Abstract
Terahertz (THz) imaging is progressing as a robust platform for myriad applications in the field of security, health, and material science. The THz regime, which comprises wavelengths spanning from microns to millimeters, is non-ionizing and has very low photon energy: Making it inherently safe for biological imaging. Colorectal cancer is one of the most common causes of death in the world, while the conventional screening and standard of care yet relies exclusively on the physician’s experience. Researchers have been working on the development of a flexible THz endoscope, as a potential tool to aid in colorectal cancer screening. This involves building a single-channel THz endoscope, and profiling the THz response from colorectal tissue, and demonstrating endogenous contrast levels between normal and diseased tissue when imaging in reflection modality. The current level of contrast provided by the prototype THz endoscopic system represents a significant step towards clinical endoscopic application of THz technology for in-vivo colorectal cancer screening. The aim of this paper is to provide a short review of the recent advances in THz endoscopic technology and cancer imaging. In particular, the potential of single-channel THz endoscopic imaging for colonic cancer screening will be highlighted.
Keywords: Endoscopy, Terahertz imaging, Colonoscopy, Colon, Cancer detection, Flexible waveguides, Metal-coated, Polarization-sensitive, Polarization, Cross-pol
Core tip: Terahertz (THz) imaging is progressing as a robust platform for a myriad of applications in the field of medicine. The non-ionizing THz radiation associated with safe energy levels has the potential to achieve high-resolution images of an organ or tissue, effectively combining both macroscopic and microscopic information. THz reflection imaging provides an intrinsic contrast between normal and diseased tissues, in real-time. This review describes the design, development, and practical implication of flexible THz endoscopic system, while simultaneously obtaining an overview of the existing technology. In addition to the state-of-art THz endoscopy, the feasibility study of a single-channel THz endoscopic system for colorectal cancer screening will be highlighted.
INTRODUCTION
Colorectal cancer
Cancers represents the most common reason for death worldwide causing 8.2 million deaths each year with more than 14 million new diagnosed cases. Colorectal cancer (CRC) is the third most commonly diagnosed cancer in the world causing 0.7 million deaths per year (WHO Data and Statistics). The most effective method of bringing down the cancer risk is the early diagnosis. The current staging and treatment of CRC relies on the traditional imaging technologies; such as conventional colonoscopy[1,2], optical coherence tomography (OCT)[3,4], computed tomography (CT)[5,6], magnetic resonance imaging (MRI)[7,8], and positron emission tomography (PET)[9,10]. The present method for CRC screening is colonoscopy, which relies exclusively on the physician’s experience and judgment. During colonoscopy, the obtained abnormal tissue will be sent for pathological examination for diagnosis.
Besides colonoscopy, the aforementioned CT, MRI and PET are the conventional diagnostic imaging modalities for the detection of CRC. Optical coherence tomography offers micrometer resolution and is proved to be ideal for cancer imaging. However, it has the limitation due to unwanted high optical scattering in the tissue[11]. Computed tomography is a noninvasive technique and provides 3D tomographic images of the entire colon. CT is better at detecting small lesions (less than 1 cm size) as compared with MRI. Despite of that CT cannot detect most common tumors, especially the lesions smaller than 0.5 cm diameter[12]. Furthermore, CT uses harmful ionizing X-rays[13] and cannot be used in renal failure patients[14]. In contrast, magnetic resonance imaging relies on liquid enema for contrast and hence is expensive[12]. On the other hand, positron emission tomography provides good sensitivity and specificity of 80%-90% and can differentiate tumors from scar tissue created by surgery. However, MRI provides very low resolution if the tumor is not metabolically active and also has less sensitivity for lymph node staging[15].
Macroscopic information of the tissue can be attained using conventional CT and MRI techniques, but they provide low-resolution images with less specificity. The microscopic (structural and functional) information can be extracted only from the biopsied samples. It is still not plausible to achieve in-vivo high-resolution images of an organ or tissue with microscopic information in real-time using conventional imaging methods. One can potentially bridge this gap between macroscopic and microscopic imaging using the terahertz (THz) wavelengths spanning from microns to millimeters. In addition, to ascertain the presence of cancer during conventional colonoscopy, a biopsy will be performed from the suspected regions or polyps[16]. Since most of the CRCs, above 80%, are difficult to detect in the early stage; clinicians often schedule regular patient visits and perform biopsy excisions for pathological examination. If an imaging modality provides the ability of delineating the diseased or abnormal region of fresh tissue in real-time, without staining the tissue, it’s not only time effective but also improves the screening capability of endoscopy. Since, THz is nonionizing and provide endogenous contrast within the tissue based on the abnormalities[17], alternative to the conventional colonoscopy, a THz endoscope can potentially be used for the in-vivo cancer screening.
Tissue abnormality and cell disorder
Figure 1 displays the histology slides[18-20] of hyperplastic, normal, and various stages of colon cancer tissues. Usually, a tumorous tissue contains larger size nuclei with irregular shapes. The structures are disorganized and crowded. Figure 1 (N) shows the enface section of normal mucosa with an inset showing normal mucus-secreting colon cell. In the enface direction, Figure 1 (HP) shows both normal and hyperplastic mucosa structures for comparison. Crypts are the columnar structures in the mucosa layer of the colon tissue, made up of goblet cells, with approximately 100 μm diameter. The hyperplastic crypts tend to be order of magnitude larger and elliptical in shape. The hyperplastic crypts shown in the Figure 1 (HP) are 4 times larger than normal crypts and oblong in shape. Figure 1 (P) shows an enface cut of a sporadic juvenile polyp (benign). The smooth eroded surface with numerous mucus retention cysts is typical of these polyps. Figure 1 (S1) shows a benign neoplasm of mucus-secreting colon cell. The Mu denoted in the figure is the mucin contained inside goblet cells. The benign tumor is characterized by crowded nuclei and shortage of mucin production in goblet cells. Figure 1 (S2) exhibits neoplasm of mucus-secreting colon cell. The characteristics shown are larger nuclei, nuclei that are no longer arranged at the bottom of goblet cells, and almost no mucin production.
Figure 1.
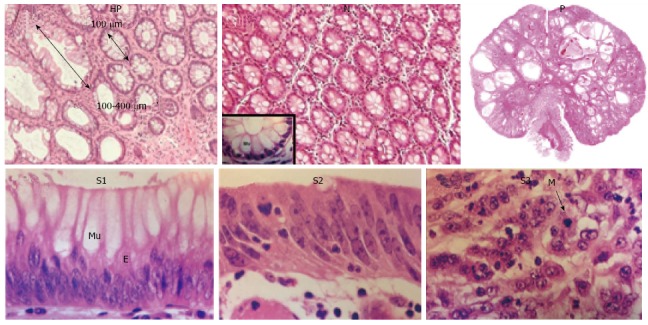
Enface histology[19,20] sections of hyperplastic mucosa (HP), normal (inset: Mucus secreting colon cell) (N), sporadic juvenile benign polyp (P), low grade stage I (S1), intermediate stage II (S2), and high grade stage III colon (S3). Mu: Mucin; E: Epithelium; M: Mitoses.
The typical size of the nucleus is around 1 micron, whereas in neoplastic cells the nuclei tend to be larger and around 3 to 5 μm. Figure 1 (S3) shows a malignant neoplasm of mucus-secreting colon cell, which is characterized by the disorganization of cellular components such that it no longer resembles the normal colon tissue. The aggressive tumor cells are randomly arranged and contain large nuclei that vary in size and shape, dominating most of the cell volume. Therefore, the normal tissue is very homogenous at THz wavelengths while cancerous and dysplastic tissue has structures approaching the size of the wavelength. In addition, the dense structure of abnormal region can lead to higher refractive indices and can result in greater reflectance values. As a result, both of these mechanisms can engender an intrinsic contrast between normal and cancerous regions.
Screening techniques
CRC is one of the most common cancers across the world. The disease is slow to develop, but the early diagnosis and removal of abnormal growths is an effective method of reducing cancer risk. Expert groups recommend that people at average risk for CRC should start regular screening at the age of 50. Several tests can be used to screen CRCs[21] and these tests were classified into two types; tests that can detect both polyps as well as cancer and tests that detect mainly cancer. The first kind looks at the structural information to recognize abnormal regions, which can be achieved with the insertion of scope into the rectum or by using a special X-ray imaging method. This test can prevent CRC, since the polyps found in the benign stage will be removed during the test. The second type diagnostics involve testing stools for the presence of cancer. These tests are less invasive and can be easily performed but are less likely to detect polyps. Although most expert groups generally recommend high sensitivity fecal occult blood test, sigmoidoscopy, and colonoscopy for cancer screening; several other tests such as virtual colonoscopy and barium enema are also used. Table 1 describes the merits and demerits of the techniques used for CRC screening.
Table 1.
Merits and demerits of current conventional techniques used in colorectal cancer screening
| Test | Advantages | Disadvantages |
| Flexible sigmoidoscopy | Quick and safe method | Bowel cleansing is required |
| Biopsy or polypectomy can be done | Can miss small polyps | |
| Usually doesn’t require full bowel preparation | Views only the lower third of the colon | |
| Sedation is not required | Can’t remove all polyps | |
| Done every 5 yr | If an abnormality is found, colonoscopy will be required | |
| Standard colonoscopy | Very sensitive | Full bowel preparation needed |
| Can view entire colon | Can miss small polyps | |
| Can do biopsy and remove polyps | More expensive | |
| Can diagnose other diseases | Minor sedation is required | |
| Done every 10 yr | Small risk of bleeding, bowel tears, or infection | |
| Virtual colonoscopy | Quick and noninvasive | Need full bowel preparation |
| Can view entire colon | Cannot detect polyps < 5 mm | |
| No sedation is needed | Possibility of false positive test results | |
| Done every 5 yr | Cannot remove polyps | |
| If an abnormality is found, colonoscopy will be required | ||
| Fecal occult blood test | Non-invasive | May miss polyps and cancers that doesn’t cause bleeding |
| No bowel preparation is required | Some false positive results | |
| No sedation is required | Pre-test dietary limitations | |
| Inexpensive | Should be done every year | |
| Sampling done at home | If an abnormality is found, colonoscopy will be required |
THz endoscopy
The THz frequency region is situated between microwave and infrared regions of the electromagnetic spectrum with frequencies ranging from 1011 to 5 × 1012 Hz. THz imaging has shown a great potential for in-vivo and ex-vivo identification of tissue abnormalities, hydration and sub-layer probing[22]. Since THz frequencies are sensitive to water content and they can penetrate deep into the tissue, THz was proven to be ideal for cancer[23,24] imaging. Researchers have affirmed the use of THz wavelengths and in turn the potential of THz colonoscopic imaging by demonstrating positive results with dental[25,26], skin[17,27], breast[28], liver[29], oral[30] and especially gastric cancer studies[31].
Endoscopy is a less invasive medical procedure to diagnose the interior surfaces of an organ or cavity of body without the need for surgery. To address the physician’s requirement in accessing different areas of the body[32], endoscopes were traditionally designed in “rigid” and “flexible” configurations. Rigid endoscopes relay images from the tip of the scope to eyepieces with the help of arranged stack of lenses and provide high-quality images. These rigid endoscopes are surgical devices and have to be inserted through temporary access ports created by the physician. Unlike the rigid endoscope, flexible endoscope is more versatile and can be directly inserted through natural body cavities. Usually flexible endoscopes provide low quality images and typically contain either a fiber-optic or miniature video camera at the tip[33]. Using conventional endoscopes, the cancer screening and decision to remove abnormal region solely depends on the visual inspection and experience of a physician. In contrast, a THz endoscope integrated into a conventional endoscopic system will suffice the in-vivo CRC screening requirement in real time. The THz endoscope is a medical device consisting of a flexible THz waveguide instead of an optical fiber and uses a THz laser as light source and a THz detector in place of a video camera for examining the interior surface of an organ or cavity and detects abnormal regions.
THz endoscopic imaging has the potential to offer a safe, minimally invasive medical imaging modality for screening and detecting CRCs. To test this hypothesis, the experimental measurements have to be performed in four steps: Obtaining ideal system-imaging frequency, evaluating base contrast, testing flexible THz waveguides for use as an endoscope, and demonstrating THz waveguide based imaging of colorectal tissue. To confirm system-imaging frequency, the frequency dependent absorption coefficient and refractive index of colorectal tissues must be acquired using a traditional time domain pulsed THz system with frequency bandwidth of 0.1 to 5 THz. To evaluate the base contrast, THz reflectance images of human colonic tissues need to be obtained on ex vivo specimens and compared with the tissue histology. To test the flexible THz waveguides for use as an endoscope, waveguides should be characterized at the desired imaging frequency prior to the determination of waveguide operational parameters. Finally to demonstrate THz endoscopic imaging, the requirement is to integrate flexible waveguide with the transceiver system, implement waveguide based reflection modality imaging, and obtain sensitivity and specificity of the device from colorectal specimens.
Previously proposed THz endoscopes fall into two categories. The first category uses an uncoated polymer tube to transmit THz radiation and works in transmission modality. This study based on anti-resonant hollow core waveguides used a Teflon pipe to transmit THz radiation. However, the guiding capability is compromised due to the radiation not confining inside the bent tube and results in high bending losses[34]. Also, for endoscopic applications that require extensive bending, the guided field easily escapes into the air and interacts with the surrounding and ultimately contaminates the resultant image. In addition, a recent study that relied on a polymer tube to propagate the THz beam with an attached bull’s-eye structure, works in transmission modality, to obtain near-field enhancement[35]. However, in general, the high absorption associated with THz demands reflection based imaging for in vivo applications. The second category uses a mode locked femtosecond laser and relies on optical fibers for pulse propagation. It contains the THz source at the end of the optical fiber and is inserted into the patient[36]. Consequently, electrical connections to drive the THz source must be inserted into the patient. Also it requires two channels, including a first channel for guiding radiation to the sample and a second channel for guiding the reflected light to a detector. In addition, the photoconductive antenna connected with the optical fiber necessitates high input voltage that is inadmissible for in-vivo imaging.
A recent study by Doradla et al[37] demonstrated a bendable prototype endoscopic system that relies on metal-coated THz waveguides for cancer imaging. The endoscopic system uses a single flexible waveguide channel to transmit the THz and collect the reflected signal from the tissue. The system is able to operate in both transmission and reflection configurations. Using a metal-coated THz waveguide provides 99% inner surface reflectivity at all THz wavelengths and confines the THz radiation. It preserves the linearly polarized launched mode and exhibits low bending loss even at larger bending angles. The hyper hemi spherical lens attached to the waveguide output end provides diffraction limited, approximately half the wavelength (λ/2) sized beam waist, which is free from lens aberrations. The resulting THz intensity images, attained using polarization sensitive detection, exhibited an endogenous natural contrast between normal and abnormal (cancer) regions of both formalin fixed and fresh tissues. Henceforth, this study shows the potential of THz endoscopic imaging for cancer screening and detection.
OVERVIEW OF EXPERIMENTAL WORK
THz spectroscopy of colorectal tissue
Intrinsic contrast observed in THz images of human colonic tissues is indicative of a change in the complex refractive index between cancer and normal tissue at THz frequencies. Thus the first step to develop an imaging system is to measure the THz spectroscopic response of colorectal tissues and determine frequency regimes for the contrast. Reid et al[38] and Faustino et al[39] performed THz time domain spectroscopy on cancerous and normal colon tissues, in this section we summarize their results.
Reid et al[38] used a conventional THz-TDS system to image cancer, dysplastic and healthy colon tissues from 30 patients. Their study was carried out in reflection mode and histopathological sections of the imaged tissues were used as the gold standard to classify tissue regions as cancer/dysplastic/normal and the corresponding optical properties were determined and averaged over different specimens. Their results for the frequency dependent absorption coefficient and refractive index are shown in Figure 2. As expected, the absorption increases with increasing frequency (this mimics how liquid water responds in this frequency region) and the refractive index (real part) is fairly steady in the region of interest. What is of interest for imaging applications, however, is the variation of these parameters between healthy and diseased tissue.
Figure 2.
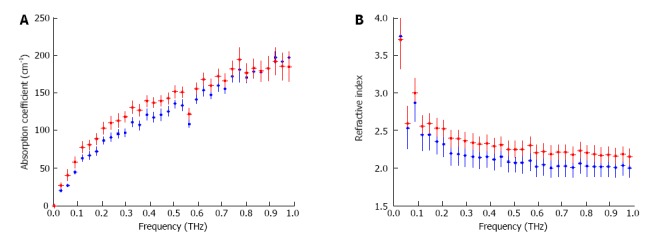
Terahertz spectroscopic results for the absorption coefficient (A) and refractive index (B) of fresh excisions of normal (blue) and cancerous (red) colon tissues[38] (Printed with permission). THz: Terahertz.
Faustino et al[39] investigated the THz reflectance and transmittance of specimens of paraffin embedded colon cancer and normal tissues. The samples investigated were cut to 2 mm thicknesses and the results are displayed in Figure 3.
Figure 3.
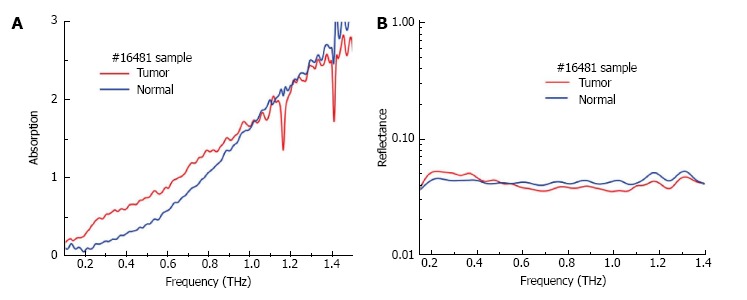
Absorption (A) and reflectance (B) measurements of paraffin embedded dehydrated fixed specimens of normal and cancerous colon tissue[39] (printed with permission). THz: Terahertz.
As seen in Figure 3, there is a difference in the absorption coefficient of normal and cancerous colon in dehydrated formalin fixed samples. This result is extremely interesting as it indicates that water is not the sole contributor to THz contrast. Other studies[40], have shown that while water does contribute to the observed contrast in fresh tissues, it is not the sole mechanism. Other factors such as tissue morphology leading to scattering might also measurably affect the tissue response. We discuss possible contrast mechanisms later in this review, however, at this point the complete mechanism for the intrinsic contrast seen in THz images of colon tissue is not completely understood.
When determining the exposure frequency for THz imaging of colon cancers, it is the difference in the complex refractive index that ultimately determines contrast. Transmission images rely primarily on differences in the absorption coefficient while sample reflectance is dominated by changes to the real part of the refractive index. As seen in Reid et al[38]’s data (Figure 3) while the absorption increases with increasing frequency, the difference in absorption decreases- thus frequencies above approximately 0.7 THz are not suited for transmittance based images. For reflection based imaging, however, the frequency region of interest spans 0.2-1 THz, as the difference in refractive index is equitably constant.
Different imaging approaches are discussed in later sections; however, there are other factors that also influence modality and frequency selection that we discuss below. In vivo applications require reflection based imaging-THz radiation is strongly absorbed by tissue, thus transmission through thick sections is not feasible. Lower frequencies correspond to longer wavelengths and thus lower resolution in the far field. However, higher frequencies experience stronger absorption, thus exhibit less penetration into tissue. Most single frequency systems used for imaging colon tissue thus far work at around 0.6 THz (500 µm) as a compromise between these two factors. A notable exception is the work done by Chen et al[41] in transmission imaging at 0.3 THz (approximately 1 mm); they compensate for the lower far-field resolution by using a specially designed aperture which allows for significantly higher resolution in the near field.
THz imaging of human colorectal tissues
Continuous-Wave (CW), or single frequency imaging of ex vivo samples of normal and cancerous colon tissues has been demonstrated. Faustino et al[39] have imaged paraffin embedded, formalin fixed specimens of normal and cancerous colon in both transmission and reflection modalities. They used a solid-state multiplier/ amplifier chain as their source (VDI systems) and a microbolometer array for detection. The frequency of the imaging system was 0.6 THz (500 μm). As can be seen in Figure 4, the transmittance images of dehydrated fixed tissue still show contrast between normal and cancer, while the reflection images do not show any appreciable difference. This is expected based on the spectroscopy results for these tissues, which are discussed in prior section. The change in absorption persists in the imaging while the lack of difference in the real part of the refractive index shows up as no observable contrast in the reflectance images.
Figure 4.
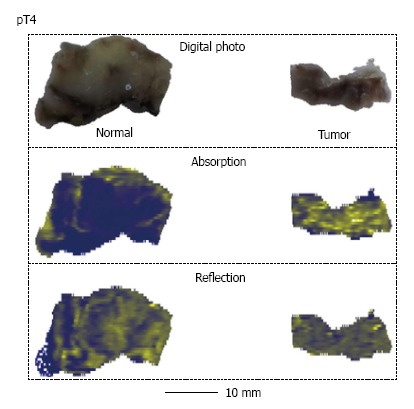
Photographs, absorption (transmittance) and reflection images of formalin fixed dehydrated colon tissue[39] (printed with permission).
Reid et al[38] have imaged excised healthy, dysplastic, and cancerous colonic tissues obtained from 30 patients in reflection modality. They used a stand-alone portable THz imaging system TIP imaga1000. The frequency of the imaging system was 0.03-1 THz. The difference in the reflected waveforms and the ultimate contrast between normal, dysplastic, and cancerous tissue regions were depicted in Figure 5.
Figure 5.
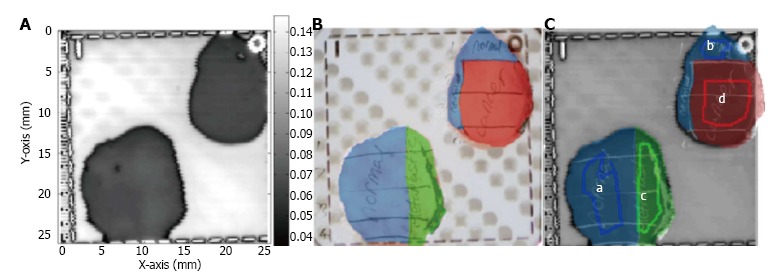
An example terahertz image of excised cancerous, dysplastic and healthy colonic tissues. A: Example terahertz (THz) image of tissue containing healthy regions, dysplasia and cancerous tissue; B: The histology results (drawn onto a photographic image of the tissue samples); C: The histology results are overlaid on the THz image. In this example, regions a and b are normal tissue, c is dysplastic tissue and d is cancerous tissue[38] (printed with permission).
Doradla et al[42] measured the THz reflectance of thick, fresh excisions of cancerous and normal colon tissue using a CW THz imaging system operating at 0.584 THz (513 μm). They used far-infrared laser based on CO2 gas and a silicon bolometer that runs with liquid helium as a detector. Figure 6, below shows a schematic of the imaging system. The beam is incident normal to the sample and the reflectance is measured using a beam-splitter. Wire-grid polarizers allow for the selection of specific polarizations and both images comprised of the co-polarized and cross-polarized remittance of the samples can be measured. The samples used in this study were thick fresh excisions of normal and cancerous colon tissues. The samples were measured the same day as the surgical procedure and were backed with saline soaked gauze during the measurement process to make sure that they did not dry out. Figure 7 shows some of the images collected alongside digital photographs of the sample.
Figure 6.
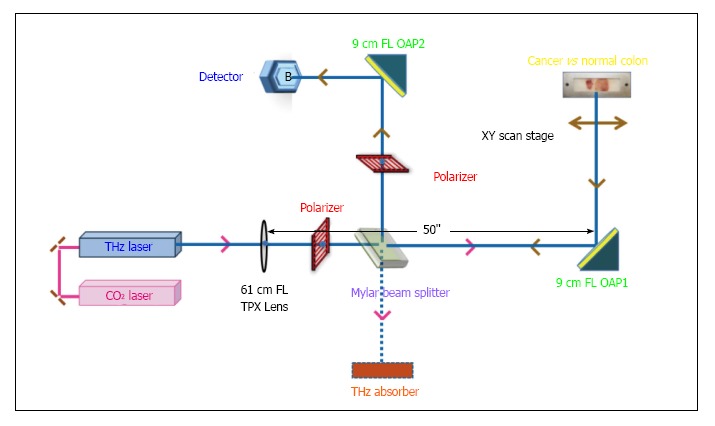
Schematic of continuous-wave terahertz reflection imaging system[42].
Figure 7.
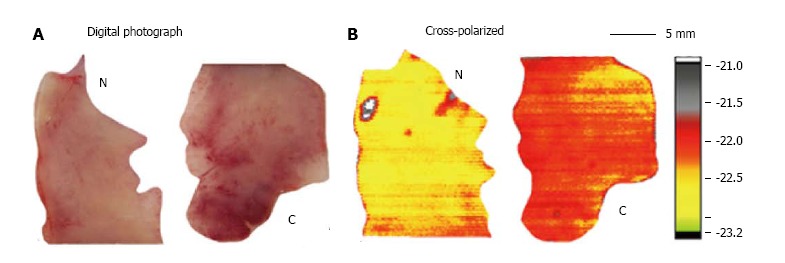
Digital photograph (A) and corresponding terahertz reflectance images (B) of normal (N) and cancerous (C) colon tissue[42].
As shown in Figure 7, the cross-polarized reflectance of normal colon is lower than the cross-polarized reflectance of cancerous colon. This result was found for all 4 sample sets (each sample set consisted of one normal and one cancerous tissue) measured in this study. The authors also computed the percent reflectivity difference between normal and cancerous colon tissue for both the cross-polarized and co-polarized data for each sample set while accounting for background.
As can be seen in Table 2, the cross-polarization channel exhibits a significantly larger reflectivity difference than the co-polarized channel. Moreover, the difference observed in cross-polarization is consistent across different sample sets (i.e., it is consistent across samples from different patients), thus it presents a potential quantitative screening tool for cancer detection.
Table 2.
The relative reflectance difference between normal and cancerous colonic tissue[42]
| Sample # | Co-pol (× 10-1 %) | Cross-pol (%) |
| Set 1 | 1.53 | 7.74 |
| Set 2 | 3.03 | 7.74 |
| Set 3 | 1.56 | 7.75 |
| Set 4 | 2.44 | 7.30 |
Waveguide based imaging
Biomedical imaging of organs or hollow cavities of human body often demands endoscopic access. Highly bendable waveguides with low transmission loss are inevitable for endoscopic applications. Therefore, flexible THz waveguides with good mode preservation characteristics and low propagation and bending losses are essential for in-vivo THz imaging of CRC. Previously, THz waveguides were fabricated from various materials[43-45] with multifarious cross sectional designs[46-48]. Most of these waveguides are either rigid or not flexible at larger bore diameters[49,50]. In addition the flexible THz waveguides suffered from excessive propagation losses[51,52]. On the other hand, the fabrication technique used for the fabrication of the cylindrical waveguides is not applicable for waveguides with < 3 mm diameter[53]. Doradla et al[54,55] reported the characteristics of hollow, flexible, cylindrical THz waveguides that were fabricated with inner metal and metal/dielectric coatings. They provide low loss (less than 1 dB/m) and are small enough in diameter and satisfy the criteria for endoscopic applications.
The three operational parameters of waveguides that are crucial in determining the transmission losses and modal characteristics are waveguide inner diameter, coating material, and material thickness. Selection of coating materials such as silver and polystyrene were described in the preliminary investigation[56]. Also, the optimal coating thicknesses and requisite fabrication processes were detailed[55]. In order to choose a suitable candidate waveguide for THz endoscopic imaging, the characterization was done in three steps: Measuring propagation loss of the waveguide as a function of its inner diameter and coating material, obtaining bending loss as a function of bend radius and bending angle, and acquiring modal characteristics as a function of bending angle, bend radius, waveguide inner diameter, and coating material. The transmission losses and modal characteristics for flexible waveguides can be obtained using the optical layout shown in Figure 8. Harrington et al[49] showed that when the waveguide bore size is about 17 times wavelength the guide is multimode, but when it is 12 times the wavelength or less then the waveguide becomes essentially single mode[54]. The characterization of flexible waveguides at the selected frequency[56], suitable for THz endoscopic system, is described in Ref 56.
Figure 8.
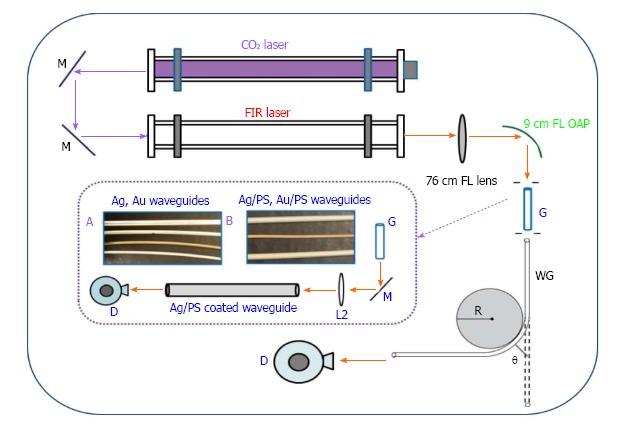
Experimental setup for the transmission loss measurement in metal and metal dielectric. Inset: A: 4 mm Ag (top), 3 mm Ag, 2 mm Au, and 2 mm Ag; B: 3 mm Ag/PS (top), 2 mm Au/PS, and 4 mm Ag/PS) coated terahertz waveguides[54].
Two groups so far have demonstrated waveguide based THz imaging. Chen et al[41] used a polymethyl-methacrylate waveguide to demonstrate THz transmission imaging of human colon tissue and Doradla et al[37] demonstrated reflection modality imaging using a single channel THz waveguide.
The work by Chen et al[41] utilized a continuous-wave source (Gunn diode) centered at 0.3 THz. Figure 9 shows a schematic of their system. As mentioned in Section 2, while 0.3 THz offers contrast in absorption, the resolution is limited in the far-field by the relatively long wavelength (1 mm). Chen et al[41] overcome the resolution restriction by using a bull’s eye structure with a sub-wavelength aperture to get a near field resolution of 0.2 mm.
Figure 9.
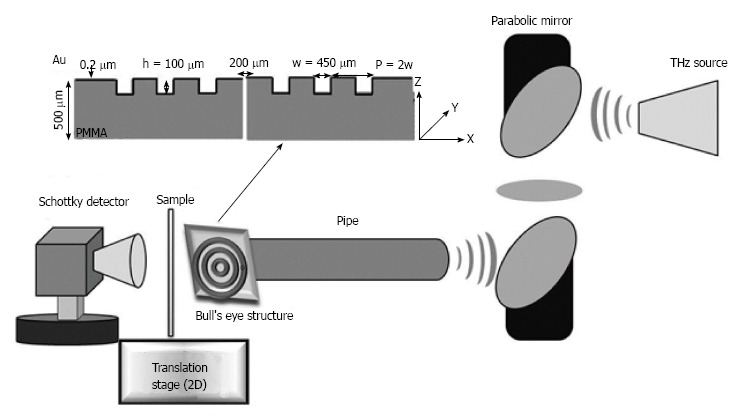
Schematic of waveguide based terahertz near-field transmission imaging system[41] (printed with permission). PMMA: Polymethyl methacrylate.
Figure 10 shows THz transmission images at 0.3 THz of specimens of fresh normal and cancerous colon that have been sectioned into 30 µm thick slices. As expected, the cancerous specimens exhibit significantly higher absorption than normal tissue. Chen et al[41] investigated the response of 30 specimens and were able to demonstrate 100% sensitivity and specificity.
Figure 10.
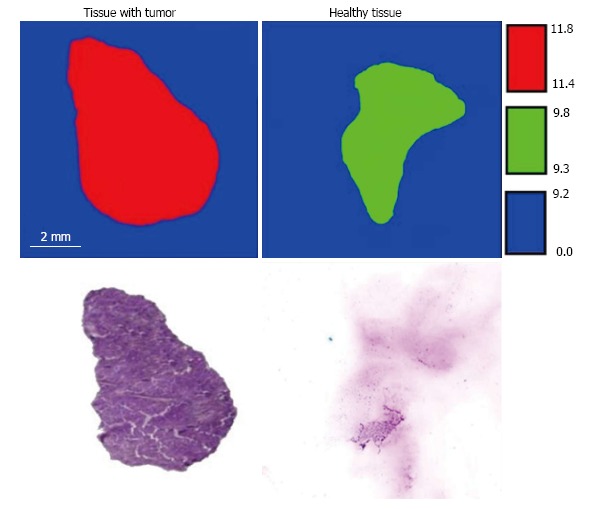
Terahertz transmittance images and stained histology sections showing cancerous and normal colon tissue[41] (printed with permission).
The work by Doradla et al[42,57,58] utilized a far-infrared gas laser operating at 513 μm wavelength (0.58 THz). The THz endoscopic system contains THz transceiver system, system optics and a low-loss flexible THz waveguide. The transceiver system is used for the generation and detection of the THz signal. System optics control and guide the THz beam based on the coupling requirements. Hollow metal-coated waveguide confines and transport the THz beam. Ultimately, to achieve the maximal coupling efficiency and transmission through the waveguide, off axis parabolic mirror (OAP1 of Figure 11) has been adjusted to maintain the ratio of beam size and waveguide diameter as 0.77. This prototype endoscopic system utilized a single-channel for the THz signal transmission, collection from the specimen and works in both transmission and reflection configurations to overcome the higher THz absorption associated with the tissue and satisfy the in-vivo imaging criteria. It uses a highly reflective flexible waveguide lens assembly to propagate THz beam.
Figure 11.
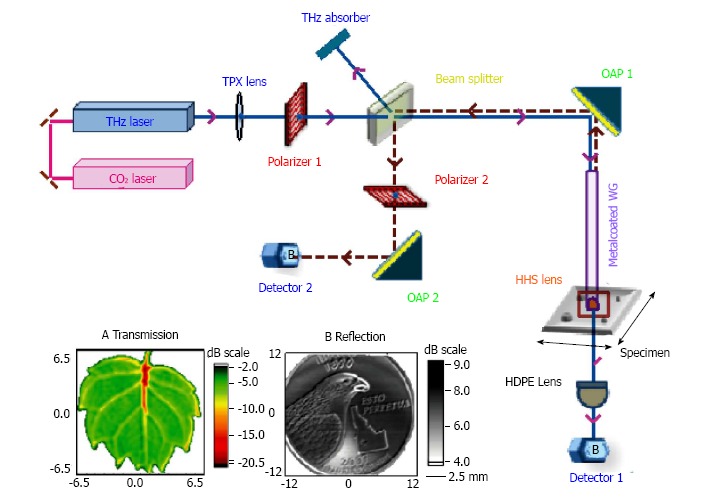
Schematic of single-channel prototype terahertz endoscopic imaging setup. Inset: Terahertz (A) transmission imaging of a small 10 mm leaf, and (B) reflection imaging of a 25-cent coin. THz: Terahertz.
Metal-coated waveguides provide 99% inner surface reflectivity at all THz wavelengths and confine the radiation inside the tube. Metal-coated waveguides preserve the linearly polarized launched mode and exhibits low bending loss even at larger bending angles. The hyper hemispherical lens attached to the waveguide output end provides an aberration free diffraction limited beam waist. The technique in accordance with the present work acquires both co- and cross-polarized THz images using polarization sensitive detection. The data analysis indicates utilizing the cross-polarized component not only helps in obtaining Fresnel reflection free volume sampling but also in achieving a reflectance parameter that doesn’t vary with patient/individual[42,58]. The THz endoscopic system doesn’t need any conventional contrast agents to detect abnormal tissue as an intrinsic contrast was observed between normal and diseased tissue in fresh colonic specimens. Also, the device uses just one channel and hence can be easily integrated with the conventional optical endoscope. Moreover, the prototype THz endoscope is integrated with the flexible THz waveguides, which are small enough in diameter (2 mm to 100 μm). Therefore, based on the application and requirement, the dimensions of the THz probe can be reduced further.
This study[37,58] demonstrated the first prototype continuous-wave THz endoscopic system for cancer detection. The 2D THz intensity images attained using polarization based detection scheme exhibited an endogenous natural contrast between normal and abnormal (cancerous) regions of both formalin fixed and fresh colorectal tissue (Figure 12). The imaging system demonstrated the capability of identifying cancerous colonic tissue based on the intrinsic reflectance difference. The optical layout evident the potential and the experimental manifestation confirms the feasibility of using THz endoscopic device in accessing data from previously inaccessible organs[59]. Furthermore, this study significantly increased and prevail the overall impact of THz imaging for biomedical detection/screening applications[60].
Figure 12.
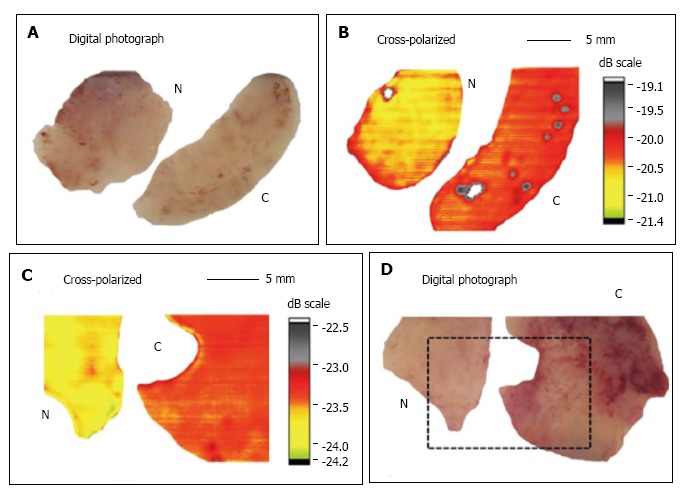
Digital photograph, cross-polarized terahertz reflection images of normal N vs cancerous C human colonic formalin fixed (A and B) and fresh (C and D) tissue sets[58].
CONCLUSION
CRC is the third most commonly diagnosed cancer in the world. Early detection and treatment of CRC can significantly reduce the number of deaths. Current standard of care for CRC screening is an optical endoscopy, which relies on physician’s visual inspection and experience followed by histological analysis of biopsied specimens. Thus, an in vivo imaging modality capable of measuring quantitative differences between diseased (cancerous) and normal colon can significantly improve the screening of CRCs. THz imaging, which is non-ionizing and highly sensitive to tissue water content can potentially fill this niche.
This review article has outlined the steps required for clinical application of THz imaging of CRC and provided an update on the current status of the technology. The first step was to measure the refractive indices and absorption coefficients of normal and diseased colon tissue in the THz region. This has been accomplished by several groups using both fresh and formalin fixed dehydrated colon tissue. The results indicate a measurable difference in specific frequency ranges for both fresh and fixed tissue. The second step was to image normal and cancerous colon at desired frequencies to confirm the contrast can be imaged. This has also been accomplished for both fresh and fixed tissue in both transmission and reflection imaging modalities using THz imaging systems. In order to proceed to clinical systems, the next step was to develop thin, flexible waveguides capable of endoscopic applications. This step has also been accomplished by multiple groups postulating a variety of endoscopic setups. The fourth step was to integrate the waveguide with a THz imaging system and test if waveguide enabled image acquisition was feasible. This was also demonstrated by different groups in both transmission and reflection modalities on fresh colon tissues. There is considerable evidence that THz imaging can potentially screen for colon cancers. A lot of the technological barriers have been overcome and the next step for the field is the development and testing of an in vivo THz endoscopy system capable of providing sensitivity and specificity numbers for the technique in identifying multiple stages of colon cancer.
Footnotes
Conflict-of-interest statement: Authors declare no conflicts of interests for this article.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
Peer-review started: January 5, 2017
First decision: February 21, 2017
Article in press: July 15, 2017
P- Reviewer: Fujino S, Sieg A S- Editor: Kong JX L- Editor: A E- Editor: Lu YJ
References
- 1.Lieberman DA, Weiss DG, Bond JH, Ahnen DJ, Garewal H, Chejfec G. Use of colonoscopy to screen asymptomatic adults for colorectal cancer. Veterans Affairs Cooperative Study Group 380. N Engl J Med. 2000;343:162–168. doi: 10.1056/NEJM200007203430301. [DOI] [PubMed] [Google Scholar]
- 2.Müller AD, Sonnenberg A. Prevention of colorectal cancer by flexible endoscopy and polypectomy. A case-control study of 32,702 veterans. Ann Intern Med. 1995;123:904–910. doi: 10.7326/0003-4819-123-12-199512150-00002. [DOI] [PubMed] [Google Scholar]
- 3.Hariri LP, Tumlinson AR, Besselsen DG, Utzinger U, Gerner EW, Barton JK. Endoscopic optical coherence tomography and laser induced fluorescence spectroscopy in a murine colon cancer model. Lasers in Surgery and Medicine. 2006;38:305–313. doi: 10.1002/lsm.20305. [DOI] [PubMed] [Google Scholar]
- 4.Fercher AF, Drexler W, Hitzenberger CK, Lasser T. Optical coherence tomography-principles and applications. Reports on Progress in Physics. 2003;66:239. [Google Scholar]
- 5.Veerappan GR, Ally MR, Choi JH, Pak JS, Maydonovitch C, Wong RK. Extracolonic findings on CT colonography increases yield of colorectal cancer screening. AJR Am J Roentgenol. 2010;195:677–686. doi: 10.2214/AJR.09.3779. [DOI] [PubMed] [Google Scholar]
- 6.Mathur P, Smith JJ, Ramsey C, Owen M, Thorpe A, Karim S, Burke C, Ramesh S, Dawson PM. Comparison of CT and MRI in the pre-operative staging of rectal adenocarcinoma and prediction of circumferential resection margin involvement by MRI. Colorectal Dis. 2003;5:396–401. doi: 10.1046/j.1463-1318.2003.00537.x. [DOI] [PubMed] [Google Scholar]
- 7.Hadfield MB, Nicholson AA, MacDonald AW, Farouk R, Lee PW, Duthie GS, Monson JR. Preoperative staging of rectal carcinoma by magnetic resonance imaging with a pelvic phased-array coil. Br J Surg. 1997;84:529–531. [PubMed] [Google Scholar]
- 8.Ajaj W, Ruehm SG, Gerken G, Goyen M. Strengths and weaknesses of dark-lumen MR colonography: clinical relevance of polyps smaller than 5 mm in diameter at the moment of their detection. J Magn Reson Imaging. 2006;24:1088–1094. doi: 10.1002/jmri.20734. [DOI] [PubMed] [Google Scholar]
- 9.Kantorová I, Lipská L, Bêlohlávek O, Visokai V, Trubaĉ M, Schneiderová M. Routine (18)F-FDG PET preoperative staging of colorectal cancer: comparison with conventional staging and its impact on treatment decision making. J Nucl Med. 2003;44:1784–1788. [PubMed] [Google Scholar]
- 10.Whiteford MH, Whiteford HM, Yee LF, Ogunbiyi OA, Dehdashti F, Siegel BA, Birnbaum EH, Fleshman JW, Kodner IJ, Read TE. Usefulness of FDG-PET scan in the assessment of suspected metastatic or recurrent adenocarcinoma of the colon and rectum. Dis Colon Rectum. 2000;43:759–767; discussion 767-770. doi: 10.1007/BF02238010. [DOI] [PubMed] [Google Scholar]
- 11.Schmitt JM. Optical coherence tomography (OCT): a review. IEEE Journal of Selected Topics in Quantum Electronics. 1999;5:1205–1215. doi: 10.1109/2944.796347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fletcher JG, Luboldt W. CT colonography and MR colonography: current status, research directions and comparison. Eur Radiol. 2000;10:786–801. doi: 10.1007/s003300051006. [DOI] [PubMed] [Google Scholar]
- 13.Van Reeth E, Tham IW, Tan CH, Poh CL. Super resolution in magnetic resonance imaging: A review. Concepts in Magnetic Resonance Part A. 2012;40:306–325. [Google Scholar]
- 14.Sun L, Wu H, Guan YS. Colonography by CT, MRI and PET/CT combined with conventional colonoscopy in colorectal cancer screening and staging. World J Gastroenterol. 2008;14:853–863. doi: 10.3748/wjg.14.853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schaefer O, Langer M. Detection of recurrent rectal cancer with CT, MRI and PET/CT. Eur Radiol. 2007;17:2044–2054. doi: 10.1007/s00330-007-0613-2. [DOI] [PubMed] [Google Scholar]
- 16.Rex DK, Bond JH, Winawer S, Levin TR, Burt RW, Johnson DA, Kirk LM, Litlin S, Lieberman DA, Waye JD, et al. S. Multi-Society Task Force on Colorectal Cancer. Quality in the technical performance of colonoscopy and the continuous quality improvement process for colonoscopy: recommendations of the U.S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2002;97:1296–1308. doi: 10.1111/j.1572-0241.2002.05812.x. [DOI] [PubMed] [Google Scholar]
- 17.Woodward RM, Cole BE, Wallace VP, Pye RJ, Arnone DD, Linfield EH, Pepper M. Terahertz pulse imaging in reflection geometry of human skin cancer and skin tissue. Phys Med Biol. 2002;47:3853–3863. doi: 10.1088/0031-9155/47/21/325. [DOI] [PubMed] [Google Scholar]
- 18.O’Connell JB, Maggard MA, Ko CY. Colon cancer survival rates with the new American Joint Committee on Cancer sixth edition staging. J Natl Cancer Inst. 2004;96:1420–1425. doi: 10.1093/jnci/djh275. [DOI] [PubMed] [Google Scholar]
- 19.Burkitt HG. New York, NY: Churchill Livingston Inc; 1996. Wheather’s Basic Histopathology. [Google Scholar]
- 20.Andreoni B, Crosta C, Sonzogni A, Pirola M, Pavan A, Bisanti L, Senore C, Sassatelli R, Sguinzi R, Bertani E, et al. Comparison between endoscopic and surgical treatment of screen-detected versus non-screen-detected colorectal cancers. Ecancermedicalscience. 2009;3:142. doi: 10.3332/ecancer.2009.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Burt RW. Colon cancer screening. Gastroenterology. 2000;119:837–853. doi: 10.1053/gast.2000.16508. [DOI] [PubMed] [Google Scholar]
- 22.Mittleman DM, Gupta M, Neelamani R, Baraniuk RG, Rudd JV, Koch M. Recent advances in terahertz imaging. Applied Physics B. 1999;68:1085–1094. [Google Scholar]
- 23.Fitzgerald AJ, Wallace VP, Jimenez-Linan M, Bobrow L, Pye RJ, Purushotham AD, Arnone DD. Terahertz pulsed imaging of human breast tumors. Radiology. 2006;239:533–540. doi: 10.1148/radiol.2392041315. [DOI] [PubMed] [Google Scholar]
- 24.Doradla P, Alavi K, Joseph CS, Giles RH. Terahertz polarization imaging for colon cancer detection. Proc. SPIE 8685, Terahertz, RF, Millimeter, and Submillimeter-Wave Technology and Applications VI, 2014, 89850K. [Google Scholar]
- 25.Crawley D, Longbottom C, Wallace VP, Cole B, Arnone D, Pepper M. Three-dimensional terahertz pulse imaging of dental tissue. J Biomed Opt. 2003;8:303–307. doi: 10.1117/1.1559059. [DOI] [PubMed] [Google Scholar]
- 26.Longbottom C, Crawley DA, Cole BE, Arnone DD, Wallace VP, Pepper M. Potential uses of terahertz pulse imaging in dentistry: caries and erosion detection. International Society for Optics and Photonics, Proceedings of SPIE. 2002;4610:109–112. [Google Scholar]
- 27.Tewari P, Kealey CP, Bennett DB, Bajwa N, Barnett KS, Singh RS, Culjat MO, Stojadinovic A, Grundfest WS, Taylor ZD. In vivo terahertz imaging of rat skin burns. J Biomed Opt. 2012;17:040503. doi: 10.1117/1.JBO.17.4.040503. [DOI] [PubMed] [Google Scholar]
- 28.Ashworth PC, Pickwell-MacPherson E, Provenzano E, Pinder SE, Purushotham AD, Pepper M, Wallace VP. Terahertz pulsed spectroscopy of freshly excised human breast cancer. Opt Express. 2009;17:12444–12454. doi: 10.1364/oe.17.012444. [DOI] [PubMed] [Google Scholar]
- 29.Enatsu T, Kitahara H, Takano K, Nagashima T. Terahertz spectroscopic imaging of paraffin-embedded liver cancer samples. Joint 32nd Int. Conf. Infrared and Millimeter Waves and the 15th Int. Conf. Terahertz Electronics. IRMMW-THz. 2007;1:557–558. [Google Scholar]
- 30.Specchia G, De Servi S, Poma E, Ghio S, Ferrario M, Angoli L, Ardissino D, Bramucci E, Mussini A. Clinical application of monitoring techniques: coronary sinus blood flow monitoring. Can J Cardiol. 1986;Suppl A:170A–172A. [PubMed] [Google Scholar]
- 31.Hou D, Li X, Cai J, Ma Y, Kang X, Huang P, Zhang G. Terahertz spectroscopic investigation of human gastric normal and tumor tissues. Phys Med Biol. 2014;59:5423–5440. doi: 10.1088/0031-9155/59/18/5423. [DOI] [PubMed] [Google Scholar]
- 32.Hake LW, inventor; Hake Lawrence W, assignee Endoscope construction with means for controlling rigidity and curvature of flexible endoscope tube. United States patent US 4890602. 1990:Jan 2.
- 33.Dennis CL. Digital Endoscope Design, SPIE Press Book, Volume: SL10, 2016. ISBN: 9781510601611.
- 34.Chen HZ, Lu JY, You B. Terahertz endoscope based on anti- resonant reflecting hollow core waveguides. Lasers & Electro-optics. 2011;86146:08855–1331. [Google Scholar]
- 35.Chiu CM, Chen HW, Huang YR, Hwang YJ, Lee WJ, Huang HY, Sun CK. All-terahertz fiber-scanning near-field microscopy. Opt Lett. 2009;34:1084–1086. doi: 10.1364/ol.34.001084. [DOI] [PubMed] [Google Scholar]
- 36.Ji YB, Lee ES, Kim SH, Son JH, Jeon TI. A miniaturized fiber-coupled terahertz endoscope system. Opt Express. 2009;17:17082–17087. doi: 10.1364/OE.17.017082. [DOI] [PubMed] [Google Scholar]
- 37.Doradla P, Alavi K, Joseph C, Giles R. Single-channel prototype terahertz endoscopic system. J Biomed Opt. 2014;19:080501. doi: 10.1117/1.JBO.19.8.080501. [DOI] [PubMed] [Google Scholar]
- 38.Reid CB, Fitzgerald A, Reese G, Goldin R, Tekkis P, O’Kelly PS, Pickwell-MacPherson E, Gibson AP, Wallace VP. Terahertz pulsed imaging of freshly excised human colonic tissues. Phys Med Biol. 2011;56:4333–4353. doi: 10.1088/0031-9155/56/14/008. [DOI] [PubMed] [Google Scholar]
- 39.Faustino W, Kasalynas I, Venckevicius R, Seliuta D, Valusis G, Urbanowicz A, Molis G, Carneiro F, Silva CDC, Granja PL. Terahertz absorption and reflection imaging of carcinoma-affected colon tissues embedded in paraffin. Journal of Molecular Structure. 2016;1107:214–219. [Google Scholar]
- 40.Sy S, Huang S, Wang YX, Yu J, Ahuja AT, Zhang YT, Pickwell-MacPherson E. Terahertz spectroscopy of liver cirrhosis: investigating the origin of contrast. Phys Med Biol. 2010;55:7587–7596. doi: 10.1088/0031-9155/55/24/013. [DOI] [PubMed] [Google Scholar]
- 41.Chen H, Ma S, Wu X, Yang W, Zhao T. Diagnose human colonic tissues by terahertz near-field imaging. J Biomed Opt. 2015;20:036017. doi: 10.1117/1.JBO.20.3.036017. [DOI] [PubMed] [Google Scholar]
- 42.Doradla P, Alavi K, Joseph C, Giles R. Detection of colon cancer by continuous-wave terahertz polarization imaging technique. J Biomed Opt. 2013;18:090504–090504. [Google Scholar]
- 43.Lu JT, Hsueh YC, Huang YR, Hwang YJ, Sun CK. Bending loss of terahertz pipe waveguides. Opt Express. 2010;18:26332–26338. doi: 10.1364/OE.18.026332. [DOI] [PubMed] [Google Scholar]
- 44.George R, Harrington JA. Infrared transmissive, hollow plastic waveguides with inner Ag-Agl coatings. Appl Opt. 2005;44:6449–6455. doi: 10.1364/ao.44.006449. [DOI] [PubMed] [Google Scholar]
- 45.Nielsen K, Rasmussen HK, Adam AJ, Planken PC, Bang O, Jepsen PU. Bendable, low-loss Topas fibers for the terahertz frequency range. Opt Express. 2009;17:8592–8601. doi: 10.1364/oe.17.008592. [DOI] [PubMed] [Google Scholar]
- 46.Yeh C, Shimabukuro F, Siegel PH. Low-loss terahertz ribbon waveguides. Appl Opt. 2005;44:5937–5946. doi: 10.1364/ao.44.005937. [DOI] [PubMed] [Google Scholar]
- 47.Mitrofanov O, James R, Fernández FA, Mavrogordatos TK, Harrington JA. Reducing transmission losses in hollow THz waveguides. IEEE Transactions Terahertz Science and Technology. 2011;1:124–132. [Google Scholar]
- 48.Lu JT, Lai CH, Tseng TF, Chen H, Tsai YF, Chen IJ, Hwang YJ, Chang HC, Sun CK. Terahertz polarization-sensitive rectangular pipe waveguides. Opt Express. 2011;19:21532–21539. doi: 10.1364/OE.19.021532. [DOI] [PubMed] [Google Scholar]
- 49.Harrington J, George R, Pedersen P, Mueller E. Hollow polycarbonate waveguides with inner Cu coatings for delivery of terahertz radiation. Opt Express. 2004;12:5263–5268. doi: 10.1364/opex.12.005263. [DOI] [PubMed] [Google Scholar]
- 50.Bowden B, Harrington JA, Mitrofanov O. Silver/polystyrene-coated hollow glass waveguides for the transmission of terahertz radiation. Optics Letters. 2007;32:2945–2947. doi: 10.1364/ol.32.002945. [DOI] [PubMed] [Google Scholar]
- 51.Vitiello MS, Xu J, Beltram F, Tredicucci A, Mitrofanov O, Harrington J, Ritchie DA. Guiding a terahertz quantum cascade laser into a flexible silver-coated waveguide. Journal of Applied Physics. 2011;110:0631121–0631125. [Google Scholar]
- 52.Dupuis A, Stoeffler K, Ung B, Dubois C, Skorobogatiy M. Transmission measurements of hollow-core THz Bragg fibers. JOSA B. 2011;28:896–907. [Google Scholar]
- 53.Matsuura Y, Takeda E. Hollow optical fibers loaded with an inner dielectric film for terahertz broadband spectroscopy. JOSA B. 2008;25:1949–1954. [Google Scholar]
- 54.Doradla P, Joseph CS, Kumar J, Giles RH. Characterization of bending loss in hollow flexible terahertz waveguides. Opt Express. 2012;20:19176–19184. doi: 10.1364/OE.20.019176. [DOI] [PubMed] [Google Scholar]
- 55.Doradla P, Joseph CS, Kumar J, Giles RH. Propagation loss optimization in metal/dielectric coated hollow flexible terahertz waveguides. International Society for Optics and Photonics, Proceedings of SPIE. 2012;8261:82610P1–82610P10. [Google Scholar]
- 56.Doradla P, Giles RH. Dual-frequency characterization of bending loss in hollow flexible terahertz waveguides. Proc. SPIE 8685, Terahertz, RF, Millimeter, and Submillimeter-Wave Technology and Applications VI; 2014. p. 898518. [Google Scholar]
- 57.Doradla P, Alavi K, Joseph C, Giles R. Continuous wave terahertz reflection imaging of human colorectal tissue. Proc. SPIE 8624, Terahertz, RF, Millimeter, and Submillimeter-Wave Technology and Applications VI; 2013. p. 86240O. [Google Scholar]
- 58.Doradla P, Joseph CS, Kumar J, Giles RH. Development of terahertz endoscopic system for cancer detection. Proc. SPIE 9747, Terahertz, RF, Millimeter, and Submillimeter-Wave Technology and Applications IX; 2016. p. 97470F. [Google Scholar]
- 59.Doradla P, Alavi K, Joseph CS, Giles RH. Flexible waveguide enabled single-channel terahertz endoscopic system. Proc. SPIE 9362, Terahertz, RF, Millimeter, and Submillimeter-Wave Technology and Applications IX; 2015. p. 93620D. [Google Scholar]
- 60.Doradla P. 2015. Terahertz Endoscopic System for Cancer Detection. Lambert Academic Publishing; p. 1. [Google Scholar]


