Abstract
Background:
The reported rate of second anterior cruciate ligament (ACL) injuries (20%-30%), including graft failure and contralateral ACL tears, after ACL reconstruction (ACLR) or nonoperative therapy indicates that multiple factors may predispose patients to subsequent ACL injuries.
Purpose:
To determine the incidence of second ACL injuries in a population-based cohort over a 10-year observation period (2001-2010) and to identify factors that contribute to the risk of second injuries.
Study Design:
Descriptive epidemiological study.
Methods:
International Classification of Diseases, 9th Revision (ICD-9) codes relevant to the diagnosis of an ACL tear and the procedure code for ACLR were utilized to search the Rochester Epidemiology Project, a multidisciplinary county database, between the years of 2001 and 2010. The complete medical records for all cases were reviewed to confirm diagnosis and treatment details. A total of 914 unique patients with 1019 acute, isolated ACL tears were identified. These patients were stratified by primary and secondary tears, sex, age, activity level, side of injury, sex × side of injury, and graft type of reconstruction.
Results:
Second ACL tears were recorded in 141 (13.8%) of the 914 patients diagnosed with an ACL tear in Olmsted County, Minnesota, USA, from 2001 to 2010; 50.4% of these occurred in the contralateral knee. A noncontact mechanism was responsible for 76.4% of all ACL injuries. A second ACL injury was influenced by factors of sex × age group, treatment type × age group, and treatment type × activity level. Nonparametric analysis of graft disruption × graft type demonstrated that a higher prevalence of second ACL tears occurred with allografts compared with hamstring autografts (P = .0054) and patellar tendon autografts (P = .0001).
Conclusion:
The incidence of second ACL tears in this population-based cohort was 13.8%, and half occurred to the ACL of the contralateral knee. Statistically, second ACL injuries differed by sex, occurring in female patients younger than 25 years and male patients aged 26 to 45 years. Allografts continued to be associated with a greater risk of second ACL injuries compared with hamstring and patellar tendon autografts. Nonoperative treatment carried more risk of contralateral tears than ACLR.
Keywords: anterior cruciate ligament (ACL), graft tear, epidemiology, incidence, secondary
Second anterior cruciate ligament (ACL) tears, either ipsilateral (graft failure) or contralateral,34 continue to devastate patients and the economy. Annual costs for ACL reconstruction (ACLR) and rehabilitation (either after surgery or nonoperative therapy) exceed US$2 billion.3,11,12,16 ACL tears are associated with serious concomitant injuries, including meniscal lesions,23 bone bruises, fractures, and sequelae of cartilage degeneration25 and early-onset osteoarthritis within 10 to 15 years.6,19 A patient with a second ACL injury may also experience fear upon returning to sports2,24 or require additional rehabilitation beyond what insurance coverage will allow. The risk of second ACL injuries has been reported to be as high as one-third,8,9,27,44 which is a high and likely preventable recurrence rate. A reduction in the occurrence of subsequent ACL tears would be ideal, as the long-term consequences of a second ACL injury increase the future economic burden and individual suffering.
Previous studies of second ACL injuries have indicated that factors such as patient age,22,27,50,52 sex,27 activity level,5,22,27,52 time delay before ACLR,45 and graft type22,27,50 are predictive of future ACL injuries.28 ACLR continues to be a common orthopaedic procedure, but many controversies exist over prevention, graft selection, and rehabilitation.5,13,22,37,51,53 Geographically based epidemiological data are lacking to support these outcomes. Studies should examine the geographic, population-based epidemiological trends of second ACL injuries because the number of children engaging in high-level athletics is increasing and older patients are staying more active.28
As a follow-up to our previous geographic, population-based epidemiological report on second ACL injuries,41 the purpose of this continuation study was (1) to determine the incidence of second ACL injuries in a population-based cohort over a 10-year time span (2001-2010) and (2) to determine factors associated with a second ACL injury. Our rationale for this continuation study is that knowledge of both the historical and geographically based incidence of second ACL injuries will (1) allow for improved understanding of the epidemiological progression of the disease, especially with advances in technology and technique, and (2) assist in the prevention and rehabilitation of a second ACL injury8,33,34 and its resultant sequelae.
Methods
The Rochester Epidemiology Project38 (REP) is a medical record linkage system that provides access to complete medical records for all residents of Olmsted County, Minnesota, USA, regardless of the medical facility in which the care was delivered.38,46–48 Since its inception, the REP database has included over 6.1 million health records. This unique population-based data infrastructure allows the complete determination and follow-up of all clinically diagnosed cases in a geographically defined community.38 In addition, the epidemiological data of the REP have demonstrated generalizability to larger populations.47
The REP database was utilized with inclusion criteria of all occurrences of ACL tears (based on International Classification of Diseases, 9th Revision [ICD-9] billing codes consistent with an ACL injury) from 2001 to 2010. Second ACL injuries, defined as any ACL tear after a primary injury (either ipsilateral or contralateral), were tracked in this same cohort of patients through December 31, 2016. Contralateral ACL injuries were defined as an ACL injury to the opposite knee of the original index injury. Records were searched for evidence of a second ACL injury via orthopaedic examinations, arthroscopic examinations, magnetic resonance imaging (MRI), or surgical records of ACLR. The results yielded 1738 patients in the geographic locale. Three authors (N.D.S., C.N., and N.A.B.) reviewed all medical records individually to confirm the accuracy of the diagnosis and gather relevant data regarding each patient and his or her outcomes. Subsequently, 719 of the 1738 patients were excluded from further analysis because of the confirmation of non-ACL injuries (eg, posterior cruciate ligament tears, meniscal injuries, MRI confirmation of tear absence) or chronic ACL injuries (defined as >2 years from the time of diagnosis). We identified 1019 unique, acute-onset, isolated ACL tears, regardless of the reconstruction status, in 914 unique patients (approximately 1.0% of the total population). Of these patients, 141 sustained a secondary ACL injury. Additionally, 756 (80.4%) of the 914 patients elected to undergo ACLR. Various factors potentially predictive of a second ACL injury were examined, including sex, age, activity level, sex × side of injury, sex × activity level (sedentary, recreational, or competitive), side of tear, and graft type of reconstruction. All allografts were combined for analysis because of the variety of allografts and the limited number of allografts available. All ACL tears were categorized as complete, partial, or unknown by MRI or arthroscopic examinations. If a partial tear was diagnosed, a later diagnosis of a complete tear was not considered as a secondary injury. Institutional review board approval was obtained from both the Mayo Clinic (14-003215) and the Olmsted Medical Center (026-OMC-14), and informed consent was obtained previously from all patients.
All statistical analyses were performed using JMP 10 (SAS Institute). The nonparametric Wilcoxon rank test and post hoc Wilcoxon each-pair test were utilized for nonparametric factors. One-way analyses of variance were utilized to calculate means regarding the risk of second ACL injuries. Contingency analyses were performed for graft type selection. Statistical significance was set at P < .05.
Results
The mean (±SD) occurrence of ACL tears from 2001 to 2010 in Olmsted County, Minnesota was 97.9 ± 8.4 per year. This averaged trend of ACL tears was steady over time. A noncontact mechanism was responsible for 76.6% of these injuries. Of the 914 patients (mean age, 29.4 ± 11.7 years; 581 male) (Table 1), a second ACL tear was recorded in 141 (13.8%); these included 65 (46.1%) graft ruptures, 71 (50.4%) contralateral tears, and 5 (3.5%) ruptures of a contralateral graft (ie, contralateral retear). Also, 6.4% of all ACL injuries were graft ruptures, and 7.4% were contralateral tears. Of the second injuries, 74.5% occurred via noncontact mechanisms. Subsequently, 819 (80.4%) of the 1019 recorded ACL injuries underwent ACLR. Moreover, 24.7% of the patients were lost to follow-up, defined as no health record entry after January 1, 2013. The mean follow-up was 8.1 ± 3.7 years. A graft rupture occurred, on average, at 3.7 ± 3.0 years, and a contralateral tear occurred, on average, at 4.7 ± 3.8 years.
TABLE 1.
Demographics of Anterior Cruciate Ligament Tearsa
| No. of tears | 1019 |
| Age, mean ± SD, y | 29.4 ± 11.7 |
| Sex | |
| Male | 581 (57.0) |
| Female | 438 (43.0) |
| Tear type | |
| Complete | 828 (81.3) |
| Partial | 130 (12.7) |
| Unknown | 61 (6.0) |
| Activity level | |
| Competitive | 197 (19.3) |
| Recreational | 673 (66.0) |
| Sedentary | 70 (6.9) |
| Unknown | 79 (7.8) |
| Tear occurrenceb | |
| Primary | 878 (86.2) |
| Secondary | 141 (13.8) |
| Graft failure | 65 (46.1) |
| Contralateral tear | |
| ACL reconstruction | 73 (51.8) |
| Nonoperative therapy | 3 (2.1) |
aValues are expressed as n (%) unless otherwise specified.
bOf the 914 unique patients, 141 patients sustained additional anterior cruciate ligament (ACL) tears from the time of initial inclusion to 2017, 40 of the secondary injuries included occurred after 2010, and 8 patients sustained multiple second injuries.
There were 828 complete tears and 130 partial tears. Of the 130 partial tears, 89 underwent surgical treatment, and 41 were treated nonoperatively. Of the 828 complete tears, 696 underwent surgical treatment, and 132 were treated nonoperatively. There was no statistically significant influence of treatment selection × tear type (partial vs complete) on second ACL injury.
Age ≤16 years compared to all other ages was not significant for a second ACL injury (Z 1 = 0.0379; P = .8456). Additionally, sex × age ≤16 years did not demonstrate predictive strength for a second injury (Z 1 = 0.1481; P = .7004). However, there was a higher percentage of primary (69.4%) and secondary (64.7%) injuries in female patients aged ≤16 years compared to their male counterparts (Table 2).
TABLE 2.
Anterior Cruciate Ligament Tears by Age Groupa
| Male | Female | Total | |
|---|---|---|---|
| Primary tears | |||
| ≤16 y | 34 (30.6) | 77 (69.4) | 111 (12.6) |
| 17-25 y | 192 (66.7) | 96 (33.3) | 288 (32.8) |
| 26-35 y | 137 (67.8) | 65 (32.2) | 202 (23.0) |
| 36-45 y | 94 (53.1) | 83 (46.9) | 177 (20.2) |
| 46-55 y | 34 (39.5) | 52 (60.5) | 86 (9.8) |
| >55 y | 8 (57.1) | 6 (42.9) | 14 (1.6) |
| All | 878 (100.0) | ||
| Secondary tears | |||
| ≤16 y | 6 (35.3) | 11 (64.7) | 17 (12.1) |
| 17-25 y | 24 (48.0) | 26 (52.0) | 50 (35.5) |
| 26-35 y | 26 (83.9) | 5 (16.1) | 31 (22.0) |
| 36-45 y | 20 (66.7) | 10 (33.3) | 30 (21.3) |
| 46-55 y | 5 (50.0) | 5 (50.0) | 10 (7.1) |
| >55 y | 1 (33.3) | 2 (66.7) | 3 (2.1) |
| All | 141 (100.0) | ||
aValues are expressed as n (%).
The Wilcoxon test demonstrated that patient sex was not predictive of a second ACL injury (Z 1 = 0.0866; P = .7686). After excluding patients who experienced a contralateral second ACL tear, there was no significant influence of injured side (Z 1 = 1.5954; P = .2065), sex × left side (Z 1 = .1057; P = .7451), or sex × right side (Z 1 = 0.4586; P = .4983) on second ACL injury.
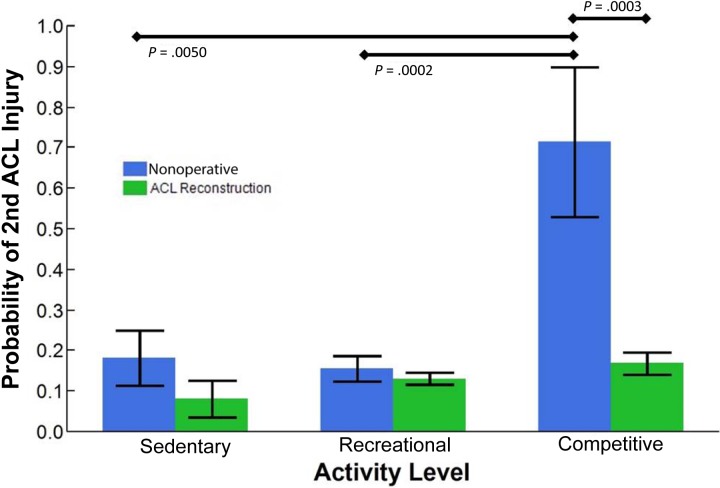
We stratified all patients into 6 age groups and assessed each according to the probability of a second ACL injury. Most primary and secondary ACL tears of both sexes occurred between the ages of 17 and 35 years (Table 2). In reference to second ACL injuries, female patients were more likely to sustain a second ACL tear compared to age-matched male patients except from ages 26 to 45 years (Table 2). Analysis of sex × age group demonstrated a significant predictive value for second injuries (P = .0101) for female patients aged 17 to 25 years (26/122 female patients [21.3%] and 24/216 male patients [11.1%] experienced a second ACL injury) and a predictive value that approached significance for male patients between the ages of 26 and 35 years (P = .0722). In addition, treatment type (ACLR or nonoperative therapy) × age group demonstrated a high predictive value for second ACL injuries in patients who underwent nonoperative therapy at younger ages: ≤16 years (P = .0060) and 17 to 25 years (P < .0001) (Figure 1). This analysis was performed constraining second injuries for nonoperative therapy only to the contralateral limb, as a second injury to the index limb was not possible.
Figure 1.
Probability of sustaining a second ACL injury by age group and treatment type. A value of 1 indicates a second ACL injury. From adolescence through age 25 years, nonoperative therapy significantly increased the probability of sustaining a second ACL injury. ACL, anterior cruciate ligament; ACLR, ACL reconstruction.
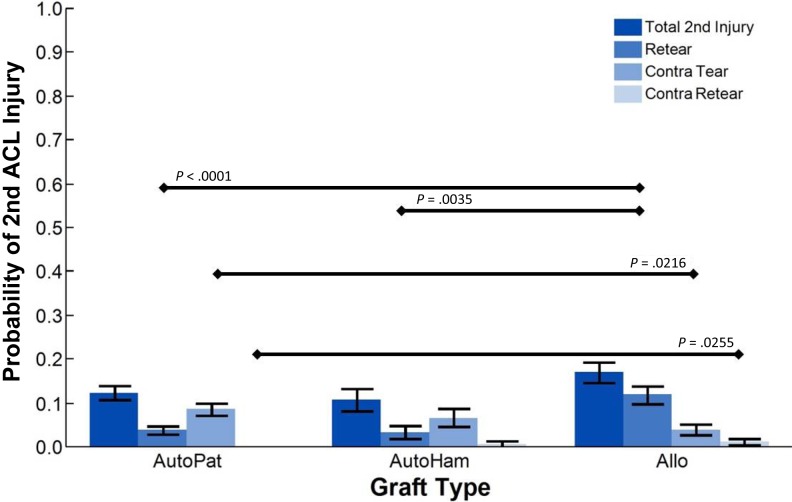
With regard to recorded activity levels and the resultant risk of second ACL injuries, most patients who suffered an ACL tear identified their activity level as recreational (66.0%), with 19.3% at the competitive and 6.9% at the sedentary levels (Table 1). An analysis of second injuries was carried out by activity level according to treatment group. This analysis revealed a significant effect for those who underwent nonoperative therapy with little modification of their activity level (Z 2 = 13.8248; P = .0010) with post hoc comparisons of competitive versus recreational (P = .0002) and competitive versus sedentary (P = .0050). In addition, nonoperative therapy at the competitive level significantly increased the risk of second injuries to those who underwent ACLR (Z 1 = 13.1207; P = .0003) (Figure 2). Overall, if ACLR was elected, allografts were most likely to fail, with a probability of 17.0% (Table 3). Hamstring autografts were 10.7% likely to suffer a second ACL tear, which differed from patellar tendon autografts at 12.4%.37
Figure 2.
Probability of sustaining a second ACL injury by activity level and treatment type. A value of 1 indicates a second ACL injury. Nonoperative therapy with continued participation in competitive-level sports significantly increased the probability of sustaining a second ACL injury. ACL, anterior cruciate ligament.
TABLE 3.
Statistical Analysis of Observed Epidemiological Factors for the Risk of Second ACL Injuriesa
| Factor | Mean | n | P |
|---|---|---|---|
| Sex | .7686 | ||
| Male | 0.1411 | 581 | |
| Female | 0.1347 | 438 | |
| Activity level | .2020 | ||
| Sedentary | 0.1286 | 70 | |
| Recreational | 0.1382 | 673 | |
| Competitive | 0.1878 | 197 | |
| Sex × sedentaryb | .8740 | ||
| Male | 0.1200 | 25 | |
| Female | 0.1333 | 45 | |
| Sex × recreationalb | .1050 | ||
| Male | 0.1546 | 427 | |
| Female | 0.1098 | 246 | |
| Sex × competitiveb | .0733 | ||
| Male | 0.1333 | 90 | |
| Female | 0.2336 | 107 | |
| Age | .4201 | ||
| <20 y | 0.1636 | 269 | |
| ≥20 y | 0.1429 | 672 | |
| Age group | .9201 | ||
| ≤16 y | 0.1339 | 127 | |
| 17-25 y | 0.1563 | 320 | |
| 26-35 y | 0.1403 | 221 | |
| 36-45 y | 0.1629 | 178 | |
| 46-55 y | 0.1250 | 80 | |
| >55 y | 0.2000 | 15 | |
| Age × sedentaryb | .7009 | ||
| ≤20 y | 0.0000 | 1 | |
| >20 y | 0.1304 | 69 | |
| Age × recreationalb | .9423 | ||
| ≤20 y | 0.1359 | 103 | |
| >20 y | 0.1386 | 570 | |
| Age × competitiveb | .6253 | ||
| ≤20 y | 0.1818 | 165 | |
| >20 y | 0.2188 | 32 | |
| Side of injuryb | .1860 | ||
| Left | 0.1519 | 540 | |
| Right | 0.1232 | 479 | |
| Sex × left sideb | .8903 | ||
| Male | 0.1654 | 272 | |
| Female | 0.1609 | 230 | |
| Sex × right sideb | .9244 | ||
| Male | 0.1333 | 270 | |
| Female | 0.1302 | 169 | |
| Sex × age ≤16 y | .7182 | ||
| Male | 0.1500 | 40 | |
| Female | 0.1264 | 87 | |
| Sex × age 17-25 y | .0101 | ||
| Male | 0.1171 | 205 | |
| Female | 0.2261 | 115 | |
| Sex × age 26-35 y | .0722 | ||
| Male | 0.1677 | 155 | |
| Female | 0.0758 | 66 | |
| Sex × age 36-45 y | .2693 | ||
| Male | 0.1900 | 100 | |
| Female | 0.1282 | 78 | |
| Sex × age 46-55 y | .6103 | ||
| Male | 0.1471 | 34 | |
| Female | 0.1087 | 46 | |
| Sex × age >55 y | .4533 | ||
| Male | 0.1250 | 8 | |
| Female | 0.2857 | 7 | |
| Treatment | .3571 | ||
| No ACLR | 0.1531 | 196 | |
| ACLR | 0.1349 | 823 | |
| Graft typeb | .1310 | ||
| Allograft | 0.1700 | 253 | |
| Hamstring autograft | 0.1074 | 149 | |
| Patellar tendon autograft | 0.1238 | 420 |
aA mean value that approximates 1 indicates an increased risk for second ACL injuries. ACL, anterior cruciate ligament; ACLR, ACL reconstruction. Bolded value represents statistical significance (P < .05). Italicized values represent a value that is approaching statistical significance.
bFor each category of analysis, the total n value may deviate from 1019, as unknown classifications were removed from analysis.
Contingency analyses were performed for graft type × age group and graft type × activity level. Graft type × age group (χ2 = 357.653; P < .0001) and graft type × activity level (χ2 = 117.565; P < .0001) both demonstrated significance and thus a correlation between the variables. A contingency analysis of activity level × age group (χ2 = 326.463; P < .0001) demonstrated that a correlation between these variables also existed.
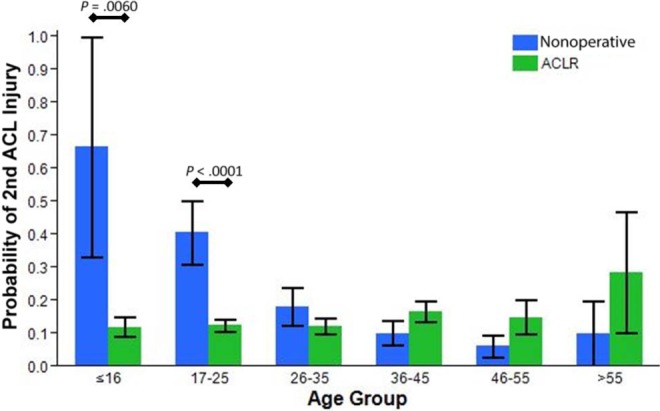
An analysis of the risk of second injuries by graft type (Z 2 = 4.0658; P = .1310) revealed trends toward significance, with an increased risk for allografts versus hamstring autografts (P = .0873) and patellar tendon autografts (P = .0961). Specifically, for the subset of graft ruptures (retears) that comprised second injuries (Z 2 = 20.0872; P < .0001), allografts carried a significantly greater risk of second injuries versus hamstring autografts (P = .0035) and patellar tendon autografts (P < .0001) (Figure 3). For the subset of contralateral tears (Z 2 = 5.3023; P = .0706), patellar tendon autografts demonstrated a significantly greater risk of second injuries than allografts (P = .0216). Finally, for the subset of contralateral retears (Z 2 = 4.7067; P = .0951) in which the patient experienced a third ACL injury, allografts demonstrated a significantly greater risk of second injuries than patellar tendon autografts (P = .0255; grafts that sustained a contralateral retear were 4 allografts and 1 patellar tendon autograft).
Figure 3.
Probability of sustaining a second anterior cruciate ligament (ACL) injury by graft type. A value of 1 indicates a second ACL injury. All allograft types were combined. Allo, allograft (hamstring or patellar tendon); AutoHam, hamstring autograft; AutoPat, patellar tendon autograft.
Graft type × age group demonstrated significance for predicting second injuries for age ≤16 years (Z 2 = 6.4321; P = .0401) and age 17 to 25 years (Z 2 = 17.1612; P = .0002). In the age group of ≤16 years, post hoc analysis revealed the significance of allografts versus hamstring autografts (P = .0093). In the age group of 17 to 25 years, post hoc analysis revealed the significance of allografts versus hamstring autografts (P = .0067) and patellar tendon autografts (P < .0001).
Discussion
This geographic cohort study provides valuable information with regard to the reported rate of second ACL injuries from a population of patients with acute-onset, isolated ACL tears. There were 76.4% of reported ACL tears that occurred from a noncontact mechanism, consistent with other reports.4,14 This dataset continues to provide unique insight to the current, published epidemiological literature with regard to second ACL injuries in that it provides a purely geographic analysis that is not exclusive to incidence based on a particular hospital, subscribers to a particular health insurance company, or a community-based registry, as has been reported previously in the literature.26,27,50 Thus, this dataset allows for improved generalizability of the epidemiological data to larger populations47 with minimal financial or social bias.
With the mean occurrence of ACL tears at 97.9 each year in this geographic cohort and the 2010 population of Olmsted County at 144,500, this equates to 67.8 ACL injuries per 100,000.40 This number correlates well with that reported previously from the National Hospital Discharge Survey28 and the reported 200,000 to 250,000 ACL injuries that occur in the United States,20,35 which would equate to 64.7 to 80.8 ACL injuries per 100,000. This correlation to other datasets demonstrates the inference that this dataset can have to other geographic locales within the United States. The overall incidence of second ACL tears in our cohort of 13.8% does not agree with a study with a high 30% second injury rate,21 but it does coincide with other previous reports.39,54 The general consensus in the literature seems to denote rates between 10% and 20%,36,39,43,54 whereas the report with the 30% second injury rate21 may have been caused by a sampling error with the small sample size.
Female sex by age in this cohort was predictive of a second ACL tear. Female patients aged ≤16 years were at a higher risk of second ACL injuries compared to their male counterparts (Table 2). However, the statistically significant age range for second ACL injuries was 17 to 25 years for female patients (P = .0101). In both sexes, the highest prevalence of second ACL injuries was between the ages of 17 and 25 years (Table 2). Based on the previous literature, the higher incidence of second injuries in young female patients may be based on unmodified risk factors that may have led to their primary ACL injury.10,16–18,30 Side of injury and sex × side of injury were not predictive of second ACL injuries. Sex × activity level demonstrated a trend toward significance for female athletes versus their male counterparts in competitive-level sports (P = .0733). This is important because of the increased participation of female athletes in competitive- and high-level sports worldwide. Although activity level alone was not a statistically significant factor for the risk of second ACL injuries in this report, it should be noted that competitive-level activity increased the risk by 36% compared to recreational activity. Combined, these 2 aspects of activity level indicate that return-to-play criteria should be an important aspect of clinical evaluations, especially for young female athletes.
Patients who were young and elected to not undergo surgical reconstruction were very likely to experience another ACL injury through age 25 years (Figure 1). This is likely because of the high level of activity in this age group, especially at the high school and college competitive level, as age and activity level were correlated. Additionally, the young athlete may not entirely understand the consequences of the primary ACL injury and the increased risk that is possible for a second injury after a primary injury.34
Graft type selection correlated with both age group and activity level. Both activity level and age group were correlated, meaning that as age increased, patients were less involved at the competitive level and engaged in more sedentary activity. As age increased, there was a higher selection of both nonoperative therapy and allografts. This is expected, as activity level and appropriate activity modification can largely determine whether patients will deem both the cost and therapeutic time of surgical intervention necessary to participate in their desired activities of daily living.
Of particular interest is the occurrence of second ACL injuries by graft type. The current data indicated that allografts had a higher failure rate than autografts (Table 3). Although we reported that patellar tendon autografts carried a higher risk of contralateral tears than allografts in the previous section, it should be acknowledged that the older population carried a bias toward allografts and had a lower activity level. Our current data could not clearly distinguish whether hamstring or patellar tendon autografts lowered the risk of second injuries. This dataset is heavily favored toward patellar tendon autografts, which predisposes more failures of patellar tendon autografts and thus may be biased to the incidence of these. However, similar to our previous report (1990-2000), allografts do carry higher failure rates than autografts. The overall probability of second injuries has decreased from our previous report (1990-2000) most likely because of improved surgical techniques with anatomic graft placement. Previous ACLRs were performed with a more “vertical” orientation to the reconstructed ligament. Modern techniques attempt to place the graft anatomically, placing the graft over the original footprint of the native ligament. Future epidemiological studies should continue to assess the outcomes of the various graft types and identify the optimal graft selection for improved patient outcomes.
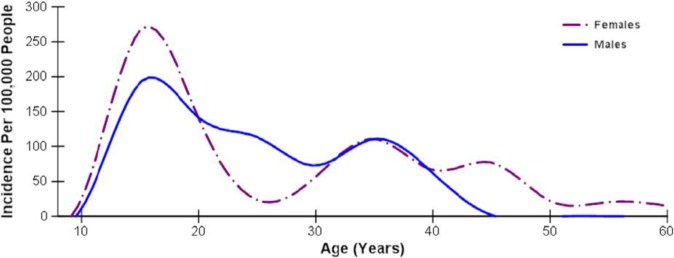
This current epidemiological report has many similarities and some differences to our previous epidemiological report on the incidence of second ACL injuries (1990-2000).41 Both decades of data demonstrated a higher incidence of age-specific second injuries in a biphasic fashion for young female patients (aged ≤16-25 years) and older female patients (aged 40-60 years) (Figure 4). During the decade of life between 20 and 30 years (Tables 2 and 3), male patients had a trend toward significance for a high incidence of second ACL injuries. Although this trend was noted, we speculate as to whether it occurs because of the life demands of female patients during this particular time frame (ie, pregnancy, work/family balance), which would modify their activity level and lead to a decrease in competitive-level athletics for female patients. These data are critical, as 2 decades of data demonstrate that the incidence of second ACL injuries is highest for young female athletes, who already also have a high risk of primary ACL injuries compared to their male counterparts.1,17 Even though male participation in sports continues to be higher than female participation, a recent survey demonstrated that the female athletic participation rate continue to increase at nearly double that of male athletic participation each decade.32 With increasingly more female athletes involved in competitive-level sports, our 2 reports lead to high concern for the medical, financial, and societal burden of second ACL injuries with the debilitating sequelae of multiple ACL injuries, which include early-onset osteoarthritis, quadriceps atrophy, decrease in an active lifestyle, and modification of activities of daily living.7
Figure 4.
Age-specific incidence of second anterior cruciate ligament injuries in male and female patients. Data fit with a sixth-order polynomial.
An important strength of this study is the use of a large geographically defined database, but the data are limited to Olmsted County in southeast Minnesota. We acknowledge that we had a 24.7% loss to follow-up and that these second injury rates are best-case estimates. Additional strengths of the study include the reporting of sex, age, and activity level; chart-based verification; determination of associated injuries; and ability to account for all care provided. It should also be noted that the data reported here are strictly based on athletic trends in the United States. Populations in other countries may have different incidences of second ACL injuries based on their unique exposure to high-risk sports involving cutting, pivoting, and rapid deceleration.
Future studies should continue to examine the trends of a second ACL injury over longer and more recent observation periods, as societal trends are likely to change. It is likely that the trends in ACL injuries will continue to change with improved surgical reconstruction techniques and rehabilitation protocols. We continue to promote research efforts that emphasize targeting prevention and outcome measures of high-risk groups, specifically activity modification, improved rehabilitation guidelines,8,15,31,42 and use of integrative neuromuscular training,8,29,42,49 to help athletes reduce the risk of second ACL injuries.8,52 Our future research plans are to continue these analyses of the REP epidemiological data for the years 2011 to 2016 and report the incidence of both primary and secondary ACL injuries in this new cohort of patients. In addition, we will report trends observed in the REP data that follow changes in the approach to ACLR and graft type selection.
Conclusion
This population-based cohort of 1019 ACL injuries identified a 13.8% incidence of second ACL tears over a 10-year period, half of which occurred to the contralateral knee. Statistically, female patients younger than age 25 years and male patients aged 26 to 45 years were most likely to suffer a second ACL tear than the opposite sex. Allografts were associated with a higher risk of second ACL injuries compared to autografts. Nonoperative treatment carried more risk of contralateral second injuries than ACLR.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: Funding for this research was received from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01AR056259 [T.E.H.] and K12HD065987 and L30AR070273 [N.D.S.]). This study was also made possible using the resources of the Rochester Epidemiology Project, which is supported by the National Institute on Aging of the National Institutes of Health under award No. R01AG034676.
Ethical approval for this study was obtained from the Olmsted Medical Center Institutional Review Board (study No. 026-OMC-14) and the Mayo Clinic Institutional Review Board (application No. 14-005089).
References
- 1. Allen MM, Pareek A, Krych AJ, et al. Are female soccer players at an increased risk of second anterior cruciate ligament injury compared with their athletic peers? Am J Sports Med. 2016;44(10):2492–2498. [DOI] [PubMed] [Google Scholar]
- 2. Ardern CL, Taylor NF, Feller JA, Webster KE. Fear of re-injury in people who have returned to sport following anterior cruciate ligament reconstruction surgery. J Sci Med Sport. 2012;15(6):488–495. [DOI] [PubMed] [Google Scholar]
- 3. Bates NA, McPherson AL, Rao MB, Myer GD, Hewett TE. Characteristics of inpatient anterior cruciate ligament reconstructions and concomitant injuries. Knee Surg Sports Traumatol Arthrosc. 2016;24(9):2778–2786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Boden B, Dean G, Feagin JJ, Garrett WJ. Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23(6):573–578. [DOI] [PubMed] [Google Scholar]
- 5. Borchers JR, Pedroza A, Kaeding C. Activity level and graft type as risk factors for anterior cruciate ligament graft failure: a case-control study. Am J Sports Med. 2009;37(12):2362–2367. [DOI] [PubMed] [Google Scholar]
- 6. Bozynski CC, Kuroki K, Stannard JP, et al. Evaluation of partial transection versus synovial debridement of the ACL as novel canine models for management of ACL injuries. J Knee Surg. 2015;28(5):404–410. [DOI] [PubMed] [Google Scholar]
- 7. Dare D, Rodeo S. Mechanisms of post-traumatic osteoarthritis after ACL injury. Curr Rheumatol Rep. 2014;16(10):1–5. [DOI] [PubMed] [Google Scholar]
- 8. Di Stasi S, Myer GD, Hewett TE. Neuromuscular training to target deficits associated with second anterior cruciate ligament injury. J Orthop Sport Phys Ther. 2013;43(11):777–792, A1–A11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dodwell E, LaMont L, Green D, Pan T, Marx R, Lyman S. 20 years of pediatric anterior cruciate ligament reconstruction in New York state. Am J Sports Med. 2014;42(3):675–680. [DOI] [PubMed] [Google Scholar]
- 10. Ford KR, Myer GD, Schmitt LC, Uhl TL, Hewett TE. Preferential quadriceps activation in female athletes with incremental increases in landing intensity. J Appl Biomech. 2011;27(3):215–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ford KR, Myer GD, Toms HE, Hewett TE. Gender differences in the kinematics of unanticipated cutting in young athletes. Med Sci Sports Exerc. 2005;37(1):124–129. [PubMed] [Google Scholar]
- 12. Freedman KB, Glasgow MT, Glasgow SG, Bernstein J. Anterior cruciate ligament injury and reconstruction among university students. Clin Orthop Relat Res. 1998;(356):208–212. [DOI] [PubMed] [Google Scholar]
- 13. Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med. 2010;363(4):331–342. [DOI] [PubMed] [Google Scholar]
- 14. Griffin LY, Agel J, Albohm MJ, et al. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2008;8:141–150. [DOI] [PubMed] [Google Scholar]
- 15. Hewett TE, Di Stasi SL, Myer GD. Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41(1):216–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hewett TE, Ford KR, Myer GD. Anterior cruciate ligament injuries in female athletes, part 2: a meta-analysis of neuromuscular interventions aimed at injury prevention. Am J Sports Med. 2006;34(3):490–498. [DOI] [PubMed] [Google Scholar]
- 17. Hewett TE, Myer GD, Ford KR. Anterior cruciate ligament injuries in female athletes, part 1: mechanisms and risk factors. Am J Sports Med. 2006;34(2):299–311. [DOI] [PubMed] [Google Scholar]
- 18. Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. [DOI] [PubMed] [Google Scholar]
- 19. Hewett TE, Myer GD, Ford KR, Paterno MV, Quatman CE. The 2012 ABJS Nicolas Andry Award. The sequence of prevention: a systematic approach to prevent anterior cruciate ligament injury. Clin Orthop Relat Res. 2012;470(10):2930–2940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hewett TE, Myer GD, Ford KR, Paterno MV, Quatman CE. Mechanisms, prediction, and prevention of ACL injuries: cut risk with three sharpened and validated tools. J Orthop Res. 2016;34(11):1843–1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hui C, Salmon LJ, Kok A, Maeno S, Linklater J, Pinczewski LA. Fifteen-year outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft for “isolated” anterior cruciate ligament tear. Am J Sports Med. 2011;39(1):89–98. [DOI] [PubMed] [Google Scholar]
- 22. Kaeding CC, Pedroza AD, Reinke EK, et al. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43(7):1583–1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kessler MA, Behrend H, Henz S, Stutz G, Rukavina A, Kuster MS. Function, osteoarthritis and activity after ACL-rupture: 11 years follow-up results of conservative versus reconstructive treatment. Knee Surg Sports Traumatol Arthrosc. 2008;16(5):442–448. [DOI] [PubMed] [Google Scholar]
- 24. Kvist J, Ek A, Sporrstedt K, Good L. Fear of re-injury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2005;13(5):393–397. [DOI] [PubMed] [Google Scholar]
- 25. Levy YD, Hasegawa A, Patil S, Koziol JA, Lotz MK, D’Lima DD. Histopathological changes in the human posterior cruciate ligament during aging and osteoarthritis: correlations with anterior cruciate ligament and cartilage changes. Ann Rheum Dis. 2013;72(2):271–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Maletis GB, Inacio MCS, Funahashi TT. Analysis of 16,192 anterior cruciate ligament reconstructions from a community-based registry. Am J Sports Med. 2013;41(9):2090–2098. [DOI] [PubMed] [Google Scholar]
- 27. Maletis GB, Inacio MCS, Funahashi TT. Risk factors associated with revision and contralateral anterior cruciate ligament reconstructions in the Kaiser Permanente ACLR registry. Am J Sports Med. 2015;43(3):641–647. [DOI] [PubMed] [Google Scholar]
- 28. Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42(10):2363–2370. [DOI] [PubMed] [Google Scholar]
- 29. Myer GD, Chu DA, Brent JL, Hewett TE. Trunk and hip control neuromuscular training for the prevention of knee joint injury. Clin Sport Med. 2008;27(3):425–448, ix. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Biomechanics laboratory-based prediction algorithm to identify female athletes with high knee loads that increase risk of ACL injury. Br J Sports Med. 2011;45(4):245–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Myer GD, Paterno MV, Ford KR, Quatman CE, Hewett TE. Rehabilitation after anterior cruciate ligament reconstruction: criteria-based progression through the return-to-sport phase. J Orthop Sports Phys Ther. 2006;36(6):385–402. [DOI] [PubMed] [Google Scholar]
- 32. National Federation of State High School Associations. 2015-16 High School Participation Survey. Indianapolis, Indiana: National Federation of State High School Associations; 2016. [Google Scholar]
- 33. Paterno MV, Kiefer AW, Bonnette S, et al. Prospectively identified deficits in sagittal plane hip-ankle coordination in female athletes who sustain a second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Clin Biomech. 2015;30(10):1094–1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med. 2012;22(2):116–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42(7):1567–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind M. Comparison of hamstring tendon and patellar tendon grafts in anterior cruciate ligament reconstruction in a nationwide population-based cohort study: results from the Danish registry of knee ligament reconstruction. Am J Sports Med. 2014;42(2):278–284. [DOI] [PubMed] [Google Scholar]
- 38. Rocca W, Yawn B, St Sauver J, Grossardt B, Melton L. History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012;87(12):1202–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21(8):948–957. [DOI] [PubMed] [Google Scholar]
- 40. Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med. 2016;44(6):1502–1507. [DOI] [PubMed] [Google Scholar]
- 41. Schilaty ND, Bates NA, Sanders TL, Krych AJ, Stuart MJ, Hewett TE. Incidence of second anterior cruciate ligament tears (1990-2000) and associate factors by geographic locale. Am J Sports Med. 2017;45(7):1567–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Schilaty ND, Nagelli CV, Hewett TE. Use of objective neurocognitive measures to assess the psychological states that influence return to sport following injury. Sport Med. 2015;46(3):299–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37(2):246–251. [DOI] [PubMed] [Google Scholar]
- 44. Snaebjörnsson T, Hamrin Senorski E, Sundemo D, et al. Adolescents and female patients are at increased risk for contralateral anterior cruciate ligament reconstruction: a cohort study from the Swedish national knee ligament register based on 17,682 patients [published online March 15, 2017]. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-017-4517-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Sri-Ram K, Salmon LJ, Pinczewski LA, Roe JP. The incidence of secondary pathology after anterior cruciate ligament rupture in 5086 patients requiring ligament reconstruction. Bone Joint J. 2013;95-B(1):59–64. [DOI] [PubMed] [Google Scholar]
- 46. St Sauver J, Grossardt B, Yawn B, et al. Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol. 2012;41(6):1614–1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. St Sauver J, Grossardt B, Yawn B, Melton L, Rocca W. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Am J Epidemiol. 2011;173(9):1059–1068.21430193 [Google Scholar]
- 48. St Sauver J, Grossardt B, Yawn B, Melton L, Rocca W. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester Epidemiolgoy Project. Am J Epidemiol. 2011;173(9):1059–1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Sugimoto D, Myer GD, Barber Foss KD, Hewett TE. Specific exercise effects of preventive neuromuscular training intervention on anterior cruciate ligament injury risk reduction in young females: meta-analysis and subgroup analysis. Br J Sports Med. 2015;49(5):282–289. [DOI] [PubMed] [Google Scholar]
- 50. Tejwani SG, Chen J, Funahashi TT, Love R, Maletis GB. Revision risk after allograft anterior cruciate ligament reconstruction: association with graft processing techniques, patient characteristics, and graft type. Am J Sports Med. 2015;43(11):2696–2705. [DOI] [PubMed] [Google Scholar]
- 51. Vaishya R, Agarwal AK, Ingole S, Vijay V. Current trends in anterior cruciate ligament reconstruction: a review. Cureus. 2015;7(11):e378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44(7):1861–1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Wright RW, Haas AK, Anderson J, et al. Anterior cruciate ligament reconstruction rehabilitation: MOON guidelines. Sports Health. 2014;7(3):239–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Wright RW, Magnussen RA, Dunn WR, Spindler KP. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction. J Bone Joint Surg Am. 2011;93(12):1159–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]