Abstract
Excessive consumption of over-the-counter stimulants is associated with coronary vasospasm, thrombotic complications, and sudden cardiac death. Their effects on cerebrovascular physiology are not yet described in the neurointerventional literature. Patients are increasingly exposed to high levels of these vasoactive substances in the form of caffeinated energy drinks and specialty coffees. We report a case of aneurysmal subarachnoid hemorrhage (SAH) and severe, catheter-induced vasospasm during attempted endovascular repair of a ruptured anterior communicating artery (AComA) aneurysm in the setting of excessive energy drink consumption. We review the literature and alert clinicians to this potentially serious complication.
Keywords: Caffeine, catheter-induced vasospasm, energy drink, subarachnoid hemorrhage, thrombosis
Introduction
The intentional consumption and abuse of legal, over-the-counter stimulants, such as caffeinated energy drinks, are known to have numerous effects on human physiology, including the cardiovascular and nervous systems. For example, excessive (and inappropriate) consumption of caffeinated energy drinks has been associated with coronary vasospasm, acute coronary thrombosis, sudden cardiac death, and cerebral vasospasm.1–5
Catheter-induced vasospasm is a well-recognized complication of interventional procedures.6–9 Unlike subarachnoid hemorrhage (SAH)-related vasospasm, it is caused by mechanical irritation of the endoluminal surface of a blood vessel by contact with a catheter or guidewire. This type of vasospasm is typically non-flow-limiting, self-limited, and often resolves with withdrawal of the offending catheter and passage of time. Less frequently, the administration of pharmacological vasodilators is required.10,11 Thromboembolic complications are a major concern during any neurointerventional procedure, but are particularly prevalent in the treatment of ruptured intracranial aneurysms, perhaps due to a systemic, prothrombotic state.
Herein, we report a case of aneurysmal SAH complicated by severe, catheter-induced vasospasm and symptomatic thromboembolism during attempted endovascular coiling of a ruptured anterior communicating artery (AComA) aneurysm in the setting of excessive energy drink consumption. We review the literature regarding vasospasm and thromboembolism related to the use of caffeinated energy drinks, and alert clinicians to this potentially serious complication.
Case report
History and examination
This 44-year-old woman presented with a sudden-onset, severe headache. Her past medical history was significant for habitual, excessive energy drink consumption. Indeed, over the course of that day, she had consumed five oversized cans (16 ounces/can) of Monster Energy® drink (totaling 800 mg caffeine). She was neurologically intact and reported moderate-to-severe headache, neck stiffness, and sensitivity to light (Hunt & Hess grade 2). Her admission non-contrast computed tomography (CT) of the brain demonstrated thick SAH in a classical starburst pattern (Fisher grade 3, Figure 1(a)). The accompanying CT angiogram demonstrated a wide-necked 5-mm AComA aneurysm with conspicuous daughter sac (Figure 1(b)). High-resolution vessel wall magnetic resonance imaging (MRI) demonstrated avid enhancement of the aneurysm wall consistent with the site of rupture (Figure 1(c), (d)).12,13 A decision was made to proceed with endovascular coiling using a balloon-remodeling technique as a first-line treatment option. The patient was intubated and a right-sided external ventricular drain inserted in preparation for endovascular coiling the next day.
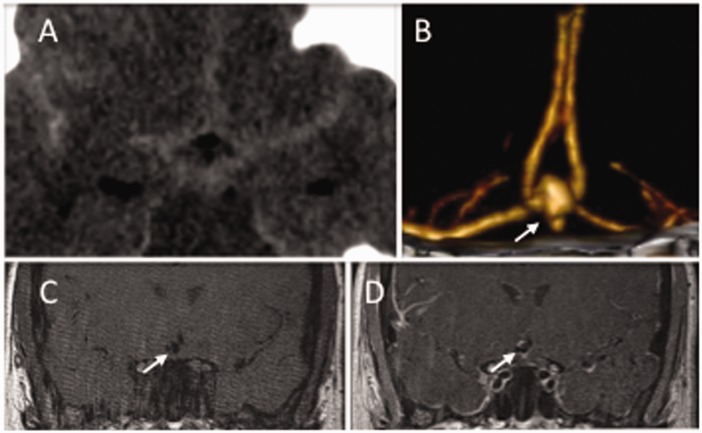
Figure 1.
(a) Axial noncontrast CT demonstrating diffuse SAH. (b) The accompanying CT angiogram demonstrates a small AComA aneurysm. T1-weighted black blood vessel wall sequences (coronal plane) before (c) and after (d) administration of gadolinium demonstrate thick contrast enhancement of the AComA aneurysm wall, consistent with its being the site of rupture. The arrow points to the AComA aneurysm. AComA: anterior communicating artery; SAH: subarachnoid hemorrhage. CT: computed tomography; SAH: subarachnoid hemorrhage; AComA: anterior communicating artery.
Neurointerventional procedure
The patient was anticoagulated with a bolus dose of intravenous (IV) heparin (100 units/kg) immediately after groin access. Additional doses of IV heparin were administered as needed (activated clotting time (ACT) maintained >250 throughout the procedure). An exchange maneuver was performed in the right external carotid artery to position a 6 F Flexor Shuttle Guiding Sheath (Cook Medical, Bloomington, IN) into the distal right common carotid artery. From this base position, a Neuron 6 F 070 Delivery Catheter (Penumbra Inc, Alameda, CA) was positioned in the petrous segment of the right internal carotid artery (ICA). A HyperForm Occlusion Balloon Catheter (4 × 7-mm, ev3 Neurovascular, Irvine, CA) was positioned in the right A1 segment in preparation for a balloon-remodeling technique. Control runs demonstrated anterograde flow with no evidence of vasospasm (Figure 2(a)). During attempts to navigate the balloon catheter across the neck of the aneurysm, back-and-forth movement of the delivery catheter was observed. Control runs demonstrated severe, flow-limiting, delivery catheter-induced vasospasm in the petrous ICA (Figure 2(b), (c)). This improved over the course of a few minutes with more proximal repositioning of the delivery catheter. Unfortunately, a new, non-flow-limiting filling defect was observed in the right supraclinoid ICA with rapid clot migration into the right M1 segment (Figure 2(d)). Soon thereafter, the M1 thrombus spontaneously migrated distally and fragmented into multiple M2/3 vessels. Revascularization of a majority of the MCA territory (Thrombolysis in Cerebral Infarction (TICI) 2b) was achieved by administration of 325 mg of aspirin via orogastric tube, infusion of 5 mg intra-arterial Abciximab (ReoPro®) via a microcatheter placed in the distal M1 segment, optimization of systemic heparinization, and multiple passes with the Solitaire™ FR Revascularization Device (4 × 20-mm, ev3 Neurovascular, Irvine, CA), (Figure 2(e)). An MRI of the brain performed immediately post-intervention demonstrated a right MCA territory stroke (Figure 2(f), (g)). The patient had a new left-sided hemiplegia. The aneurysm was successfully coiled the next day. During the second interventional procedure, ICA vasospasm was again encountered (Figure 2(h)), but successfully managed with early recognition, intra-arterial verapamil administration (10 mg), and more proximal positioning of the delivery catheter.
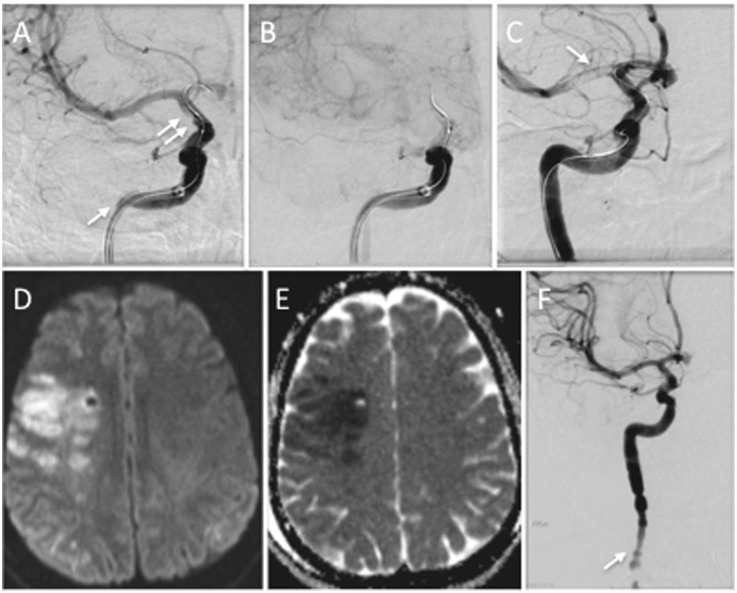
Figure 2.
(a) Digital subtraction angiogram (AP view) demonstrates catheter-induced vasospasm in the high cervical/petrous segments of the ICA (arrow) around a delivery catheter with a balloon catheter positioned in the right A1 segment over a guidewire. Note the early formation of a filling defect in the supraclinoid ICA (double arrows). (b) A later frame in the same angiographic run demonstrates the near occlusive nature of the vasospasm with significant stasis of contrast. (c) Digital subtraction angiogram (AP view) demonstrates migration of a clot from the supraclinoid ICA into the right M1 segment (arrow). (d) Axial diffusion-weighted imaging with apparent diffusion coefficient mapping (e) demonstrates a post-procedural right MCA infarct. (f) Digital subtraction angiogram (AP view) demonstrates recurrent, catheter-induced vasospasm in the cervical ICA during a second endovascular procedure (arrow). This was successfully managed with early recognition, intra-arterial verapamil administration, and repositioning of the delivery catheter. AP: anteroposterior; ICA: internal carotid artery; MCA: middle cerebral artery.
Postoperative course
The patient’s postoperative course was complicated by severe, right MCA vasospasm resulting in extension of her right MCA stroke, and a left lower extremity deep vein thrombosis on post-SAH Day 9. At her six-month follow-up, the patient was ambulating normally without the use of an assist device; she continued to have severe right arm and hand weakness that did not improve significantly over time (modified Ranking Scale (mRS) = 2). There was no evidence of aneurysm recanalization on contrast-enhanced MR angiogram (three-year follow-up).
Discussion
Energy drink beverages have become a popular form of caffeine consumption, with some brands containing the caffeine equivalent of one to three cups of coffee. For example, the Red Bull Energy Drink® has 80 mg of caffeine per can and the Monster Energy Drink® has 160 mg of caffeine per can. These drinks also have additional psychoactive substances, including glucuronolactone, L-carnitine, taurine, guarana extract (a plant extract), and ginseng extract (an herb).14 Guarana contains both theophylline and up to 40–80 mg of additional caffeine, yielding more caffeine exposure than the packaging may state.15 The adverse events ascribed to energy drink use are largely attributed to the sympathomimetic effects of high-dose caffeine.16,17 Taurine is believed to improve cardiac contractility and lower blood pressure. However, in combination with high caffeine exposure, taurine may exacerbate the sympathomimetic effects of caffeine, increasing blood pressure, contractility, and stroke volume (translating into increased work).18,19
Energy drink consumption has detrimental effects both on platelet and endothelial function (see Table 1). A single energy drink increases platelet aggregation in response to both arachidonic acid and adenosine diphosphate (ADP) in as little as 60–90 minutes in young, healthy volunteers.20,21 Notably, these are the same pathways inhibited by antiplatelet agents that are used to prevent thrombosis and resultant cardiovascular and neurovascular events. Individuals at risk of stroke and myocardial infarction (MI) may be even more at risk of adverse events in the context of energy drink consumption. In addition to inducing a pro-thrombotic state, energy drinks also alter endothelial function. A single energy drink reduces the ability of the endothelium to mediate vascular relaxation in young, healthy volunteers.21,22 In combination, the pro-thrombotic and vasospastic state induced by energy drink consumption may place individuals at risk for cardiovascular and neurovascular events. There are several reports of MI,1–3 and cerebral vasospasm and stroke,4,5 linked to energy drink “binges” often coupled with strenuous physical exercise.
Table 1.
Effects of energy drinks on cerebral and cardiac vasculature.
| Platelet dysfunction—laboratory studies | |
| Pommerening et al., 201520 | Increased platelet aggregation via arachidonic acid-induced activation one hour following energy drink consumption in young, healthy volunteers |
| Worthley et al., 201021 | Increased platelet aggregation via adenosine diphosphate (ADP)-induced activation one hour following energy drink consumption in young, healthy volunteers |
| Vascular tone—laboratory studies | |
| Worthley et al., 201021 | Significant endothelial dysfunction (decreased reactive hyperemia index) one hour following energy drink consumption in young, healthy volunteers |
| Higgins, 201322 | Significant endothelial dysfunction (decreased reactive hyperemia measured by flow mediated dilation) 90 minutes following energy drink consumption in a young, healthy volunteer |
| Cerebral vasculature—case reports | |
| Samanta et al., 20154 | Reversible cerebral vasospasm several hours after binge-consuming four energy drinks in a healthy 16-year-old |
| Worrall et al., 20055 | Cerebral vasculopathy with concurrent strokes shortly after consuming herbal “energy drink” coupled with strenuous physical activity in a 21-year-old |
| Cardiac vasculature—case reports | |
| Unal et al., 201523 | Acute myocardial infarction (AMI) with multi-vessel coronary thrombi (occlusive and near-occlusive) five to six hours after consuming five energy drinks in a healthy 32-year-old |
| Benjo et al., 20122 | AMI with large, multi-vessel coronary thrombi (near occlusive) one to two hours after consuming three vodka/energy drink mixtures in a healthy 24-year-old smoker |
| Wilson et al., 20121 | Coronary vasospasm several hours after consuming five to seven energy drinks in a healthy 17-year-old |
| Berger et al., 20093 | AMI following consumption of seven to eight energy drinks over 12 hours coupled with strenuous physical activity in a healthy 28-year-old smoker |
With the rise in popularity of heavily caffeinated energy drinks, the incidence of psychoactive-induced vasospasm and thrombotic events may rise. Although there are no prospective studies to demonstrate a direct link between caffeine intake in the form of energy drinks and vasospasm or thrombosis, the indirect evidence is mounting, especially in the cardiac literature. While it is not uncommon to see vasospasm in young healthy female patients, it is possible that the severe intracerebral vasospasm and clot formation seen in our patient was, in part, associated with a primed vasculature and coagulation system from habitual and excessive energy drink consumption.
Conclusion
As this is a single case report, it is impossible to confirm a causal link between our patient’s excessive caffeine intake and her resultant vasospasm and thromboembolic event. However, this case adds further indirect evidence that energy drinks may contribute to cardiopulmonary or neurovascular events. In physiologically predisposed individuals, a combination of excessive sympathomimetic intake in association with mechanical irritation of the cerebral vasculature may contribute to vasospasm with potentially deleterious effects. Such substances can also increase platelet aggregation and resultant thrombus formation. Given the increasing use of these substances, we recommend that clinicians ask their patients about their use as part of the standard physical history, and to be cognizant of the potential neuro- and cardiovascular effects.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Wilson RE, Kado HS, Samson R, et al. A case of caffeine-induced coronary artery vasospasm of a 17-year-old male. Cardiovasc Toxicol 2012; 12: 175–179. [DOI] [PubMed] [Google Scholar]
- 2.Benjo AM, Pineda AM, Nascimento FO, et al. Left main coronary artery acute thrombosis related to energy drink intake. Circulation 2012; 125: 1447–1448. [DOI] [PubMed] [Google Scholar]
- 3.Berger AJ, Alford K. Cardiac arrest in a young man following excess consumption of caffeinated “energy drinks”. Med J Aust 2009; 190: 41–43. [DOI] [PubMed] [Google Scholar]
- 4.Samanta D. Reversible cerebral vasoconstriction syndrome: Another health hazard of energy drinks? Clin Pediatr (Phila) 2015; 54: 186–187. [DOI] [PubMed] [Google Scholar]
- 5.Worrall BB, Phillips CD, Henderson KK. Herbal energy drinks, phenylpropanoid compounds, and cerebral vasculopathy. Neurology 2005; 65: 1137–1138. [DOI] [PubMed] [Google Scholar]
- 6.Deligonul U, Kern MJ, Caralis D. Left main and right catheter-induced coronary artery spasm in a patient with vasospastic angina. Cathet Cardiovasc Diagn 1989; 17: 39–44. [DOI] [PubMed] [Google Scholar]
- 7.Shortal BP, Mahmud E, Tsimikas S. Catheter-induced vasospasm of both the right external iliac and right coronary arteries during coronary angiography. Int J Cardiovasc Imaging 2005; 21: 481–485. [DOI] [PubMed] [Google Scholar]
- 8.Sriganesh K, Chatterjee N, Singha S. Bispectral Index monitoring facilitates early detection of catheter-induced vasospasm during neuro-endovascular procedures. Acta Anaesthesiol Scand 2009; 53: 406–407. [DOI] [PubMed] [Google Scholar]
- 9.Morris P. Practical neuroangiography. Baltimore, MD: Williams & Wilkins, 1997, p. 37.
- 10.Coon AL, Colby GP, Mack WJ, et al. Treatment of mechanically-induced vasospasm of the carotid artery in a primate using intra-arterial verapamil: A technical case report. BMC Cardiovasc Disord 2004; 4: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eckard DA, Purdy PD, Girson MS, et al. Intraarterial papaverine for relief of catheter-induced intracranial vasospasm. AJR Am J Roentgenol 1992; 158: 883–884. [DOI] [PubMed] [Google Scholar]
- 12.Matouk CC, Cord BJ, Yeung J, et al. High-resolution vessel wall magnetic resonance imaging in intracranial aneurysms and brain arteriovenous malformations. Top Magn Reson Imaging 2016; 25: 49–55. [DOI] [PubMed] [Google Scholar]
- 13.Matouk CC, Mandell DM, Gunel M, et al. Vessel wall magnetic resonance imaging identifies the site of rupture in patients with multiple intracranial aneurysms: Proof of principle. Neurosurgery 2013; 72: 492–496; discussion 496. [DOI] [PubMed] [Google Scholar]
- 14.Higgins JP, Tuttle TD, Higgins CL. Energy beverages: Content and safety. Mayo Clin Proc 2010; 85: 1033–1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sanaei-Zadeh H. With which mechanism the overuse of energy drinks may induce acute myocardial ischemia? Cardiovasc Toxicol 2012; 12: 273–274. [DOI] [PubMed] [Google Scholar]
- 16.Gunja N, Brown JA. Energy drinks: Health risks and toxicity. Med J Aust 2012; 196: 46–49. [DOI] [PubMed] [Google Scholar]
- 17.Seifert SM, Schaechter JL, Hershorin ER, et al. Health effects of energy drinks on children, adolescents, and young adults. Pediatrics 2011; 127: 511–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baum M, Weiss M. The influence of a taurine containing drink on cardiac parameters before and after exercise measured by echocardiography. Amino Acids 2001; 20: 75–82. [DOI] [PubMed] [Google Scholar]
- 19.Franks AM, Schmidt JM, McCain KR, et al. Comparison of the effects of energy drink versus caffeine supplementation on indices of 24-hour ambulatory blood pressure. Ann Pharmacother 2012; 46: 192–199. [DOI] [PubMed] [Google Scholar]
- 20.Pommerening MJ, Cardenas JC, Radwan ZA, et al. Hypercoagulability after energy drink consumption. J Surg Res 2015; 199: 635–640. [DOI] [PubMed] [Google Scholar]
- 21.Worthley MI, Prabhu A, De Sciscio P, et al. Detrimental effects of energy drink consumption on platelet and endothelial function. Am J Med 2010; 123: 184–187. [DOI] [PubMed] [Google Scholar]
- 22.Higgins JP. Endothelial function acutely worse after drinking energy beverage. Int J Cardiol 2013; 168: e47–e49. [DOI] [PubMed] [Google Scholar]
- 23.Unal S, Sensoy B, Yilmaz S, et al. Left main coronary artery thrombosis and acute anterior myocardial infarction related to energy drink. Int J Cardiol 2015; 179: 66–67. [DOI] [PubMed]