Abstract
Objective:
Suicide is a leading cause of death for transition-aged youth (TAY), and yet few studies examine correlates of suicidal ideation specifically in this age demographic (age 18-24 years). The transition to adulthood is a unique context, marked by novel stressors (e.g., joining the workforce) and increased independence, which may influence risk factors for suicidal ideation. This study examined correlates of suicidal ideation in TAY and adults and contrasted profiles across age.
Methods:
We used 4 biannual cycles (2005, 2007, 2009, 2011) of the Canadian Community Health Survey, a population-based cross-sectional survey on health. We used logistic regression to assess the association between suicidal ideation and depression, distress, alcohol use, smoking, exercise, sedentary behaviour, chronic illness, restrictions to daily living, perceived physical and mental health, and perceived social support independently in both TAY (n = 4427) and adults (n = 14,452). We subsequently assessed possible interactions with age (18-24 v. 25-44 years) and sex and differences in help-seeking behaviour in a combined model.
Result:
TAY exhibited higher rates of suicidal ideation than adults did (P < 0.001). Numerous factors were associated with suicidal ideation in TAY. Notably, alcohol abstinence was associated with decreased suicidal ideation in TAY but not for adults. Moreover, when depressed, TAY were significantly less likely to have received professional mental health help than adults (odds ratio = 0.64, 95% CI, 0.43 to 0.94).
Conclusions:
Suicidal ideation is more prevalent in TAY than adults, and its consequences may be aggravated by poor treatment-seeking behaviour in at-risk (i.e. depressed) individuals. These different risk profiles substantiate the recent shift toward clinical interventions focusing on transition-aged youth, rather than traditional child (<18 years) and adult (>18 years) services.
Keywords: suicide, transition-aged youth, emerging adulthood, adolescent, adult, risk factors
Abstract
Objectif:
Le suicide est une cause principale de décès chez les jeunes en transition à l’âge adulte (JTA), et pourtant, peu d’études examinent les corrélats de l’idéation suicidaire spécifiquement chez ce groupe d’âge (18-24 ans). La transition à l’âge adulte est un contexte unique, marqué de nouveaux stresseurs (p. ex., joindre la population active) et d’une indépendance accrue, qui peuvent influencer les facteurs de risque de l’idéation suicidaire. Cette étude a examiné les corrélats de l’idéation suicidaire chez les JTA et les adultes, et a contrasté les profils de tous âges.
Méthode:
Nous avons utilisé 4 cycles biennaux (2005, 2007, 2009, 2011) de l’Enquête sur la santé dans les collectivités canadiennes, une enquête sur la santé transversale dans la population. La régression logistique a servi à évaluer l’association entre l’idéation suicidaire et la dépression, la détresse, la consommation d’alcool, le tabagisme, l’exercice, le comportement sédentaire, la maladie chronique, les restrictions des activités quotidiennes, la santé physique et mentale perçue, et le soutien social perçu indépendamment chez les JTA (n = 4427) et les adultes (n = 14,452). Nous avons ensuite évalué les interactions possibles avec l’âge (18-24 c. 25-44) et le sexe, et les différences de comportement de recherche d’aide dans un modèle combiné.
Résultat:
Les JTA révélaient des taux plus élevés d’idéation suicidaire que les adultes (p < 0,001). De nombreux facteurs étaient associés à l’idéation suicidaire chez les JTA. Notablement, l’abstinence d’alcool était associée à une moindre idéation suicidaire chez les JTA mais pas chez les adultes. En outre, lorsqu’ils étaient déprimés, les JTA étaient significativement moins susceptibles d’avoir reçu une aide professionnelle en santé mentale que les adultes (RC = 0,64; IC à 95% 0,43 à 0,94).
Conclusions:
L’idéation suicidaire est plus prévalente chez les JTA que chez les adultes, et ses conséquences peuvent être aggravées par un faible comportement de recherche d’aide chez les personnes à risque (c.-à-d. déprimées). Ces différents profils de risque justifient la récente tendance vers des interventions cliniques qui portent sur les jeunes en transition à l’âge adulte, plutôt que sur les services traditionnels pour les enfants (< 18 ans) et les adultes (> 18 ans).
Late adolescents and young adults are a unique and vulnerable demographic for mental health disorders and suicidality. In Canada, suicide is the second leading cause of death for those aged 15 to 24 years,1 and a prospective study reported past suicidal ideation to be as high as 28.8% by age 21.2 Moreover, it has been shown that among this demographic, those aged 16 to 20 years exhibit the highest prevalence of suicidal thought, followed by individuals 21 to 25 years, then 26 to 35 years.3 This is paralleled by a surge in the incidence and severity of overall psychiatric symptoms, with most mental illness onset occurring before age 25.4 This burden is further exacerbated by low treatment rates as this age group exhibits poor help-seeking behaviour.5
The vulnerability of this age demographic is thought to be attributed, in part, to the stress of transitioning from child to adult societal roles. Transition-aged youth (TAY) are exposed to novel stressors such as financial independence, housing instability, entering the workforce, and so forth. Moreover, demographic changes in the past half-century, such as later marriage, increased post–secondary school attendance, and later childbirth, render this period not a brief transition but a longer stage without clear indicators of successful development (e.g., beginning a career, starting a family).6,7 The unique context of today’s TAY therefore appears to be more established than that of previous generations. While the age demarcation for transitioning youth is not distinct, we define TAY as age 18 to 24 years to capture those who have transitioned out of secondary school, are legally autonomous, and are still highly vulnerable to psychiatric symptoms. This is consistent with the concept of “emerging adulthood” previously proposed in the literature.6
Despite the growing literature on TAY, there is limited information about how risk factors for suicidal ideation might differ in this demographic compared with youth and adult populations. A large proportion of the existing literature uses clinical samples, and more representative population studies are underpowered because of the difficulty of suicidal ideation ascertainment and relatively small age range of TAY in cohort studies.7 In many cases, risk factor analysis in adults has been split into early adulthood (18-34 years) and later adulthood (35+ years) or studies of youth extended into early 20s, but even these distinctions fail to uniquely target the transition into adulthood.2,8 Thus, many of the current risk factors and interventions for TAY are extrapolated from childhood, adolescents, and adult studies of nonrepresentative samples and may not accurately identify the risk factors most pertinent during transition to adulthood. Moreover, there is very limited research on the interaction between age and common risk factors or help seeking for suicidal ideation. The current literature on depression suggests the strength of many common risk factors varies across age, yet few have investigated similar associations with suicidal ideation.9 One study demonstrated that depression is a stronger risk factor for suicidality in TAY, as with equal severities of depression, younger individuals were more likely to report significant suicidal ideation and attempted suicide.10
The objective of the current study was to use data from 4 waves of a population-based survey to examine correlates of suicidal thought in TAY compared with those in early/mid adult life, including measures of mental health, substance use, physical activity, physical health, perceived social support, and help-seeking behaviour.
Methods
Sample
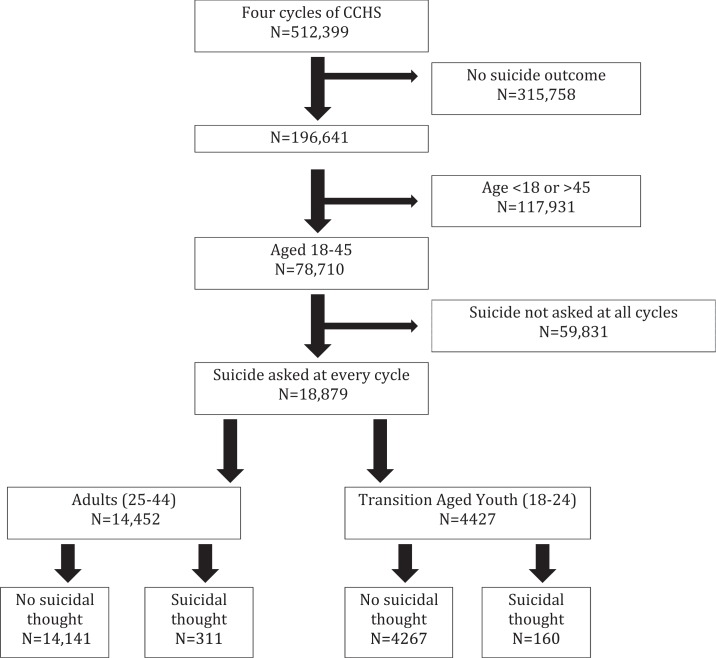
Data for this study came from the Canadian Community Health Survey (CCHS), a repeated cross-sectional survey on health and health care administered by computer or telephone. The CCHS excludes (1) those living on aboriginal reserves, (2) full-time Canadian Armed Forces employees, and (3) institutionalized populations, which together comprise 3% of the population. We included residents of Alberta who responded to CCHS cycles in 2005, 2007-2008, 2009-2010, or 2011-2012. Other provinces did not consistently report suicidal ideation over this time period and therefore could not be pooled into one sample population with appropriate use of sampling weights. Our study was limited to those aged 18 to 44 years, leaving a sample of 19,380, of whom 18,879 responded to questions about suicidal thought. Age was regrouped into a binary variable: TAY (age 18-24, n = 4544) and adult (age 25-44, n = 14,836; Figure 1).
Figure 1.
Flow diagram of participant eligibility in the Canadian Community Health Survey (CCHS).
Measures
Outcome
Suicidal ideation in the past 12 months was measured by self-report from the question, “Have you ever seriously considered committing suicide or taking your own life?” and if so, “Has this happened in the past 12 months?”
Exposures
Common and proximal risk factors for adult and youth suicidality/depression were identified in the literature.8,11–13 Of the identified factors, those available in the survey were included in the study: depression, distress, alcohol use, smoking, exercise and sedentary behaviour, chronic illness, restrictions to daily living, perceived physical and mental health, perceived social support, and help seeking.
Depression was assessed using the Derived Depression Scale, based on the Composite International Diagnostic Interview.14 An individual with a predictive probability of 90% or higher was considered to have major depression (a score of 5 or higher on a 0-8 scale). This corresponds to the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV), criteria for a major depressive episode (5 of 9 depressive symptoms in a 2-week period during the past year, including either loss of interest or depressed mood). Similarly, distress was assessed using the Kessler K10 questionnaire out of 40 and was recoded into no (0-19), mild (20-24), moderate (25-29), and severe (30+) risk of mental disorder according to past practices.15 In the help-seeking analysis, distress was dichotomized at the 90th percentile for comparability with depression.
Alcohol use was assessed by history and frequency of drinking. We dichotomized drinkers and abstainers and, in a second variable of drinkers, those who drink occasionally versus regularly. Smoking was assessed by the question, “At the present time, do you smoke cigarettes daily, occasionally, or not at all?” Exercise was quantified by frequency and types of activities such as swimming, bicycling, and so on. Energy expenditure was calculated and categorized into active, moderate, and inactive.16 Similarly, we coded tertiles of sedentary behaviour, ascertained by number of hours spent in the past 3 months doing low-energy activities such as TV, computer, and video game use.
Chronic illness was a self-reported measure from a list of 22 physician-diagnosed illnesses such as asthma, arthritis, and diabetes. “Restrictions to daily living” was dichotomized as self-reported “never” versus “sometimes” or “often” difficulty with hearing, seeing, communicating, walking, climbing stairs, bending, learning, and/or doing any similar activities.
Perceived health and mental health were based on self-report of the question, “In general, how would you say your (mental) health is now?” whereby participants marked poor, fair, good, very good, or excellent. Tangible social support was derived from the Medical Outcomes Study Social Support Survey.17 It ranges from 0 to 16, whereby high scores denote better support.
Lastly, help seeking was assessed by the question, “In the past 12 months, have you ever seen or talked to a health professional about your emotional or mental health?”
Statistical Analysis
Prevalence was calculated for each cycle individually and presented over time. For the remaining analyses, 4 biannual cycles were combined into 1 sample using the pooled approach.18 Variance was calculated using population weights and provincial design effects provided by Statistics Canada to account for the complex survey design. Initially, logistic regression was used to test the strength of common risk factors of suicidal ideation and any sex interactions only in TAY. Subsequently, for each identified risk factor in TAY, we repeated the analysis with age and sex interactions in a sample that comprised both TAY and adults aged 25 to 44 years. We calculated the prevalence of help seeking only in those with depression, suicidal thought, and high distress in both TAY and adults and then compared these 2 groups using Pearson’s chi-squared test. Logistic regression was used to estimate odds ratios (ORs) for help-seeking behaviours across age (i.e., TAY v. adults). All analyses were complete case analyses. All analyses were conducted using Stata v12.19
Results
Sample Demographic Information
Demographic characteristics of the sample are provided in Table 1. TAY were significantly more likely to be depressed, drink alcohol and drink alcohol regularly, engage in more sedentary activity, and were less likely to have received mental health help in the past 12 months. Conversely, they were less likely to have a chronic illness and more likely to be physically active.
Table 1.
Sample demographic information.
| Total (N = 19380) | Transition-aged youth (n = 4544) | Adults (n = 14,836) | P Valuea | Proportion with missing data (n = 19,380) | |
|---|---|---|---|---|---|
| Population characteristic | |||||
| Suicidal thoughts | 2.5 | 3.6 | 2.2 | <0.001 | 2.5 |
| Sex (male) | 48.1 | 48.5 | 48.0 | 0.578 | 0 |
| Mental health | |||||
| Depressed (≥5/8) | 7.6 | 8.6 | 7.2 | 0.006 | 24.6 |
| Perceived poor/fair mental health | 5.3 | 5.1 | 5.4 | 0.363 | 0.05 |
| K10 Distress Score (0-40) | 0.226 | 50.1 | |||
| Minimal (0-19) | 97.5 | 97.4 | 97.6 | ||
| Mild (20-24) | 1.6 | 1.9 | 1.5 | ||
| Moderate/severe (25-40) | 0.9 | 0.7 | 0.8 | ||
| Substance use | |||||
| Current smoker | 29.1 | 29.8 | 29.0 | 0.258 | 0.3 |
| Current drinker | 85.2 | 88.4 | 84.2 | <0.001 | 1.2 |
| Of drinkers, regular users | 79.9 | 82.9 | 78.9 | <0.001 | 1.2 |
| Physical activity | |||||
| Exercise (moderate/high) | <0.001 | 1.0 | |||
| Inactive | 43.8 | 37.4 | 45.8 | ||
| Moderate activity | 25.4 | 23.9 | 25.9 | ||
| Active | 30.8 | 38.6 | 28.3 | ||
| Sedentary behaviour | <0.001 | 53.1 | |||
| Lowest tertile | 38.0 | 33.6 | 39.3 | ||
| Middle tertile | 34.7 | 32.3 | 35.4 | ||
| Highest tertile | 27.3 | 34.0 | 25.3 | ||
| Physical health | |||||
| Perceived poor/fair physical health | 6.9 | 6.9 | 6.9 | 0.984 | 0.1 |
| Chronic illness | 50.1 | 45.0 | 51.6 | <0.001 | 0.1 |
| Help-seeking factors | |||||
| 75th percentile perceived social support (0-16) | 11 | 12 | 11 | 0.007 | 75.1 |
| Received previous mental health support | 13.8 | 11.2 | 14.7 | <0.001 | 2.2 |
Results are presented as percentages of the total sample size.
aCorresponding to Pearson’s chi-squared test for categorical variables and analysis of variance for continuous variables (i.e., social support).
Prevalence
The overall prevalence of suicidal thought in the past 12 months was stable in TAY, decreasing insignificantly from 4.34% (2.80-5.87) in 2005 to 3.02% (1.25-4.80) in 2011. Adult suicidal thought was similarly prevalent and stable, ranging from 2.26% (1.62-2.90) to 2.00% (1.19-2.80; Figures 2 and 3). Overall, TAY exhibited a higher prevalence of suicidal ideation than adults (P < 0.001; Table 1).
Figure 2.
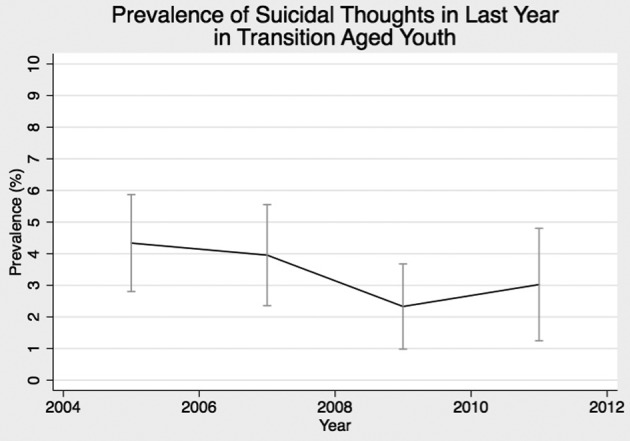
Prevalence of suicidal ideation among transition-aged youth (18-24 years) across 4 cycles of the Canadian Community Health Survey.
Figure 3.
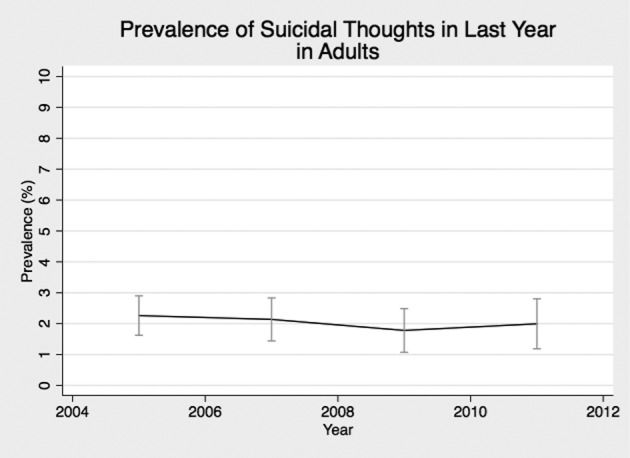
Prevalence of suicidal ideation among adults (25-44 years) across 4 cycles of the Canadian Community Health Survey.
Associations with Suicidal Thought in Transition-Aged Youth
There were significant associations between all investigated risk factors and suicidal ideation in TAY except physical activity and perceived social support (Table 2). The strongest predictors were mental health predictors: moderate/severe level of distress (OR = 22.8; 95% CI, 7.1 to 73.1), fairly or poorly perceived mental health (OR = 17.5; 95% CI, 10.5 to 29.2), and depression (OR = 14.3; 95% CI, 8.3 to 24.6). All markers of poor physical health were also strong predictors of suicidal ideation, with ORs ranging from 3.8 to 4.5. Of the modifiable lifestyle factors, only alcohol consumption (OR = 3.4; 95% CI, 1.6 to 7.2) and smoking (OR = 2.5; 95% CI, 1.5 to 3.9) were significant risk factors. The association between regularity of alcohol consumption and suicidal ideation among drinkers was nonsignificant.
Table 2.
Association between risk factors and suicidal ideation in transition-aged youth.
| Risk Factor | OR (95% CI) |
|---|---|
| Demographic | |
| Sex (male) | 0.9 (0.6 to 1.4) |
| Mental health | |
| High risk of depression | 14.3 (8.3 to 24.6)* |
| Poor/fair perceived mental health | 17.5 (10.5 to 29.2)* |
| Distress | |
| Mild | 18.9 (7.3 to 48.7)* |
| Moderate/severe | 22.8 (7.1 to 73.1)* |
| Substance use | |
| Smoking | 2.58 (1.6, to 3.9)* |
| Any alcohol consumption | 3.4 (1.6 to 7.2)* |
| Of drinkers, regular consumption | 1.0 (0.5 to 1.8) |
| Physical activity | |
| Exercise | |
| Inactive | 1.00 |
| Moderate | 0.7 (0.4 to 1.2) |
| Active | 1.4 (0.8 to 2.3) |
| Sedentary behaviour | |
| Low | 1.00 |
| Medium | 1.0 (0.4 to 2.3) |
| High | 1.0 (0.5 to 2.3) |
| Physical health | |
| Chronic illnesses | 4.5 (2.6 to 7.8)* |
| Restrictions to daily living | 4.2 (2.4 to 7.2)* |
| Poor/fair perceived physical health | 3.8 (2.1 to 6.9)* |
| Help seeking | |
| Social support | 0.9 (0.8 to 1.0) |
| Received mental health support | 11.9 (7.6 to 19.5)* |
Odds ratios with 95% confidence intervals are presented.
*P < .05.
Two significant sex interactions were found. Severely distressed men had an increased odds of suicidal ideation (OR = 49.0; 95% CI, 19.1 to 125.7) compared with women (OR = 11.3; 95% CI, 4.3 to 29.8). Conversely, women with poor perceptions of physical health had increased odds of suicidal ideations (OR = 7.6; 95% CI, 3.3 to 17.1) compared with men (OR = 1.9; 95% CI, 0.9 to 4.0).
Comparison between TAY and Adults
Interaction analyses suggested that age group modified the correlation between (1) depression and suicidal thought (P = 0.041) and (2) alcohol use and suicidal thoughts (P = 0.009).
Depression increased the odds of suicidal thought in TAY by a factor of 14.3 (95% CI, 8.3 to 24.6), whereas in adults, depression increased the odds of suicidal thought by a factor of 29.5 (95% CI, 19.1 to 45.6). For alcohol, any alcohol use was associated with an increased risk in suicidal ideation for TAY (OR = 3.4; 95% CI, 1.6 to 7.1), whereas any alcohol use in adults showed no difference (OR = 1.0; 95% CI, 0.6 to 1.7).
In addition, there was a significant 3-way interaction between sex, age, and exercise, wherein inactive male TAY and female adults had the highest odds of suicidal ideation (OR = 2.1; 95% CI, 1.1 to 3.9; and OR = 1.7; 95% CI, 1.1 to 2.8, respectively). Conversely, there was no significant effect of inactivity in female TAY (OR = 1.1; 95% CI, 0.6 to 2.3) or male adults (OR = 1.0; 95% CI, 0.6 to 1.6).
Help-Seeking Behaviour
Help seeking was less common in depressed, distressed, or suicidal TAY compared with adults (Table 3). In the logistic regression model, transition age was significantly associated with decreased odds of getting help when depressed (OR = 0.64; 0.43 to 0.94). Distressed patients showed a similar but nonsignificant trend.
Table 3.
Help-seeking behaviour.a
| Depressed (n = 1102) | Distressed (n = 699) | Suicidal (n = 470) | |
|---|---|---|---|
| TAY | 39.8% (32.0 to 47.5) | 35.7% (26.9 to 44.5) | 54.8% (43.8 to 65.7) |
| Adults | 50.7% (45.2 to 56.2) | 44.3% (36.9 to 51.7) | 56.4% (47.2 to 65.6) |
| Odds ratio (95% CI) | 0.64 (0.43 to 0.94)* | 0.70 (0.43 to 1.14) | 0.92 (0.51 to 1.64) |
aProportions with confidence intervals of past help-seeking behaviour among transition-aged youth (TAY) and adults who are depressed, distressed, and/or suicidal. Odds ratios with 95% confidence intervals are presented.
*P < .05.
Discussion
In this large, repeated cross-sectional study, we demonstrated a stable prevalence of suicidal thought in TAY over time, consistent with a previous Centers for Disease Control and Prevention report on adolescents showing a change of only 0.1% from 2005 to 2013.20 We also found that TAY were significantly more likely to have suicidal ideation than adults aged 25 to 44 years. This finding is supported in the literature, wherein a multinational survey, those aged 18 to 34 years were approximately twice as likely to have lifetime suicidal ideation compared with those aged 35 to 49 years,8 and in a second study dividing age by smaller intervals, suicidal ideation was found to be highest in the <20 years age group.21 However, the former assessed lifetime risk retrospectively, and the latter did not test the age distinction statistically. The age categories were also not specific to transition age. Our study is the first to assess and compare the past 12-month prevalence of adults specifically with TAY.
We found 9 factors correlated with suicidal ideation in TAY: depression, distress, smoking, alcohol consumption, chronic illness, restrictions to daily living, social support, perceived physical health, and perceived mental health. Of these risk factors, alcohol and depression were differentially associated with suicidal ideation across age groups. Alcohol consumption was a stronger risk factor for suicidal ideation in TAY than in adults. As there was no distinction between occasional and regular drinkers, we believe abstinence from alcohol may have indirect protective effects in TAY. For example, youth abstainers have reported better home well-being than light drinkers,22 a protective factor for suicidal ideation.23 Conversely, depression was a weaker risk factor in TAY than in adults, contrary to previous findings.10 This association is likely confounded by the buffering effects of social support, as the interaction was no longer significant when perceived social support was included in the model.24 A Canadian cohort study found that TAY with high social support were less likely to become depressed after experiencing stressful life events.25 In the current sample, social support scores were higher in TAY compared with adults, which could explain the observed age interaction.
In addition to risk factor strength, the prevalence of these risk factors contributes to overall pertinence. For example, depression is more prevalent in TAY than adults, and despite depression being a weaker risk factor for depression than in adults, its overall prevalence may account for the higher prevalence of suicidal ideation in TAY.
Lastly, TAY were less likely than adults to have sought mental health help when depressed, a finding that has been suggested in the literature5,26 but has not been explicitly tested. Societal contexts likely explain this difference. For example, desire for autonomy during this stage of life has previously been proposed as a moderator of help-seeking behaviour in TAY.5 Alternatively, TAY are transitioning out of a phase in which guidance counselors, teachers, and family were gatekeepers to mental health services and may therefore have fewer role models to encourage help-seeking behaviour. Without such guidance, there might be confusion about where to get help. For example, few young adults consider a general practitioner a source of help, even when no alternatives are available.27
The results contribute to the growing literature that child and adult psychiatric services should not be dichotomized at age 18 but should account for the vulnerability of TAY.28 We demonstrated that TAY have slightly different risk factor patterns, have different prevalence rates of the relevant risk factors, and exhibit different help-seeking behaviour compared with adults. These differences occur in conjunction with decreased availability, legal right to refuse treatment, and less family involvement in adult services that have previously contributed to poor transition rates, and they may account for the decreased use of psychiatric services in this demographic.29 New models of psychiatric care have therefore begun to focus on services specifically for transitioning youth. For example, Youthspace in the United Kingdom is providing guidance to general practitioners to help identify and treat 16- to 25-year-olds for mental illness in a low-stigma environment.30 Our results are useful to inform these clinical services in Canada in the absence of existing epidemiological evidence for this demographic.
The interpretation of these results must be made in the context of several limitations. Namely, the data source was not designed specifically for investigating suicidal ideation and thus did not have appropriate variables for all relevant risk factors for suicidal ideation, such as drug use.31 Moreover, the sensitive nature of questions on suicidality may have discouraged participants to accurately report suicidal thought; however, all participants were assured of confidentiality to mitigate this possibility. We further were limited to concurrent correlates given the cross-sectional nature of the study and thus could not analyze individual history. By doing so, we focused on proximal risk factors that are more reliably ascertained and modifiable in the future. With respect to generalizability, our study is limited by inclusion of one province and exclusion of institutionalized populations. The latter suggests we may have underestimated the prevalence of suicidal ideation; however, past studies have shown similar rates of inpatient and outpatient uses between age categories, suggesting the remaining comparative analysis are valid.32 Lastly, the assessment of help-seeking behaviour did not specify for what the subject got help. Thus, it is possible that even those who did get help were not benefiting with respect to depression, distress, or suicidal ideation. However, this renders our estimates conservative and strengthens our claim that there is a significant difference between TAY and adults.
The limitations are offset by notable strengths. The study uses a large, representative survey and therefore has sufficient power to analyze a small demographic with a relatively rare outcome. Our data set further mitigates any selection bias present in past studies of TAY suicide by using a population-based sample rather than volunteers or clinical samples. Moreover, we are the first to specifically look at correlates at age 18 to 24 years, the most transition-dense period of early adulthood.6 Our study is well suited to assess correlates of suicidal ideation associated with the transition of adolescents to adulthood, and the results have important implications for improving Canadian mental health literacy in this population.33
Conclusion
In this study, we demonstrate similar patterns of suicidal ideation in TAY and adults. The prevalence over time showed similar trends, and the strength of the investigated risk factors was comparable in both age groups. Three robust differences between TAY and adult populations were identified: We demonstrated a significant difference in prevalence of suicidal thought between age; TAY have more suicidal ideation in the past 12 months. Second, alcohol abstinence was associated with decreased suicidal ideation in TAY but not for adults. Third, of those who are depressed, TAY were less likely to seek help. The latter finding identifies a clear target for intervention, and together, these results encourage a focus on help-seeking and clinical treatments designed specifically for TAY.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported, in part, by funding from the Canada Research Chairs program for IC.
References
- 1. Bennett K, Rhodes AE, Duda S, et al. A youth suicide prevention plan for Canada: A systematic review of reviews. Can J Psychiatry. 2015;60(6):245–257. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4501582/pdf/cjp-2015-vol60-june245-257-rev.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fergusson DM, Woodward LJ, Horwood LJ. Risk factors and life processes associated with the onset of suicidal behaviour during adolescence and early adulthood. Psychol Med. 2000;30:23–39. [DOI] [PubMed] [Google Scholar]
- 3. Sumnall H, Bellis MA, Hughes K, Calafat A, Juan M, Mendes F. A choice between fun or health? Relationships between nightlife substance use, happiness, and mental well-being. J Subst Use. 2010;15(2):89–104. [Google Scholar]
- 4. Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56(7):617–626. [DOI] [PubMed] [Google Scholar]
- 5. Wilson CJ, Rickwood DJ, Bushnell JA, Caputi P, Thomas SJ. The effects of need for autonomy and preference for seeking help from informal sources on emerging adults’ intentions to access mental health services for common mental disorders and suicidal thoughts. Adv Ment Health. 2011;10(1):29–38. [Google Scholar]
- 6. Arnett JJ. Emerging adulthood: a theory of development from the late teens through the twenties. Am Psychol. 2000;55(5):469–480. [PubMed] [Google Scholar]
- 7. Terzian M, Moore K, Constance N. Transition to Adulthood: The Role of Adolescent Depression and Suicidal Ideation. Child Trends; 2014. Available from: http://www.childtrends.org/wp-content/uploads/2014/11/2014-45SuicidalIdeation.pdf
- 8. Nock MK, Borges G, Bromet EJ, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008;192(2):98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Naicker K, Galambos NL, Zeng Y, Senthilselvan A, Colman I. Social, demographic, and health outcomes in the 10 years following adolescent depression. J Adolesc Heal. 2013;52(5):533–538. [DOI] [PubMed] [Google Scholar]
- 10. Seo HJ, Song HR, Yim HW, et al. Age-related differences in suicidality between young people and older adults with depression: data from a nationwide depression cohort study in Korea (the CRESCEND study). Compr Psychiatry. 2015;56:85–92. [DOI] [PubMed] [Google Scholar]
- 11. Nock MK, Kessler RC. Prevalence of and risk factors for suicide attempts versus suicide gestures: analysis of the National Comorbidity Survey. J Abnorm Psychol. 2006;115(3):616–623. [DOI] [PubMed] [Google Scholar]
- 12. Lindeman S, Hämäläinen J, Isometsä E, et al. The 12-month prevalence and risk factors for major depressive episode in Finland: representative sample of 5993 adults. Acta Psychiatr Scand. 2000;102(3):178–184. [DOI] [PubMed] [Google Scholar]
- 13. Brown GK, Beck AT, Steer RA, Grisham JR. Risk factors for suicide in psychiatric outpatients: a 20-year prospective study. J Consult Clin Psychol. 2000;68(3):371–377. [PubMed] [Google Scholar]
- 14. Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen H-U. The World Health Organization Composite International Diagnostic Interview. Int J Methods Psychiatr Res. 1998;7(4):171–185. Available form: http://onlinelibrary.wiley.com/store/10.1002/mpr.47/asset/47_ftp.pdf?v=1&t=ikzk6sr2&s=e6d05bd2eecf285d785907d29b5c909342bc208b [Google Scholar]
- 15. Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–976. [DOI] [PubMed] [Google Scholar]
- 16. Statistics Canada. Canadian Community Health Survey Cycle 3.1 Public Use Micro Data File. Vol 368. Ottawa (Ontario): Statistics Canada; 2006. Available from: http://www23.statcan.gc.ca/imdb-bmdi/document/3226_D5_T9_V3-eng.pdf [Google Scholar]
- 17. Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–714. [DOI] [PubMed] [Google Scholar]
- 18. Thomas S, Wannell B. Health Reports: Combining Cycles of the Canadian Community Health Survey. Ottawa (Ontario: ): Statistics Canada; 2009. [PubMed] [Google Scholar]
- 19. StataCorp. Stata Statistical Software: Release 12. College Station (TX): Statistics Canada; 2011. [Google Scholar]
- 20. Centers for Disease Control and Prevention. Trends in the Prevalence of Suicide-Related Behavior. National YRBS: 1991-2013. 2013:4636. Available from: http://www.cdc.gov/healthyyouth/data/yrbs/pdf/trends/us_suicide_trend_yrbs.pdf
- 21. Forkmann T, Brähler E, Gauggel S, Glaesmer H. Prevalence of suicidal ideation and related risk factors in the German general population. J Nerv Ment Dis. 2012;200(5):401–405. [DOI] [PubMed] [Google Scholar]
- 22. Leifman HK, Kühlhorn E, Allebeck P, Andréasson S, Romelsjö A. Abstinence in late adolescence: antecedents to and covariates of a sober lifestyle and its consequences. Soc Sci Med. 1995;41(1):113–121. [DOI] [PubMed] [Google Scholar]
- 23. Taliaferro LA, Muehlenkamp JJ. Risk and protective factors that distinguish adolescents who attempt suicide from those who only consider suicide in the past year. Suicide Life-Threatening Behav. 2014;44(1):6–22. [DOI] [PubMed] [Google Scholar]
- 24. Olstad R, Sexton H, Søgaard AJ. The Finnmark study. A prospective population study of the social support buffer hypothesis, specific stressors and mental distress. Soc Psychiatry Psychiatr Epidemiol. 2001;36(12):582–589. [DOI] [PubMed] [Google Scholar]
- 25. Colman I, Zeng Y, McMartin SE, et al. Protective factors against depression during the transition from adolescence to adulthood: findings from a national Canadian cohort. Prev Med (Baltim). 2014;65:28–32. [DOI] [PubMed] [Google Scholar]
- 26. Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry. 2010;10(113):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Biddle L, Donovan J, Sharp D, Gunnell D. Explaining non-help-seeking amongst young adults with mental distress: a dynamic interpretive model of illness behaviour. Soc Health Illn. 2007;29(7):983–1002. [DOI] [PubMed] [Google Scholar]
- 28. Iyer SN, Boksa P, Lal S, et al. Transforming youth mental health: a Canadian perspective. Ir J Psychol Med. 2015;32(1):51–60. [DOI] [PubMed] [Google Scholar]
- 29. Singh SP, Paul M, Ford T, et al. Process, outcome and experience of transition from child to adult mental healthcare: multiperspective study. Br J Psychiatry. 2010;197(4):305–312. [DOI] [PubMed] [Google Scholar]
- 30. McGorry P, Bates T, Birchwood M. Designing youth mental health services for the 21st century: examples from Australia, Ireland and the UK. Br J Psychiatry. 2013;202(Suppl. 54):30–36. [DOI] [PubMed] [Google Scholar]
- 31. Wong SS, Zhou B, Goebert D, Hishinuma ES. The risk of adolescent suicide across patterns of drug use: a nationally representative study of high school students in the United States from 1999 to 2009. Soc Psychiatry Psychiatr Epidemiol. 2013;48(10):1611–1620. [DOI] [PubMed] [Google Scholar]
- 32. Pottick KJ, Bilder S, Vander Stoep A, Warner LA, Alvarez MF. US patterns of mental health service utilization for transition-age youth and young adults. J Behav Heal Serv Res. 2008;35(4 Special Issue):373–389. [DOI] [PubMed] [Google Scholar]
- 33. Marcus M, Westra H. Mental health literacy in Canadian young adults: results of a national survey. Can J Community Ment Heal. 2012;31(1):1–15. [Google Scholar]