’s corpus callosum, and thus may not have occurred in a patient with a normal corpus callosum, this finding, like the upward ballooning of the TVF, also indicated the presence of a pressure gradient.
In our case, we opted to perform LPS placement because the patient’s symptoms improved during continuous lumbar drainage. However, a complication occurred owing to a pressure adjustment error of the programmable valves. Le et al.10 reported that LPS placement is an effective treatment option in a certain subset of patients with SVS, namely those with symptoms arising from increased intracerebral pressure and high opening pressure in combination with significant symptom improvement or resolution after LP. Indeed, LPS placement is an efficacious treatment for SVS, but management of the double-programmable valves in the intra- and extraventricular spaces is troublesome and associated with the potential risk of tonsillar herniation, especially in non-communicating hydrocephalus.10,12 Retrospectively, if we had performed ETV and stent placement as the initial surgical treatment based on the upward ballooning of the TVF and its recovery after LP, this complication could have been prevented.
In summary, our case demonstrated a rare pathogenesis of SVS wherein the intracranial pressure in the extraventricular space was higher than that in the intraventricular space. In patients with this condition, upward ballooning of the TVF and its recovery after LP on MR images are important radiological findings for determining the appropriate surgical treatment. We believe our findings will help clinicians to better understand the pathogenesis of SVS, which will allow them to select the appropriate surgical treatment strategy for patients with this syndrome.
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Khorasani L, Sikorski CW, Frim DM. Lumbar CSF shunting preferentially drains the cerebral subarachnoid over the ventricular spaces: Implications for the treatment of slit ventricle syndrome. Pediatr Neurosurg 2004; 40: 270–276. [DOI] [PubMed] [Google Scholar]
- 2.Rekate HL. Classification of slit-ventricle syndromes using intracranial pressure monitoring. Pediatr Neurosurg 1993; 19: 15–20. [DOI] [PubMed] [Google Scholar]
- 3.Serlo W, Heikkinen E, Saukkonen AL, et al. Classification and management of the slit ventricle syndrome. Childs Nerv Syst 1985; 1: 194–199. [DOI] [PubMed] [Google Scholar]
- 4.Rekate HL. The slit ventricle syndrome: Advances based on technology and understanding. Pediatr Neurosurg 2004; 40: 259–263. [DOI] [PubMed] [Google Scholar]
- 5.Sood S, Barrett RJ, Powell T, et al. The role of lumbar shunts in the management of slit ventricles: Does the slit-ventricle syndrome exist? J Neurosurg 2005; 103: 119–123. [DOI] [PubMed] [Google Scholar]
- 6.Bateman GA. Hypertensive slit ventricle syndrome: Pseudotumor cerebri with a malfunctioning shunt? J Neurosurg 2013; 119: 1503–1510. [DOI] [PubMed] [Google Scholar]
- 7.Jang M, Yoon SH. Hypothesis for intracranial hypertension in slit ventricle syndrome: New concept of capillary absorption laziness in the hydrocephalic patients with long-term shunts. Med Hypotheses 2013; 81: 199–201. [DOI] [PubMed] [Google Scholar]
- 8.Baskin JJ, Manwaring KH, Rekate HL. Ventricular shunt removal: The ultimate treatment of the slit ventricle syndrome. J Neurosurg 1998; 88: 478–484. [DOI] [PubMed] [Google Scholar]
- 9.Eide PK, Helseth E, Due-Tønnessen B, et al. Changes in intracranial pressure after calvarial expansion surgery in children with slit ventricle syndrome. Pediatr Neurosurg 2001; 35: 195–204. [DOI] [PubMed] [Google Scholar]
- 10.Le H, Yamini B, Frim DM. Lumboperitoneal shunting as a treatment for slit ventricle syndrome. Pediatr Neurosurg 2002; 36: 178–182. [DOI] [PubMed] [Google Scholar]
- 11.Chernov MF, Kamikawa S, Yamane F, et al. Neurofiberscope-guided management of slit-ventricle syndrome due to shunt placement. J Neurosurg 2005; 102: 260–267. [DOI] [PubMed] [Google Scholar]
- 12.Chumas PD, Kulkarni AV, Drake JM, et al. Lumboperitoneal shunting: A retrospective study in the pediatric population. Neurosurgery 1993; 32: 376–383. [DOI] [PubMed] [Google Scholar]