Abstract
As many as 80% of the nearly five million adults under community supervision (i.e., probation, parole) are substance involved; however, treatment utilization is low. Using a multi-site randomized controlled trial, we tested the efficacy of in-person motivational interviewing (MI), a motivational computer intervention (MAPIT), or standard probation intake (SAU) to encourage treatment initiation among 316 substance-involved probationers in Dallas, Texas and Baltimore City, Maryland. Ninety-three percent (n=295) of participants completed the 2-month follow-up and ninety percent (n=285) completed the 6-month follow-up. At 2-months, individuals in the MAPIT condition were more likely to report treatment initiation compared to the SAU condition (OR=2.40, 95% CI=1.06, 5.47) via intent-to-treat analysis, especially among those completing both sessions (RE=.50, 95% CI=.05, .95) via instrumental variable analysis. At 6-months, MAPIT approached significance for treatment initiation in both analyses. MI did not achieve significance in any model. We did not find any differential impact on substance use. The success of MAPIT suggests that an integrated health-justice computerized intervention as part of a Screening, Brief Intervention, and Referral to Treatment (SBIRT) can be used to address public safety and health issues.
Keywords: treatment initiation, substance use, computer, motivation, probation, MAPIT
1. Introduction
In 2015, nearly 25 million adults in the United States reported illicit drug use in the past month, and nearly 65 million adults reported binge alcohol use in the past month. Treatment initiation was low among substance users in need of treatment, with only 14% of those needing treatment receiving treatment services (Center for Behavioral Health Statistics and Quality, 2016). Screening, Brief Intervention, and Referral to Treatment (SBIRT) has emerged as a favored framework to identify and refer at-risk individuals to treatment. The White House, Substance Abuse Mental Health Services Administration (SAMHSA), and World Health Organization (WHO) promote SBIRT as an evidence-based intervention in settings such as emergency rooms, medical offices, schools, and specialty treatment programs (Humeniuk, Henry-Edwards, Ali, Poznyak, & Monteiro, 2010; The White House, Office of the Press Secretary, 2012; U.S. Department of Health and Human Services (HHS), Office of the Surgeon General, 2016). When implemented as a brief intervention (5–10 minutes), SBIRT has been shown to reduce risky alcohol use in adult primary care (Moyer, 2013), but does not garner the same results for illicit drug use (Hingson & Compton, 2014; Roy-Byrne, Bumgardner, & Krupski, 2014; Saitz, 2014). A recent review of 13 randomized trials found that SBIRT does not improve alcohol treatment initiation rates (Glass, Hamilton, et al., 2015); however, no such studies exist on treatment initiation for drug use. More research needs to explore whether SBIRT influences treatment initiation, which is often considered a precursor to changes in drug use.
Related research on brief counseling (2–4 sessions) provides robust support for the effectiveness of adaptations of motivational interviewing (MI) at reducing both alcohol and drug use, as well as increasing treatment initiation. MI has been widely validated as a stand-alone treatment, as a precursor to more extensive treatment, or as a clinical style for delivering other components, such as tailored feedback (Hettema, Steele, & Miller, 2005). There is also emerging evidence that MI can improve treatment compliance for individuals in the criminal justice system (McMurran, 2009). Challenges to the dissemination of MI (and SBIRT in general) include the difficulty of sustaining quality practice over time (Hall, Staiger, Simpson, Best, & Lubman, 2016). One solution is to use technology-based interventions that do not rely on provider availability or skill level. In fact, there is a substantial literature on the effectiveness of technology-based interventions at reducing substance use and related risk behaviors in primary care and specialty treatment settings (Marsch, Carroll, & Kiluk, 2014).
Of the nearly 5 million adults under community supervision (i.e., probation and parole) in the United States (Kaeble, Maruschak, & Bonczar, 2015), as many as 60 to 80 percent are substance-involved (Feucht & Gfroerer, 2011). Nearly 3.5 million individuals under community supervision are estimated to be in need of substance abuse treatment (Taxman, Perdoni, & Harrison, 2007), but only 17% access treatment services (Karberg & James, 2005). Improved rates of treatment initiation could significantly reduce failures on community supervision, which fuel the use of jail or prison incarceration as responses to continued drug use (Phelps, 2013). Technology-based interventions may be particularly well suited to justice settings where the workforce has limited training in behavioral health (Bonta, Bourgon, Rugge, et al., 2011; Chadwick, Dawolf, & Serin, 2015) and there are relatively few treatment resources available (Taxman, Perdoni, & Caudy, 2013). One study of a prison-based substance abuse computer education program found that inmates had comparable attendance at a computerized intervention and similar gains in coping skills as traditional counseling groups (Chaple, Sacks, McKendrick, et al., 2014).
This study reports on a randomized controlled trial comparing the efficacy of an in-person MI intervention, a motivational computer intervention, or standard probation intake to encourage treatment initiation and reduce substance use among substance-involved probationers in Dallas, Texas and Baltimore City, Maryland.
2. Material and Methods
2.1. Design and Procedures
We randomized substance-using probationers in Dallas, Texas and Baltimore City, Maryland to one of three conditions: a 2-session motivational computer intervention (MAPIT), a 2-session in-person MI intervention (MI), or supervision as usual (SAU). Participants in all three conditions followed the standard probation process at their respective sites. Study participants were English-speaking adults (>=18 years old) who had been recently placed on probation. Participants reported at least one instance of heavy alcohol (>=5 drinks per day for men; >=4 drinks per day for women) or any illicit drug use during the past 90 days. After consenting, participants completed a baseline assessment and were randomized to one of the study conditions. If assigned to MAPIT or MI, participants completed the first intervention session after the baseline assessment, and the second session approximately 4 weeks later. The first session targeted motivation to complete probation, initiate treatment, and obtain HIV testing. The second session emphasized goal setting, coping strategies, and social support. Participants completed follow-up assessments at 2- and 6-months post-randomization. The study protocol was reviewed and approved by the human subjects institutional review boards at George Mason University and University of North Texas Health Science Center. More detail on the study design and procedures are reported elsewhere (Taxman, Walters, Sloas, Lerch, & Rodriguez, 2015).
In terms of intervention theory, MAPIT drew from the extended parallel process model in how it framed risk messages (Witte & Allen, 2000) and Social Cognitive Theory in terms of how it presented comparative information and suggestions (Bandura, 1986). MAPIT also incorporated a number of MI-based strategies, such as open questions, affirmations, and summary statements; personalized feedback; and selective reinforcement of client responses that were consistent with change. MAPIT used theory-based algorithms and a text-to-speech engine to deliver personalized reflections, feedback, and suggestions. At the participant’s request, the program could send emails or mobile texts to remind participants of their goals. The development and content of MAPIT is described more fully elsewhere (Walters et al., 2014); samples of the program can be viewed at: http://youtu.be/9yV6bTn1tVE; http://youtu.be/XEZ5o48WwTg; http://youtu.be/u2SHWG0QXe8; http://youtu.be/wMShVdPpcsw. We structured the MI intervention similarly to MAPIT, using a tailored feedback report and activities that addressed motivation to engage in treatment and successfully complete probation. We used training and fidelity procedures similar to other large clinical trials (Project MATCH Research Group, 1993). The development and content of the MI condition is described more fully elsewhere (Spohr, Taxman, Rodriguez, & Walters, 2016; Walters, Ressler, Douglas, & Taxman, 2011).
2.2. Measures
2.2.1. Dependent measures
We created dichotomous outcomes measuring whether any substance use and/or treatment initiation occurred at follow-up. We assessed these measures via a self-report Timeline Follow-back (TLFB), a calendar-based recall system that has been widely validated in substance treatment trials (Sobell & Sobell, 1996). The primary outcome of treatment initiation was measured as two or more days of any treatment involvement (i.e., self-help, group sessions, individual sessions, in-patient, detoxification, intensive outpatient, medication, residential, religious services, or other services) at 2- and 6-month follow-up, when the participant had not been in treatment in the 30 days before randomization. This definition of treatment resembles those used in prior research (McLellan et al., 1994; Green, Polen, Dickinson, Lynch, & Bennett, 2002; Garnick, Lee, Horgan, Acevedo, & the Washington Circle Public Sector Workgroup, 2009). This definition reduces the potential inclusion of one-time only treatment attendance, such as a required substance abuse assessment visit, and ensures a reliable estimate of actual initiation. Successful recovery can be aheived through both formal (e.g., residential) and informal (e.g., self-help) modalities (Laudet, Savage, & Mahmood, 2002; De Leon, 2004; Humphreys, et al., 2004; Gossop, Stewart, & Marsden, 2015), and thus we included informal treatment modalities (e.g., self-help) to broaden our ability to identify participants who were seeking recovery outside of traditional mechanisms (De Leon, 2004). Of those who initiated treatment at the 2-month follow-up, one participant used only self-help groups (2.1%), while five participants (10.4%) used self-help with some other form of treatment as well. Of those who initiated treatment at the 6-month follow-up, one participant used only self-help groups (1.2%), while eighteen participants (20.9%) used self-help with another form of treatment. The secondary outcome of substance use was determined by any instance of heavy alcohol use (>=5 drinks per day for men; >=4 drinks per day for women), marijuana use, or hard drug use (e.g., cocaine, opiates) at 2- and 6-month follow-up.
2.2.2. Covariate measures
We examined several baseline characteristics as potential covariates. Demographic characteristics included age, race, gender, and housing stability. Composite scores from the Addiction Severity Index-Lite (ASI) (McGahan, Griffith, Parente, & McLellan, 1986) included employment/education (2-month follow-up (2MFU) α= .75; 6-month follow-up (6MFU) α= .75), alcohol (2MFU α= .77; 6MFU α= .77), drug (2MFU α= .76; 6MFU α= .76), medical (2MFU α= .91; 6MFU α= .91), and family/social (2MFU α= .66; 6MFU α= .64). We also examined measures of recidivism risk, positive screening for a mental health disorder, lifetime prior treatment, age of first substance use, and whether the participant had a court ordered requirement for substance abuse testing or treatment. Finally, we examined readiness for treatment (2MFU α= .94; 6MFU α= .94) from the Criminal Justice Client Evaluation of Self and Treatment Intake (Institute of Behavioral Research, Texas Christian University, 2005). When examining correlations between baseline characteristics covariates, we found that problem recognition and desire for help subscales were highly correlated (r = .85, p < .000). A factor analysis revealed that these two subscales loaded as a single item representing motivational readiness.
2.3. Analysis Plan
The effect size for each dependent variable was calculated based on frequency distributions unadjusted for covariates (Lipsey & Wilson, 2001). We conducted an intent-to-treat (ITT) analysis using logistic regressions to obtain an unbiased estimate of the treatment effect. This estimate tends to underestimate the effect of the treatment because it does not account for compliance to the study protocol. The noncompliance leads to endogeneity since errors in the logistic regression can be correlated with the treatment assignment. We conducted an instrumental variable (IV) analysis to account for compliance with the study condition. IV analysis considers outcomes from all participants, controlling for treatment compliance (Terza, Basu, & Rathouz, 2008; Clarke & Windmeijer, 2012). This approach gives a valid estimate of the treatment effect between compliant participants in the treatment and control conditions with an assumption that treatment assignment has no effect on non-compliant participants.
We used treatment assignment as the instrumental variable, a common technique for randomized clinical trials (Sussman & Hayward, 2010). Each of the IV models solves two equations simultaneously, with the first equation relating the binary random outcome variable to the treatment actually received (i.e., zero, one, or two sessions) and the second equation relating the binary status of treatment actually received to the treatment assignment. The model estimates the causal effect of the treatment assignment on the outcome variables. The parameter estimates presented in this paper show the treatment effects for those who complied with the intended interventions (i.e., completed both sessions). Since the outcome variable and the randomization variable were both binary, the parameter estimates were log odds ratios adjusting for treatment actually received (Burgess, Small, & Thompson, 2015). The ratio estimates from the IV analysis give the treatment effect estimates. The numerator of the ratio estimate is the difference between log odds of the outcome for the treatment and control groups. The denominator of the ratio is the difference between the compliance probabilities of the two groups. Similar to the interpretation of the odds ratio logarithm, the treatment effect is significant if the 95% confidence interval (CI) does not include 0, or the CI for the exponential of the ratio estimate does not include 1. Exponential transformation was used to convert log odds ratios to odds ratios in the IV analysis (ORIV).
Any baseline characteristics that varied significantly between study conditions or those retained versus lost to follow-up were used as covariates in the ITT and IV analyses. Because this was a multisite trial, we tested each model for the impact of the site, as presented in Table 3. Since site did not affect the model results, another model was constructed adjusting for the covariates that affected retention in the study as shown in Table 4. For more details regarding the analyses, contact the authors.
Table 3.
Intent-to-treat analyses adjusting for site only
| Outcome | 2-Month Follow-Up
|
6-Month Follow-Up
|
||
|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Treatment initiation | ||||
| MAPIT | 2.09 (0.94, 4.67) | 0.07 | 1.78 (0.96, 3.3) | 0.07 |
| MI | 1.93 (0.86, 4.35) | 0.11 | 1.23 (0.64, 2.34) | 0.53 |
|
| ||||
| Heavy alcohol use | ||||
| MAPIT | 1.44 (0.77, 2.68) | 0.25 | 1.13 (0.64, 1.99) | 0.66 |
| MI | 0.83 (0.43, 1.61) | 0.58 | 0.73 (0.41, 1.3) | 0.28 |
|
| ||||
| Marijuana use | ||||
| MAPIT | 1.11 (0.57, 2.16) | 0.76 | 1.57 (0.88, 2.82) | 0.13 |
| MI | 0.85 (0.43, 1.7) | 0.65 | 1.18 (0.65, 2.16) | 0.58 |
|
| ||||
| Hard drug use | ||||
| MAPIT | 1.11 (0.54, 2.26) | 0.78 | 1.26 (0.69, 2.29) | 0.45 |
| MI | 0.93 (0.44, 1.95) | 0.84 | 1.08 (0.58, 2.01) | 0.81 |
OR=odds ratio; CI=confidence interval; MAPIT=motivational computer program; MI=in-person motivational interviewing; reference category is SAU (i.e., research assessments only)
Table 4.
Intent-to-treat analyses adjusting for Covariates Related to Retention in the Study
| Outcome | 2-Month Follow-Up
|
6-Month Follow-Up
|
||
|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Treatment initiation | ||||
| MAPIT | 2.40 (1.06, 5.47) | 0.04 | 1.84 (0.98, 3.46) | 0.06 |
| MI | 2.15 (0.94, 4.91) | 0.07 | 1.28 (0.67, 2.46) | 0.46 |
|
| ||||
| Heavy alcohol use | ||||
| MAPIT | 1.32 (0.70, 2.48) | 0.39 | 1.03 (0.58, 1.84) | 0.91 |
| MI | 0.81 (0.42, 1.58) | 0.54 | 0.70 (0.39, 1.25) | 0.23 |
|
| ||||
| Marijuana use* | ||||
| MAPIT | 1.03 (0.52, 2.05) | 0.92 | 1.50 (0.83, 2.73) | 0.18 |
| MI | 0.86 (0.43, 1.73) | 0.68 | 1.14 (0.62, 2.11) | 0.67 |
|
| ||||
| Hard drug use** | ||||
| MAPIT | 1.22 (0.59, 2.53) | 0.59 | 1.42 (0.76, 2.63) | 0.27 |
| MI | 1.09 (0.52, 2.27) | 0.82 | 1.29 (0.69, 2.41) | 0.43 |
OR=odds ratio; CI=confidence interval; MAPIT=motivational computer program; MI=in-person motivational interviewing; reference category is SAU (i.e., research assessments only)
Stable housing significant: 2MFU marijuana use (p=0.01); 6MFU marijuana use (p=0.04)
Treatment order significant: 6MFU hard drug use (p=0.02)
3. Results
3.1. Study Flow
Figure 1 shows the Consolidated Standards of Reporting Trials (CONSORT) flow diagram. We screened 2,307 individuals and found 783 eligible. We consented and randomized 360 participants; however, 44 participants who screened as eligible were determined to be ineligible post-hoc (insufficient substance use= 23; not recently placed on probation= 18; both reasons= 3), and excluded from further analyses. The resulting sample included 316 participants (MAPIT=104, MI=103, and SAU=109). Seventy (70) percent of people assigned to MAPIT completed both sessions; 72% of people assigned to MI completed both sessions. Ninety-three (93) percent (n=295) completed the 2-month follow-up and 90% (n=285) completed the 6-month follow-up.
Figure 1.
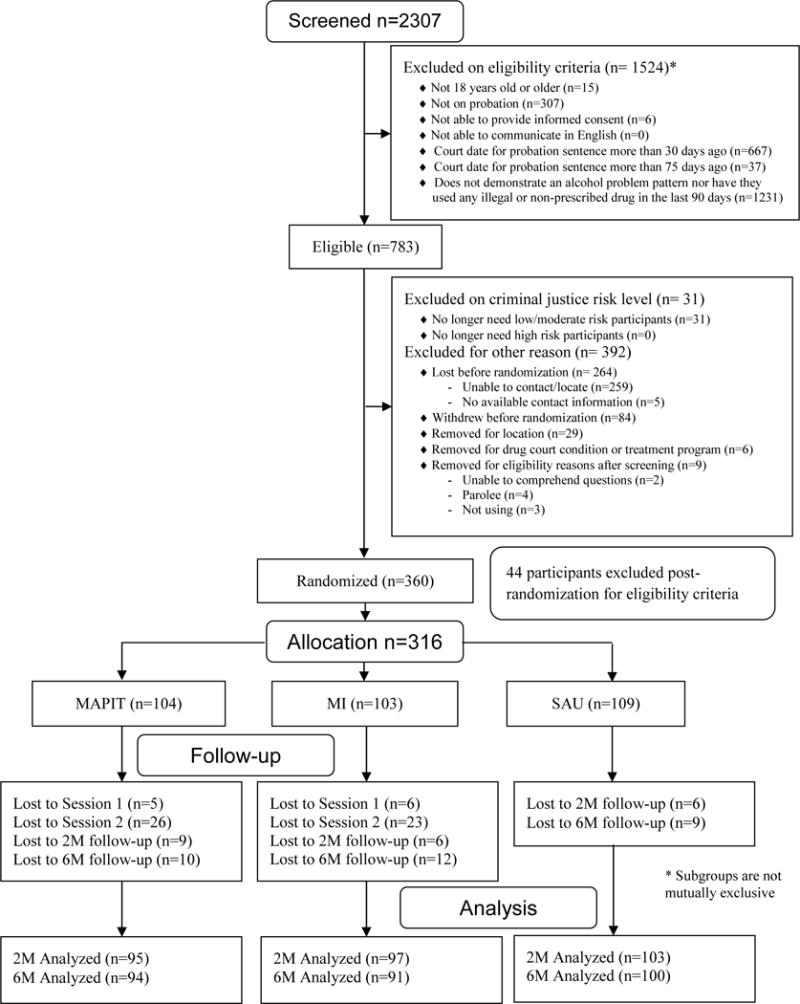
MAPIT Study CONSORT Flow Diagram
In Baltimore we screened 1,448 individuals and found 428 eligible, while in Dallas we screened 859 individuals and found 355 eligible. Of the 160 consented and randomized in Baltimore, 25 participants were deemed ineligible post-hoc (insufficient substance use= 10; not newly on probation= 12; both reasons= 3). Of the 200 consented and randomized in Dallas, 19 participants were determined to be ineligible post-hoc (insufficient substance use= 13; not newly on probation= 6). The resulting Baltimore sample was 135 (MAPIT=42, MI=46, and SAU=47), while the Dallas sample was 181 (MAPIT=62, MI=57, and SAU=62). Eighty four (84) percent of the Dallas sample completed both MAPIT sessions; 62% of Baltimore completed both MAPIT sessions. Seventy nine (79) percent of Dallas participants completed both MI sessions; 76% of Baltimore participants completed both MI sessions. Ninety one (91) percent of Baltimore participants completed the 2-month follow-up, and 87% completed the 6-month follow-up. Ninety five (95) percent of Dallas participants completed the 2-month follow-up, and 92% completed the 6-month follow-up.
3.2. Baseline Characteristics
Baseline sample characteristics were largely balanced across the study arms. Participants randomized to SAU were more likely to have a court-ordered requirement to attend substance abuse treatment (χ2(2, N=316) =8.04, p=0.02), but otherwise the study conditions were equivalent at baseline. Those lost to follow-up at 2-months were more likely to report having employment and education problems at baseline (F (1,313) = 4.31, p= 0.04), but were also more likely to report having stable housing (χ2(1, N=316) =3.84, p=0.05). Those lost to follow-up at 6-months were more likely to have a court order for substance abuse treatment at baseline (χ2(1, N=316) =5.30, p=0.02). Based on these findings and the significant relationship between these variables and several of our outcomes, we included substance abuse treatment court order, housing stability, and ASI employment/education status as covariates in the ITT and IV analyses.
There were several notable differences between the sites. As shown in Table 1, Baltimore participants tended to be older (F (1,315) = 46.98, p<0.001) and less likely to be White (χ2(1, N=315) =20.04, p<0.001). Dallas participants reported less employment and education problems (F (1,314) = 34.61, p<0.001), drug problems (F (1,315) = 31.61, p<0.001), medical problems (F (1,315) = 23.79, p<0.001), and lower motivation (F (1,313) = 23.24, p<0.001). Dallas participants were more likely to have a drug testing court order (χ2(1, N=316) =67.59, p<0.001), but were of a lower criminal justice risk (F (1,315) = 44.84, p<0.001), compared to Baltimore participants. Finally, Baltimore participants were less likely to have stable housing χ2(1, N=316) =13.86, p<0.001), but more likely to have had prior treatment experience (χ2(1, N=316) =36.74, p<0.001), compared to Dallas participants.
Table 1.
Baseline characteristics by study site (n=316)
| Study Sites
|
||
|---|---|---|
| Dallas (n=181) No.(%) or Mean ± SD | Baltimore (n=135) No.(%) or Mean ±SD | |
| Age*** | 31.4 ±10 | 39.9 ±12 |
| ASI employment/education*** | 0.6 ±0.3 | 0.8 ±0.2 |
| ASI alcohol | 0.2 ±0.2 | 0.2 ±0.1 |
| ASI drug*** | 0.1 ±0.1 | 0.2 ±0.1 |
| ASI medical*** | 0.1 ±0.2 | 0.3 ±0.4 |
| ASI family/social | 0.3 ±0.2 | 0.3 ±0.2 |
| Motivation*** | 26.6 ±9 | 31.5 ±9.5 |
| Criminal justice risk score*** | 3.7 ±2 | 5.1 ±2 |
| Race*** | ||
| White | 57 (31.7) | 14 (10.4) |
| Nonwhite | 123 (68.3) | 121 (89.6) |
| Gender | ||
| Male | 120 (66.3) | 94 (69.6) |
| Female | 61 (33.7) | 41 (30.4) |
| Housing Stability*** | ||
| Yes | 155 (85.6) | 92 (68.1) |
| No | 26 (14.4) | 43 (31.9) |
| SMI positive screen | ||
| Yes | 62 (34.3) | 56 (41.5) |
| No | 119 (65.7) | 79 (58.5) |
| Lifetime prior treatment*** | ||
| Yes | 61 (33.7) | 92 (68.1) |
| No | 120 (66.3) | 43 (31.9) |
| Age first used substance(s) | ||
| >= 16 | 67 (37.0) | 38 (28.1) |
| < 16 | 114 (63.0) | 97 (71.9) |
| Drug testing order*** | ||
| Yes | 163 (90.1) | 65 (48.1) |
| No | 18 (9.9) | 70 (51.9) |
| Treatment order | ||
| Yes | 66 (36.5) | 57 (42.2) |
| No | 115 (63.5) | 78 (57.8) |
p < .05;
p < .01;
p < .000
3.3. Effect Sizes
Table 2 shows the between-group effect sizes at 2- and 6-months. At 2-months, participants in both MAPIT (d=.41, 95% CI=−.04, .85) and MI (d=.36, 95% CI=−.09, .80) were more likely to report treatment initiation, compared to SAU. At 6-months, participants in MAPIT were more likely to report treatment initiation compared to the SAU (d=.32, 95% CI=−.02, .66). Treatment condition did not affect substance use, except that participants in MAPIT were more likely to report binge alcohol use as compared to SAU at 2-months (d=.20, 95% CI=−.14, .54) and marijuana use as compared to SAU at 6-months (d=.25, 95% CI=−.07, .57). Both were small effect sizes.
Table 2.
Outcome distributions by study condition and unadjusted effect sizes
| MI % (SD) |
MAPIT % (SD) |
SAU % (SD) |
MAPIT vs SAU, d (95% CIs) |
MI vs SAU, d (95% CIs) |
||
|---|---|---|---|---|---|---|
| Treatment Initiation | 2M | 18.6 (0.4) | 20.0 (0.4) | 10.7 (0.3) | 0.41 (−0.04, 0.85) | 0.36 (−0.09, 0.80) |
| 6M | 28.6 (0.5) | 37.2 (0.5) | 25.0 (0.4) | 0.32 (−0.02, 0.66) | 0.10 (−0.25, 0.45) | |
|
| ||||||
| Heavy alcohol use | 2M | 22.7 (0.4) | 32.6 (0.5) | 25.2 (0.4) | 0.20 (−0.14, 0.54) | −0.08 (−0.44, 0.28) |
| 6M | 41.8 (0.5) | 52.1 (0.5) | 49.0 (0.5) | 0.07 (−0.24, 0.38) | −0.16 (−0.48, 0.15) | |
|
| ||||||
| Marijuana use | 2M | 20.6 (0.4) | 24.2 (0.4) | 22.3 (0.4) | 0.06 (−0.31, 0.42) | −0.06 (−0.43, 0.32) |
| 6M | 37.4 (0.5) | 43.6 (0.5) | 33.0 (0.5) | 0.25 (−0.07, 0.57) | 0.11 (−0.22, 0.43) | |
|
| ||||||
| Hard drug use | 2M | 18.6 (0.4) | 20.0 (0.4) | 18.4 (0.4) | 0.06 (−0.33, 0.45) | 0.00 (−0.39, 0.40) |
| 6M | 34.1 (0.5) | 36.2 (0.5) | 31.0 (0.5) | 0.13 (−0.20, 0.46) | 0.08 (−0.26, 0.41) | |
3.4. Intent-to-Treat Analysis
Table 3 shows the ITT analysis adjusting for the site variable. At 2- and 6-months, MAPIT approached significance for treatment initiation compared to SAU. At two months, the odds ratio was 2.09 (95% CI=0.94, 4.67); at 6 months the odds ratio was 1.78 (95% CI=0.96, 3.3).
Table 4 shows the ITT analyses adjusted for other covariates related to study retention. At 2-months, participants in the MAPIT condition were more likely than the participants in the SAU condition to initiate treatment (odds ratio [OR]=2.40, 95% CI=1.06, 5.47). At 6-months, MAPIT approached significance for treatment initiation compared to SAU (OR=1.84, 95% CI=.98, 3.46). At 2-months, MI approached significance for treatment initiation compared to the SAU (OR=2.15, 95% CI=.94, 4.91). With respect to covariates, those without stable housing were less likely to report marijuana use than those with stable housing at the 2- (OR=.42, 95% CI=.23, .78) and 6-month follow-ups (OR=.54, 95% CI=.31, .96), controlling for all other independent variables. People who reported using hard drugs more likely to be court mandated to treatment, compared to people who did not use hard drugs, (OR=1.91, 95% CI=1.13, 3.24), holding constant all other independent variables.
3.5. Instrumental Variables (IV) Analysis: Treatment Receipt
Table 5 shows the IV analysis for treatment effect while adjusting for the percent of participants actually receiving the treatment. At 2-months, the odds of initiating treatment for those assigned to MAPIT who completed both sessions were 65% higher than those assigned to SAU (odds ratio adjusting for treatment actually received [ORIV]=1.65, 95% CI=1.05, 2.59). The lower limit of the CI exceeds one, indicating that there was a significantly higher odds of treatment initiation in the MAPIT condition, adjusting for the treatment actually received. At 6-months, this relationship approached significance with the odds of initiating treatment in the MAPIT condition being 43% higher than the SAU (ORIV=1.43, 95% CI=0.99, 2.08).
Table 5.
Instrumental variables analyses
| Outcome | 2-Month Follow-Up
|
6-Month Follow-Up
|
||
|---|---|---|---|---|
| ORIV (95% CI) | p-value | ORIV (95% CI) | p-value | |
| Treatment initiation | ||||
| MAPIT† | 1.65 (1.05, 2.59) | 0.03 | 1.43 (0.99, 2.08) | 0.07 |
| MI | 2.29 (0.41, 12.55) | 0.34 | 1.25 (0.50, 3.13) | 0.65 |
|
| ||||
| Heavy alcohol use | ||||
| MAPIT | 1.17 (0.81, 1.70) | 0.42 | 1.00 (0.69, 1.45) | 1.00 |
| MI | 0.79 (0.38, 1.67) | 0.53 | 0.68 (0.30, 1.58) | 0.38 |
|
| ||||
| Marijuana use | ||||
| MAPIT | 1.04 (0.70, 1.54) | 0.83 | 1.30 (0.90, 1.88) | 0.17 |
| MI*† | 0.80 (0.38, 1.72) | 0.57 | 1.26 (0.49, 3.22) | 0.64 |
|
| ||||
| Hard drug use | ||||
| MAPIT** | 1.14 (0.76, 1.72) | 0.54 | 1.26 (0.87, 1.82) | 0.24 |
| MI** | 1.06 (0.42, 2.66) | 0.90 | 1.43 (0.54, 3.82) | 0.47 |
ORIV= odds ratio adjusting for treatment actually received; MAPIT=motivational computer program; MI=in-person motivational interviewing; SAU=research assessments only
Stable housing significant: 2MFU marijuana use (MI vs SAU: p=0.04)
Treatment order significant: 2MFU hard drug use (MI vs SAU: p=0.05); 6MFU hard drug use (MAPIT vs SAU: p=0.04; MI vs SAU: p=0.03)
ASI employment/education significant: 6MFU marijuana use (MI vs SAU: p=0.05); 2MFU treatment initiation (MAPIT vs SAU: p=0.04)
In the MI versus SAU models, several significant relationships were found among the covariates. The odds of reporting marijuana use at the 2-month follow-up for those without stable housing were 1.62 times as likely (ORIV =1.62, 95% CI=1.03, 2.53) compared to those with stable housing. The odds of reporting marijuana use at the 6-month follow-up for participants with more employment/education problems were about twice as likely as those without these problems (ORIV =1.95, 95% CI=1.02, 3.74). At the 2-month (ORIV =1.52, 95% CI=1.01, 2.29) and 6-month (ORIV =1.57, 95% CI=1.06, 2.32) follow-ups, the odds of reporting hard drug use for participants court-ordered to substance abuse treatment were about 52% to 57% as likely than those not court-ordered. For the MAPIT versus SAU models, those court-ordered to substance abuse treatment were 54% more likely to report hard drug use as those not court-ordered at the 6-month follow-up (ORIV =1.54, 95% CI=1.04, 2.27). Finally, those with more employment/education problems were about 50% less likely to report treatment initiation at the 2-month follow-up (ORIV =0.47, 95% CI=0.23, 0.96).
4. Discussion
MAPIT is an example of a computerized SBIRT-style intervention intended to move substance-using probationers from awareness to motivation to action. We tested this computerized intervention on a hard-to-treat population (i.e., probationers), who tend to have higher rates of substance use disorders than the general population (Feucht & Gfroerer, 2011). We found that MAPIT participants had increased rates of treatment initiation, compared to standard probation services alone, in both the ITT and IV models at 2-months, with diminished findings at 6-months. If we removed covariates related to retention and only adjusted for site, MAPIT approached significance. Contrary to some past studies (Carroll, Libby, Sheehan, & Hyland, 2001; Lundahl, Kunz, Brownell, Tollefson, & Burke, 2010), in-person MI did not improve rates of treatment initiation, compared to SAU.
SBIRT has not been widely applied in criminal justice settings, but our findings suggest that a computerized version of this model can improve treatment initiation, one important marker of probation success. In developing MAPIT, we were attempting to create an integrated health-justice framework that could address issues pertinent to both the justice and treatment service delivery systems. The motivational computer intervention, using dual processing risk messaging components, assessed readiness for success in both probation and treatment services. MAPIT presented information about both substance use and criminal justice risk, and intertwined these themes into messages that facilitated motivation to make positive changes.
The failure to directly impact substance use behaviors was disappointing, but consistent with prior SBIRT research in other settings (Saitz et al., 2010; Saitz et al., 2014). Importantly, this study was designed to compare two SBIRT models, without disrupting the existing probation system of care. This means that participants entered whatever standard intake process that was available to them at these agencies. It is possible that some participants encountered difficulties entering substance abuse treatment due to limited services or lengthy wait lists. In this study, participants were often resourceful in commencing treatment programming by using a range of faith-based services, formal treatment clinics, and medications for psychological disorders to begin the change process. Despite this resourcefulness, many participants experienced delays in commencing formal treatment even 60 to 90 days after random assignment. Keeping in mind that treatment is often a precursor to actual changes in substance use behaviors, it is possible that these barriers to obtaining treatment services contributed to our failure to find differences in substance use behaviors in our final adjusted models despite greater rates of treatment initiation.
Examination of the effect sizes revealed that MAPIT participants reported slightly more binge alcohol use at the 2-month follow-up and more marijuana use at 6-month follow-up as compared to the SAU. These effects were not found for the MI participants or for hard drug use in either intervention condition. It is possible that this finding resulted from our desire to test motivational interventions that addressed multiple risk behaviors and different types of substance use (i.e., alcohol, marijuana, hard drugs). While it makes sense to cover a broad range of behaviors, this is unique in how interventions are generally designed or implemented; most other intervention tend to focus on a narrower set of behaviors. Despite the prevalence of polysubstance use for individual involved in the criminal justice system, very few studies have developed or tested interventions that address multiple types of substances. The findings from this study findings suggest that it may be necessary to address substance use behavior differently based on the type(s) of substance(s) being used and how they affect individuals.
A somewhat surprising finding was the lack of impact for MI on treatment initiation and/or drug use outcomes. Despite a robust MI research base demonstrating small to moderate effects on substance use behaviors, research with criminal justice populations is more inconclusive (Madson, Schumacher, Baer, & Martino, 2016; Lundahl et al., 2010; McMurran, 2009). Research has begun to examine how relational (e.g., being non-judgmental, expressing empathy) and technical components (e.g., eliciting client change or sustain talk) may impact outcomes, but thusfar there is no clear picture how these may operate with justice-involved clients (Madson et al., 2016; Lundahl et al., 2010). Within our MI condition, Spohr and colleagues (2016) reported that MI spirit ratings (e.g., evocation, collaboration, autonomy support) predicted treatment initiation at the 2-month follow-up. However, other technical skills such as % open questions, % complex reflections, and the reflection-to-question ratio were unrelated to outcome. It could also be that the characteristics of our population may have played a role in our failure to find a significant effect of the MI condition. Participant characteristics such as age and ethnicity can moderate the effectiveness of MI (Madson et al., 2016; Lundahl et al., 2010), and as prior reviews have noted, getting individuals to initiate and engage in treatment is a difficult undertaking, particularly for brief interventions targeted at individuals with challenging, complex needs and certain demographic characteristics (Glass et al., 2015; Saitz et al., 2010).
The differences between the sites were not surprising. A strength of choosing these two diverse sites was the ability to generalize these findings to other probation systems (see Taxman, et al., 2015 for a description of site differences). To test the generalizability of these findings, we ran the models with site included as a covariate (not reported) and found that the effects of the interventions did not change. Future research should address how to better engage criminal justice populations, especially those with complex needs, in different geographical settings.
This study confirms the promise of a dual-processing model that integrates both substance use and criminal justice risk. Further research is needed to assess how to use integrated justice-health messages within computerized interventions, particularly to extend counselor and/or probation officer services in between formal contacts. In this study, MAPIT and MI were implemented outside of the existing probation system to ensure fidelity of the interventions being tested; however, this does limit our knowledge of what effect the probation process may have had on our outcomes. The MAPIT framework also holds promise as a way to encourage probation systems to accommodate the change process where clients are addressing chronic, relapsing behavioral health issues. Future research that incorporates MAPIT-style interventions into existing probation practices will assist in better understanding the full potential of this approach. Future tests of the interventions in this clinical trial will include treatment engagement and retention, as well as probation progress and criminal activity.
This study has a few limitations discussed elsewhere (e.g., inability to verify self-reported treatment initiation) (Taxman, et al., 2015). One additional limitation to this study is the challenge of determining the mechanism within each study arm that most impacted the outcomes. While considerable attention was given to making these interventions as comparable as possible, there were still unique, and potentially beneficial, components to each approach. For instance, MAPIT was able to send automated texts and emails to remind the participants about their goals. Those participants opting to receive these texts and emails were more likely to initiate treatment and reduce substance use at the 2-month follow-up (Spohr, Taxman, & Walters, 2015). However, the MI study arm also had unique strengths, including the counselor’s ability to develop a relationship and more readily adapt the intervention to the participant’s needs. Indeed, we found that MI fidelity predicted treatment initiation at the 2-month follow-up (Spohr, et al., 2016).
Another limitation of this study is the relatively low alcohol and drug severity scores reported for the participants using the Addiction Severity Index. Limited substance use (e.g., recreational use) may negate the participants’ perceived need for abstinence or treatment, thus reducing the ability to detect treatment initiation behavior. However, the restrictions placed on individuals regarding substance use while on community supervision set a very low threshold of use (i.e., most require abstinence) for which the probationer may be sent to treatment or further disciplined. Our inclusion of both formal and informal treatment modalities in our measurement may offset some of this limitation, but future research should consider the severity of substance use behaviors when determining eligibility criteria. Additionally, the inclusion of post-hoc prognostic covariates in the models may increase the possibility of Type 1 error (Kahan, Jairath, Dore, & Morris, 2014). Despite these limitations, the outcomes of this study contribute greatly to understanding the potential benefit of a computerized intervention when it is compared to a counselor-driven approach.
5. Conclusions
MAPIT confirms that a motivational computer program can improve short-term treatment initiation among substance-using probationers. The start of probation is a critical time to educate and motivate clients, and to provide a platform for developing goals that will help address substance use and other risk behaviors. Our study demonstrated that this can be accomplished without additional burdens on the criminal justice system, such as hiring or training staff. Overall, our findings suggest that a computerized intervention can help address public safety and health issues among this high-risk group.
Highlights.
Motivational computer intervention (MAPIT) increased treatment initiation at 2-month follow-up.
The significance of MAPIT diminished by the 6-month follow-up.
Motivational interviewing (MI) was not significant in any model.
No differential impact on substance use.
Acknowledgments
We are grateful to the Dallas County Community Supervision and Corrections Department and the Maryland Department of Public Safety and Correctional Servcies for their assistance in conducting this study. This work was supported by the National Institute on Drug Abuse (R01 DA029010). The trial registration number is NCT01891656 (initiated on October 18, 2011).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: The authors declare that they have no competing interests.
Authors’ Contributions: All authors contributed to writing and revising this article, as well as reading and approving the final content. STW and FST are the principal investigators on this project and led the team in carrying out all aspects of the study. JL served as project manager and statistician for this project. LT contributed to statistical analyses for this project.
Note: The opinions expressed in this paper are those of the authors and do not represent any government agency.
References
- Bandura A. Social Foundations of thought and action: a social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- Bonta J, Bourgon G, Rugge T, Scott TL, Yessine AK, Gutierrez L, Li J. An experimental demonstration of training probation officers in evidence-based community supervision. Criminal Justice Behavior. 2011;38:1127–1148. [Google Scholar]
- Burgess S, Small DS, Thompson SG. A review of instrumental variable estimators for Mendelian randomization. Statistical Methods in Medical Research. 2015;0(0):1–26. doi: 10.1177/0962280215597579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Libby B, Sheehan J, Hyland N. Motivational Interviewing to Enhance Treatment Initiation in Substance Abusers: An Effectiveness Study. The American Journal on Addictions. 2001;10(4):335–339. doi: 10.1080/aja.10.4.335.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. Key Substance Use and Mental Health Indicators in the United States: Results from the 2015 National Survey on Drug Use and Health. Rockville, MD: Substance Abuse and Mental Health Services Administration US Dept. of Health and Human Services; 2016. [Google Scholar]
- Chadwick N, Dawolf A, Serin R. Effectively training community supervision officers: a meta-analytic review of the impact on offender outcome. Criminal Justice Behavior. 2015;42:977–989. [Google Scholar]
- Chaple M, Sacks S, McKendrick K, Marsch LA, Belenko S, Leukefeld C, Prendergast M, French M. Feasibility of a computerized intervention for offenders with substance use disorders: a research note. Journal of Experimental Criminology. 2014;10(1):105–127. doi: 10.1007/s11292-013-9187-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke PS, Windmeijer F. Instrumental variable estimators for binary outcomes. Journal of the American Statistical Association. 2012;107(500):1638–52. [Google Scholar]
- De Leon G. Commentary on “Self-help organizations for alcohol and drug problems: Toward evidence-based practice and policy”. Journal of Substance Abuse Treatment. 2004;26:163–165. doi: 10.1016/S0740-5472(03)00212-5. [DOI] [PubMed] [Google Scholar]
- Feucht TE, Gfroerer J. Data review: mental and substance use disorders among adult men on probation or parole: some success against a persistent challenge. Rockville, MD: Substance Abuse and Mental Health Services Administration US Dept of Health and Human Services; 2011. [Google Scholar]
- Garnick DW, Lee T, Horgan CM, Acevedo MS, the Washington Circle Public Sector Workgroup Adapting Washington Circle Performance Measures for Public Sector Substance Abuse Treatment Systems. Journal of Substance Abuse Treatment. 2009;36(3):265–277. doi: 10.1016/j.jsat.2008.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass JE, Hamilton AM, Powell BJ, Perron BE, Brown RT, Ilgen MA. Specialty substance use disorder services following brief alcohol intervention: a meta-analysis of randomized controlled trials. Addiction. 2015;110:1404–1415. doi: 10.1111/add.12950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gossop M, Stewart D, Marsden J. Attendance at Narcotics Anonymous and Alcoholics Anonymous meetings, frequency of attendance and substance use outcomes after residential treatment for drug dependence: a 5-year follow-up study. Addiction. 2015;103:119–125. doi: 10.1111/j.1360-0443.2007.02050.x. [DOI] [PubMed] [Google Scholar]
- Green CA, Polen MR, Dickinson DM, Lynch FL, Bennett MD. Gender differences in predictors of initiation, retention, and completion of an HMO-based substance abuse treatment program. Journal of Substance Abuse Treatment. 2002;23:285–295. doi: 10.1016/s0740-5472(02)00278-7. [DOI] [PubMed] [Google Scholar]
- Hall K, Staiger PK, Simpson A, Best D, Lubman DI. After 30 years of dissemination, have we achieved sustained practice change in motivational interviewing? Addiction. 2016;111:1144–1150. doi: 10.1111/add.13014. [DOI] [PubMed] [Google Scholar]
- Hettema J, Steele J, Miller WR. Motivational interviewing. Annual Review of Clinical Psychology. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- Hingson R, Compton WM. Screening and brief intervention and referral to treatment for drug use in primary care: back to the drawing board. Journal of the American Medical Association. 2014;312(5):488–489. doi: 10.1001/jama.2014.7863. [DOI] [PubMed] [Google Scholar]
- Humeniuk RE, Henry-Edwards S, Ali RL, Poznyak V, Monteiro M. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): manual for use in primary care. Geneva: World Health Organization; 2010. [Google Scholar]
- Humphreys K, Wing S, McCarty D, Chappel J, Gallant L, Haberle B, Weiss R. Self-help organizations for alcohol and drug problems: Toward evidence-based practice and policy. Journal of Substance Abuse Treatment. 2004;26:151–158. doi: 10.1016/S0740-5472(03)00212-5. [DOI] [PubMed] [Google Scholar]
- Institute of Behavioral Research, Texas Christian University. CJ Client Evaluation of Self and Treatment Intake Version. 2005 http://www.ibr.tcu.edu/pubs/datacoll/cjtrt.html.
- Kaeble D, Maruschak LM, Bonczar TP. Probation and parole in the United States, 2014. Washington, DC: Bureau of Justice Statistics US Dept of Justice; 2015. [Google Scholar]
- Kahan BC, Jairath V, Dore CJ, Morris TP. The risks and rewards of covariate adjustment in randomized trials: an assessment of 12 outcomes from 8 studies. Trials. 2014;15(139):1–7. doi: 10.1186/1745-6215-15-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karberg JC, James DJ. Substance dependence, abuse and treatment of jail inmates, 2002. Washington, DC: Bureau of Justice Statistics US Department of Justice; 2005. [Google Scholar]
- Laudet AB, Savage R, Mahmood D. Pathways to Long-Term Recovery: A Preliminary Investigation. Journal of Psychoactive Drugs. 2002;34(3):305–311. doi: 10.1080/02791072.2002.10399968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundahl BW, Kunz C, Brownell C, Tollefson D, Burke BL. A meta-analysis of motivational interviewing: Twenty-five years of empirical studies. Research on Social Work Practice. 2010;20(2):137–160. [Google Scholar]
- Madson MB, Schumacher JA, Baer JS, Martino S. Motivational Interviewing for Substance Use: Mapping Out the Next Generation of Research. Journal of Substance Abuse Treatment. 2016;65:1–5. doi: 10.1016/j.jsat.2016.02.003. [DOI] [PubMed] [Google Scholar]
- Lipsey MW, Wilson DB. Practical meta-analysis. Vol. 49. Thousand Oaks, CA: Sage publications; 2001. [Google Scholar]
- Marsch LA, Carroll KM, Kiluk BD. Technology-based interventions for the treatment and recovery management of substance use disorders: a JSAT special issue. Journal of Substance Abuse Treatment. 2014;46(1):1–4. doi: 10.1016/j.jsat.2013.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Alternman AI, Metzger DS, Grissom GR, Woody GE, Luborsky L, O’Brien CP. Similarity of Outcome Predictors Across Opiate, Cocaine, and Alcohol Treatments: Role of Treatment Services. Journal of Consulting and Clinical Psychology. 1994;62(6):1141–1158. doi: 10.1037//0022-006x.62.6.1141. [DOI] [PubMed] [Google Scholar]
- McGahan PL, Griffith JA, Parente R, McLellan AT. Addiction Severity Index: Composite Scores Manual. Philadelphia, PA: The University of Pennsylvania/Veterans Administration Center for Studies of Addiction; 1986. [Google Scholar]
- McMurran M. Motivational interviewing with offenders: a systematic review. Legal and Criminological Psychology. 2009;14:83–100. [Google Scholar]
- Moyer VA. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: U.S. preventive services task force recommendation statement. Annals of Internal Medicine. 2013;159:210–218. doi: 10.7326/0003-4819-159-3-201308060-00652. [DOI] [PubMed] [Google Scholar]
- Phelps MS. The Paradox of Probation: Community Supervision in the Age of Mass Incarceration. Law & policy. 2013;35(1–2):51–80. doi: 10.1111/lapo.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Project MATCH Research Group. Project MATCH (matching alcoholism treatment to client heterogeneity): rationale and methods for a multisite clinical trial matching patients to alcoholism treatment. Alcoholism: Clinical and Experimental Research. 1993;17(6):1130–45. doi: 10.1111/j.1530-0277.1993.tb05219.x. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne P, Bumgardner K, Krupski A, Dunn C, Ries R, Donovan D, Zarkin GA. Brief intervention for problem drug use in safety-net primary care settings: a randomized clinical trial. Journal of the American Medical Association. 2014;312(5):492–501. doi: 10.1001/jama.2014.7860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saitz R, Alford DP, Bernstein J, Cheng DM, Samet J, Palfai T. Screening and Brief Intervention for Unhealthy Drug Use in Primary Care Settings: Randomized Clinical Trials Are Needed. Journal of Addiction Medicine. 2010;4(3):123–130. doi: 10.1097/ADM.0b013e3181db6b67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saitz R, Palfai TPA, Cheng DM, Alford DP, Bernstein JA, Lloyd-Travaglini CA, Meli SM, Chaisson CE, Samet JH. Screening and Brief Intervention for Drug Use in Primary Care: The ASPIRE Randomized Clinical Trial. The Journal of the American Medical Association. 2014;312(5):502–513. doi: 10.1001/jama.2014.7862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saitz R. Screening and brief intervention for unhealthy drug use: little or no efficacy. Frontiers in Psychiatry. 2014;5:1–5. doi: 10.3389/fpsyt.2014.00121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline Followback user’s guide: A calendar method for assessing alcohol and drug use. Toronto, Ontario, Canada: Addiction Research Foundation; 1996. [Google Scholar]
- Spohr SA, Taxman FS, Rodriguez M, Walters ST. Motivational interviewing fidelity in a community corrections setting: Treatment initation and subsequent drug use. Journal of Substance Abuse Treatment. 2016;65:20–25. doi: 10.1016/j.jsat.2015.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spohr SA, Taxman FS, Walters ST. The relationship between electronic goal reminders and drug use and treatment initiation outcomes in a criminal justice setting. Addictive Behaviors. 2015;51:51–56. doi: 10.1016/j.addbeh.2015.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sussman JB, Hayward RA. An IV for the RCT: Using instrumental variables to adjust for treatment contamination in randomized controlled trials. British Medical Journal. 2010;340:c2073. doi: 10.1136/bmj.c2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taxman FS, Perdoni ML, Caudy M. The plight of providing appropriate substance abuse treatment services to offenders: Modeling the gaps in service delivery. Victim Offender. 2013;8(1):70–93. [Google Scholar]
- Taxman FS, Perdoni ML, Harrison LD. Drug treatment services for adult offenders: The state of the state. Journal of Substance Abuse Treatment. 2007;32(3):239–254. doi: 10.1016/j.jsat.2006.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taxman FS, Walters ST, Sloas LB, Lerch J, Rodriguez M. Motivational tools to improve probationer treatment outcomes. Contemporary Clinical Trials. 2015;43:120–128. doi: 10.1016/j.cct.2015.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terza JV, Basu A, Rathouz PJ. Two-stage residual inclusion estimation: Addressing endogeneity in health econometric modeling. Journal of Health Economics. 2008;27(3):531–543. doi: 10.1016/j.jhealeco.2007.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The White House, Office of the Press Secretary. Obama Administration Officials Announces $22 Million Expansion of Innovative Health Program Aimed at Detecting and Intervening in Drug Addiction Early [Press release] 2012 Retrieved from https://obamawhitehouse.archives.gov/ondcp/news-releases-remarks/22-million-dollar-grant-medicalizing-drug-prevention.
- U.S. Department of Health and Human Services (HHS), Office of the Surgeon General. Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health. Washington, DC: HHS; 2016. [PubMed] [Google Scholar]
- Walters ST, Ondersma SJ, Ingersoll KS, Rodriguez M, Lerch J, Rossheim ME, Taxman FS. MAPIT: Development of a web-based intervention targeting substance abuse treatment in the criminal justice system. Journal of Substance Abuse Treatment. 2014;46:60–65. doi: 10.1016/j.jsat.2013.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters ST, Ressler E, Douglas L, Taxman FS. Motivational interviewing in criminal justice: A new approach to addressing treatment motivation and related behaviors. Counselor: The Magazine for Addictions Professionals 2011 [Google Scholar]
- Witte K, Allen MA. Meta-analysis of fear appeals: implications for effective public health campaigns. Health Education & Behavior. 2000;27(5):591–615. doi: 10.1177/109019810002700506. [DOI] [PubMed] [Google Scholar]


