Abstract
Background:
Patients with end-stage renal disease (ESRD) frequently have a relatively poor prognosis with complex care needs that depend on prognosis. While many means of assessing prognosis are available, little is known about how Canadian nephrologists predict prognosis, whether they routinely share prognostic information with their patients, and how this information guides management.
Objective:
To guide improvements in the management of patients with ESRD, we aimed to better understand how Canadian nephrologists consider prognosis during routine care.
Design and methods:
A web-based multiple choice survey was designed, and administered to adult nephrologists in Canada through the e-mail list of the Canadian Society of Nephrology. The survey asked the respondents about their routine practice of estimating survival and the perceived importance of prognostic practices and tools in patients with ESRD. Descriptive statistics were used in analyzing the responses.
Results:
Less than half of the respondents indicated they always or often make an explicit attempt to estimate and/or discuss survival with ESRD patients not on dialysis, and 25% reported they do so always or often with patients on dialysis. Survival estimation is most frequently based on clinical gestalt. Respondents endorse a wide range of issues that may be influenced by prognosis, including advance care planning, transplant referral, choice of dialysis access, medication management, and consideration of conservative care.
Limitations:
This is a Canadian sample of self-reported behavior, which was not validated, and may be less generalizable to non-Canadian health care jurisdictions.
Conclusions:
In conclusion, prognostication of patients with ESRD is an important issue for nephrologists and impacts management in fairly sophisticated ways. Information sharing on prognosis may be suboptimal.
Keywords: end-stage renal disease, chronic kidney disease, prognostication, dialysis, conservative care
Abrégé
Contexte:
En règle générale, le pronostic des patients atteints d’insuffisance rénale terminale (IRT) est plutôt sombre et implique des besoins complexes en matière de soins. Bien qu’il existe diverses approches, on en sait peu sur la façon dont les néphrologues canadiens s’y prennent réellement pour établir le pronostic de leurs patients, et on ignore, premièrement, si l’information pronostique est systématiquement communiquée au patient et deuxièmement, comment cette information oriente la prise en charge du patient.
Objectifs de l’étude:
Nous avons voulu mieux comprendre la manière dont les néphrologues canadiens tiennent compte du pronostic dans les soins aux patients afin d’éclairer les avancées dans la prise en charge des patients atteints d’IRT.
Conception de l’étude et méthodologie:
On a envoyé par courriel, un sondage Web à choix multiples à des néphrologues canadiens figurant sur la liste d’envoi de la Société canadienne de néphrologie. Le sondage interrogeait les répondants sur leur pratique habituelle d’évaluation de la durée de survie et sur leur perception de l’importance des outils et des pratiques pronostiques chez les patients atteints d’IRT. On a effectué une analyse statistique descriptive des réponses reçues.
Résultats:
Moins de la moitié des répondants a indiqué faire systématiquement ou souvent une tentative claire d’estimer la durée de survie ou d’en discuter avec le patient atteints d’IRT non dialysé, alors que seulement 25% le font dans le cas d’un patients dialysé. L’estimation de la durée de survie est le plus fréquemment basée sur une gestalt clinique. Les répondants rapportent un large éventail de questions pouvant être influencé par le pronostic, notamment la planification préalable des soins, la consultation en vue d’une transplantation, le choix de l’accès pour la dialyse, la gestion de la médication et la prise en considération d’un traitement conservateur.
Limites de l’étude:
Il s’agit d’un échantillon canadien non validé dont le comportement est autodéclaré et par conséquent, il pourrait ne pas correspondre à des systèmes de soins de santé à l’extérieur du Canada.
Conclusions:
L’établissement d’un pronostic chez les patients atteints d’IRT est un enjeu majeur dans la pratique des néphrologues canadiens et entraîne des répercussions relativement pointues sur la prise en charge du patient. La transmission de renseignements pronostiques pourrait ne pas être optimale.
What was known before
Patients with end-stage renal disease (ESRD) frequently have a poor prognosis, with a complex set of care needs that depend on prognosis. While there are tools to assess prognosis, little is known about whether Canadian nephrologists estimate the life span of these patients, whether the information is regularly shared with patients in clinical practice, and how it will be used to guide clinical management.
What this adds
This pan-Canadian survey of nephrologists describes the diversity in practice of communicating and using prognostic information in the clinical care of kidney patients on and off dialysis. There may be a need to improve communications with patients to enable shared decision-making, and to improve on prognostic tools that will aid individual discussions and clinical management.
Introduction
End-stage renal disease (ESRD) is an important health condition associated with high morbidity and mortality.1,2 In Canada, well over 5000 patients have initiated dialysis annually and 28% of those individuals are aged >75 years over the past decade.3 However, only 27% of patients in this age group are alive 5 years after initiating dialysis, which reflects a survivorship comparable to amyotrophic lateral sclerosis,4 and stage III colon cancer.5
The relatively poor survival in this age bracket highlights the need for having conversations around goals of treatment in advance. Relatively little is known about prognosis conversations between nephrologists and patients with ESRD, including what patients want to know about prognosis. A small number of studies have reported that Canadians,6 including those living with ESRD7,8 want to receive honest prognostic information from their doctor even if the prognosis is poor. A systematic review on communicating prognosis in cancer care found that the majority of patients wanted to know their prognosis, and many wanted to be asked about their preferences for receiving prognostic information.9 The frequency of these conversations is not well reported, however, and is perceived to be inadequate.7,8,10 Reviews have proposed broad elements of good end-of-life care that include advance care planning, symptom-based medication prescribing, consideration of nondialytic management of ESRD,11 which are closely related to and dependent on the prognosis of individual patients.
Optimal care for patients on dialysis depends on accurate prognostication. Patients with a poor expected survival or frail state are expected to benefit more from a palliative approach11 and may even be harmed by intensive medical and surgical procedures associated with renal replacement therapy.12,13 However, predicting prognosis is a complex activity. While some prognostic models focus exclusively on the use of clinical prognostic markers,14-16 more emerging models include a mix of clinical variables as well as variables related to lifestyle habit, functional status, and other nonclinical variables.17-22 Despite a growing body of literature on prognosis in ESRD, little is known about how often nephrologists explicitly prognosticate for their patients with ESRD, how they do this, and what they do with the prognostic information to guide the clinical management of their patients.
In this study, we aimed to explore practice among Canadian nephrologists regarding estimation of prognosis and the use of prognostic information for the clinical management of adult patients with ESRD. A secondary objective was to assess face validity of a possible set of variables that may be used in prognosticating in patients with ESRD.
Methods
A web-based survey was designed by a panel with nephrologists, methodologists, researchers, and administrators with expertise in risk prediction modeling and knowledge translation. The survey was pilot-tested with nephrologists in British Columbia, Canada, to ensure clarity of the questions and ease of completion. The final survey (Supplemental material) with minor modifications was administered to nephrologists in Canada via the e-mail list of the Canadian Society of Nephrology (CSN) over a 2-month period from February to April 2015. Two e-mail reminders were sent within the time period. All survey responses were anonymous.
Questionnaire Content
We asked the respondents to provide general demographic information: age group, years of practice in nephrology, overall patient load per week, and an estimated number of conservatively managed patients in the last 6 months. A 20-item version of the questionnaire was administered to all nephrologist respondents. The survey was divided into 3 sections: (1) demographic information of our respondents; (2) questions pertaining to prognostication practice and utility for patients with glomerular filtration rate (GFR) <15 mL/min not on dialysis; and (3) questions pertaining to prognostication practice and utility for patients on dialysis. Free text was enabled for the “other” options in some items. The majority of the questions are in multiple choice except for the item, “Rank the importance of the following factors that you would generally consider when recommending to your patients conservative care versus dialysis,” in which the respondents were asked to arrange the list of factors in order of importance.
Analysis
Survey data downloaded from the online host were analyzed in Microsoft Excel (version 2013; Microsoft Corporation, Redmond, Washington). Although the survey was sent to adult and pediatric nephrologists, we asked that only adult nephrologists respond to the survey. Nevertheless, we conservatively calculated the response rate as defined by the number of respondents to the total number of both adult and pediatric nephrologists included on the mailing list. Completion rate was the proportion of those who have completed the entire survey to total number of respondents. For the item, “Rank the importance of the following factors that you would generally consider when recommending to your patients conservative care versus dialysis,” the ranking of factors was based on weighted average score of the responses on individual factors listed. For the remainder of the survey, descriptive statistics were used to summarize individual responses for each item. The result of each item was summarized in percentages of responses for each choice to the total number of responses for the item and presented in bar charts or written in text.
Results
Of the 259 nephrologists contacted, 111 persons replied; the response rate was 43%. Eighty-one percent of the respondents completed the entire survey.
Characteristics of Respondents
Table 1 shows the demographic of responding nephrologists in terms of age, practice experience, and patient load. Respondents had been in practice for <5 years (19%), 5-10 years (24%), 11-15 years (23%), and >15 years (33%). The median patient volume per week was 40 to 69 patients per week, and the median number of conservatively managed patients cared for in the last 6 months was 5 to 10 patients.
Table 1.
Characteristics of Nephrologist Respondents (N = 111).
| Characteristics | % |
|---|---|
| Age | |
| ≤35 | 10 |
| 36-45 | 47 |
| 46-55 | 18 |
| 56-65 | 17 |
| 65+ | 8 |
| Years in practice | |
| <5 | 19 |
| 5-10 | 24 |
| 11-15 | 23 |
| >15 | 33 |
| Patient volume per week | |
| <10 | 1 |
| 10-39 | 29 |
| 40-69 | 36 |
| 70-89 | 16 |
| ≥90 | 18 |
| Number of conservatively managed patients managed in the last 6 months | |
| <5 | 25 |
| 5-10 | 33 |
| 11-15 | 13 |
| 16-20 | 8 |
| >20 | 21 |
Prognostication in Patients With Nondialysis ESRD
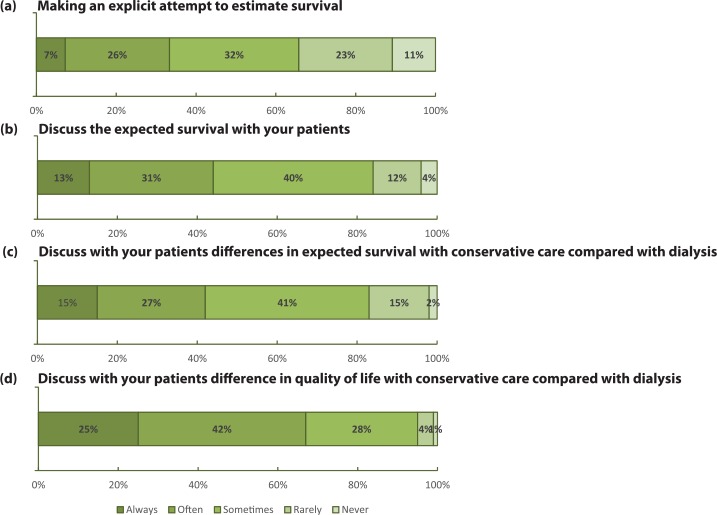
Among the respondents, 33% indicated that they either often or always explicitly attempt to estimate survival of their patients with chronic kidney disease (CKD) and GFR <15 mL/min who are not on dialysis (Figure 1a). Most respondents (57%) would generally estimate and compare survival with and without dialysis. Less than half of the respondents would always or often discuss the survival (44%; Figure 1b) and the differences in expected survival with conservative care compared with dialysis (42%; Figure 1c) with their patients who are not on dialysis but have low kidney function. Conversely, the majority of respondents (67%) indicated that they always or often discuss with these patients differences in quality of life with conservative care versus dialysis. When considering expected survival thresholds for recommending conservative care over dialysis, a number of life expectancy thresholds were provided (<3, <6, <9, <12 months). More than half of respondents (54%) reported that they do not consider a specific life expectancy threshold. The most important factors impacting a recommendation for conservative care versus dialysis were the patient’s stated quality of life, the severity of comorbidities, and the patient’s values and beliefs (Table 2). Two of the respondents noted in “other, please specify” that ranking is difficult as it involves discerning among competing or equally important choices.
Figure 1.
Prognostication in patients with ESRD not on dialysis.
Table 2.
Factors that Nephrologists Would Generally Consider When Recommending Conservative Care vs Dialysis.
| Most important |
|---|
| Patient’s stated quality of life |
| Severity of comorbidities |
| Patient’s values and believes |
| Expected survival |
| Functional status |
| Symptom burden |
| Specific diagnoses |
| Life circumstances/logistics |
| Patient’s age |
| Least important |
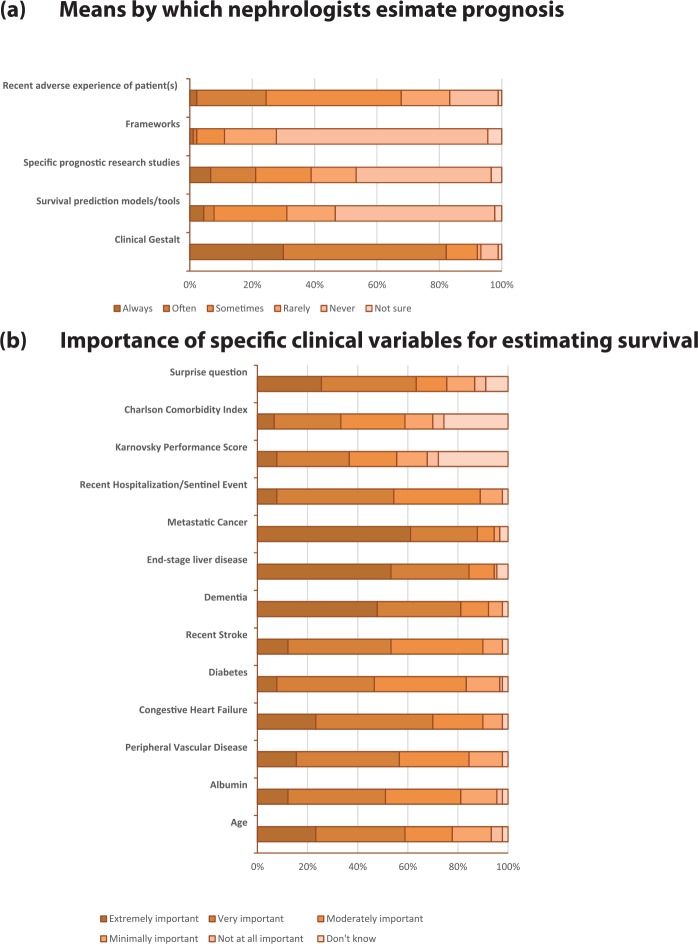
The most common means by which survival was estimated was clinical gestalt (>80% for always or often; Figure 2a). About half of the respondents deemed a validated prognostic tool for guiding clinical management decisions in their patients with ESRD extremely or very important. As shown in Figure 2b, the respondents indicated a wide range of management decisions that the tool could support, particularly to enable shared decision-making and guide advance care planning discussions with their patients. Nephrologist perception of the value of clinical predictor variables reported in the literature is presented in Figure 2c. The variables perceived to have the greatest importance for estimating survival in patients with ESRD but not on dialysis included a diagnosis of metastatic cancer, end-stage liver disease, and dementia.
Figure 2.
Prognostic utility and parameters of prognostication in patients with ESRD not on dialysis.
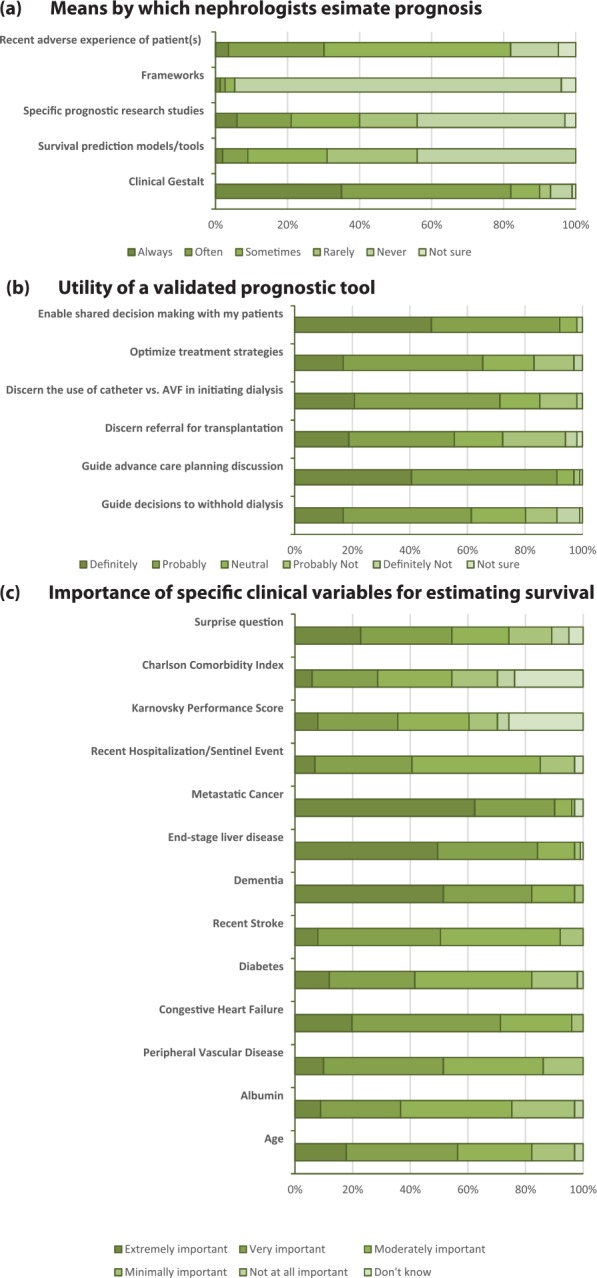
Prognostication in Patients on Dialysis
When asking nephrologists about prognostication in patients on dialysis, 25% of respondent indicated they always or often make explicit attempts to estimate survival (Figure 3a). Nineteen percent of nephrologists indicated they always or often discuss prognosis with their patients (Figure 3b).
Figure 3.
Prognostication in patients on dialysis.
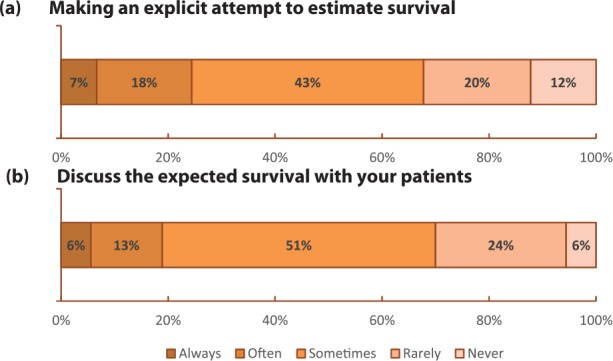
Clinical gestalt remained the most common means by which survival was estimated (>80%; Figure 4a). Approximately 70% of respondents indicated they never or rarely use clinical prediction tools. About three-quarters of respondents indicated they definitely or probably would use a prognostic tool validated in a Canadian population that estimates survival for patients on dialysis. As illustrated in Figure 4b, the variables perceived to have the greatest importance for estimating survival in patients on dialysis included a diagnosis of metastatic cancer, end-stage liver disease, and dementia.
Figure 4.
Prognostic utility and parameters of prognostication in patients on dialysis.
Discussion
This study explores how Canadian nephrologists address the issue of survival estimation and sharing that information in routine management of adult patients with ESRD. While many nephrologists indicated that they would generally estimate and compare survival of patients with and without dialysis, only a minority of them reported that they explicitly attempt to estimate prognosis, and overtly discuss these assessments with their patients, either on or off dialysis. This finding might indicate suboptimal information sharing given the advanced age group of many patients initiating dialysis, who are known to have a relatively poor long-term survivorship. Alternately, this finding could be consistent with appropriate information sharing taking into account what individual nephrologists may know about preferences of their patients, as well as the relatively good prognosis of many patients with ESRD. Acknowledging the information gap in this area, the available published literature supports that most patients deem prognosis an important aspect of informed decision-making.6-9 The survey by Davison8 reported that 61% of the patient respondents regretted their decision to start dialysis. The phenomenon of patients on dialysis questioning their initial decision to receive dialysis later on in their journey was also a finding in a recent systematic review.23 The issues here are complex, but these findings suggest the importance of optimal information sharing to support optimal decision-making.
Among our respondents, clinical gestalt was by far the most prevalent means by which prognosis is estimated in patients with advanced CKD, both on and off dialysis. Use of clinical prediction tools was far less common. It may be that a prediction tool with adequate clinical utility that is validated for a Canadian population is perceived to be lacking, or that other factors explain this. The survey identified a wide variety of clinical issues that nephrologists reported are impacted by prognosis in patients with advanced CKD not yet on dialysis. Respondents suggested that patient’s stated quality of life was the most important factor to be considered when recommending conservative care versus dialysis. This accords with findings by Carson et al24 which showed that extended survival on dialysis was accompanied by extended time spent hospitalized in elderly patients. Ongoing large-scale patient-centered initiatives (ie, SONG,25 Can-SOLVE CKD26) are addressing this complex issue of survival time as compared with quality of life in patients with advanced CKD.
This study highlights an important role for validated prognostic tools for guiding clinical management decisions in patients with advanced CKD. Many prediction tools have been developed for this purpose and reported reasonable discrimination (area under the curve [AUC] range 0.68 to 0.87 across these studies).14,17,18,20,22,27-31 We are not aware of any studies that externally validate the predictive performance and clinical utility32,33 of any of these models, which could explain the finding that the majority of respondents indicated they never or rarely use prediction tools. From these studies, we selected for this survey the majority of the predictor variables contained in the final models. This predictor variable selection was not exhaustive, and did not include similar variables that we judged were already present in our selection, were not as well studied, or were not as consistently shown to be predictive. To our knowledge, there is no prognostic model for predicting mortality in patients on dialysis that includes all top 3 variables (metastatic cancer, end-stage liver disease, and dementia) as identified by the respondents.
The shared decision to proceed with conservative management and withdrawal from dialysis is complex, and not simply limited to survival. A systematic review of qualitative studies addressing this noted clinicians focused on “biomedical factors.”23 Furthermore, their judgment was when treatment was “prolonging the process of dying rather than adding quality days to a patient’s life.”23 Conversely, patients reflected on quality of life with dialysis and “gut instinct.”23 A recent review argues that patient informed decisions need to include prognostic factors in prediction tools beyond survival.34 Indeed, our respondents identified that quality of life is the most important factor, ahead of survival, for recommending conservative care over dialysis.
Strengths of this survey include a reasonable response rate for an online survey, a geographically broad sampling across Canada and a diversity of practice duration. This survey provided a broad documentation of attitudes and methods used for prognostication at the current time in Canada. Potential sources of bias may include our convenience sampling strategy and response rate. It is difficult to know the characteristics and attitudes of nonresponders, whose practices could differ systematically. However, the age distribution of our respondents accords with the age distribution of nephrologists in the most recent workforce survey done for the Canadian Medical Association, which estimated 680 nephrologists in Canada (both adult and pediatric nephrologists).35 A response rate of 43% is relatively favorable and comparable to other similar published surveys.36-40 It is also unreliable to judge the quality of the survey data solely by its response rate.41,42 In addition, given the complex and potentially sensitive nature of end-of-life care, nephrologist self-report responses may introduce a degree of bias toward greater attention to these end-of-life care matters than what actually transpires in practice. Thus, this survey may be biased conservatively, and represent a “better” than “actual” snapshot of current practices in the area of prognosis discussions. An observational study of actual practices, and documentation, may be useful to corroborate the self-reported practices here. Our study also focused on survival estimate and did not assess prediction and information sharing on other factors such as quality of life or symptom burden, which informs optimal information sharing.
In conclusion, this study described that prognosis is perceived by Canadian nephrologists as an important issue that impacts the clinical management of patients with ESRD, irrespective of whether or not they are on dialysis. A mortality prediction tool validated in a Canadian population may impact several aspects of clinical management, identifying a need for further work in this area. Our findings indicate prioritization of quality of life which could be a prediction outcome for future study. Our findings suggest frequent yet potentially suboptimal sharing of prognostic information with patients during routine practice. This requires further investigation to support optimum communication with our patients with kidney disease.
Acknowledgments
We appreciate the time and efforts from all nephrologists who participated in the study. Moreover, we thank all participants in British Columbia for the pilot test of the survey and Alexandra Romanns for her assistance with the analysis of the pilot results. Many thanks to the staff at the Canadian Society of Nephrology for the distribution of the online survey and reminders through their distribution list. Finally, we are grateful to Dr Adeera Levin for her advice on the development of this work and the preparation of this report.
Footnotes
Ethics Approval and Consent to Participate: The study was approved by the Research Ethics Board of the Providence Health Care Research Ethics Board.
Consent for Publication: All authors consent to the publication of this study.
Availability of Data and Materials: The raw data of this study is not publicly available.
Author Contributions: All authors contributed to the design and development of the survey and interpretation of the survey results. H.H.L.C. analyzed the results. B.F. drafted the manuscript. B.F. and H.H.L.C. critically revised the manuscript. All authors read and approved the final manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received financial support for the research, authorship, and/or publication of this article: The research and publication of this article are sponsored by the BC Provincial Renal Agency.
References
- 1. Davison SN, Jhangri GS. Impact of pain and symptom burden on the health-related quality of life of hemodialysis patients. J Pain Symptom Manage. 2010;39(3):477-485. [DOI] [PubMed] [Google Scholar]
- 2. Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351(13):1296-1305. [DOI] [PubMed] [Google Scholar]
- 3. Canadian Organ Replacement Register (CORR), Canadian Institute for Health Information. 2015 CORR annual report: treatment of end-stage organ failure in Canada, 2004-2013.
- 4. Elamin M, Bede P, Montuschi A, Pender N, Chio A, Hardiman O. Predicting prognosis in amyotrophic lateral sclerosis: a simple algorithm. J Neurol. 2015;262(6):1447-1454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. The American Joint Committee on Cancer. AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer; 2010. [Google Scholar]
- 6. You JJ, Dodek P, Lamontagne F, et al. What really matters in end-of-life discussions? Perspectives of patients in hospital with serious illness and their families. Can Med Assoc J. 2014;186(18):E679-E687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fine A, Fontaine B, Kraushar MM, Rich BR. Nephrologists should voluntarily divulge survival data to potential dialysis patients: a questionnaire study. Perit Dial Int. 2005;25(3):269-273. [PubMed] [Google Scholar]
- 8. Davison SN. End-of-life care preferences and needs: perceptions of patients with chronic kidney disease. Clin J Am Soc Nephrol. 2010;5(2):195-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hagerty RG, Butow PN, Ellis PM, Dimitry S, Tattersall MH. Communicating prognosis in cancer care: a systematic review of the literature. Ann Oncol. 2005;16(7):1005-1053. [DOI] [PubMed] [Google Scholar]
- 10. Eneanya ND, Goff SL, Martinez T, et al. Shared decision-making in end-stage renal disease: a protocol for a multi-center study of a communication intervention to improve end-of-life care for dialysis patients. BMC Palliat Care. 2015;14:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Davison R, Sheerin NS. Prognosis and management of chronic kidney disease (CKD) at the end of life. Postgrad Med J. 2014;90(1060):98-105. [DOI] [PubMed] [Google Scholar]
- 12. O’Hare AM, Bertenthal D, Walter LC, et al. When to refer patients with chronic kidney disease for vascular access surgery: should age be a consideration? Kidney Int. 2007;71(6):555-561. [DOI] [PubMed] [Google Scholar]
- 13. Kurella Tamura M, Covinsky KE, Chertow GM, Yaffe K, Landefeld CS, McCulloch CE. Functional status of elderly adults before and after initiation of dialysis. N Engl J Med. 2009;361(16):1539-1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Couchoud C, Labeeuw M, Moranne O, et al. A clinical score to predict 6-month prognosis in elderly patients starting dialysis for end-stage renal disease. Nephrol Dial Transplant. 2009;24(5):1553-1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Liu J, Huang Z, Gilbertson DT, Foley RN, Collins AJ. An improved comorbidity index for outcome analyses among dialysis patients. Kidney Int. 2010;77(2):141-151. [DOI] [PubMed] [Google Scholar]
- 16. Chua HR, Lau T, Luo N, et al. Predicting first-year mortality in incident dialysis patients with end-stage renal disease—the UREA5 study. Blood Purif. 2014;37(2):85-92. [DOI] [PubMed] [Google Scholar]
- 17. Cohen LM, Ruthazer R, Moss AH, Germain MJ. Predicting six-month mortality for patients who are on maintenance hemodialysis. Clin J Am Soc Nephrol. 2010;5(1):72-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wagner M, Ansell D, Kent DM, et al. Predicting mortality in incident dialysis patients: an analysis of the United Kingdom Renal Registry. Am J Kidney Dis. 2011;57(6):894-902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Weiss JW, Platt RW, Thorp ML, et al. Predicting mortality in older adults with kidney disease: a pragmatic prediction model. J Am Geriatr Soc. 2015;63(3):508-515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Floege J, Gillespie IA, Kronenberg F, et al. Development and validation of a predictive mortality risk score from a European hemodialysis cohort. Kidney Int. 2015;87(5):996-1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. van Diepen M, Schroijen MA, Dekkers OM, et al. Predicting mortality in patients with diabetes starting dialysis. PLoS ONE. 2014;9(3):e89744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Thamer M, Kaufman JS, Zhang Y, Zhang Q, Cotter DJ, Bang H. Predicting early death among elderly dialysis patients: development and validation of a risk score to assist shared decision making for dialysis initiation. Am J Kidney Dis. 2015;66(6):1024-1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hussain JA, Flemming K, Murtagh FE, Johnson MJ. Patient and health care professional decision-making to commence and withdraw from renal dialysis: a systematic review of qualitative research. Clin J Am Soc Nephrol. 2015;10(7):1201-1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Carson RC, Juszczak M, Davenport A, Burns A. Is maximum conservative management an equivalent treatment option to dialysis for elderly patients with significant comorbid disease? Clin J Am Soc Nephrol. 2009;4(10):1611-1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tong A, Manns B, Hemmelgarn B, et al. Establishing core outcome domains in hemodialysis: report of the Standardized Outcomes in Nephrology-Hemodialysis (SONG-HD) consensus workshop. Am J Kidney Dis. 2016;69(1):97-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Canadians Seeking Solutions and Innovations to Overcome Chronic Kidney Disease (Can-SOLVE CKD) Network. 2016. https://cansolveckd.ca/. Accessed December 20, 2016. [DOI] [PMC free article] [PubMed]
- 27. Mauri JM, Cleries M, Vela E. Design and validation of a model to predict early mortality in haemodialysis patients. Nephrol Dial Transplant. 2008;23(5):1690-1696. [DOI] [PubMed] [Google Scholar]
- 28. Chen JY, Tsai SH, Chuang PH, et al. A comorbidity index for mortality prediction in Chinese patients with ESRD receiving hemodialysis. Clin J Am Soc Nephrol. 2014;9(3):513-519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Holme I, Fellstrom BC, Jardin AG, Schmieder RE, Zannad F, Holdaas H. Prognostic model for total mortality in patients with haemodialysis from the Assessments of Survival and Cardiovascular Events (AURORA) study. J Intern Med. 2012;271(5):463-471. [DOI] [PubMed] [Google Scholar]
- 30. Chung SH, Noh H, Jeon JS, Han DC, Lindholm B, Lee HB. Impact of incremental risk factors on peritoneal dialysis patient survival: proposal of a simplified clinical mortality risk score. Blood Purif. 2009;27(2):165-171. [DOI] [PubMed] [Google Scholar]
- 31. Quinn RR, Laupacis A, Hux JE, Oliver MJ, Austin PC. Predicting the risk of 1-year mortality in incident dialysis patients: accounting for case-mix severity in studies using administrative data. Med Care. 2011;49(3):257-266. [DOI] [PubMed] [Google Scholar]
- 32. Vickers AJ, Elkin EB. Decision curve analysis: a novel method for evaluating prediction models. Med Decis Making. 2006;26(6):565-574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Steyerberg EW, Vergouwe Y. Towards better clinical prediction models: seven steps for development and an ABCD for validation. Eur Heart J. 2014;35(29):1925-1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Couchoud C, Hemmelgarn B, Kotanko P, Germain MJ, Moranne O, Davison SN. Supportive care: time to change our prognostic tools and their use in CKD. Clin J Am Soc Nephrol. 2016;11(10):1892-1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Canadian Medical Association. Nephrology Profile. 2016. https://www.cma.ca/Assets/assets-library/document/en/advocacy/profiles/nephrology-e.pdf. Accessed December 20, 2016.
- 36. Chiu HH, Tangri N, Djurdjev O, et al. Perceptions of prognostic risks in chronic kidney disease: a national survey. Can J Kidney Health Dis. 2015;2:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Levey AS, Eckardt KU, Tsukamoto Y, et al. Definition and classification of chronic kidney disease: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2005;67(6):2089-2100. [DOI] [PubMed] [Google Scholar]
- 38. Ludlow MJ, George CR, Hawley CM, et al. How Australian nephrologists view home dialysis: results of a national survey. Nephrology. 2011;16(4):446-452. [DOI] [PubMed] [Google Scholar]
- 39. Davison SN, Jhangri GS, Holley JL, Moss AH. Nephrologists’ reported preparedness for end-of-life decision-making. Clin J Am Soc Nephrol. 2006;1(6):1256-1262. [DOI] [PubMed] [Google Scholar]
- 40. Ward DR, Manns B, Gil S, Au F, Kappel JE. Results of the 2014-2015 Canadian Society of Nephrology workforce survey. Can J Kidney Health Dis. 2016;3:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Halbesleben JR, Whitman MV. Evaluating survey quality in health services research: a decision framework for assessing nonresponse bias. Health Serv Res. 2013;48(3):913-930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Johnson TP, Wislar JS. Response rates and nonresponse errors in surveys. JAMA. 2012;307(17):1805-1806. [DOI] [PubMed] [Google Scholar]