Abstract
Photovoice is a research method developed to help communities share images as a tool for discussion of key issues. Although this may be useful to promote healthy behavior, using Photovoice in adolescents has been logistically challenging. Given adolescents’ engagement in social media, our study explored the feasibility of using a photo-sharing mobile phone application, Instagram, to accomplish the principles of Photovoice. Twenty adolescents 14 to 18 years old with type 1 diabetes were asked to use Instagram to post any diabetes-related photo for 3 weeks. Individual interviews and a focus group were also offered, and recruitment and retention statistics were tracked. Of those approached (n = 47), 43% agreed to participate. Twelve were actively engaged. Shared photos were most likely to fall into the categories of diabetes care, humor, or food. Engaged participants universally reported the project to be a positive experience; however, there were technological and personal factors to consider for widespread implementation.
Keywords: photography / photovoice; diabetes, adolescents / youth, at risk; concept development; technology, use in research; qualitative; feasibility study; United States, Northwest
Photovoice is a participatory action research method developed to help communities of people use and share images as a means to reflect strengths and concerns and promote discussion of key issues (Wang, 1999; Wang & Burris, 1997). Our study seeks to examine the feasibility of combining Photovoice methodology with social media in adolescents with type 1 diabetes (T1D). Traditional Photovoice methodology includes providing disposable cameras to participants and asking them to photograph particular themes of a given topic. Participants then come together to discuss the photos. Using photography and group work to give people an opportunity to document and reflect on their daily experiences, Photovoice has been used in many diverse populations, including lower income/minority adults and youth, adults with mental illness, adolescents with chronic illness such as cancer, and in adults and youth with obesity (Kramer, Schwartz, Cheadle, & Rauzon, 2013; Necheles et al., 2007; Padgett, Smith, Derejko, Henwood, & Tiderington, 2013). Outcomes have included improved meaning-making, life satisfaction, and empowerment (Duffy, 2011; Thomas, Owens, Friedman, Torres, & Hébert, 2013; Yi & Zebrack, 2010).
Using photography in youth populations in general has shown to elicit perspectives relevant and specific to the child’s point of view on a variety of topics, including food experiences, and experiences with play and school (Alexander, Frohlich, & Fusco, 2014; Genuis, Willows, Alexander, & Jardine, 2014; Warne, Snyder, & Gillander Gådin, 2013). However, Photovoice projects conducted with adolescents have found working with youth to be difficult, taking more time and coordination than adults (Drew, Duncan, & Sawyer, 2010; Kramer et al., 2013; Strack, Magill, & McDonagh, 2004). Adolescents struggled with knowing what to photograph and with remembering their cameras (Drew et al., 2010). One logical evolution in making Photovoice successful with adolescents would be to engage them through their mobile phones, given their high engagement with technology and previous work suggesting that adolescents liked phone messages with images (Woolford, Clark, Strecher, & Resnicow, 2010). One intervention study of obese adolescents used modified Photovoice methods using photo texting through their mobile phone (Woolford et al., 2012). This study asked participants to use their mobile phone to text personal photos about topics related to weight loss or exercise to a research assistant. Participants reported high satisfaction of the process, and the authors concluded that a mobile intervention incorporating personal images would increase adherence to treatment. Given the wider range of Internet capabilities beyond text messaging now available through mobile phones, the aim of our study was to take the Woolford et al. findings one step further by asking participants to use a popular photo application linked to social media, Instagram, as a means to discuss health behavior. Instagram is a free, photo-sharing mobile phone application. Instagram has 300 million monthly active users, 70 million photo uploads per day, and garners 2.5 billion “likes” per day (Instagram.com/press). Nielson rankings cite Instagram as the top photography site among teens aged 12 to 17 (Meyers, 2012).
Social media is a cultural standard that engages up to 90% of 13- to 17-year-olds (Common Sense Media, 2012). Participants report a resulting positive impact on their emotional well-being, citing social networking makes them feel more outgoing, confident, and better about themselves (Common Sense Media, 2012). Emerging scientific research in this area has shown that self-representation on social media sites such as Facebook is overwhelmingly positive (Qiu, Lin, Leung, & Tov, 2012). These reports suggest that the use of directed social media may facilitate health promotion through mechanisms that may include increased social support, benefit-finding (meaning-making), or positive peer-modeling. The influence of social media in influencing adolescent health behavior fits nicely within the theoretical perspective of social learning theory, which states that individuals learn from observing, and modeling, each other’s behaviors, attitudes, and outcomes (Bandura, 1977, 1986, 1998). In modern culture, the observation of these behaviors, attitudes, and outcomes occurs in multiple ways, including live modeling and influence of the media (Trujillo, Suárez, Lema, & Londoño, 2015). Social networking sites have been shown to significantly affect health behavior across multiple age groups and health domains (Laranjo et al., 2015).
Thus, the goal of this study was to test the feasibility (defined as recruitment, retention, and satisfaction) of using Photovoice techniques through Instagram in a high-risk group of youth, adolescents with T1D, and to explore the types of photos shared in this setting. Because of the inherent sharing component of social media and the possibility that participants may be hesitant using Instagram for purposes related to their health condition, we intentionally designed this study to assess feasibility to determine whether future studies designed to promote positive health behaviors through modeling and sharing may be achievable using Instagram. Adolescents with T1D are a group facing elevated stress from a burdensome and challenging treatment plan to optimally control the disease, on top of the everyday challenges that any adolescent experiences. Individuals with T1D are expected to engage in a wide range of intensive daily behaviors, including blood sugar monitoring, taking the appropriate amount of insulin, and adhering to proper diet and exercise guidelines. It is well known that adolescents with T1D have high rates of poor glycemic control, putting them at increased risk for microvascular and macrovascular complications (Flack, Kaar, & Laatikainen, 1996; Paris et al., 2009). A national study reported only 32.4% of 13- to 18-year-olds with T1D were classified as having optimal glycemic control, as measured by glycated hemoglobin (A1C; Petitti et al., 2009). As the Diabetes Control and Complications Trial (DCCT) has shown, every 1% increase in A1C can increase risk for complications by 40% (Diabetes Control and Complications Trial Research Group, 1993). However, early glycemic control is particularly critical for long-term durability of benefits, including a significantly reduced risk for complications (White et al., 2010).
In addition to suboptimal A1C, research has documented high rates of depression, stress, and anxiety for adolescents with T1D (Birmaher et al., 1996; Di Battista, Hart, Greco, & Gloizer, 2009; Kanner, Hamrin, & Grey, 2003). Compared with nondiabetic youth, the prevalence of major depression is reportedly at least 2 to 3 times greater for T1D youth (Grey, Whittemore, & Tamborlane, 2002; Kovacs, Goldston, Obrosky, & Bonar, 1997). Depression and distress have been associated with worse glycemic control, more complications, higher health care costs, and increased frequency of adverse events (Herzer & Hood, 2010; Lawrence et al., 2006; Leichter & See, 2005; Yi, Yi, Vitaliano, & Weinger, 2008). The high rates of distress and depression coupled with poor outcomes in adolescents with T1D are of legitimate public health concern. Age-specific preventive interventions are desperately needed to address this dangerous downward spiral, and efforts are needed to find age-appropriate means to promote health in this population.
To our knowledge, this is the first instance of using Instagram as an application of Photovoice, and in fact, using photo-based methodology in the diabetes population is novel, with only two studies found, both in older adults with type 2 diabetes (Fritz, 2014; Yankeelov, Faul, D’Ambrosio, Collins, & Gordon, 2015). Thus, our primary aim was to assess feasibility markers for the proposed intervention platform. Feasibility was defined as rates of recruitment and retention and satisfaction for using Instagram for diabetes-related topics. In addition, we would examine and categorize the type of diabetes-related photos that would be shared.
Method
Participants
Eligible participants were adolescents aged 14 to 18 with a diagnosis of T1D for 6 months or longer, English-speaking, with personal access to Instagram on an Android (v. 2.2 or above) or Apple iOS device (v.4.2.1 or above) with a camera attached. Recruitment was purposive, such that patients with upcoming clinic appointments at a large tertiary care hospital were contacted by mail, phone, or in-person about the study. The Institutional Review Board approved the protocol, and voluntary written informed consent was obtained from each participant and his or her caregiver (for those <18). A total of 20 patients agreed to participate in the study.
De-identified information was collected on all patients approached. Race/ethnicity, sex, age, insurance status, and any reasons they gave for not enrolling were tracked for those who declined the study.
Study Protocol
Basic training
After consenting, prior Instagram experience was assessed. All participants received basic training with Instagram as needed either in-person or by phone. Participants who were not familiar with Instagram were asked to download the application on their mobile device and instructed on how to set up an account. Prior Instagram users were given the option of using their current accounts or setting up a new account for the project. Privacy settings were carefully reviewed but not specified; personal preference regarding keeping their account public or private was honored.
Creating the photo feed
Participants were asked to post photos to their Instagram feed that “represented anything about their diabetes.” The protocol was intentionally left wide open so that we could evaluate the types of themes that emerged. Data were collected as to how many photos were posted each week. Participants were given an incentive of US$10 per week for each week that a minimum of three photos were posted. They were asked to maintain this participation for 3 consecutive weeks.
Use of hashtags
The purpose of a hashtag is to make it possible to group messages or photos within social network sites such as Instagram or Twitter by a particular hashtag phrase. Participants were encouraged to caption their photo and use the hashtag “#diabetesteenproject” as a descriptor, but the hashtag was not required. As hashtags are searchable and publicly viewable from all public accounts, this function of Instagram allows for a collection of public photos resulting from this project to be maintained. The number of hashtags used and whether the #diabetesteenproject hashtag was searched were tracked.
Follow-up individual interview and focus group
After the 3 weeks of the Instagram feed were complete, participants were interviewed individually for qualitative assessments of themes and experiences. They were also invited to a focus group where photos were printed and discussed. Both the individual and group discussions centered around the content of the photos, using traditional Photovoice techniques including the SHOWeD method of interviewing (Wang, 1999). The SHOWeD method focuses on five questions: (a) what do you See here, (b) what is Happening here, (c) how does this relate to Our lives, (d) Why does this issue exist, and (e) what can we Do about it (Wang, 1999). Photovoice methods including pile-sorting photos for development of themes, and participant ranking of photos for more in-depth discussions were also used (Wang, 1999). General satisfaction and suggestions were also ascertained.
Data Analyses
Demographic variables between enrollees and decliners and engaged and nonengaged participants were compared using independent-samples t tests or chi-square tests. Photovoice methodology was used to codify the issues, themes, or theories that arose from the photographs through pile-sorting or discussion of favorite photos. Staff members categorized the photos by independently evaluating all photos and self-identifying the single overall, prominent theme they believed each photograph depicted. Because of the feasibility and exploratory nature of the study, no predetermined themes were given. Intraclass correlation among the four raters was calculated using SPSS v.19. Qualitative analyses were conducted for the categorization of photos and for satisfaction of using Instagram for this purpose.
Results
Feasibility
Recruitment and enrollment
Twenty patients enrolled out of a total of 47 who were approached (43%). Demographic information of those who agreed and declined is presented in Table 1. No differences on any demographic variable was evident between the two groups (all ps = ns). Common reasons for declining included not being interested in Instagram or social media in general, not having the proper mobile phone, or being too busy (Table 2).
Table 1.
Demographic Information for Patients Who Enrolled Versus Declined.
| Enrolled (n = 20) |
Declined (n = 27) |
|
|---|---|---|
| Age | 16.4 ± 1.6 | 16.0 ± 1.6 |
| Sex (% female) | 65% | 60% |
| Years diagnosed | 5.5 ± 4.2 | 6.2 ± 3.7 |
| Race (% White) | 65% | 85% |
| Ethnicity (% non-Hispanic White) | 90% | 82% |
| Insurance (% commercial/private) | 65% | 69% |
| Baseline A1C | 9.2 ± 2.5 | 8.8 ± 1.8 |
Table 2.
Reasons Given for Declining Study (n = 27).
| n | |
|---|---|
| Not interested in Instagram/social media, too private to share on social media | 9 |
| Did not have the proper mobile phone to participate | 8 |
| Too busy | 6 |
| Not interested in discussing diabetes in this way | 3 |
| Parental privacy concerns | 1 |
For those who enrolled, 16 (89%) were previous Instagram users. Of these, 81% reported using Instagram for 1 year or more, 64% reported posting to Instagram at least once a week, and 50% reported checking Instagram multiple times a day. Half of the previous Instagram users chose to create a separate Instagram account for the project, and 65% chose to keep their account public.
Retention
Of the 20 enrolled, 12 were considered active participants (“engaged”) and 8 were not (“disengaged”), having never posted a diabetes-related photo despite three reminders and/or contact attempts. Engaged participants posted an average of 11.33 photos over 3 weeks. Table 3 shows the number of posts per week, the number of hashtags used among the photos posted, and the number of participants who were able to post 3 times per week.
Table 3.
Study Protocol Statistics, by Week.
| Total No. of Photos Posted |
No. of Diabetesteenproject Hashtags Used (% of Total Photos Posted) |
No. of Participants Who Posted 3 Photos Each Week (% of 12 Engaged Participants) |
|
|---|---|---|---|
| Week 1 | 56 | 46 (82) | 11 (92) |
| Week 2 | 44 | 40 (91) | 12 (100) |
| Week 3 | 36 | 33 (92) | 11 (92) |
Of those disengaged, two were active on Instagram for other personal photos but chose not to post diabetes-related photos. Some reported being too busy or changing their mind (n = 1 for both). Others were lost to follow-up. No differences were found between engaged and disengaged groups on demographic variables.
Thematic Analyses
Categorization by study staff
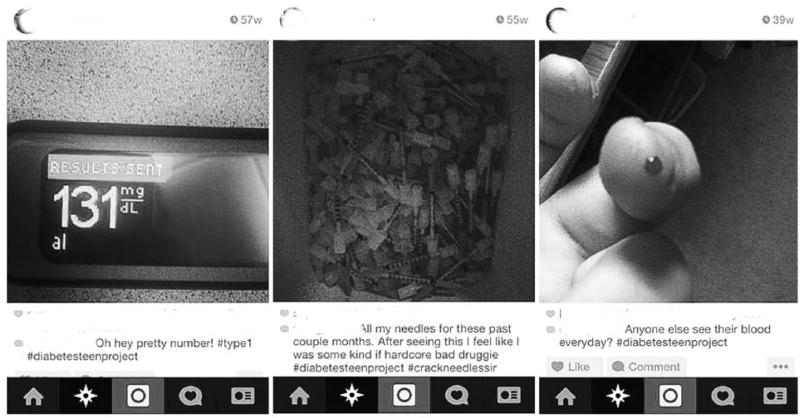
Four study staff independently sorted the compilation of Week 1 photos (57 photos total). Interrater reliability was determined by calculating the intraclass correlation, which was .56, indicating moderate agreement (Landis & Koch, 1977). Of these, 33% were photos that participants took themselves and 67% were “Internet memes” which are pictures with catchphrases or concepts that circulate via the Internet. Each research staff member was asked to sort all the photos into whatever themes they believed summarized the photo; no predetermined categories were given. Five main categories emerged: diabetes care, humor, food, exercise/sports, and life with diabetes. Each staff person cited the top three most frequent categories as being diabetes care, humor, and food. Photographs that were categorized as “diabetes care” included photos that showed how participants took care of themselves using diabetes self-care tools and supplies (Figure 1). There were many photos that showed values from glucose meters, and tools used for self-management, including needles, insulin pumps and pens, and logbooks. These pictures were often accompanied by captions reporting their emotions surrounding the photo, such as “Perfect BG reading” describing a blood glucose meter reading with a value of 125. Given the number of photos posted about this topic, this category seemed to reveal just how salient their diabetes-related equipment was to their daily lives, and how happy (or disappointed/surprised) they were with optimal (or low/high) numbers.
Figure 1.
Example photos and captions from “diabetes care” category, as posted on Instagram.
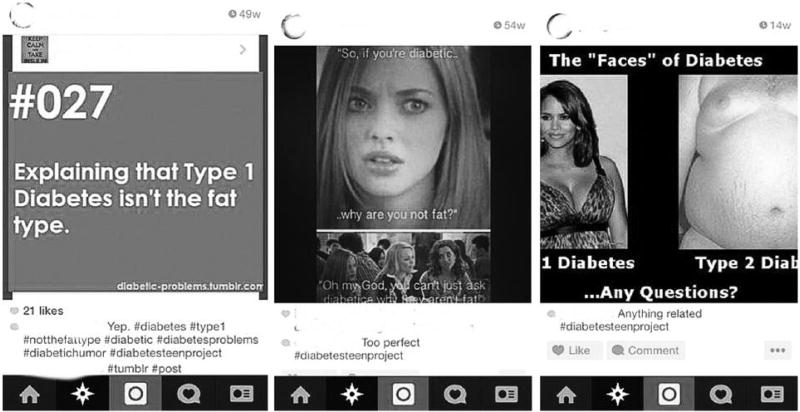
The category “humor” was a robust category with jokes and “Internet memes” (Figure 2). These posts often included funny photos with diabetes-related captions, puns about their diabetes (i.e., “Man I hate dull needles.” “Yeah they’re pointless.”), or a humorous literal perspective about diabetes (i.e., “I’ve got a needle and I’m not afraid to use it”). This category seemed to reveal how adolescents used humor as a coping mechanism for their disease. The humor touched many aspects of their diabetes management, including needles, being “high,” and explaining diabetes to their peers.
Figure 2.
Example photos and captions from “humor” category, as posted on Instagram.
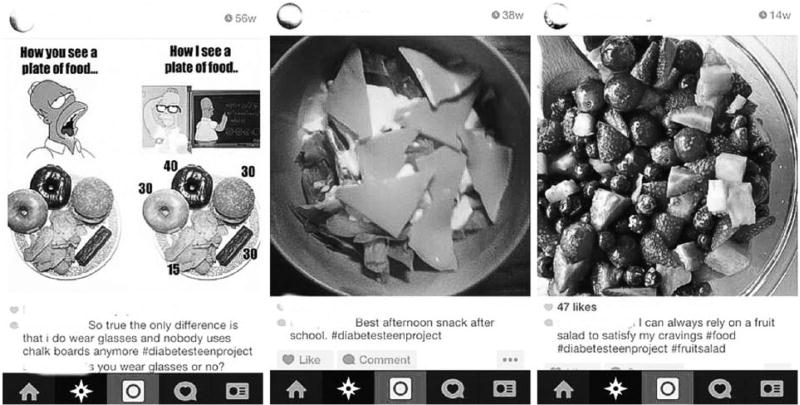
The photos under the category “food” showed many different types of food eaten in various situations relevant to diabetes management (Figure 3). There were many photos of foods eaten to correct low blood sugars (i.e., favorite candies and juice), and participants also shared photos of meals or snacks that were healthy and/or kept their glucose levels stable (i.e., salad with cheese and peanut butter and banana toast). Some participants shared photos of foods they liked to eat to keep unhealthy cravings at bay (i.e., picture of fruit salad, or a picture of a burger made of turkey with a whole wheat bun instead of the typical cheeseburger). Clearly finding healthy foods that were appealing to them was important, as was understanding how certain foods affected their blood glucose levels.
Figure 3.
Example photos and captions from “food” category, as posted on Instagram.
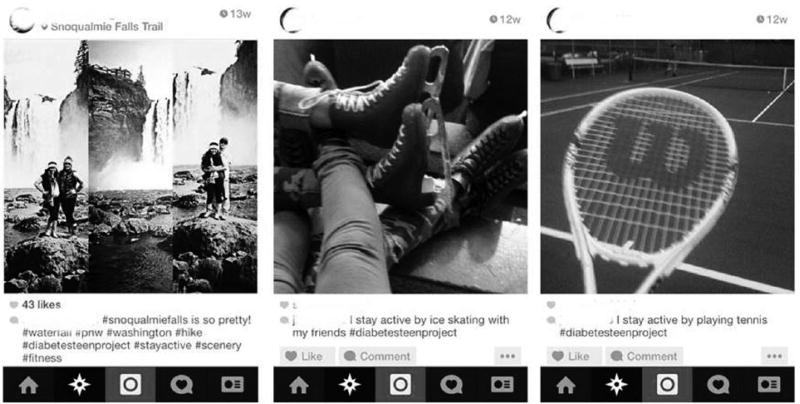
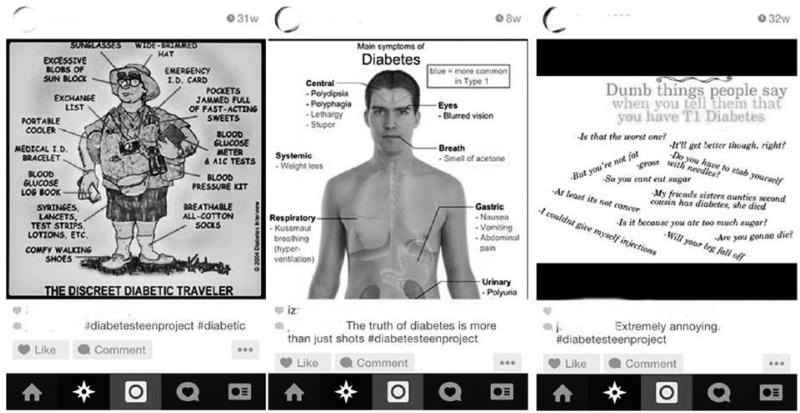
“Exercise/sports” depicted the types of activities that participants did to stay active and included pictures of themselves or others engaging in these activities (such as hiking or jumping) or pictures of related equipment used to be active (i.e., tennis racket; Figure 4). The final category, “Life with diabetes,” was also described as “the truth about diabetes” among coders (Figure 5). This was another diverse category with photos that were mainly used to describe common diabetes moments, such as an Internet meme stating “Going low during your tests and your professors not understanding.” There were also memes explaining what diabetes actually was, and posts describing the difference between T1D and type 2 diabetes were also placed in this category.
Figure 4.
Example photos and captions from “exercise/sports” category, as posted on Instagram.
Figure 5.
Example photos and captions from “life with diabetes” category, as posted on Instagram.
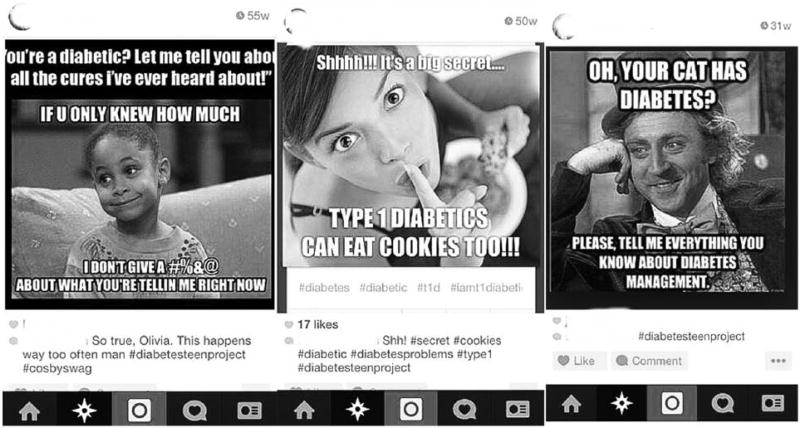
Individual interviews
Study staff conducted individual interviews with 10 enrolled participants. Overarching themes of the photos from the perspective of these participants were in agreement with the staff coding: humor, diabetes care, and food. An additional extension of the above themes coded by study staff members included specifically identifying photos that distinguished between type 1 and type 2 (Figure 6), and photos that summarized how they explained diabetes to people who do not have diabetes (Figure 7). Almost all the participants interviewed expressed ongoing frustration in those two categories, often leading to posting about those topics. Beyond these two additional categories, each participant’s themes coherently fit in all previously identified categories and the data were saturated. In the individual interviews, 21 specific photos were discussed. Of these photos, 14 were categorized as “positive,” 3 as “negative,” and 4 as “neutral,” with neither negative nor positive connotation. When asked what types of photos they liked best, the humor category had the most endorsements.
Figure 6.
Example photos and captions from “type 1 vs. type 2” category, as posted on Instagram.
Figure 7.
Example photos and captions from “talking with others who don’t have diabetes” category, as posted on Instagram.
Participants found the project to be universally positive. Suggestions included being assigned into a group or being given access to more Instagram users with diabetes so they could see what other diabetes teens were posting. Although our protocol asked participants to hashtag their photos, we did not explicitly ask participants to search the #diabetesteenproject hashtag to see what others posted. However, this was done by a majority of the interviewed participants. On occasion, participants “liked” or commented on a photo they discovered. As one participant stated,
After a couple of times of posting I started searching what other people posted and it gave me a feeling like I’m not the only one who has to do this (manage diabetes), other people can relate. It showed that not everyone is happy with their diabetes and it’s fine.
All participants reported it being easy to remember to post and hashtag the photos over the course of the 3 weeks.
Focus group
The focus group was held in a 1 hour session on a weekday evening facilitated by study staff. The focus group was intended to mirror the Photovoice model and discuss the photos in an in-person, group setting. Five participants attended. Participants’ pile-sort resulted in six categories: funny, negative, encouraging, how you see your diabetes, how others see your diabetes, and other. Feedback quotes included stating that it was “fun to discuss diabetes” using Instagram, that they liked using Instagram because it was “fast, simple, and faceless”; “it’s nice to know others are out there”; and that using Instagram in this way is a “good way to get people together and see something in a different way.” The focus group participants universally agreed that the focus group itself was also a positive addition to the project, and that by putting a face to an Instagram account, they would be more likely to feel comfortable posting.
Discussion
The purpose of this study was to establish feasibility of using Instagram for the sharing of diabetes-related photos among adolescents with T1D to determine its candidacy and appeal for use in future interventions targeting health behaviors in this population. We believe this extension of traditional Photovoice methodology to be promising for adolescents with chronic diseases such as diabetes. Those who engaged in the protocol were active for the duration of the 3-week period. Feedback about use was universally positive for those participants who engaged. Although the goal of this study was feasibility and not to elicit active social networking with other Instagram members, the majority of participants sought this out through searching of the #diabetesteenproject hashtag, some of whom even commented on or “liked” these photos. Individual interviews and the focus group confirmed that interacting with other teens with diabetes was clearly desired. Interestingly, all those who participated in the focus group stated that they felt the in-person piece was important and valuable, despite reporting not feeling that way before the group took place.
Thus, despite Instagram being an easy-to-access mobile application, we believe the in-person component to be a critical one, both in keeping true to the Photovoice methodology and also in helping participants feel more comfortable posting photos they personally take themselves. Surprisingly, only 33% of the collection of photos posted in this study were taken by themselves. The majority were “Internet memes,” or a generic photo with caption, used to more generally describe an aspect of their diabetes. This was one unexpected finding that we believe might change if participants knew more about their audience.
The topics of photos posted most frequently were diabetes care photos, such as meter readings or logbooks, food, or humor-related photos. The humor category was a vibrant one and seemed to help the adolescent participants relate to each other in their own way, as confirmed in the interviews and focus groups, where participants cited humor photos as ones they enjoyed most. The topics of the photos were most often “positive,” which confirms research in social media stating that self-disclosure is most often positive (Qiu et al., 2012). This is promising for future research that may look to use this methodology to promote positive health behaviors through modeling or sharing.
The topics that emerged, particularly diabetes care, food, and exercise, are important points of potential intervention for behavioral health change. Future studies should move beyond feasibility and explore the efficacy of using this medium to change behavior, particularly for these categories. Humor seemed to be a prominent coping strategy and could be used to address the negative feelings that often emerge in adolescents with T1D, such as burnout, depression, anxiety, or feelings of isolation (Birmaher et al., 1996; Di Battista et al., 2009; Kanner et al., 2003; Lowes et al., 2015).
Despite these important findings, it was clear that this intervention was not for everyone, and care should be taken in terms of selecting who might benefit most from this type of program. For one, we found our recruitment rate to be moderate at 43%. Many of the reasons for declining focused on being a private person, or not wanting to share about diabetes using social media. These are legitimate concerns and extra effort should be taken to ensure that the participant is comfortable with this medium. We also had 8 out of 20 participants who enrolled but did not participate. In many of these cases, the adolescent was a bit hesitant at the time of consent. Our study team realized this issue early on, when 6 of the first 9 consented participants failed to engage. We began to spend more time during the explanation and study consent process to better clarify the demands of the protocol and address any privacy issues that may arise by participating. By doing this, study staff were able to better identify patients who were truly interested in using Instagram for this purpose. Thus, a limitation of this type of project is its widespread acceptability. Interventions using Instagram would clearly be tailored to an individual more open and receptive to using social media for health-related topics. Also, 8 out of the 27 decliners (30%) were unable to participate because they did not own the proper type of mobile device. Although we did not find differences between enrollers and decliners on demographic variables including insurance type which was used as a proxy for socioeconomic status, it should be considered that those who do have the proper equipment to participate may have a different socioeconomic or family profile than those who do not. Our study did not have sufficient diversity to address potential differences by racial, ethnic, or socioeconomic groups.
Conclusion
To our knowledge, this was the first study using Instagram to share diabetes-related photos among youth with T1D. This modification of Photovoice was desirable in that using Instagram instead of a separate camera or even in place of mobile text messaging made it easy for those engaged in Instagram to remember to participate, took place in a medium that adolescents are used to participating in, and allowed for sharing of photos using the common hashtag, making it easy and possible to see what others were posting. Limitations of this modification include the potential inequality of participation based on mobile phone availability and the personal preference of the individual for using social media for sharing health-related information.
Future studies are needed to explore the efficacy of using Instagram for an intervention to improve outcomes such as self-care behaviors in youth with chronic illness. Integration of a social network will be a critical component in determining whether interest and engagement improve. Promoting and sustaining positive health behaviors can be difficult, particularly for adolescents with chronic disease. Exploring novel efforts such as this one, directed more specifically to where many adolescents naturally interact, is needed to improve outcomes for those most at risk.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was supported in part by NIH CTSA Grant UL1 TR00423 of the University of Washington (UW), Institute of Translational Health Science (ITHS). Other support was granted from the Department of Endocrinology funds, Seattle Children’s Hospital.
Biographies
Joyce P. Yi-Frazier, PhD, is a research assistant professor at the University of Washington School of Medicine, Department of Pediatrics and the Seattle Children’s Research Institute in Seattle, WA, USA.
Katherine Cochrane, BS, is a clinical research associate at the Seattle Children’s Research Institute, Center for Clinical and Translational Research, in Seattle, WA, USA.
Connor Mitrovich, BA, is a clinical research associate at the Seattle Children’s Research Institute, Center for Clinical and Translational Research, in Seattle, WA, USA.
Michael Pascual, BA, is a clinical research associate at the Seattle Children’s Research Institute, Center for Clinical and Translational Research, in Seattle, WA, USA.
Emil Buscaino, BS, was a clinical research associate at the Seattle Children’s Research Institute, Center for Clinical and Translational Research, in Seattle, WA, USA.
Lauren Eaton, MA, is a clinical research associate at the Seattle Children’s Research Institute, Center for Clinical and Translational Research, in Seattle, WA, USA.
Neil Panlasigui, is an undergraduate research student at the University of Washington, doing his research course at the Seattle Children’s Research Institute, Center for Clinical and Translational Research, in Seattle, WA, USA.
Bailey Clopp, is an undergraduate research student at the University of Washington, doing her research course at the Seattle Children’s Research Institute, Center for Clinical and Translational Research, in Seattle, WA, USA.
Faisal Malik, MD, is a dual pediatric endocrinology and quality of care research fellow at the University of Washington and Seattle Children’s Hospital in Seattle, WA, USA.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Alexander SA, Frohlich KL, Fusco C. Problematizing “play-for-health” discourses through children’s photo-elicited narratives. Qualitative Health Research. 2014;24:1329–1341. doi: 10.1177/1049732314546753. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social learning theory. Englewood Cliffs, NJ: Prentice Hall; 1977. [Google Scholar]
- Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- Bandura A. Health promotion from the perspective of social cognitive theory. Psychology & Health. 1998;13:623–649. [Google Scholar]
- Birmaher B, Ryan ND, Williamson DE, Brent DA, Kaufman J, Dahl RE, Nelson B. Childhood and adolescent depression: A review of the past 10 years. Part I. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35:1427–1439. doi: 10.1097/00004583-199611000-00011. [DOI] [PubMed] [Google Scholar]
- Common Sense Media. Social media, social life: How teens view their digital lives. 2012 Retrieved from http://www.commonsensemedia.org/sites/default/files/research/social-mediasociallife-final-061812.pdf.
- Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. New England Journal of Medicine. 1993;329:977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- Di Battista AM, Hart TA, Greco L, Gloizer J. Type 1 diabetes among adolescents: Reduced diabetes self-care caused by social fear and fear of hypoglycemia. The Diabetes Educator. 2009;35:465–475. doi: 10.1177/0145721709333492. [DOI] [PubMed] [Google Scholar]
- Drew SE, Duncan RE, Sawyer SM. Visual storytelling: A beneficial but challenging method for health research with young people. Qualitative Health Research. 2010;20:1677–1688. doi: 10.1177/1049732310377455. [DOI] [PubMed] [Google Scholar]
- Duffy L. “Step-by-step we are stronger”: Women’s empowerment through photovoice. Journal of Community Health Nursing. 2011;28:105–116. doi: 10.1080/07370016.2011.564070. [DOI] [PubMed] [Google Scholar]
- Flack A, Kaar ML, Laatikainen L. A prospective, longitudinal study examining the development of retinopathy in children with diabetes. Acta Paediatrica. 1996;85:313–319. doi: 10.1111/j.1651-2227.1996.tb14023.x. [DOI] [PubMed] [Google Scholar]
- Fritz HA. Learning to do better: The transactional model of diabetes self-management integration. Qualitative Health Research. 2014 doi: 10.1177/1049732314552453. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genuis SK, Willows N, Alexander FN, Jardine C. Through the lens of our cameras: Children’s lived experience with food security in a Canadian Indigenous community. Child: Care Health and Development. 2014 doi: 10.1111/cch.12182. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Grey M, Whittemore R, Tamborlane W. Depression in type 1 diabetes in children: Natural history and correlates. Journal of Psychosomatic Research. 2002;53:907–911. doi: 10.1016/s0022-3999(02)00312-4. [DOI] [PubMed] [Google Scholar]
- Herzer M, Hood KK. Anxiety symptoms in adolescents with type 1 diabetes: Association with blood glucose monitoring and glycemic control. Journal of Pediatric Psychology. 2010;35:415–425. doi: 10.1093/jpepsy/jsp063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanner S, Hamrin V, Grey M. Depression in adolescents with diabetes. Journal of Child and Adolescent Psychiatric Nursing. 2003;16:15–24. doi: 10.1111/j.1744-6171.2003.tb00342.x. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Goldston D, Obrosky DS, Bonar LK. Psychiatric disorders in youths with IDDM: Rates and risk factors. Diabetes Care. 1997;20:36–44. doi: 10.2337/diacare.20.1.36. [DOI] [PubMed] [Google Scholar]
- Kramer L, Schwartz P, Cheadle A, Rauzon S. Using photovoice as a participatory evaluation tool in Kaiser Permanente’s Community Health Initiative. Health Promotion Practice. 2013;14:686–694. doi: 10.1177/1524839912463232. [DOI] [PubMed] [Google Scholar]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- Laranjo L, Arguel A, Neves AL, Gallagher AM, Kaplan R, Mortimer N, Lau AY. The influence of social networking sites on health behavior change: A systematic review and meta-analysis. Journal of American Medical Informatics Association. 2015;22:243–256. doi: 10.1136/amiajnl-2014-002841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence JM, Standiford DA, Loots B, Klingensmith GJ, Williams DE, Ruggiero A SEARCH for Diabetes in Youth Study. Prevalence and correlates of depressed mood among youth with diabetes: The SEARCH for Diabetes in Youth study. Pediatrics. 2006;117:1348–1358. doi: 10.1542/peds.2005-1398. [DOI] [PubMed] [Google Scholar]
- Leichter SB, See Y. Problems that extend visit time and cost in diabetes care: 1. How depression may affect the efficacy and cost of care of diabetic patients. Clinical Diabetes. 2005;23:53–54. [Google Scholar]
- Lowes L, Eddy D, Channon S, McNamara R, Robling M, Gregory JW DEPICTED Study Team. The experience of living with type 1 diabetes and attending clinic from the perception of children, adolescents and carers: Analysis of qualitative data from the DEPICTED study. Journal of Pediatric Nursing. 2015;30:54–62. doi: 10.1016/j.pedn.2014.09.006. [DOI] [PubMed] [Google Scholar]
- Meyers M. How Instagram became the social network for tweens. 2012 Retrieved from news.cnet.com/8301-1023_3-57508430-93/how-instagram-became-the-social-network-for-tweens/
- Necheles JW, Chung EQ, Hawes-Dawson J, Ryan GW, Williams SB, Holmes HN, Schuster MA. The Teen Photovoice Project: A pilot study to promote health through advocacy. Progress in Community Health Partnerships: Research, Education, and Action. 2007;1:221–229. doi: 10.1353/cpr.2007.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padgett DK, Smith BT, Derejko KS, Henwood BF, Tiderington E. A picture is worth … ? Photo elicitation interviewing with formerly homeless adults. Qualitative Health Research. 2013;23:1435–1444. doi: 10.1177/1049732313507752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paris CA, Imperatore G, Klingensmith GJ, Petitti DB, Rodriguez B, Anderson AM, Pihoker C. Predictors of insulin regimens and impact on outcomes in youth with type 1 diabetes: The SEARCH for Diabetes in Youth study. Journal of Pediatrics. 2009;155:183–189. doi: 10.1016/j.jpeds.2009.01.063. [DOI] [PubMed] [Google Scholar]
- Petitti DB, Klingensmith GJ, Bell RA, Andrews JS, Dabelea D, Imperatore G, Mayer-Davis E. Glycemic control in youth with diabetes: The SEARCH for diabetes in Youth study. Journal of Pediatrics. 2009;155:668–672. doi: 10.1016/j.jpeds.2009.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu L, Lin H, Leung AK, Tov W. Putting their best foot forward: Emotional disclosure on Facebook. Cyberpsychology, Behavior, and Social Networking. 2012;15:569–572. doi: 10.1089/cyber.2012.0200. [DOI] [PubMed] [Google Scholar]
- Strack RW, Magill C, McDonagh K. Engaging youth through photovoice. Health Promotion Practice. 2004;5:49–58. doi: 10.1177/1524839903258015. [DOI] [PubMed] [Google Scholar]
- Thomas TL, Owens OL, Friedman DB, Torres ME, Hébert JR. Written and spoken narratives about health and cancer decision making: A novel application of photovoice. Health Promotion Practice. 2013;14:833–840. doi: 10.1177/1524839912465749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trujillo EM, Suárez DE, Lema M, Londoño A. How adolescents learn about risk perception and behavior in regards to alcohol use in light of social learning theory: A qualitative study in Bogotá, Colombia. International Journal of Adolescent Medicine and Health. 2015;27:3–9. doi: 10.1515/ijamh-2014-0003. [DOI] [PubMed] [Google Scholar]
- Wang CC. Photovoice: A participatory action research strategy applied to women’s health. Journal of Women’s Health. 1999;8:185–192. doi: 10.1089/jwh.1999.8.185. [DOI] [PubMed] [Google Scholar]
- Wang CC, Burris MA. Photovoice: Concept, methodology, and use for participatory needs assessment. Health Education & Behavior. 1997;24:369–387. doi: 10.1177/109019819702400309. [DOI] [PubMed] [Google Scholar]
- Warne M, Snyder K, Gillander Gådin K. Promoting an equal and healthy environment: Swedish students’ views of daily life at school. Qualitative Health Research. 2013;23:1354–1368. doi: 10.1177/1049732313505914. [DOI] [PubMed] [Google Scholar]
- White NH, Sun W, Cleary PA, Tamborlane WV, Danis RP, Hainsworth DP DCCT-EDIC Research Group. Effect of prior intensive therapy in type 1 diabetes on 10-year progression of retinopathy in the DCCT/EDIC: Comparison of adults and adolescents. Diabetes. 2010;59:1244–1253. doi: 10.2337/db09-1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolford SJ, Clark SJ, Strecher VJ, Resnicow K. Tailored mobile phone text messages as an adjunct to obesity treatment for adolescents. Journal of Telemedicine and Telecare. 2010;16:458–461. doi: 10.1258/jtt.2010.100207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolford SJ, Khan S, Barr KL, Clark SJ, Strecher VJ, Resnicow K. A picture may be worth a thousand texts: Obese adolescents’ perspectives on a modified photovoice activity to aid weight loss. Childhood Obesity. 2012;8:230–236. doi: 10.1089/chi.2011.0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yankeelov PA, Faul AC, D’Ambrosio JG, Collins WL, Gordon B. “Another day in paradise”: A photovoice journey of rural older adults living with diabetes. Journal of Applied Gerontology. 2015;34:199–218. doi: 10.1177/0733464813493136. [DOI] [PubMed] [Google Scholar]
- Yi J, Zebrack B. Self-portraits of families with young adult cancer survivors: Using photovoice. Journal of Psychosocial Oncology. 2010;28:219–243. doi: 10.1080/07347331003678329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi JP, Yi JC, Vitaliano PP, Weinger K. How does anger coping style affect glycemic control in diabetes patients? International Journal of Behavioral Medicine. 2008;15:167–172. doi: 10.1080/10705500802219481. [DOI] [PMC free article] [PubMed] [Google Scholar]