Abstract
Dural arteriovenous fistulas (DAVFs) are direct communications between the intracranial arterial and venous systems without an intervening nidus. Clinicians sometimes fail to give a correct diagnosis of DAVF. Given the similarity of their clinical and magnetic resonance imaging (MRI) manifestations, diagnostic confusion may arise between DAVF and cerebral venous sinus thrombosis (CVST) (Simon et al., 2009). The clinical management of DAVFs differs from that of CVST (Ma et al., 2015; Yang et al., 2015). Anticoagulation therapy is restricted in some cases of DAVFs, especially when they are associated with retrograde venous flow, due to the increased risk of hemorrhage. Here we present a case of a DAVF patient who had been initially misdiagnosed as CVST. We summarize the reasons for misdiagnosis and give some recommendations to address this problem.
Keywords: Dural arteriovenous fistula, Cerebral sinus thrombosis, Susceptibility-weighted MRI, Digital subtraction angiography
Dural arteriovenous fistulas (DAVFs) are direct communications between the intracranial arterial and venous systems without an intervening nidus. Clinicians sometimes fail to give a correct diagnosis of DAVF. Given the similarity of their clinical and magnetic resonance imaging (MRI) manifestations, diagnostic confusion may arise between DAVF and cerebral venous sinus thrombosis (CVST) (Simon et al., 2009). The clinical management of DAVFs differs from that of CVST (Ma et al., 2015; Yang et al., 2015). Anticoagulation therapy is restricted in some cases of DAVFs, especially when they are associated with retrograde venous flow, due to the increased risk of hemorrhage. Here we present a case of a DAVF patient who had been initially misdiagnosed as CVST. We summarize the reasons for misdiagnosis and give some recommendations to address this problem.
A 61-year-old male was admitted on 3rd August, 2015, after suffering a speech disorder after dinner and slow reactions for 15 d. One day after admission, he had two episodes of general epileptic seizure. Then, he complained of headache and fever. MRI at a local hospital revealed ischemic lesions of the left temporal and occipital lobes with mass effect and perifocal edema (Figs. 1a and 1b). Results from a cerebral spinal fluid test were unremarkable. Magnetic resonance venography (MRV) revealed a filling defect in the torcular and left transverse and sigmoid sinus, which strongly suggested sinus thrombosis (Fig. 1c). Therefore, the initial diagnosis was made as left transverse and sigmoid sinus thrombosis. Anti-platelet and anti-infection treatments were administered at the local hospital. However, no improvement was observed. The patient developed weakness of the right arm on Day 14. On Day 15, he was transferred to our hospital. On neurological examination, he had mixed aphasia with drowsiness. Susceptibility-weighted imaging (SWI) showed multiple hypointense vessels in the left temporal and occipital lobes, and hyperintensity in the left temporal lobe (Fig. 1d).
Fig. 1.
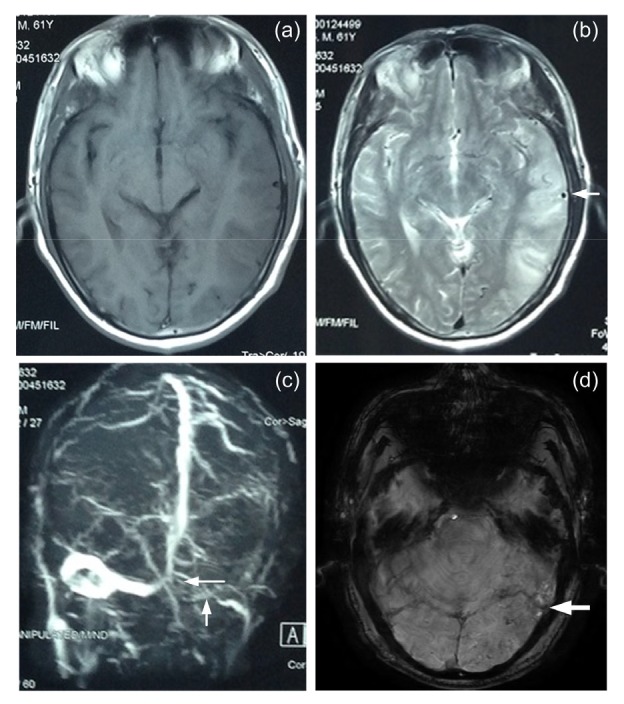
Magnetic resonance imaging (MRI), magnetic resonance venography (MRV), and susceptibility-weighted imaging (SWI)
(a) T1-weighted MRI; (b) T2-weighted MRI, and the arrow shows a flow void shadow of enlarged meningeal vessels in the left temporal lobe; (c) MRV, and the white arrows show a filling defect in the torcular and left transverse and sigmoid sinus; (d) SWI, and the white arrow shows hyperintensity in the left temporal lobe
Digital subtraction angiography (DSA) was performed, which revealed an arteriovenous fistula fed by both the middle meningeal artery and the occipital artery, and draining into the left transverse and sigmoid sinus (Figs. 2a and 2b). A thick vein at the left transverse sinus was draining into the sphenoparietal sinus, and multiple retrograde cortical venous filling on the surface of the left hemisphere was draining into the superior sagittal sinus (Fig. 2c). The DSA also showed the occlusion of the proximal part of the left sigmoid sinus. Catheters were unable to reach the fistula from the peripheral vessel system. The patient underwent embolization with detachable coils under the condition of craniotomy after general anaesthesia. Under the guidance of the route map, we planned an incision based on the left transverse sinus localization on the scalp surface. A left transverse and sigmoid sinus puncture was performed under direct vision after craniotomy. The sinus was occluded after embolization with detachable coils. Postoperative DSA revealed no arteriovenous fistula (Figs. 2d–2f). Besides, preoperative DSA images of the left vertebral injection (Figs. 2g and 2h) revealed no fistula. After an uneventful postoperative course, the patient was discharged. Six months post operation, follow-up DSA again revealed no arteriovenous fistula.
Fig. 2.
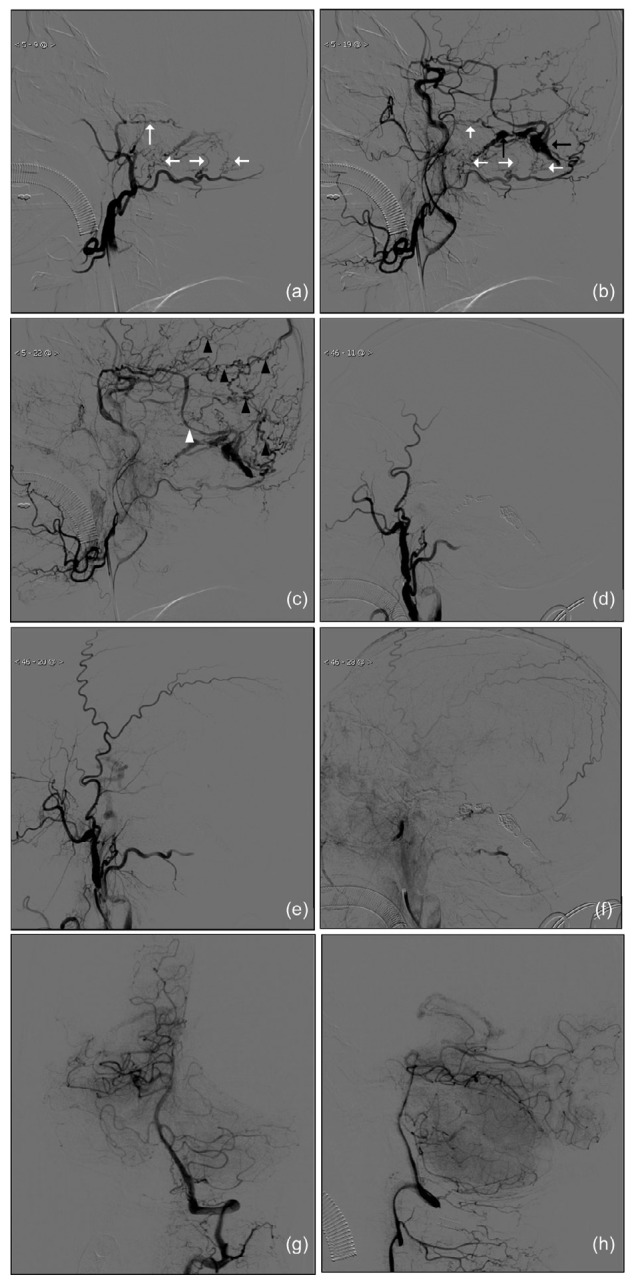
Preoperative and postoperative lateral digital subtraction angiography (DSA) images of the left external carotid artery (ECA) injection and preoperative DSA images of the left vertebral injection
Early (a), middle (b), and late (c) stages of the preoperative lateral DSA images; Early (d), middle (e), and late (f) stages of the postoperative lateral DSA images; Towne (g) and lateral (h) views of the preoperative DSA images of left vertebral injection. Black arrows show the early appearance of the left transverse and sigmoid sinus, confirming the diagnosis of a DAVF. White arrows show abnormally enlarged branches of the middle meningeal artery and occipital artery serving as feeders. The white arrowhead shows a thick vein at the left transverse sinus draining into the sphenoparietal sinus. Black arrowheads showed multiple retrograde cortical venous draining into the superior sagittal sinus
Here, we report a case with initial diagnosis of CVST based on non-invasive examinations. However, DAVF was revealed by DSA. Two cases of DAVF misdiagnosed as CVST in the absence of DSA examination were reported by Simon et al. (2009). The reasons may help explain the clinical confusion. Firstly, DAVF and CVST can present as very similar clinical scenarios. CVST has been widely recognized in recent years, but not DAVF. Secondly, non-invasive examinations such as MRI/MRV have limitations that can lead to misdiagnosis (Kimchi et al., 2007). In our case, MRI revealed left temporal and occipital infarction with perifocal edema, and MRV revealed a filling defect in the left transverse and sigmoid sinus which could be misinterpreted as dural sinus thrombosis. The external carotid artery (ECA) is usually ignored by magnetic resonance angiography (MRA) or computed tomography angiography (CTA). Thirdly, among DAVF patients, a thrombosis in the affected dural sinus may represent either a cause or a consequence. Based on these reasons, DSA is recommended for patients with a diagnosis of CVST, especially among those with follow-up complaints of headache or tinnitus.
The relationship between CVST and DAVF is complicated (Nishio et al., 2002; Shimizu et al., 2003; Safavi-Abbasi et al., 2008; Yeh et al., 2010). In a study by Tsai et al. (2004), 27 of 69 DAVF patients had CVST and most thromboses were located in the downstream area or around the DAVF. It has been proposed that the development of a fistula is related to sinus thrombosis, which leads to the opening up of small physiological arteriovenous pathways in the wall of the sinus or abnormal connections forming during recanalization (Kojima et al., 2007). Also, the question why a fistula may give rise to thrombosed sinuses needs to be addressed. It is most likely that thrombosis occurs at some stages in fistula development, possibly due to stenosis or thickening of sinus walls leading to turbulence and subsequent thrombus formation (Shimizu et al., 2001). Our patients’ angiography revealed a fistula with coexistence of a venous sinus filling defect and retrograde drainage, which led to the question: was DAVF subsequent to venous sinus thrombosis? The answer was that this was unlikely, because the patient did not previously present symptoms related to venous sinus thrombosis. Furthermore, there was a lack of causative local and general conditions for thrombosis, such as trauma, infection, or coagulopathy as pathophysiology evidence. On the other hand, filling defects were located in both upstream and downstream areas, which might support the pathophysiology. So in this case, we tended to conclude that the thrombus followed and was a result of DAVF development.
In addition, CVST is an independent risk factor for aggressive manifestation of DAVF (Tsai et al., 2004). Since thrombus may amplify venous hypertension and induce retrograde flow in the cortical veins, such patients are more likely to experience aggressive manifestations as intracerebral hemorrhage. We should be cautious when making diagnosis. Further DSA examination is definitely necessary for patients with a diagnosis of CVST. When DSA examination is not available, close follow-up observation is required. Also, recent reports have highlighted the ability of SWI to identify arteriovenous shunting in brain vascular malformations, revealed by hyperintensity within dilated hypointensive leptomeningeal and medullary veins (Letourneau-Guillon et al., 2012; Kalra et al., 2013; Nakagawa et al., 2013). Prominent hypointense vessels seen in DAVF patients revealed venous congestion caused by increased venous pressure secondary to venous arterialization. The hyperintensity has been attributed to a combination of the time-of-flight phenomenon intrinsic to high-velocity arterial flow and to the lack of a paramagnetic phase shift secondary to the diamagnetic oxyhemoglobin content of arterial blood (Tsui et al., 2009; Jagadeesan et al., 2011). In our case, SWI showed hyperintensity which might indicate a fistula (Fig. 1d). As a non-invasive and convenient examination, we believe that SWI has potential clinical application in DAVF diagnosis. Fig. 1b shows a flow void shadow of enlarged meningeal vessels in the left temporal lobe, which was probably associated with venous hypertension secondary to the fistula.
In conclusion, we present a case of dural arteriovenous fistula which was initially diagnosed as CVST. Based on a literature review and our experience, a DSA examination should be recommended for patients with sinus thrombosis following non-invasive examinations, especially when hyperintensity is revealed by SWI.
Footnotes
Project supported by the National Natural Science Foundation of China (No. 81173595) and the China-Japan Friendship Hospital Youth Science and Technology Excellence Project (No. 2014-QNYC-A-04), China
Compliance with ethics guidelines: Li-li SUN, Wen-xiong TANG, Lei LIU, Wei WANG, Si-xun ZHANG, and Zun-jing LIU declare that they have no conflict of interest.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5). Informed consent was obtained from the patient for being included in the study. Additional informed consent was obtained from the patient for which identifying information is included in this article.
References
- 1.Jagadeesan BD, Almandoz JED, Moran CJ, et al. Accuracy of susceptibility-weighted imaging for the detection of arteriovenous shunting in vascular malformations of the brain. Stroke. 2011;42(1):87–92. doi: 10.1161/STROKEAHA.110.584862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kimchi TJ, Lee SK, Agid R, et al. Cerebral sinovenous thrombosis in children. Neuroimag Clin N Am. 2007;17(2):239–244. doi: 10.1016/j.nic.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 3.Kalra VB, Malhotra A, Matouk CC. Teaching neuroimages: susceptibility-weighted MRI: first clue to DAVF complicating sinovenous thrombosis. Neurology. 2013;80(21):e228. doi: 10.1212/WNL.0b013e318293e323. [DOI] [PubMed] [Google Scholar]
- 4.Kojima T, Miyachi S, Sahara Y, et al. The relationship between venous hypertension and expression of vascular endothelial growth factor: hemodynamic and immunohistochemical examinations in a rat venous hypertension model. Surg Neurol. 2007;68(3):277–284. doi: 10.1016/j.surneu.2006.10.075. [DOI] [PubMed] [Google Scholar]
- 5.Letourneau-Guillon L, Krings T. Simultaneous arteriovenous shunting and venous congestion identification in dural arteriovenous fistulas using susceptibility-weighted imaging: initial experience. Am J Neuroradiol. 2012;33(2):301–307. doi: 10.3174/ajnr.A2777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ma X, Ji XM, Fu P, et al. Coexistence of high fibrinogen and low high-density lipoprotein cholesterol levels predicts recurrent cerebral venous thrombosis. Chin Med J. 2015;128(13):1732–1737. doi: 10.4103/0366-6999.159345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nakagawa I, Taoka T, Wada T, et al. The use of susceptibility-weighted imaging as an indicator of retrograde leptomeningeal venous drainage and venous congestion with dural arteriovenous fistula: diagnosis and follow-up after treatment. Neurosurgery. 2013;72(1):47–54. doi: 10.1227/NEU.0b013e318276f7cc. [DOI] [PubMed] [Google Scholar]
- 8.Nishio A, Ohata K, Tsuchida K, et al. Dural arteriovenous fistula involving the superior sagittal sinus following sinus thrombosis–case report. Neurol Med Chir. 2002;42(5):217–220. doi: 10.2176/nmc.42.217. [DOI] [PubMed] [Google Scholar]
- 9.Safavi-Abbasi S, di Rocco F, Nakaji P, et al. Thrombophilia due to factor V and factor II mutations and formation of a dural arteriovenous fistula: case report and review of a rare entity. Skull Base-Interdiscip Appr. 2008;18(2):135–143. doi: 10.1055/s-2007-1003926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shimizu S, Sato S, Iida H, et al. Sinus thrombosis probably resulting from a dural arteriovenous fistula development in the superior sagittal sinus. Acta Neurochir. 2003;145(8):719–720. doi: 10.1007/s00701-003-0049-7. [DOI] [PubMed] [Google Scholar]
- 11.Simon S, Yao T, Ulm AJ, et al. Dural arteriovenous fistulas masquerading as dural sinus thrombosis. J Neurosurg. 2009;110(3):514–517. doi: 10.3171/2008.7.JNS08253. [DOI] [PubMed] [Google Scholar]
- 12.Tsai LK, Jeng JS, Liu HM, et al. Intracranial dural arteriovenous fistulas with or without cerebral sinus thrombosis: analysis of 69 patients. J Neurol Neurosurg Psychiatry. 2004;75(11):1639–1641. doi: 10.1136/jnnp.2003.026583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tsui YK, Tsai FY, Hasso AN, et al. Susceptibility-weighted imaging for differential diagnosis of cerebral vascular pathology: a pictorial review. J Neurol Sci. 2009;287(1-2):7–16. doi: 10.1016/j.jns.2009.08.064. [DOI] [PubMed] [Google Scholar]
- 14.Yang S, Li R, Chen XN, et al. Acute cerebral thrombosis following ovarian hyperstimulation syndrome: a case report. Chin Med J. 2015;128(24):3383–3384. doi: 10.4103/0366-6999.171467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yeh PS, Wu TC, Tzeng WS, et al. Endovascular angioplasty and stent placement in venous hypertension related to dural arteriovenous fistulas and venous sinus thrombosis. Clin Neurol Neurosurg. 2010;112(2):167–171. doi: 10.1016/j.clineuro.2009.10.018. [DOI] [PubMed] [Google Scholar]


