Abstract
Background
Tobacco use is often initiated during adolescence and continued into adulthood despite desires to quit. A better understanding of the neural correlates of abstinence from smoking in adolescents may inform more effective smoking cessation interventions. Neural reward systems are implicated in tobacco-use disorder, and adolescent smokers have shown reduced reward-related ventral striatal activation related to increased smoking.
Methods
The current study evaluated nondrug reward anticipation in adolescent smokers using a monetary incentive delay task in fMRI pre- and post- smoking cessation treatment (n = 14). This study tested how changes in neural responses to reward anticipation pre- to post-treatment were related to reduced smoking. An exploratory analysis in a larger sample of adolescents with only pre-treatment fMRI (n = 28) evaluated how neural responses to reward anticipation were related to behavioral inhibition and behavioral activation scales.
Results
Adolescent smokers showed pre- to post-treatment increases in reward anticipation-related activity in the bilateral nucleus accumbens and insula, and medial prefrontal cortex, and greater increases in reward anticipation-related activity were correlated with larger percent days of smoking abstinence during treatment.
Conclusions
These findings suggest that reduced smoking during smoking cessation treatment is associated with a “recovery of function” in frontostriatal responses to nondrug reward anticipation in adolescent smokers, although comparison with a developmental control group of adolescent nonsmokers is warranted.
Keywords: adolescent, smoking, cessation, reward, monetary incentive delay
1. Introduction
Tobacco use is typically initiated and established in adolescence, with nearly 90% of cigarette smokers starting by age 18, and 99% by age 26 (U.S. Department of Health and Human Services, 2012). Although few adolescent smokers imagine themselves smoking five years later, three of four will smoke into adulthood and one in three who continues smoking will die prematurely from tobacco-related illness (U.S. Department of Health and Human Services, 2012). Most adolescent smokers report wanting to quit and attempting to quit in the past year (Teplinskaya and Gerzoff, 2011), however, success is low (Stanton and Grimshaw, 2013). A better understanding of the neural correlates of smoking abstinence in adolescents may help to develop more effective smoking cessation interventions.
Drugs of addiction including nicotine alter the sensitivity of brain regions involved in motivation and reward (Robinson and Berridge, 2001). Addiction is typically associated with responsivity to drug-related cues in the mesocorticolimbic dopaminergic reward circuit including the ventral striatum and medial prefrontal cortex (Koob and Volkow, 2010). Neuroimaging studies indicate that smokers show increased drug cue-reactivity in reward-related brain regions (Chase et al., 2011; Engelmann et al., 2012), including adolescent smokers (Rubinstein et al., 2011). Addicted individuals also show blunted responses in these brain regions to nondrug (i.e., monetary) rewards (Balodis and Potenza, 2015; Hommer et al., 2011; Sweitzer et al., 2015; Sweitzer et al., 2014), a finding also reported in adolescent smokers (Peters et al., 2011). Impaired reward processing in addiction may contribute to drug-seeking behavior and interfere with treatment. Furthermore, because adolescence is a period associated with heightened sensitivity to reward (Somerville et al., 2010), impaired reward processing may be both a risk factor for addictions and a potential target for treatment.
Behavioral tendencies also relate importantly to addictive behaviors (Kotov et al., 2010) and have been linked to early substance abuse (Malmberg et al., 2012; Shedler and Block, 1990), including adolescent smoking (Harakeh et al., 2006). In particular, individual differences in sensitivity to reinforcement may be a risk factor for addictions (Franken et al., 2006; Gray, 1994). Two brain systems have been hypothesized to underlie individual reinforcement sensitivities and impact motivated behavior and affect: an appetitive or behavioral approach system (BAS) and an aversive or behavioral inhibition system (BIS) (Carver and White, 1994; Gray, 1981). High BAS sensitivity indicates a likelihood to activate goal-directed behavior in response to reward (Franken et al., 2006; Gray, 1981) such as drug-related cues (Carver and White, 1994; Franken et al., 2006). High BIS sensitivity indicates a likelihood to inhibit behavior that may lead to negative outcomes (Gray, 1981). Prior studies report that higher BAS was associated with greater likelihood of being a smoker, and (among smokers) smoking frequency, but did not find relationships between smoking and BIS (O’Connor et al., 2009; Tapper et al., 2015), and BIS/BAS has not been evaluated in adolescent smokers.
The present study aimed to evaluate reward processing, smoking behavior and reinforcement sensitivities in adolescent smokers in treatment for smoking cessation. To evaluate reward processing, we used a monetary incentive delay task (MIDT; Andrews et al., 2011; Knutson, 2001) in functional magnetic resonance imaging (fMRI). The analysis focused on reward anticipation, based on findings that adolescent smokers showed lower ventral striatal responses to reward anticipation than nonsmokers, lowest in those who smoked more frequently (Peters et al., 2011). First, we tested for changes in reward anticipation-related brain activity pre- to post-treatment and whether those changes related to changes in smoking (n=14). We hypothesized that reward anticipation-related brain activity would increase pre- to post-treatment and correlate with reduced smoking. Next, we tested whether pre-treatment reward anticipation-related brain activity was related to BIS/BAS in a larger sample with only pre-treatment fMRI (n=28). We hypothesized that adolescents with higher BAS would show greater reward responsiveness (i.e., greater reward anticipation-related brain activity), and we explored the relationship between neural reward processing and BIS.
2. Materials and Methods
All procedures were approved by the Yale Human Investigations Committee. Parental consent and adolescent assent were obtained from adolescents aged 14–17 years, and consent was obtained from youth aged 18 years or older.
2.1. Participants
Treatment-seeking adolescent smokers were recruited from Connecticut high schools to participate in smoking cessation trials (Krishnan-Sarin et al., 2013b; NCT01145001). Adolescents were included if they reported smoking ≥ 5 cigarettes per day for the past six months and had a quantitative urine cotinine level ≥ 350 ng/ml (Graham Massey Analytical Labs, Shelton, CT). The Diagnostic Predictive Scale (Lucas et al., 2001) and an evaluation by a clinical psychologist were used to exclude adolescents with current Axis-I disorders (including substance use disorders other than nicotine dependence), significant untreated medical conditions, or suicidal or homicidal risk. (Table 1). All adolescents (n=28) took part in a pretreatment fMRI and a subset of these (n=14) also took part in a post-treatment fMRI.
Table 1.
Demographics, baseline and clinical characteristics. All adolescents took part in a pre-treatment fMRI (n=28). A subset of adolescents took part in both pre- and post-treatment fMRI (n=14), and demographics are also reported for this overlapping subset.
| Demographic | Pre-fMRI only | Pre/post subset | ||
|---|---|---|---|---|
| Age – years | 17.1 ± 1.2 | 17 ± 1.3 | ||
| Sex | Male | 18 | 9 | |
| Female | 10 | 5 | ||
| Baseline urinary cotinine – ng/ml | 876.6 ± 458.1 | 740.2 ± 342.3 | ||
| Cigarettes per day | 14.1 ± 8.1 | 14.1 ± 9.1 | ||
| Age of initiation – years | 12.1 ± 2.4 | 12.0 ± 2.9 | ||
| mFTQ | 3.38 ± 1.4 | 3.23 ± 1.58 | ||
| BIS | 18.9 ± 3.34 | 18 ± 3.7 | ||
| BAS | 41.7 ± 4.97 | 40.5 ± 5.6 | ||
| Patch No | 7 | 3 | ||
| Placebo | 10 | 0 | ||
| Yes | 11 | 11 | ||
| Completed treatment | No | 6 | 0 | |
| Yes | 22 | 14 | ||
| Percent days of abstinence | 70.7 ± 30.8 | |||
mFTQ, modified Fagerström Tolerance Questionnaire (Prokhorov et al., 2001); BAS, behavioral activation system score; BIS, behavioral inhibition system score.
2.2. Smoking cessation trials
Adolescents first scheduled a quit date and participated in a behavioral therapy session 4–7 days before their quit day, during which motivational and cognitive behavioral strategies were used to emphasize the risks of continued smoking and the benefits of quitting and to teach strategies to initiate cigarette abstinence. Data were collapsed across several trials (Krishnan-Sarin et al., 2013b; NCT01145001) to improve power for fMRI analysis. Ten adolescents had only pre-treatment fMRI: three took part in an 8-week pilot study and seven took part in a 4-week trial, both in which they were randomized to receive either CBT, contingency management (CM) for abstinence, or CBT along with CM for abstinence. Eighteen adolescents had the opportunity to take part in pre- and post-treatment fMRI (14 completed the MID task at both fMRI sessions): these adolescents took part in a 6-week trial in which they were randomized to receive CBT and either nicotine patch (21 mg/day) or placebo patch, and either CM for abstinence and patch compliance or CM for patch compliance alone. Treatment groups were therefore: (a) CBT (n=3); (b) CM for abstinence (n=3); (c) CBT and CM for abstinence (n=4); (d) CBT, nicotine patch and CM for abstinence (n=4); (e) CBT, nicotine patch and CM for patch compliance (n=7); (f) CBT, placebo patch and CM for abstinence (n=3); (g) CBT, placebo patch and CM for patch compliance (n=4). CBT and CM were manual-guided and supervised by a licensed clinical psychologist (see Krishnan-Sarin et al., 2013b; NCT01145001). Self-reported smoking was collected weekly via Time Line Follow Back (TLFB) (Sobell and Sobell, 1992) and percent days of abstinence was calculated for the 4–8 week treatment.
2.3. fMRI monetary incentive delay task
Prior to their quit date, all adolescents (n=28) chose to participate in an optional pretreatment fMRI. One to 17 days after the end of treatment, a subset of adolescents (n=14) chose to participate in a post-treatment fMRI. The range of time between pre- and post-treatment fMRI was therefore 6–10 weeks. Participants were asked not to smoke for one hour prior to scanning. Each fMRI session included two runs of a modified MIDT (modified from: Knutson et al., 2000) that parses anticipation into an “A1” phase representing motor anticipation and the prospect of working for a monetary reward/punishment and an “A2” phase representing the actual anticipation of monetary reward/punishment (Andrews et al., 2011; Balodis et al., 2012; Balodis et al., 2013). Each run included 55 trials lasting 12 s each. Each trial included reward prospect (A1), anticipation (A2) and outcome (OC) phases. During the reward prospect (A1) phase, participants viewed a cue (1000 ms) signaling the potential win or loss of money ($0, $1 or $5) and then fixated on a crosshair (variable delay of 3–5 s). During the reward anticipation (A2) phase, a target (a box) appeared onscreen (variable duration, individually calibrated), and participants pressed a button and then fixated on a crosshair (variable delay of 4–6 s). They were instructed to press a button when the target appeared and while it was onscreen in order to win or avoid losing money. Finally, during the outcome phase (OC), they received feedback (1200 ms) on the win or loss of money and viewed their cumulative earnings on the task. fMRI image acquisition was time-locked to cue offset, and trial types were pseudorandomized within each fMRI session. Adolescents practiced the task before scanning to minimize learning effects, and their practice session was used to calibrate in-scanner task difficulty (i.e., cue duration) to target wins on two-thirds of trials. They were informed that their compensation would be influenced by their in-scanner task performance.
2.4. fMRI acquisition
Images were obtained with a Siemens TIM Trio 3T MRI system. High-resolution anatomical images were acquired using a magnetization-prepared rapid gradient-echo sequence (repetition time [TR]=2530ms, echo time [TE]=3.34ms, flip angle 7°, 256×256 in-plane matrix, 1mm slices, 176 slices). Functional images were acquired using an echo-planar image gradient-echo pulse sequence (TR=1500ms, TE=27ms, flip angle 60°, field of view [FOV]=220×220, 64×64 matrix, 4mm slice thickness with 1mm skip, 25 slices). Each run acquired 486 volumes including 9s to reach signal stability that was discarded from analysis.
2.5. Image preprocessing and analysis
Image analysis used SPM12 (www.fil.ion.ucl.ac.uk/spm/software/spm12). Functional images were realigned for motion correction. Artifact Detection Tools (ART; www.nitrc.org/projects/artifact_detect) toolbox was used to identify outliers in mean global intensity (>3 standard deviations [SD] from the mean global signal) and motion (>1mm). The structural image was co-registered to the mean functional image and segmented. All images were normalized to the Montreal Neurological Institute (MNI) brain (Mazziotta et al., 1995) and smoothed using a 6mm Gaussian kernel. First-level models included regressors for each phase (A1/A2/OC) of each trial type (win/loss/neutral), with $1 and $5 trials combined by trial type to improve power. Fixation was modeled as implicit baseline. Regressors of no interest were included for motion parameters and outliers detected by ART. Four adolescents at each fMRI session completed only one run of the MIDT and two additional runs (n=2) were omitted due to excessive motion (>20% outliers); first-level contrasts were scaled to adjust for the missing data. The conditions were modeled using a boxcar function convolved with a canonical hemodynamic response function combined with time derivatives, and regressors were fit using SPM 12’s implementation of the general linear model. Analysis focused on win anticipation (A2 win) and loss anticipation (A2 loss) based on reported differences in reward anticipation in the MIDT in adolescent smokers (Peters et al., 2011), and because our previous work has found reduced ventral striatal activity specifically during the A2 phase in individuals at-risk for or with addictions (Andrews et al., 2011; Balodis et al., 2012). Win/loss anticipation was modeled relative to implicit baseline rather than neutral trials based on arguments of inter-subject variability in non-gain-related processing during neutral trials (Balodis and Potenza, 2015). An exploratory second-level whole brain analysis was conducted (see supplement1).
2.6. Region of interest (ROI) analysis
ROIs included the left and right nucleus accumbens (NAc) and insula, and the medial prefrontal cortex (MPFC). The NAc and insula ROIs were anatomical masks from Wake Forest University PickAtlas (http://fmri.wfubmc.edu/software/pickatlas). The MPFC was a 10mm radius sphere centered at (5, 45, 0) based on the MPFC peak from a meta-analysis of fMRI studies of reward anticipation using the MIDT or similar cued response tasks (Knutson and Greer, 2008). MarsBar (Brett et al., 2002) was used to extract the ROI data for each functional image to a voxel time course for each voxel in the ROI; calculate a summary time course for each ROI as the mean of the voxel values in the ROI; estimate the fMRI model with the ROI data; and apply a contrast to the model to derive an effect size (i.e., contrast value) for the ROI.
2.7. Behavioral inhibition/behavioral approach measure
The behavioral inhibition system/behavioral approach system (BIS/BAS) scale is a 24-item self-report to assess dispositional BIS (e.g., “I worry about making mistakes”) and BAS (e.g., “I crave excitement and new sensations”) sensitivities (Carver and White, 1994). The relevant items are scored and summed such that higher total scores indicate higher BIS or BAS sensitivity. BIS/BAS was completed 5–9 days prior to quit date. One adolescent did not complete the BIS/BAS.
2.8. Statistical analysis
Analyses used SPSS 22 (www.ibm.com/analytics/us/en/technology/spss/). To evaluate whether reward anticipation-related ROI activity increased pre- to post-treatment in adolescent smokers, repeated measures analyses of variance were tested with time point (pre/post) and ROI (left/right NAc and insula, MPFC) as within-subjects factors, separately for A2 win/loss (n=14). Post-hoc pairwise comparisons were used to test the mean difference between time points for each ROI. To test our primary hypothesis that increases in ROI activity pre- to post-treatment were related to reduced smoking, one-tailed Spearman’s correlations were tested between change in ROI activity and percent days of abstinence during treatment. Exploratory two-tailed Spearman’s correlations were tested between pre-treatment ROI activity and percent days of abstinence during treatment for those with complete smoking data (n=20).
To test our secondary hypothesis that higher BAS scores were related to greater reward responsiveness, separate linear regressions were tested for each ROI, with pre-treatment ROI activity during A2 win/loss as the dependent variable and BIS/BAS scores as independent variables (n=27; one participant did not complete the BIS/BAS). SPSS 22 default casewise diagnostics was used to detect and remove outliers with residuals >3 SD from the mean. Finally, two-tailed Spearman’s correlations were tested between change in ROI activity and BIS/BAS scores.
3. Results
3.1. Pre- to post-treatment changes in brain activity
A significant effect of time (pre/post) on ROI activity during A2 win was observed (F(1,13)=9.11, p=.01), and remained significant when including between-subjects factors for treatment group (F(1,10)=7.33, p=.022), sex (F(1,12)=8.26, p=.014) or age (F(1,9)=7.72, p=.021), or when including group, sex and age in the same model (F(1,3)=41.99, p=.007). No effect of ROI (F(1,10)=2.11, p=.154) or time by ROI interaction (F(1,10)=0.86, p=.52) was found. Significant pre- to post-treatment increases in ROI activity during A2 win were observed in all ROIs (Figure 1): left NAc (t=−2.53, df=13, p=.025), right NAc (t=−2.61, df=13, p=.022), left insula (t=−2.94, df=13, p=.011), right insula (t=−2.37, df=13, p=.034) and MPFC (t=−2.76, df=13, p=.016).
Figure 1.
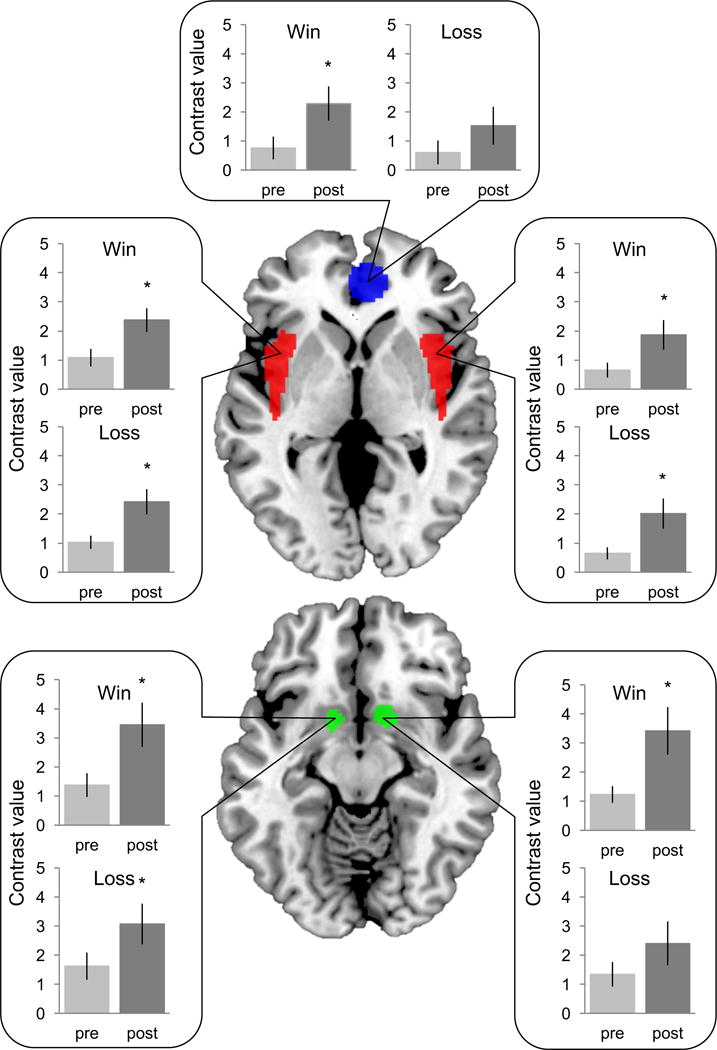
Pre- to post-treatment increases in regions of interest activity during reward anticipation (A2 win/loss) in adolescent smokers, for the medial prefrontal cortex (blue), bilateral insula (red) and bilateral nucleus accumbens (green). *p<.05, n=14.
A significant effect of time (pre/post) on ROI activity during A2 loss was observed (F(1,13)=6.50, p=.024), and remained significant when including between-subjects factors for treatment group (F(1,10)=9.81, p=.011), sex (F(1,12)=6.11, p=.029) or age (F(1,9)=7.45, p=.023), and when including group, sex and age in the same model (F(1,3)=154.55, p=.001). No effect of ROI (F(1,10)=1.65, p=.237) or time by ROI interaction (F(1,10)=0.4, p=.76) was found. Significant pre- to post-treatment increases in ROI activity during A2 loss were found in most ROIs (Figure 1): left NAc (t=−2.33, df=13, p=.037), left insula (t=−2.74, df=13, p=.017), right insula (t=−2.48, df=13, p=.028); except the right NAc (t=−1.51, df=13, p=.155) and MPFC (t=−1.40, df=13, p=.186).
3.2. Pre- to post-treatment changes in brain activity and reduced smoking
As predicted, significant positive correlations were found between percent days of abstinence during treatment and pre- to post-treatment increases in ROI activity for A2 win in the left NAc (r=.52, p=.029), left insula (r=.56, p=.02) and MPFC (r=.57, p=.017). A significant positive correlation was also found between percent days of abstinence during treatment and pre- to post-treatment increases in ROI activity for A2 loss in the left NAc (r=.58, p=.016). (Figure 2).
Figure 2.
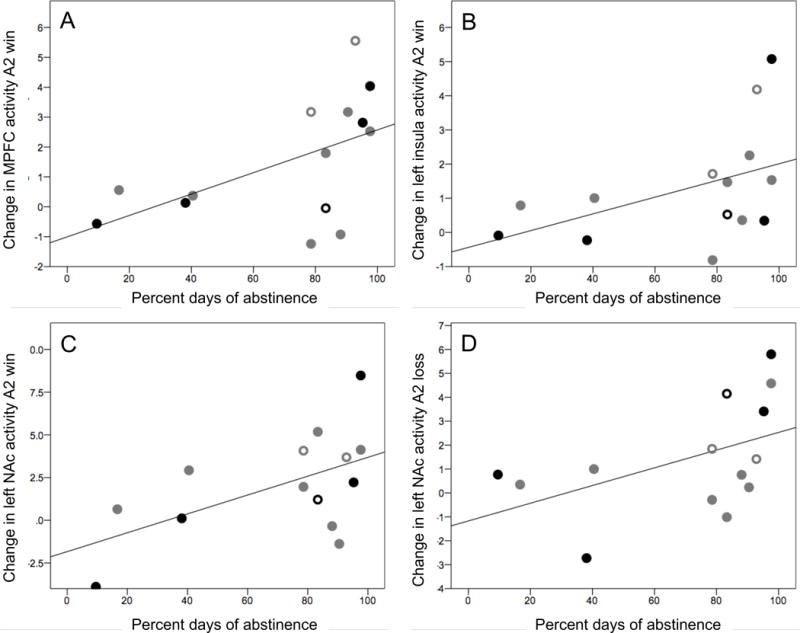
Pre- to post-treatment change in regions of interest activity during reward anticipation correlated with percent days of abstinence during treatment, for A2 win in the (A) medial prefrontal cortex (MPFC), (B) left insula and (C) left nucleus accumbens (NAc), and (D) for A2 loss in the left NAc. Black circles indicate adolescents who received contingency management (CM) for abstinence and patch compliance, gray circles received CM for patch compliance alone; closed circles received nicotine patch, open circles received placebo patch.
3.3. Pre-treatment brain activity and reduced smoking
A significant negative correlation was found between percent days of abstinence during treatment and pre-treatment ROI activity for A2 loss in the left insula (r=−.50, p=.023, n=20). No correlations were found with pre-treatment ROI activity for A2 win.
3.4. Pre-treatment brain activity and BIS/BAS scores
BAS scores were positively associated with pre-treatment ROI activity for A2 win in the left NAc (β=.577, t=2.80, p=.01), and BIS/BAS scores together explained a significant proportion of the variance in the left NAc during A2 win (R2[adjusted]=.216, F(1,25)=4.45, p=.023). BAS scores were also positively associated with pre-treatment ROI activity for A2 win in the right NAc (β=.594, t=2.85, p=.009), and BIS/BAS scores together explained a significant proportion of the variance in the right NAc during A2 win (R2=.203, F(1,25)=4.19, p=.028). BIS scores were negatively associated with pre-treatment ROI activity during A2 win in the right insula (β=−.521, t=−2.48, p=.02), and BIS/BAS scores together explained a significant proportion of the variance in the right insula during A2 win (R2=.18, F(1,26)=3.84, p=.036). BIS scores were also negatively associated with pre-treatment ROI activity during A2 loss in the left insula (β=−.47, t(25)= −2.14, p=.043). (Table 2; see supplement Figure S12).
Table 2.
Multiple linear regressions describing the effects of behavioral inhibition system (BIS) and behavioral activation system (BAS) scores on pre-treatment region of interest activity during reward (win/loss) anticipation in adolescent smokers.
| Left NAc | Right NAc | MPFC | Left insula | Right insula | |
|---|---|---|---|---|---|
| Win anticipation | β (p) | β (p) | β (p) | β (p) | β (p) |
| BIS | −.11 (.59) † | −.39 (.07)† | .20 (.40) | −.03 (.90) | −.52(.02) |
| BAS | .58 (.01) † | .59 (.009) † | −.096 (.69) | .29 (.22) | .06 (.79) |
| Loss anticipation | |||||
| BIS | −.20 (.39) † | .24 (.32) | .12 (.61) | −.47 (.04) † | .05 (.81) † |
| BAS | .42 (.07) † | .05 (.82) | .18 (.46) | .08 (.72) † | .36 (.13) † |
one outlier was removed (the same outlier); NAc, nucleus accumbens; MPFC, medial prefrontal cortex; β = beta value, bold indicates significance (p<.05).
3.5. Pre- to post-treatment changes in brain activity and BIS/BAS scores
As predicted, BAS scores positively correlated with pre- to post-treatment increases in reward anticipation-related ROI activity during A2 win in the left NAc (r=.50, p=.04 one-tailed; p=.079 two-tailed). BIS scores positively correlated with pre- to post-treatment increases in reward anticipation-related ROI activity during A2 win in the left insula (r=.69, p=.009, two-tailed) and MPFC (r=.62, p=.024, two-tailed). No significant correlations were found between BIS or BAS and changes in ROI activity during A2 loss. One adolescent did not complete the BIS/BAS. (see supplement Figure S22).
4. Discussion
This study evaluated brain activity during monetary reward anticipation in adolescent smokers participating in smoking cessation treatment, to better understand how brain correlates of reward processing relate to smoking abstinence in adolescents. Adolescent smokers have previously demonstrated lower ventral striatal activity during monetary reward anticipation that was associated with higher smoking frequency (Peters et al., 2011). The current findings suggest that adolescents who reduced their smoking frequency during treatment showed correlated pre- to post-treatment increases in frontostriatal activity during monetary reward anticipation. In both our study and that by Peters et al., left NAc activity related to smoking frequency. The NAc has a central role in reward-seeking behavior (Ikemoto and Panksepp, 1999) and codes positive incentive values (Knutson, 2001). Blunted responses in the NAc to nondrug (i.e., monetary) rewards have been repeatedly implicated in tobacco addiction (e.g., Buhler et al., 2010; Lessov-Schlaggar et al., 2013; Sweitzer et al., 2015). Several studies report that individuals with lower ventral striatal response to monetary rewards during short-term abstinence were more likely to smoke despite monetary incentives for continued abstinence (Sweitzer et al., 2015; Wilson et al., 2014). For example, smokers with lower ventral striatal activity during monetary reward anticipation after 24hr abstinence were more likely to lapse in a 3wk contingency management-supported quit attempt (Sweitzer et al., 2015). Our finding that reduced smoking was linked to increases in monetary reward anticipation (win/loss)-related NAc activity suggests that, at least among youth, reduced smoking may “reverse” some smoking-related deficits in NAc responsiveness.
Reduced smoking was also correlated with pre- to post-treatment increases in reward (win) anticipation-related MPFC activity. The MPFC contributes to goal-directed behavior in response to motivational salience and reward expectation (Goldstein and Volkow, 2002), and prefrontal supervisory functions may be down-regulated in addiction (Goldstein and Volkow, 2002). Together, the prefrontal cortex and NAc contribute to the initiation of drug-seeking behaviors (Kalivas and Volkow, 2005). Our findings suggest that for adolescent smokers, reducing smoking may “reverse” addiction-related changes in MPFC and NAc reward responsiveness and possibly increase the value of nondrug reinforcers. This suggests that interventions that provide nondrug reinforcers, such as contingency management, or increase the salience and motivational value of nondrug rewards, such as behavioral activation therapy (MacPherson et al., 2010), may be beneficial to help maintain smoking abstinence (Kalivas and Volkow, 2005) among youth. Furthermore, whereas acute nicotine delivery (i.e., nicotine patch during fMRI) was found to be insufficient to recover reduced reward-related frontostriatal activity in smokers (Rose et al., 2012), varenicline has been found to reduce the salience of primary rewards such as high monetary gain on the MID task (Fedota et al., 2015), an effect which may contribute to the efficacy of varenicline and similar pharmacological interventions compared with nicotine replacement therapy for smoking cessation.
Individual differences in BIS/BAS sensitivities also related to brain activity during reward anticipation. As predicted, BAS scores were positively associated with reward (win) anticipation-related NAc activity at pre-treatment and with increases in win-anticipation-related NAc activity pre- to post-treatment. Moreover, increases in win-anticipation-related NAc activity correlated with reduced smoking. BAS scores indicate reward responsiveness or motivated behavior in response to reward signals (Carver and White, 1994; Franken et al., 2006). The neurobiology of BAS involves the dopaminergic reward system including the NAc (Depue and Collins, 1999; Knutson and Cooper, 2005). BAS scores have been previously associated with responses to appetitive stimuli in reward-related brain regions including the ventral striatum (e.g., Beaver et al., 2006; Kelley, 2004), and linked to disordered approach behaviors including substance abuse (Franken, 2002; Franken et al., 2006; Knyazev, 2004). Higher BAS sensitivity in young adults and adults has been related to higher likelihood of being a smoker (O’Connor et al., 2009; Tapper et al., 2015), and to higher smoking frequency (Tapper et al., 2015; Voigt et al., 2009). Subscales of the BAS (fun-seeking, reward responsiveness and drive) have been related to smoking status in young adults (Baumann et al., 2014). BAS subscales were not evaluated here due to a lack of power to examine the four-factor BIS/BAS structure; however, a recent study validated the two-factor BIS/BAS in a large group of adolescents (Yu et al., 2011). One interpretation of our findings is that adolescents who are more responsive to rewards as indicated by high BAS may respond better to incentive-based (including monetary) smoking cessation interventions. High BAS is also associated with impulsivity, and in an earlier study, adolescents who reported higher impulsivity were more likely to report interest in incentive-based smoking cessation programs (Morean et al., 2014), and responded better when treatment included a behavioral incentive for abstinence (Morean et al., 2015).
BIS scores negatively correlated with insula activity during reward (win/loss) anticipation at pre-treatment, and positively correlated with increases in win-anticipation-related insula activity pre- to post-treatment. BIS scores indicate sensitivity to negative reinforcement and the tendency to inhibit behavior that may result in negative outcomes (Carver and White, 1994; Gray and McNaughton, 2000). Adolescence is typically a period of heightened reward sensitivity without appropriate behavioral inhibition (Somerville et al., 2010). Disordered behavioral inhibition may be a risk factor for or predictor of substance use including smoking (Iacono et al., 1999), possibly due to an impaired ability to anticipate the negative consequences of these behaviors (Dinn et al., 2004). The insula is activated in response to smoking-related cues in smokers (Engelmann et al., 2012) and is implicated the interoceptive effects of smoking and the subjective experiences of craving (Naqvi et al., 2014). Pre-treatment smoking cue-reactivity in the insula has been correlated with smoking lapses during an 8-week treatment (Janes et al., 2010). Likewise, damage to the insula by stroke was found to disrupt tobacco addiction (Naqvi et al., 2007). Related to nondrug rewards, fMRI studies using the MIDT report increased insula activity during win/loss anticipation that may reflect arousal to uncertain outcomes in general (Knutson and Greer, 2008). Therefore, one possible and currently speculative interpretation of our findings is that adolescent smokers who are more sensitive to negative outcomes as indicated by high BIS show lower arousal in response to uncertain outcomes in general as indicated by low insula activity during win/loss anticipation on the MIDT. Again, our findings indicate some potential “recovery” of this response across treatment.
BIS scores also positively correlated with pre- to post-treatment increases in reward (win) anticipation-related MPFC activity. Greater inhibition-related MPFC activity has been associated with reduced smoking and reduced dependence in adolescents (Galvan et al., 2011). Lower reward-related MPFC activity has been associated with poor self-control and low motivation in individuals with addictions (Goldstein et al., 2007; Goldstein and Volkow, 2002). In the current study, reward-related MPFC activity also increased pre- to post-treatment and positively correlated with reduced smoking. Taken together, these findings suggest that particularly among adolescent smokers with high BIS sensitivity, reduced smoking may lead to increases in reward-related MPFC activity. More work is needed to evaluate whether these changes reflect increases in inhibition-related MPFC activity that may be relevant to treatment.
Interpretation of these findings would be strengthened by comparison with a control group of adolescent nonsmokers to differentiate the observed effects from typical developmental changes in reward processing. Maladaptive reward seeking and risky behaviors are often seen during adolescence, when the neural circuitry implicated in reward processing and decision-making continues to develop (Fareri et al., 2008). Brain structural and functional developmental changes are ongoing in the prefrontal cortex and limbic regions critical for reward processing, and impaired reward responsiveness may lead adolescents to seek novel positive reinforcers such as smoking (Spear, 2000). Neural reward responses change across development, such as lower ventral striatal activity in response to reward (win) anticipation in adolescents compared with young adults (Bjork et al., 2004). A recent large longitudinal fMRI study reported that within-subject reward anticipation-related NAc activity increased from childhood to adolescence and decreased from adolescence to young adulthood (Heitzeg et al., 2014). Most participants in that study were children of individuals with alcohol use disorders, and NAc response was found to mediate the effects of a genotype associated with alcohol dependence on later problems. These effects are somewhat mitigated in the present study by the relatively short time interval between fMRI scans (6–10 weeks). Nevertheless, more work is needed to differentiate the effects of development from those of reduced smoking on changes in reward processing in adolescents. Additionally, more work is warranted to evaluate whether the current findings are related to abstinence and/or treatment, as well as how they may relate to functioning of specific neurotransmitter systems.
This study was also limited by its small sample, limiting the generalizability of findings. Replication in a larger sample powered to correct for multiple comparisons is necessary. The small sample size precluded our ability to evaluate the specific effects of different treatment modalities and the effects of nicotine replacement therapy. However, previous studies have proposed neural mechanisms underlying the efficacy of these treatments (DeVito et al., 2012; Feldstein Ewing et al., 2011), and prior studies have similarly collapsed data across treatments to examine relationships between brain changes and smoking behavior as we did here (e.g., Krishnan-Sarin et al., 2013a). Finally, biochemical verification would have provided a more reliable marker of smoking abstinence versus self-report; however, we could not use cotinine to biochemically validate abstinence since some adolescents received nicotine replacement. Importantly, self-reports of percent days of abstinence have been shown to be a sensitive indicator of the effects of substance abuse treatment (Carroll et al., 2014).
In conclusion, this study demonstrates that adolescent smokers who were successful at reducing smoking during treatment showed related increases in frontostriatal responses to monetary reward anticipation. These findings improve our understanding of the neural correlates of reduced smoking during behavioral interventions in adolescents, which should inform more effective interventions. Improving smoking cessation treatments in adolescents is critical given the high rates of adolescent smoking and lifelong health implications.
Supplementary Material
Highlights.
One of the first longitudinal fMRI studies of smoking cessation treatment in adolescents.
Adolescents show increased non-drug reward-related brain activity pre- to post-treatment.
Increases in reward-related brain activity were associated with smoking abstinence.
Acknowledgments
We thank our research participants for their time and efforts. We thank Theresa Babuscio and Thomas Liss for their assistance with data management. This study was supported by National Institute on Drug Abuse grants P50 DA 009241, K12 DA00167, RL1AA017539, K01 DA039299; American Heart Association grant 14CRP18200010; CASA Columbia, and the National Center on Addictions and Substance Abuse.
Role of Funding Source:
This study was supported by National Institute on Drug Abuse grants P50 DA 009241, K12 DA00167, RL1AA017539, K01 DA039299; American Heart Association grant 14CRP18200010; CASA Columbia, and the National Center on Addictions and Substance Abuse. The views presented in the manuscript are not necessarily those of the funding agencies who did not have input into the content of the manuscript outside of funding the proposed research.
Footnotes
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Contributors:
Drs. Krishnan-Sarin, Potenza and Carroll designed the protocol and study. Dr. Garrison conducted statistical analysis and wrote the manuscript. Drs. Yip and Balodis contributed to statistical analysis. All authors approved of the final manuscript before submission.
Conflict of Interest:
Dr. Potenza has consulted for Ironwood, Lundbeck, Shire, INSYS, RiverMend Health, Opiant/Lakelight Therapeutics, and Jazz Pharmaceuticals; received research support (to Yale) from Mohegan Sun Casino, the National Center for Responsible Gaming, and Pfizer; has participated in surveys, mailings or telephone consultations related to drug addiction, impulse-control disorders or other health topics; has consulted for legal and gambling entities on issues related to impulse-control disorders; provides clinical care in the Connecticut Department of Mental Health and Addiction Services Problem Gambling Services Program; has performed grant reviews for the National Institutes of Health and other agencies; has edited/guest-edited journals or sections thereof; has given academic lectures in grand rounds, CME events and other clinical or scientific venues; and has generated books or book chapters for publishers of mental health texts. Drs. Garrison, Yip, Balodis, Carroll and Krishnan-Sarin report no potential conflicts of interest.
References
- Andrews MM, Meda SA, Thomas AD, Potenza MN, Krystal JH, Worhunsky P, Stevens MC, O’Malley S, Book GA, Reynolds B, Pearlson GD. Individuals family history positive for alcoholism show functional magnetic resonance imaging differences in reward sensitivity that are related to impulsivity factors. Biol Psychiatry. 2011;69:675–683. doi: 10.1016/j.biopsych.2010.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balodis IM, Kober H, Worhunsky PD, Stevens MC, Pearlson GD, Potenza MN. Diminished frontostriatal activity during processing of monetary rewards and losses in pathological gambling. Biol Psychiatry. 2012;71:749–757. doi: 10.1016/j.biopsych.2012.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balodis IM, Kober H, Worhunsky PD, White MA, Stevens MC, Pearlson GD, Sinha R, Grilo CM, Potenza MN. Monetary reward processing in obese individuals with and without binge eating disorder. Biol Psychiatry. 2013;73:877–886. doi: 10.1016/j.biopsych.2013.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balodis IM, Potenza MN. Anticipatory reward processing in addicted populations: A focus on the monetary incentive delay task. Biol Psychiatry. 2015;77:434–444. doi: 10.1016/j.biopsych.2014.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumann M, Oviatt D, Garza R, Gonzalez-Blanks A, Lopez S, Alexander-Delpech P, Beason F, Petrova V, Hale W. Variation in bas-bis profiles across categories of cigarette use. Addict Behav. 2014;39:1477–1483. doi: 10.1016/j.addbeh.2014.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaver JD, Lawrence AD, van Ditzhuijzen J, Davis MH, Woods A, Calder AJ. Individual differences in reward drive predict neural responses to images of food. J Neurosci. 2006;26:5160–5166. doi: 10.1523/JNEUROSCI.0350-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjork JM, Knutson B, Fong GW, Caggiano DM, Bennett SM, Hommer DW. Incentive-elicited brain activation in adolescents: Similarities and differences from young adults. J Neurosci. 2004;24:1793–1802. doi: 10.1523/JNEUROSCI.4862-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brett M, Anton J, Valabregue J. Region of interest analysis using an SPM toolbox. 8th International Conference on Functional Mapping of the Human Brain; Sendai, Japan. 2002. [Google Scholar]
- Buhler M, Vollstadt-Klein S, Kobiella A, Budde H, Reed LJ, Braus DF, Buchel C, Smolka MN. Nicotine dependence is characterized by disordered reward processing in a network driving motivation. Biol Psychiatry. 2010;67:745–752. doi: 10.1016/j.biopsych.2009.10.029. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Kiluk BD, Nich C, DeVito EE, Decker S, LaPaglia D, Duffey D, Babuscio TA, Ball SA. Toward empirical identification of a clinically meaningful indicator of treatment outcome: Features of candidate indicators and evaluation of sensitivity to treatment effects and relationship to one year follow up cocaine use outcomes. Drug Alcohol Depend. 2014;137:3–19. doi: 10.1016/j.drugalcdep.2014.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, White TL. Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: The bis/bas scales. J Pers Soc Psychol. 1994;67:319–333. [Google Scholar]
- Chase HW, Eickhoff SB, Laird AR, Hogarth L. The neural basis of drug stimulus processing and craving: An activation likelihood estimation meta-analysis. Biol Psychiatry. 2011;70:785–793. doi: 10.1016/j.biopsych.2011.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depue RA, Collins PF. Neurobiology of the structure of personality: Dopamine, facilitation of incentive motivation, and extraversion. Behav Brain Sci. 1999;22:491–517. 518–469. doi: 10.1017/s0140525x99002046. [DOI] [PubMed] [Google Scholar]
- DeVito EE, Worhunsky PD, Carroll KM, Rounsaville BJ, Kober H, Potenza MN. A preliminary study of the neural effects of behavioral therapy for substance use disorders. Drug Alcohol Depend. 2012;122:228–235. doi: 10.1016/j.drugalcdep.2011.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinn WM, Aycicegi A, Harris CL. Cigarette smoking in a student sample: Neurocognitive and clinical correlates. Addict Behav. 2004;29:107–126. doi: 10.1016/j.addbeh.2003.07.001. [DOI] [PubMed] [Google Scholar]
- Engelmann JM, Versace F, Robinson JD, Minnix JA, Lam CY, Cui Y, Brown VL, Cinciripini PM. Neural substrates of smoking cue reactivity: A meta-analysis of fmri studies. Neuroimage. 2012;60:252–262. doi: 10.1016/j.neuroimage.2011.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fareri DS, Martin LN, Delgado MR. Reward-related processing in the human brain: Developmental considerations. Dev Psychopathol. 2008;20:1191–1211. doi: 10.1017/S0954579408000576. [DOI] [PubMed] [Google Scholar]
- Fedota JR, Sutherland MT, Salmeron BJ, Ross TJ, Hong LE, Stein EA. Reward anticipation is differentially modulated by varenicline and nicotine in smokers. Neuropsychopharmacology. 2015;40:2038–2046. doi: 10.1038/npp.2015.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldstein Ewing SW, Filbey FM, Hendershot CS, McEachern AD, Hutchison KE. Proposed model of the neurobiological mechanisms underlying psychosocial alcohol interventions: The example of motivational interviewing. J Stud Alcohol Drugs. 2011;72:903–916. doi: 10.15288/jsad.2011.72.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franken IH. Behavioral approach system (BAS) sensitivity predicts alcohol craving. Pers Individ Dif. 2002;32:349–355. [Google Scholar]
- Franken IH, Muris P, Georgieva I. Gray’s model of personality and addiction. Addict Behav. 2006;31:399–403. doi: 10.1016/j.addbeh.2005.05.022. [DOI] [PubMed] [Google Scholar]
- Galvan A, Poldrack RA, Baker CM, McGlennen KM, London ED. Neural correlates of response inhibition and cigarette smoking in late adolescence. Neuropsychopharmacology. 2011;36:970–978. doi: 10.1038/npp.2010.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein RZ, Alia-Klein N, Tomasi D, Zhang L, Cottone LA, Maloney T, Telang F, Caparelli EC, Chang L, Ernst T, Samaras D, Squires NK, Volkow ND. Is decreased prefrontal cortical sensitivity to monetary reward associated with impaired motivation and self-control in cocaine addiction? Am J Psychiatry. 2007;164:43–51. doi: 10.1176/appi.ajp.164.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein RZ, Volkow ND. Drug addiction and its underlying neurobiological basis: Neuroimaging evidence for the involvement of the frontal cortex. Am J Psychiatry. 2002;159:1642–1652. doi: 10.1176/appi.ajp.159.10.1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray JA. A critique of Eysenck’s theory of personality. In: Eysenck HJ, editor. A model for personality. Springer-Verlag; Berlin: 1981. pp. 246–276. [Google Scholar]
- Gray JA. Framework for a taxonomy of psychiatric disorder. In: van Goozen S, Van de Poll N, editors. Emotions: Essays on emotion theory. Lawrence Erlbaum Associates; Mahwah, NJ: 1994. pp. 29–59. [Google Scholar]
- Gray JA, McNaughton N. The neuropsychology of anxiety: An enquiry into the functions of the septo-hippocampal system. Oxford University Press; New York: 2000. [Google Scholar]
- Harakeh Z, Scholte RH, de Vries H, Engels RC. Association between personality and adolescent smoking. Addict Behav. 2006;31:232–245. doi: 10.1016/j.addbeh.2005.05.003. [DOI] [PubMed] [Google Scholar]
- Heitzeg MM, Villafuerte S, Weiland BJ, Enoch MA, Burmeister M, Zubieta JK, Zucker RA. Effect of gabra2 genotype on development of incentive-motivation circuitry in a sample enriched for alcoholism risk. Neuropsychopharmacology. 2014;39:3077–3086. doi: 10.1038/npp.2014.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hommer DW, Bjork JM, Gilman JM. Imaging brain response to reward in addictive disorders. Ann N Y Acad Sci. 2011;1216:50–61. doi: 10.1111/j.1749-6632.2010.05898.x. [DOI] [PubMed] [Google Scholar]
- Iacono WG, Carlson SR, Taylor J, Elkins IJ, McGue M. Behavioral disinhibition and the development of substance-use disorders: Findings from the Minnesota Twin Family Study. Dev Psychopathol. 1999;11:869–900. doi: 10.1017/s0954579499002369. [DOI] [PubMed] [Google Scholar]
- Ikemoto S, Panksepp J. The role of nucleus accumbens dopamine in motivated behavior: A unifying interpretation with special reference to reward-seeking. Brain Res Brain Res Rev. 1999;31:6–41. doi: 10.1016/s0165-0173(99)00023-5. [DOI] [PubMed] [Google Scholar]
- Janes AC, Pizzagalli DA, Richardt S, de BFB, Chuzi S, Pachas G, Culhane MA, Holmes AJ, Fava M, Evins AE, Kaufman MJ. Brain reactivity to smoking cues prior to smoking cessation predicts ability to maintain tobacco abstinence. Biol Psychiatry. 2010;67:722–729. doi: 10.1016/j.biopsych.2009.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalivas PW, Volkow ND. The neural basis of addiction: A pathology of motivation and choice. Am J Psychiatry. 2005;162:1403–1413. doi: 10.1176/appi.ajp.162.8.1403. [DOI] [PubMed] [Google Scholar]
- Kelley AE. Ventral striatal control of appetitive motivation: Role in ingestive behavior and reward-related learning. Neurosci Biobehav Rev. 2004;27:765–776. doi: 10.1016/j.neubiorev.2003.11.015. [DOI] [PubMed] [Google Scholar]
- Knutson B, Cooper JC. Functional magnetic resonance imaging of reward prediction. Curr Opin Neurol. 2005;18:411. doi: 10.1097/01.wco.0000173463.24758.f6. [DOI] [PubMed] [Google Scholar]
- Knutson B, Fong GW, Adams CM, Varner JL, Hommer D. Dissociation of reward anticipation and outcome with event-related fmri. Neuroreport. 2001;12:3683–3687. doi: 10.1097/00001756-200112040-00016. [DOI] [PubMed] [Google Scholar]
- Knutson B, Greer S. Anticipatory affect: Neural correlates and consequences for choice. Philos Trans R Soc Lond B Biol Sci. 2008;363:3771. doi: 10.1098/rstb.2008.0155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knutson B, Westdorp A, Kaiser E, Hommer D. Fmri visualization of brain activity during a monetary incentive delay task. Neuroimage. 2000;12:20–27. doi: 10.1006/nimg.2000.0593. [DOI] [PubMed] [Google Scholar]
- Knyazev GG. Behavioural activation as predictor of substance use: Mediating and moderating role of attitudes and social relationships. Drug Alcohol Depend. 2004;75:309–321. doi: 10.1016/j.drugalcdep.2004.03.007. [DOI] [PubMed] [Google Scholar]
- Koob GF, Volkow ND. Neurocircuitry of addiction. Neuropsychopharmacology. 2010;35:217–238. doi: 10.1038/npp.2009.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Gamez W, Schmidt F, Watson D. Linking “big” personality traits to anxiety, depressive, and substance use disorders: A meta-analysis. Psychol Bull. 2010;136:768–821. doi: 10.1037/a0020327. [DOI] [PubMed] [Google Scholar]
- Krishnan-Sarin S, Balodis IM, Kober H, Worhunsky PD, Liss T, Xu J, Potenza MN. An exploratory pilot study of the relationship between neural correlates of cognitive control and reduction in cigarette use among treatment-seeking adolescent smokers. Psychol Addict Behav. 2013a;27:526–532. doi: 10.1037/a0032479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan-Sarin S, Cavallo DA, Cooney JL, Schepis TS, Kong G, Liss TB, Liss AK, McMahon TJ, Nich C, Babuscio T, Rounsaville BJ, Carroll KM. An exploratory randomized controlled trial of a novel high-school-based smoking cessation intervention for adolescent smokers using abstinence-contingent incentives and cognitive behavioral therapy. Drug Alcohol Depend. 2013b;132:346–351. doi: 10.1016/j.drugalcdep.2013.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lessov-Schlaggar CN, Lepore RL, Kristjansson SD, Schlaggar BL, Barnes KA, Petersen SE, Madden PA, Heath AC, Barch DM. Functional neuroimaging study in identical twin pairs discordant for regular cigarette smoking. Addict Biol. 2013;18:98–108. doi: 10.1111/j.1369-1600.2012.00435.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas CP, Zhang H, Fisher PW, Shaffer D, Regier DA, Narrow WE, Bourdon K, Dulcan MK, Canino G, Rubio-Stipec M, Lahey BB, Friman P. The Disc Predictive Scales (DPS): Efficiently screening for diagnoses. J Am Acad Child Adolesc Psychiatry. 2001;40:443–449. doi: 10.1097/00004583-200104000-00013. [DOI] [PubMed] [Google Scholar]
- MacPherson L, Tull MT, Matusiewicz AK, Rodman S, Strong DR, Kahler CW, Hopko DR, Zvolensky MJ, Brown RA, Lejuez CW. Randomized controlled trial of behavioral activation smoking cessation treatment for smokers with elevated depressive symptoms. J Consult Clin Psychol. 2010;78:55–61. doi: 10.1037/a0017939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malmberg M, Kleinjan M, Vermulst AA, Overbeek G, Monshouwer K, Lammers J, Engels RC. Do substance use risk personality dimensions predict the onset of substance use in early adolescence? A variable- and person-centered approach. J Youth Adolesc. 2012;41:1512–1525. doi: 10.1007/s10964-012-9775-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazziotta JC, Toga AW, Evans A, Fox P, Lancaster J. A probabilistic atlas of the human brain: Theory and rationale for its development. The international consortium for brain mapping (ICBM) Neuroimage. 1995;2:89–101. doi: 10.1006/nimg.1995.1012. [DOI] [PubMed] [Google Scholar]
- Morean ME, Camenga DR, Kong G, Cavallo DA, Schepis TS, Krishnan-Sarin S. Predictors of middle school students’ interest in participating in an incentive-based tobacco prevention and cessation program in connecticut. J Addict. 2014;2014:915652. doi: 10.1155/2014/915652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morean ME, Kong G, Camenga DR, Cavallo DA, Carroll KM, Pittman B, Krishnan-Sarin S. Contingency management improves smoking cessation treatment outcomes among highly impulsive adolescent smokers relative to cognitive behavioral therapy. Addict Behav. 2015;42:86–90. doi: 10.1016/j.addbeh.2014.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naqvi NH, Gaznick N, Tranel D, Bechara A. The insula: A critical neural substrate for craving and drug seeking under conflict and risk. Ann N Y Acad Sci. 2014;1316:53–70. doi: 10.1111/nyas.12415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naqvi NH, Rudrauf D, Damasio H, Bechara A. Damage to the insula disrupts addiction to cigarette smoking. Science. 2007;315:531–534. doi: 10.1126/science.1135926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor R, Stewart S, Watt M. Distinguishing bas risk for university students’ drinking, smoking, and gambling behaviors. Pers Individ Dif. 2009;46:514–519. [Google Scholar]
- Peters J, Bromberg U, Schneider S, Brassen S, Menz M, Banaschewski T, Conrod PJ, Flor H, Gallinat J, Garavan H, Heinz A, Itterman B, Lathrop M, Martinot JL, Paus T, Poline JB, Robbins TW, Rietschel M, Smolka M, Strohle A, Struve M, Loth E, Schumann G, Buchel C IMAGEN Consortium. Lower ventral striatal activation during reward anticipation in adolescent smokers. Am J Psychiatry. 2011;168:540–549. doi: 10.1176/appi.ajp.2010.10071024. [DOI] [PubMed] [Google Scholar]
- Prokhorov AV, Hudmon KS, de Moor CA, Kelder SH, Conroy JL, Ordway N. Nicotine dependence, withdrawal symptoms, and adolescents’ readiness to quit smoking. Nicotine Tob Res. 2001;3:151–155. doi: 10.1080/14622200110043068. [DOI] [PubMed] [Google Scholar]
- Robinson TE, Berridge KC. Incentive-sensitization and addiction. Addiction. 2001;96:103–114. doi: 10.1046/j.1360-0443.2001.9611038.x. [DOI] [PubMed] [Google Scholar]
- Rose EJ, Ross TJ, Salmeron BJ, Lee M, Shakleya DM, Huestis M, Stein EA. Chronic exposure to nicotine is associated with reduced reward-related activity in the striatum but not the midbrain. Biol Psychiatry. 2012;71:206–213. doi: 10.1016/j.biopsych.2011.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubinstein ML, Luks TL, Moscicki AB, Dryden W, Rait MA, Simpson GV. Smoking-related cue-induced brain activation in adolescent light smokers. J Adolesc Health. 2011;48:7–12. doi: 10.1016/j.jadohealth.2010.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shedler J, Block J. Adolescent drug use and psychological health: A longitudinal inquiry. Am Psychol. 1990;45:612–630. doi: 10.1037//0003-066x.45.5.612. [DOI] [PubMed] [Google Scholar]
- Sobell L, Sobell M. Timeline Follow-Back. A technique for assessing selfreported alcohol consumption. In: Litten RZ, Allen J, editors. Measuring alcohol consumption: Psychosocial and biological methods. Humana Press; New Jersey: 1992. pp. 41–72. [Google Scholar]
- Somerville LH, Jones RM, Casey BJ. A time of change: Behavioral and neural correlates of adolescent sensitivity to appetitive and aversive environmental cues. Brain Cogn. 2010;72:124–133. doi: 10.1016/j.bandc.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spear LP. The adolescent brain and age-related behavioral manifestations. Neurosci Biobehav Rev. 2000;24:417–463. doi: 10.1016/s0149-7634(00)00014-2. [DOI] [PubMed] [Google Scholar]
- Stanton A, Grimshaw G. Tobacco cessation interventions for young people. Cochrane Database Syst Rev. 2013;8:CD003289. doi: 10.1002/14651858.CD003289.pub5. [DOI] [PubMed] [Google Scholar]
- Sweitzer MM, Geier CF, Denlinger R, Forbes EE, Raiff BR, Dallery J, McClernon FJ, Donny EC. Blunted striatal response to monetary reward anticipation during smoking abstinence predicts lapse during a contingency-managed quit attempt. Psychopharmacology (Berl) 2015;233:751–60. doi: 10.1007/s00213-015-4152-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweitzer MM, Geier CF, Joel DL, McGurrin P, Denlinger RL, Forbes EE, Donny EC. Dissociated effects of anticipating smoking versus monetary reward in the caudate as a function of smoking abstinence. Biol Psychiatry. 2014;76:681–688. doi: 10.1016/j.biopsych.2013.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tapper K, Baker L, Jiga-Boy G, Haddock G, Maio G. Sensitivity to reward and punishment: Associations with diet, alcohol consumption, and smoking. Pers Individ Dif. 2015;72:79–84. [Google Scholar]
- Teplinskaya A, Gerzoff R. Youth tobacco use—United States, 2011 Centers for Disease Control and Prevention Surveillance Summary 2011 [Google Scholar]
- U.S. Department of Health and Human Services. Preventing tobacco use among youth and young adults: A report of the Surgeon General. 2012 http://www.surgeongeneral.gov.accessed/. Accessed on November 18 2015. [PubMed]
- Voigt DC, Dillard JP, Braddock KH, Anderson JW, Sopory P, Stephenson MT. Carver and white’s (1994) bis/bas scales and their relationship to risky health behaviours. Pers Individ Dif. 2009;47:89–93. [Google Scholar]
- Wilson SJ, Delgado MR, McKee SA, Grigson PS, MacLean RR, Nichols TT, Henry SL. Weak ventral striatal responses to monetary outcomes predict an unwillingness to resist cigarette smoking. Cogn Affect Behav Neurosci. 2014;14:1196–1207. doi: 10.3758/s13415-014-0285-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu R, Branje SJ, Keijsers L, Meeus WH. Psychometric characteristics of carver and white’s bis/bas scales in dutch adolescents and their mothers. J Pers Assess. 2011;93:500–507. doi: 10.1080/00223891.2011.595745. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


