Abstract
Introduction
Few population-based data are available evaluating the prevalence of lower urinary tract symptoms (LUTS) in Asia. The objective of our study was to determine LUTS prevalence in China, Taiwan, and South Korea using International Continence Society (ICS) 2002 criteria.
Methods
An Internet-based self-administered survey among individuals aged at least 40 years with the ability to use a computer and to read the local language. Survey questions included ICS symptom definitions and the international prostate symptom score (IPSS). Data analysis was based on descriptive statistics and post hoc significance testing.
Results
There were 8284 participants, of whom 51% were women and 34% were aged at least 60 years. LUTS prevalence was slightly higher in men than women (62.8% vs. 59.6%; p = 0.004), increasing significantly with age (p = 0.001). All three ICS symptom groups (voiding, storage, and post-micturition) were present in 35% of individuals with LUTS. Symptoms with the highest overall prevalence were nocturia, frequency, incomplete emptying, and terminal dribble. The most bothersome symptoms were terminal dribble, nocturia, and urgency. According to IPSS scores, 87% of participants had at least mild symptoms; 43% of those aged over 60 years had moderate/severe symptoms. The percentage of participants with any LUTS who had visited healthcare professionals because of urinary symptoms was 26%, rising to 45% amongst individuals with all three symptom groups (p = 0.001 vs. other ICS symptom groups).
Conclusions
LUTS are highly prevalent in men and women aged at least 40 years who participated in this study in China, Taiwan, and South Korea and increases with increasing age. A minority of individuals with LUTS seek healthcare and our results suggest an increased patient awareness of LUTS is required.
Funding
Astellas Pharma Singapore Pte. Ltd.
Trial registration
ClinicalTrials.gov identifier, NCT02618421.
Electronic supplementary material
The online version of this article (doi:10.1007/s12325-017-0577-9) contains supplementary material, which is available to authorized users.
Keywords: China, Lower urinary tract symptoms, Prevalence, Republic of Korea, Taiwan, Urology
Introduction
Lower urinary tract symptoms (LUTS) include a variety of storage, voiding, and post-micturition symptoms [1, 2]. Both overactive bladder symptom complex (OAB; urinary urgency, with or without urgency incontinence, usually with increased urinary frequency and nocturia) and stress incontinence comprise the main storage symptoms; voiding symptoms include slow or interrupted stream, terminal dribble, hesitancy and straining; while incomplete emptying and post-micturition dribble are the key post-micturition symptoms. In men, symptoms may be related to prostate dysfunction, bladder dysfunction, other structural or functional abnormalities of the urinary tract and surrounding tissues, or non-urological conditions (e.g., nocturia) [3]. This multifactorial etiology of LUTS in men is reflected in the different pharmacological agents used to manage symptoms, which include alpha-adrenergic blocking agents, 5-alpha reductase inhibitors, and phosphodiesterase 5 inhibitors [3]. OAB tends to be viewed as the main cause of LUTS in women and is recognized as the most bothersome component of male LUTS. In both sexes, OAB generally responds to anticholinergic medications or the β3-adrenergic agonist mirabegron [4].
LUTS affect a significant proportion of adults and are associated with impaired quality of life (QoL) [5–7]. LUTS prevalence from large studies in Europe and North America exceeds 60%, with a slightly higher overall prevalence in women than men [8, 9]. However, prevalence is age-related and, over the age of 70 years, LUTS are more common in men than women although urinary incontinence remains more prevalent in women [9]. Recognition of LUTS has increased in both sexes in recent years, including underactive bladder among those aged over 60 years. The EpiLUTS study showed that symptoms are often bothersome: at least half of participants with symptoms occurring at least “sometimes” were bothered “somewhat” or more [8]. In Asia, few such population-based studies have been performed [10, 11], symptom definitions have varied between studies [9], and no international study has been performed in both men and women in Asia using the symptom definitions recommended by the International Continence Society (ICS) in 2002 [1]. Consequently, our understanding of the true burden of LUTS in Asia is limited.
We performed this study to evaluate for the first time the overall prevalence of LUTS in adults aged at least 40 years in China, Taiwan, and South Korea, using ICS symptom definitions [1].
Methods
Study Design and Population
This was a cross-sectional, population-representative, Internet-based study conducted among men and women aged at least 40 years in China, Taiwan, and South Korea between June 2, 2015 and July 20, 2015. Ability to access the Internet, to use a computer (with help, if required), and to read the local language were inclusion criteria. Participants who were pregnant at the time of the survey or who had a urinary tract infection within the preceding month were excluded.
As this study was based on a survey, it was not considered necessary to submit for institutional review board approval. However, principles of the Declaration of Helsinki were followed; the study was performed in compliance with Good Clinical Practice and market research guidelines (Appendix 1 in the online supplementary material). All participants provided informed consent before participating in the study.
Prior to use, quality checks and analysis were undertaken during six cycles of survey testing using a team of researchers with a healthcare background. Participants were selected via consumer survey panels (e-mail invitations automatically randomized to prevalidated individuals) that were actively managed to represent the target population, with respect to age, sex, and socioeconomic factors. Cohort management accounted for sex, income, age group, and geography, with the last of these restricted to urban areas. Participants received a secure link and log-in details to access the survey and had to provide informed consent before they could start to answer questions. Weekly reminders were sent during the survey timeframe to those who had not completed the survey. The questionnaire was over a total of 111 screens, including the informed consent page. Selection of one response was enforced for all questions apart from the optional section concerning sexual health. While undertaking the survey and before submission of the completed survey respondents were able to review and change their answers using a back button.
Proprietary algorithms and browser finger-printing technology involving IP address recognition were used to block the same person from responding multiple times to the survey by using different user credentials (avoiding the need to analyze log file data) and for anyone proceeding too fast through the survey (completion time less than 30% of the median length of the survey). De-identification of data was undertaken, with only a numerical identification available for analysis. Checking for contradictory answers was completed by healthcare analysts’ post-data collection and all responses were valid.
Endpoints
A sample of the survey is presented in the online supplementary material (Appendix 2). Participants were asked eight screening and general demographic questions, including sex, age, marital status, level of education, and employment status. Nine questions were used to evaluate general health and medical comorbidities. For some personal questions, such as marital status, respondents were given the option not to answer. Instruments/topics included the international prostate symptom score (IPSS), other ICS symptoms questions (related to splitting/spraying, hesitancy, terminal dribble, urgency), and the patient perception of bladder condition (PPBC). All instruments were validated in the local language. Further details about each scale are included in Appendix 3 in the online supplementary material.
Presence of LUTS was defined as the presence of voiding, storage, or post-micturition symptom(s) with a frequency of at least one in five times. This was in accordance with ICS criteria, except that nocturia was defined as at least two episodes per night during the preceding month (the ICS definition of at least one episode per night could lead to an artificially high LUTS prevalence in the general population) [1]. Additional information was collected, such as comorbidities, visits to healthcare professionals, and current medication.
The primary objective was to determine LUTS prevalence in the population aged at least 40 years, in China, Taiwan, and South Korea, using ICS 2002 symptom definition (presence of at least one of voiding, storage, or post-micturition symptoms) [1]. Secondary objectives included assessment of the symptom-specific bother of LUTS and exploration of the differences in prevalence of LUTS across men and women, age groups, different socioeconomic strata, and countries.
Statistical Analysis
To estimate the proportion of patients with a given response to LUTS to a precision of five percentage points, it was calculated that at least 384 respondents per group was needed. For analysis of five age groups, a minimum sample size of 1920 per country (5760 in total) was required. Assuming that approximately 28% of data would be non-evaluable due to missing or inconsistent information, total enrollment of 8000 respondents was planned across the three countries.
The initial data analyses were based on descriptive statistics. Post-stratification weighting matched the population distribution (age and sex) per country. Post hoc statistical comparisons were based on the Chi square test, with the exception of differences in LUTS prevalence (based on ICS criteria) according to work status, which were assessed using Fisher’s exact test. The Spearman method was used to investigate the relationship between IPSS and PPBC.
Results
Survey Sample
The survey sample and response rate are provided in Table S1 in the online supplementary material. Of the 8284 survey participants, 50.8% were women and 34.4% were aged at least 60 years (Table 1). Most respondents (approximately 90%) answered all of the questions.
Table 1.
Participants’ demographic data
| China (n = 4136) (%) | Taiwan (n = 2068) (%) | South Korea (n = 2080) (%) | Overall (n = 8284) (%) | |
|---|---|---|---|---|
| Sex | ||||
| Men | 50.3 | 48.6 | 47.6 | 49.2 |
| Women | 49.7 | 51.4 | 52.4 | 50.8 |
| Age group | ||||
| 40–44 years | 19.9 | 15.6 | 16.9 | 18.1 |
| 45–49 years | 19.6 | 16.1 | 16.8 | 18.0 |
| 50–54 years | 15.3 | 16.3 | 16.3 | 15.8 |
| 55–59 years | 12.7 | 14.9 | 14.4 | 13.7 |
| ≥60 years | 32.6 | 37.1 | 35.6 | 34.4 |
| Education | ||||
| High-school or less | 28.0 | 39.3 | 30.3 | 31.4 |
| Some college | 28.4 | 23.7 | 3.4 | 20.9 |
| College degree/college graduate | 40.2 | 28.2 | 57.0 | 41.4 |
| Postgraduate | 3.5 | 8.8 | 9.4 | 6.3 |
| Marital status | ||||
| Single | 2.9 | 14.9 | 9.2 | 7.5 |
| Divorced | 1.5 | 5.2 | 4.0 | 3.0 |
| Married/living with partner | 91.7 | 72.8 | 81.6 | 84.5 |
| Widow/widower | 3.2 | 6.3 | 4.5 | 4.3 |
| Prefer not to answer | 0.8 | 0.7 | 0.7 | 0.7 |
| Work status | ||||
| Homemaker | 2.6 | 12.0 | 22.4 | 9.9 |
| Retired | 28.7 | 16.9 | 6.0 | 20.1 |
| Student | 0.0 | 0.1 | 0.2 | 0.1 |
| Working, full-time | 62.6 | 60.0 | 53.9 | 59.8 |
| Working, part-time | 3.7 | 6.2 | 8.0 | 5.4 |
| Other work for pay | 0.4 | 0.8 | 3.2 | 1.2 |
| Other | 1.1 | 1.9 | 3.7 | 2.0 |
| Unemployed | 0.6 | 1.3 | 2.3 | 1.2 |
| Permanently disabled/cannot work because of ill health | 0.1 | 0.8 | 0.4 | 0.4 |
Overall Prevalence
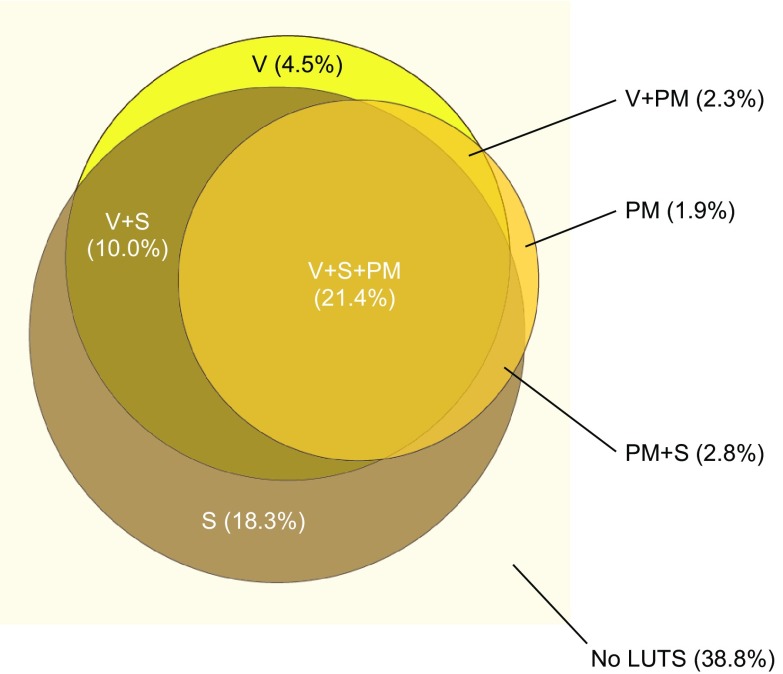
The overall prevalence of LUTS according to ICS criteria was 61.2% (Fig. 1). Prevalence in South Korea (68.2%) was higher than in China (59.0%) or Taiwan (58.5%) (p = 0.001). In participants with LUTS, the most common combination of ICS symptom groups was all three groups (35.0%); post-micturition symptoms only or voiding symptoms only were experienced by 3.0% and 7.3%. Storage symptoms commonly occurred alone (29.9% of participants with LUTS).
Fig. 1.
Prevalence of LUTS according to ICS symptom definitions (overall population, N = 8284). In total, 61.2% of patients had any LUTS. ICS International Continence Society, LUTS lower urinary tract symptoms, PM post-micturition symptoms, S storage symptoms, V voiding symptoms
Prevalence by Demographic Characteristics
LUTS were more prevalent among men (62.8%) than women (59.7%) (p = 0.004; Table 2). Prevalence of storage symptoms only was higher in women than men (23.8% versus 12.6%, respectively). Conversely, more men had voiding symptoms only (7.2%) or post-micturition symptoms only (2.1%) than women (1.8% and 1.6%, respectively). LUTS prevalence increased significantly with age from 49.9% (age 40–44 years) to 69.7% (age over 60 years) in the overall population (p = 0.001; Table 2); this trend was more marked among women than men in China and Taiwan, but it was not evident in South Korean participants. LUTS prevalence was affected by marital and work status (p = 0.001 for both) but not education (Table 2). Marital status with the highest LUTS prevalence was being a widow or widower (66.8%) and that with the lowest prevalence was being single (54.1%). Regarding work status, LUTS prevalence was highest among permanently disabled individuals or those unable to work because of ill health (84.6%), and lowest among students (48.8%).
Table 2.
Prevalence of LUTS according to ICS criteria, by demographics (overall population, N = 8284)
| Demographic group | No LUTS | Voiding only | Storage only | PM only | Voiding + storage | Voiding + PM | Storage + PM | Voiding + storage + PM | Any LUTS |
|---|---|---|---|---|---|---|---|---|---|
| Sex | |||||||||
| Men | 1516 (37.2%) | 293 (7.2%) | 512 (12.6%) | 87 (2.1%) | 438 (10.7%) | 148 (3.6%) | 113 (2.8%) | 968 (23.8%) | 2559 (62.8%) |
| Women | 1698 (40.3%) | 77 (1.8%) | 1003 (23.8%) | 67 (1.6%) | 393 (9.3%) | 42 (1%) | 121 (2.9%) | 808 (19.2%) | 2511 (59.7%) |
| Age group | |||||||||
| 40–44 years | 749 (50.1%) | 66 (4.4%) | 262 (17.5%) | 30 (2%) | 131 (8.7%) | 31 (2.1%) | 36 (2.4%) | 192 (12.8%) | 748 (49.9%) |
| 45–49 years | 670 (44.9%) | 67 (4.5%) | 301 (20.2%) | 26 (1.8%) | 124 (8.3%) | 32 (2.1%) | 40 (2.7%) | 231 (15.5%) | 821 (55.1%) |
| 50–54 years | 525 (40%) | 77 (5.9%) | 248 (19%) | 22 (1.6%) | 134 (10.2%) | 36 (2.7%) | 35 (2.7%) | 235 (17.9%) | 786 (60%) |
| 55–60 years | 407 (35.9%) | 49 (4.4%) | 169 (14.9%) | 25 (2.2%) | 110 (9.7%) | 27 (2.4%) | 30 (2.6%) | 316 (27.9%) | 726 (64.1%) |
| >60 years | 863 (30.3%) | 112 (3.9%) | 536 (18.8%) | 51 (1.8%) | 332 (11.6%) | 64 (2.2%) | 93 (3.3%) | 803 (28.1%) | 1990 (69.7%) |
| Education | |||||||||
| High-school or less | 1015 (39%) | 109 (4.2%) | 534 (20.6%) | 48 (1.8%) | 279 (10.7%) | 38 (1.5%) | 85 (3.3%) | 492 (18.9%) | 1584 (61%) |
| Some college | 692 (39.9%) | 68 (3.9%) | 285 (16.4%) | 28 (1.6%) | 160 (9.2%) | 37 (2.1%) | 48 (2.8%) | 417 (24%) | 1043 (60.1%) |
| College degree/college graduate | 1295 (37.8%) | 174 (5.1%) | 614 (17.9%) | 68 (2%) | 341 (9.9%) | 87 (2.5%) | 93 (2.7%) | 757 (22.1%) | 2134 (62.2%) |
| Postgraduate | 212 (40.7%) | 19 (3.7%) | 81 (15.5%) | 11 (2.1%) | 52 (9.9%) | 27 (5.2%) | 8 (1.6%) | 111 (21.3%) | 309 (59.3%) |
| Marital status | |||||||||
| Single | 284 (45.9%) | 28 (4.5%) | 133 (21.5%) | 10 (1.6%) | 57 (9.2%) | 15 (2.3%) | 16 (2.5%) | 77 (12.5%) | 335 (54.1%) |
| Divorced | 93 (37%) | 17 (6.9%) | 50 (19.9%) | 6 (2.4%) | 24 (9.6%) | 6 (2.2%) | 10 (3.8%) | 46 (18.2%) | 158 (63%) |
| Married/living with partner | 2695 (38.5%) | 304 (4.3%) | 1230 (17.6%) | 127 (1.8%) | 713 (10.2%) | 164 (2.3%) | 196 (2.8%) | 1567 (22.4%) | 4301 (61.5%) |
| Widow/widower | 118 (33.2%) | 13 (3.7%) | 90 (25.2%) | 11 (3.1%) | 31 (8.7%) | 4 (1.2%) | 12 (3.3%) | 77 (21.6%) | 238 (66.8%) |
| Prefer not to answer | 24 (38.7%) | 8 (12.8%) | 12 (19.3%) | 0 (0%) | 6 (9.7%) | 1 (1.6%) | 2 (2.5%) | 9 (15.4%) | 38 (61.3%) |
| Work status | |||||||||
| Homemaker | 318 (38.7%) | 9 (1.1%) | 235 (28.6%) | 16 (2%) | 90 (10.9%) | 5 (0.6%) | 34 (4.1%) | 116 (14.1%) | 504 (61.3%) |
| Retired | 510 (30.7%) | 66 (4%) | 280 (16.8%) | 25 (1.5%) | 205 (12.3%) | 31 (1.8%) | 52 (3.1%) | 495 (29.8%) | 1152 (69.3%) |
| Student | 5 (51.2%) | 1 (9.7%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 4 (39.1%) | 4 (48.8%) |
| Working, full-time | 2090 (42.2%) | 255 (5.2%) | 820 (16.6%) | 99 (2%) | 458 (9.3%) | 130 (2.6%) | 121 (2.4%) | 976 (19.7%) | 2861 (57.8%) |
| Working, part-time | 165 (36.9%) | 14 (3.2%) | 97 (21.7%) | 6 (1.4%) | 41 (9.2%) | 8 (1.7%) | 11 (2.4%) | 105 (23.5%) | 282 (63.1%) |
| Other work for pay | 28 (28.4%) | 3 (3.3%) | 27 (27.9%) | 6 (5.8%) | 6 (6%) | 3 (2.6%) | 3 (3.3%) | 22 (22.8%) | 70 (71.6%) |
| Other | 55 (34.2%) | 18 (11%) | 31 (19.4%) | 1 (0.7%) | 19 (11.6%) | 8 (5.2%) | 2 (1.1%) | 27 (16.9%) | 106 (65.8%) |
| Unemployed | 39 (38%) | 3 (2.5%) | 22 (21.2%) | 1 (1%) | 9 (8.9%) | 5 (4.7%) | 5 (4.9%) | 19 (18.7%) | 63 (62%) |
| Permanently disabled/cannot work due because of ill health | 5 (15.4%) | 1 (3.1%) | 3 (10.2%) | 0 (0%) | 3 (10.6%) | 0 (0%) | 7 (24%) | 11 (36.7%) | 26 (84.6%) |
Patient numbers are weighted and rounded, and hence may not add up; percentages are based on the weighted ‘n’
Prevalence by Comorbid Conditions
All comorbid conditions analyzed were associated with statistically significantly increased LUTS prevalence (p ≤ 0.001; Fig. S1 in the online supplementary material). Diabetes and neurological disease were associated with the greatest increases in LUTS prevalence between individuals with and without the comorbidity (differences of 26.5% and 26.1%, respectively).
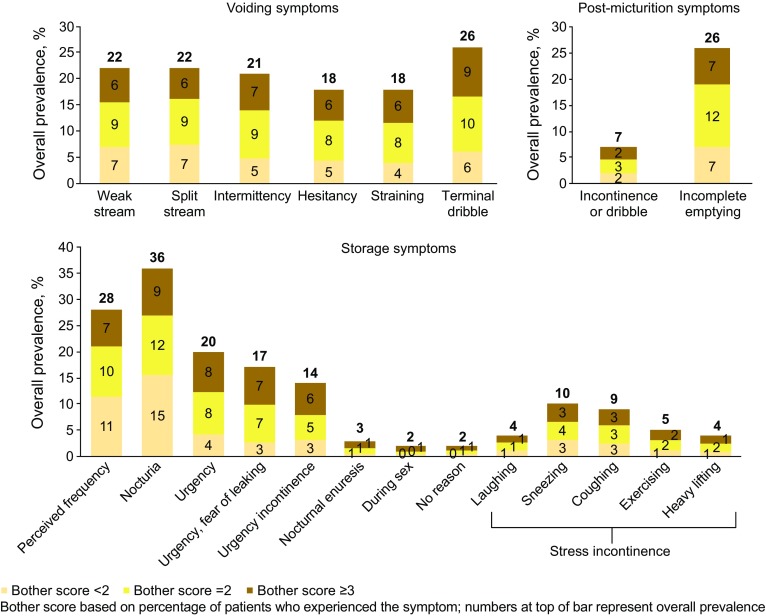
Prevalence of Symptoms and Associated Bother
Symptoms with the highest overall prevalence were nocturia, frequency, incomplete emptying, and terminal dribble (Fig. 2). Symptoms with the largest numbers of patients experiencing “quite a bit or greater” bother were terminal dribble, nocturia, and urgency. Prevalence of nocturia (at least two episodes per night) and extent of associated bother differed little between men and women, with prevalence of 35% and 37% and percentages with “quite a bit or greater” bother of 25% and 26%, respectively.
Fig. 2.
Symptoms and bother, overall population (N = 8284). Data shown are from questions relating to ICS symptom definitions. ICS International Continence Society
According to IPSS, 86.8% of participants had at least mild symptoms (Fig. S2 in the online supplementary material), which was similar across all three countries. Moderate or greater symptoms were reported in 34.0% of respondents and were more common in those aged 55–60 years and over 60 years (39.8% and 43.2%, respectively) than in younger age groups [range 22.9% (respondents aged 40–44 years) to 29.5% (those aged 50–54 years)]. This difference across age groups was statistically significant (p = 0.001). Increasing IPSS symptom severity was associated with worsening PPBC (Table S2 in the online supplementary material; Spearman correlation coefficient 0.734; p = 0.001): 60% of participants with severe IPSS had moderate or greater problems according to PPBC. This pattern was evident among men and women, and across the three countries.
Healthcare Seeking
Twenty-six percent of individuals with any LUTS according to ICS criteria reported visiting healthcare professionals during the previous 12 months because of urinary symptoms. Individuals with voiding, storage, and post-micturition symptoms (45%) had the highest healthcare professional consultation rate (Fig. S3 in the online supplementary material), with the difference versus other ICS symptom groups reaching statistical significance (p = 0.001). The lowest rate was in participants with voiding symptoms only. The percentage of individuals who had visited healthcare professionals because of urinary symptoms increased with IPSS severity (p = 0.001), from 8% (mild) to 63% (severe). A slightly higher rate of healthcare professional consultation was observed in women versus men with LUTS (27% vs. 25% [not statistically significant]). Fifty-nine percent of individuals with LUTS according to ICS criteria were following treatment (Table S3 in the online supplementary material). There were statistically significant differences between ICS symptom groups in this respect (p = 0.001), and the category with the highest percentage of individuals following treatment was voiding plus storage plus post-micturition symptoms (78%).
Discussion
Overall, 61% of participants in this study (individuals aged at least 40 years from China, Taiwan, and South Korea) fulfilled the ICS criteria for LUTS, and bothersome symptoms were common. Over one-third of men and women with LUTS reported all three ICS symptom groups. LUTS prevalence was slightly higher in men than women and tended to increase with increasing age. Only half of individuals with symptoms in all three ICS categories had consulted healthcare professionals about these symptoms. Our results confirm that in three Asian countries there is a lack of patient awareness of LUTS and an unmet need for its diagnosis and treatment, resulting in a significant health burden, as previously noted in Western studies.
LUTS prevalence varied according to work and marital status. Among individuals who are disabled or unable to work because of ill health, LUTS could be related to detrusor overactivity caused by neurological conditions [12]. High prevalence among widows/widowers and low prevalence among students may be attributable to age differences in these groups versus the overall population. Potential contributors to variability between countries include genetic/ethnicity differences (affecting susceptibility to LUTS), and cultural/linguistic differences (affecting the way study questions were answered) [13, 14].
The present LUTS prevalence data appear broadly comparable with population-based studies performed in Europe and North America [8, 9]. However, in these studies, LUTS prevalence appears to be higher in women than men, while we found the opposite was true. In the EPIC study, conducted in over 19,000 individuals aged at least 18 years, LUTS prevalence was 64.3% (men 62.5%; women 66.6%) [9]. The EpiLUTS study (30,000 participants aged at least 40 years) reported LUTS in 72.3% of men and 76.3% of women [8]. As in the present study, ICS criteria were used but direct comparisons are confounded by other differences (e.g., demographics, definition of nocturia). Although no previous international population-based studies have investigated LUTS prevalence in Asia using ICS criteria, previous studies have reported LUTS prevalence in China, South Korea, and Taiwan [10, 11, 15–21]; prevalence rates greater than 50%, consistent with our results, have been reported in China [11, 18, 21] and South Korea [10, 20]. One Chinese study involved 3023 participants aged at least 18 years who completed the International Consultation on Incontinence Questionnaire Male/Female Lower Urinary Tract Symptoms Long Form [11], while the other two used the Bristol Female Lower Urinary Tract Symptoms questionnaire in women aged at least 40 years [18] and those aged at least 20 years with selected LUTS symptoms [21]. Participants of one of the South Korean studies were men and women aged at least 18 years, and LUTS prevalence was based on ICS criteria with a nocturia cutoff of at least one episode per night [10], while the second study involved men aged at least 40 years, with LUTS prevalence determined using ICS criteria and nocturia defined as at least two episodes per night [20]. In the remaining four studies, three of which were conducted using the IPSS, LUTS prevalence rates below 30% were reported [15–17, 19]. The extent of variability might be related to differences between countries in clinical practice, the use of different assessment techniques (e.g., one study assessed only urinary frequency [15]), or small sample sizes. Also, in three of the low-prevalence studies, LUTS was assessed using IPSS; although this scale was originally validated for assessing male LUTS, it has subsequently been validated in women, including Asian women [22, 23]. While it may be helpful to determine severity of LUTS, the IPSS does not evaluate incontinence or post-micturition symptoms, and storage and emptying symptoms do not necessarily reflect disorders of storage and voiding function [24]. Hence, data based on the IPSS are often evaluated in conjunction with those from other assessment tools.
Approximately three-quarters of individuals with LUTS did not visit a healthcare professional in relation to their symptoms and LUTS was untreated in 41% of cases. The reasons for low consultation rates are varied, but they may be attributable to stigma, beliefs that LUTS occur naturally with ageing, and perceptions that LUTS are not curable or treatable [25–27]. The belief that symptoms are a minor problem may also affect the need to seek help [25]; indeed in Chinese women with urinary incontinence, seeking professional help was associated more with the perceived level of bother than with symptom severity [27]. Among individuals with LUTS, a slightly higher percentage of women than men reported visiting healthcare professionals because of urinary symptoms. This difference could be related to an increased frequency of visits to healthcare professionals for any reason among women. There is a need to encourage increased uptake of healthcare for LUTS, to reduce the impact on individuals’ QoL. Pharmacoeconomic analysis is beyond the scope of this study, but untreated LUTS have financial as well as QoL effects (e.g., decreased workplace productivity) [28].
Potential strengths of our study include the large sample size, well-balanced demographic characteristics (e.g., similar numbers of men and women), and a comparison between three countries. The instruments used in our study are well established and validated [22, 23, 29–31]. Conducting the study via the Internet was cost-efficient and suitable for asking questions of a sensitive or personal nature. However, this approach may result in bias by only including individuals with Internet access. We selected China, South Korea, and Taiwan on the basis of the highest Internet penetration rates within Asia in 2015 (50%, 92%, and 84%, respectively) [32]. National statistics suggest that our study may be biased towards individuals of a higher socioeconomic class, particularly those with a higher educational level [33–36], although income was more aligned [37–39]. This is unsurprising given the different populations and cutoff points between our study and national statistics. Nevertheless, a survey on Internet development in China reported that 22.1% of those using the Internet used online medical services, the most common of which was seeking healthcare information before seeing a doctor [40]. This suggests that the Internet may have a considerable impact on general health and healthcare. Further potential disadvantages were the use of a consumer panel, which is prone to volunteer bias, restriction to urban areas, and the lack of background data to allow more detailed analysis of the results. Nevertheless, we feel that the data emphasize important epidemiological messages that set the scene for further work and more detailed pharmacoepidemiological research across the region.
Conclusions
LUTS are present in the majority of men and women aged at least 40 years in China, Taiwan, and South Korea. Bothersome storage symptoms (the OAB symptom complex) are common, occurring in at least 50% of those with LUTS, and LUTS prevalence increases with increasing age. Comorbid conditions, particularly diabetes and neurological disease, are associated with increased risk of LUTS. Only 26% of individuals with LUTS seek healthcare and our results suggest there is a need for increased patient awareness of LUTS, its diagnosis, and treatment.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to thank the participants of the study for their time, Nanjangud Shankar Narasimhamurthy and Koni Raviprakash for statistical analyses, and Dr Ming Liu for intellectual input into the manuscript. This study was funded by Astellas Pharma Singapore Pte. Ltd. Editorial support, including writing assistance, was provided by Ken Sutor, BSc and Jackie van Bueren, BSc of Envision Scientific Solutions. Astellas Pharma Global Development, Chertsey, UK funded editorial support, article processing charges, and the open access fee. This study has been published in part in abstract form as a podium presentation at the annual ICS meeting in Tokyo, Japan, 14 September 2016; Chapple C et al. Cross-sectional, Internet-based survey to estimate prevalence of LUTS in China, Taiwan and South Korea (LUTS Asia). All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Disclosures
Christopher Chapple has acted as a consultant for Astellas during a meeting to discuss the publications from the study. David Castro-Diaz has acted as a consultant for Astellas during a meeting to discuss the publications from the study. Yao- Chi Chuang has acted as a consultant for Astellas during a meeting to discuss the publications from the study. Kyu-Sung Lee has acted as a consultant for Astellas during a meeting to discuss the publications from the study. Limin Liao has acted as a consultant for Astellas during a meeting to discuss the publications from the study. Shih-Ping Liu has acted as a consultant for Astellas during a meeting to discuss the publications from the study. Jianye Wang has acted as a consultant for Astellas during a meeting to discuss the publications from the study. Tag Keun Yoo has acted as a consultant for Astellas during a meeting to discuss the publications from the study. Romeo Chu has acted as a consultant for Astellas during a meeting to discuss the publications from the study. Budiwan Sumarsono has acted as a consultant for Astellas during a meeting to discuss the publications from the study. Tag Keun Yoo has received grants and personal fees from Astellas to act as a consultant to Astellas. Romeo Chu is a former employee of Astellas. Budiwan Sumarsono is an employee of Astellas.
Compliance with Ethics Guidelines
As this study was based on a survey, it was not considered necessary to submit for institutional review board approval. The study was performed in compliance with Good Clinical Practice and market research guidelines (Appendix 1 in the online supplementary material). All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2013. Informed consent was obtained from all patients being included in the study.
Data Availability
All data generated or analyzed during this study are included in this published article/as supplementary information files.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Footnotes
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/BD98F060172EF0B3.
References
- 1.Abrams P, Cardozo L, Fall M, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002;21(2):167–178. doi: 10.1002/nau.10052. [DOI] [PubMed] [Google Scholar]
- 2.Roehrborn CG, McConnell JD, Saltzman B, et al. Storage (irritative) and voiding (obstructive) symptoms as predictors of benign prostatic hyperplasia progression and related outcomes. Eur Urol. 2002;42(1):1–6. doi: 10.1016/S0302-2838(02)00210-5. [DOI] [PubMed] [Google Scholar]
- 3.Gravas S, Bach T, Drake M, et al. Treatment of non-neurogenic male LUTS. http://uroweb.org/guideline/treatment-of-non-neurogenic-male-luts/. Accessed 9 May 2017.
- 4.Ju R, Garrett J, Wu JM. Anticholinergic medication use for female overactive bladder in the ambulatory setting in the United States. Int Urogynecol J. 2014;25(4):479–484. doi: 10.1007/s00192-013-2246-0. [DOI] [PubMed] [Google Scholar]
- 5.Coyne KS, Sexton CC, Kopp ZS, Ebel-Bitoun C, Milsom I, Chapple C. The impact of overactive bladder on mental health, work productivity and health-related quality of life in the UK and Sweden: results from EpiLUTS. BJU Int. 2011;108(9):1459–1471. doi: 10.1111/j.1464-410X.2010.10013.x. [DOI] [PubMed] [Google Scholar]
- 6.Kim TH, Han DH, Ryu DS, Lee KS. The impact of lower urinary tract symptoms on quality of life, work productivity, depressive symptoms, and sexuality in Korean men aged 40 years and older: a population-based survey. Int Neurourol J. 2015;19(2):120–129. doi: 10.5213/inj.2015.19.2.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stewart WF, Van Rooyen JB, Cundiff GW, et al. Prevalence and burden of overactive bladder in the United States. World J Urol. 2003;20(6):327–336. doi: 10.1007/s00345-002-0301-4. [DOI] [PubMed] [Google Scholar]
- 8.Coyne KS, Sexton CC, Thompson CL, et al. The prevalence of lower urinary tract symptoms (LUTS) in the USA, the UK and Sweden: results from the Epidemiology of LUTS (EpiLUTS) study. BJU Int. 2009;104(3):352–360. doi: 10.1111/j.1464-410X.2009.08427.x. [DOI] [PubMed] [Google Scholar]
- 9.Irwin DE, Milsom I, Hunskaar S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006;50(6):1306–1314. doi: 10.1016/j.eururo.2006.09.019. [DOI] [PubMed] [Google Scholar]
- 10.Lee YS, Lee KS, Jung JH, et al. Prevalence of overactive bladder, urinary incontinence, and lower urinary tract symptoms: results of Korean EPIC study. World J Urol. 2011;29(2):185–190. doi: 10.1007/s00345-009-0490-1. [DOI] [PubMed] [Google Scholar]
- 11.Wang Y, Hu H, Xu K, Wang X, Na Y, Kang X. Prevalence, risk factors and the bother of lower urinary tract symptoms in China: a population-based survey. Int Urogynecol J. 2015;26(6):911–919. doi: 10.1007/s00192-015-2626-8. [DOI] [PubMed] [Google Scholar]
- 12.Torelli F, Terragni E, Blanco S, Di Bella N, Grasso M, Bonaiuti D. Lower urinary tract symptoms associated with neurological conditions: observations on a clinical sample of outpatients neurorehabilitation service. Arch Ital Urol Androl. 2015;87(2):154–157. doi: 10.4081/aiua.2015.2.154. [DOI] [PubMed] [Google Scholar]
- 13.Hoke GP, McWilliams GW. Epidemiology of benign prostatic hyperplasia and comorbidities in racial and ethnic minority populations. Am J Med. 2008;121(8 Suppl 2):S3–S10. doi: 10.1016/j.amjmed.2008.05.021. [DOI] [PubMed] [Google Scholar]
- 14.Maserejian NN, Chen S, Chiu GR, et al. Incidence of lower urinary tract symptoms in a population-based study of men and women. Urology. 2013;82(3):560–564. doi: 10.1016/j.urology.2013.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hsieh CH, Chen HY, Hsu CS, Chang ST, Kuo TC, Chiang CD. Prevalence of urinary frequency in Taiwanese women aged 20-59 years. Taiwan J Obstet Gynecol. 2006;45(3):244–246. doi: 10.1016/S1028-4559(09)60233-3. [DOI] [PubMed] [Google Scholar]
- 16.Lee E, Yoo KY, Kim Y, Shin Y, Lee C. Prevalence of lower urinary tract symptoms in Korean men in a community-based study. Eur Urol. 1998;33(1):17–21. doi: 10.1159/000019529. [DOI] [PubMed] [Google Scholar]
- 17.Liang GQ, Zhang SJ, Wang B, et al. Lower urinary tract symptoms and prostatic growth pattern among old and middle-aged males in Shanghai community. Zhonghua Nan Ke Xue. 2012;18(10):886–890. [PubMed] [Google Scholar]
- 18.Zhang W, Song Y, He X, et al. Prevalence and risk factors of lower urinary tract symptoms in Fuzhou Chinese women. Eur Urol. 2005;48(2):309–313. doi: 10.1016/j.eururo.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 19.Yu HJ, Chiang GJ, Chie WC, et al. Prevalence of LUTS in men—a community-based study in Taiwan. J Taiwan Urol Assoc. 1995;6:7–12. [Google Scholar]
- 20.Kim TH, Han DH, Lee KS. The prevalence of lower urinary tract symptoms in Korean men aged 40 years or older: a population-based survey. Int Neurourol J. 2014;18(3):126–132. doi: 10.5213/inj.2014.18.3.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang L, Zhu L, Xu T, et al. A population-based survey of the prevalence, potential risk factors, and symptom-specific bother of lower urinary tract symptoms in adult Chinese women. Eur Urol. 2015;68(1):97–112. doi: 10.1016/j.eururo.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 22.Choi EP, Lam CL, Chin WY. Validation of the international prostate symptom score in Chinese males and females with lower urinary tract symptoms. Health Qual Life Outcomes. 2014;12:1. doi: 10.1186/1477-7525-12-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hsiao SM, Lin HH, Kuo HC. International prostate symptom score for assessing lower urinary tract dysfunction in women. Int Urogynecol J. 2013;24(2):263–267. doi: 10.1007/s00192-012-1818-8. [DOI] [PubMed] [Google Scholar]
- 24.Madersbacher S, Pycha A, Klingler CH, Schatzl G, Marberger M. The international prostate symptom score in both sexes: a urodynamics-based comparison. Neurourol Urodyn. 1999;18(3):173–182. doi: 10.1002/(SICI)1520-6777(1999)18:3<173::AID-NAU3>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 25.Choi H, Park JY, Yeo JK, et al. Population-based survey on disease insight, quality of life, and health-seeking behavior associated with female urinary incontinence. Int Neurourol J. 2015;19(1):39–46. doi: 10.5213/inj.2015.19.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang C, Li J, Wan X, Wang X, Kane RL, Wang K. Effects of stigma on Chinese women’s attitudes towards seeking treatment for urinary incontinence. J Clin Nurs. 2015;24(7–8):1112–1121. doi: 10.1111/jocn.12729. [DOI] [PubMed] [Google Scholar]
- 27.Xu D, Wang X, Li J, Wang K. The mediating effect of ‘bothersome’ urinary incontinence on help-seeking intentions among community-dwelling women. J Adv Nurs. 2015;71(2):315–325. doi: 10.1111/jan.12514. [DOI] [PubMed] [Google Scholar]
- 28.Azam U, Castleden M, Turner D. Economics of lower urinary tract symptoms (LUTS) in older people. Drugs Aging. 2001;18(3):213–223. doi: 10.2165/00002512-200118030-00006. [DOI] [PubMed] [Google Scholar]
- 29.Barry MJ, Fowler FJ, Jr, O’Leary MP, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol. 1992;148(5):1549–1557. doi: 10.1016/S0022-5347(17)36966-5. [DOI] [PubMed] [Google Scholar]
- 30.Coyne KS, Matza LS, Kopp Z, Abrams P. The validation of the patient perception of bladder condition (PPBC): a single-item global measure for patients with overactive bladder. Eur Urol. 2006;49(6):1079–1086. doi: 10.1016/j.eururo.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 31.Jeong SJ, Homma Y, Oh SJ. Korean version of the overactive bladder symptom score questionnaire: translation and linguistic validation. Int Neurourol J. 2011;15(3):135–142. doi: 10.5213/inj.2011.15.3.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Internet World Stats. Internet usage in Asia. http://www.internetworldstats.com/. Accessed 1 Feb 2016.
- 33.National Bureau of Statistics of China. China statistical yearbook. http://www.stats.gov.cn/tjsj/ndsj/2015/indexeh.htm. Accessed 1 Feb 2017.
- 34.Organisation for Economic Co-operation and Development. Country statistical profiles: Korea. http://stats.oecd.org/. Accessed 1 Feb 2017.
- 35.Taiwan Ministry of the Interior. Statistical data from The Taiwan Ministry of the Interior; Mar 2012.
- 36.Taiwan Ministry of the Interior. Statistical data from The Taiwan Ministry of the Interior; 12 Mar 2016.
- 37.McKinsey & Company. Mapping China’s middle class. http://www.mckinsey.com/industries/retail/our-insights/mapping-chinas-middle-class. Accessed 1 Feb 2017.
- 38.Choi S-k, Lee J-h. Changes in the quality of life of Korea’s middle class. http://www.koreafocus.or.kr/design2/layout/content_print.asp?group_id=105791. Accessed 1 Feb 2017.
- 39.Pew Research Center. World population by income. http://www.pewglobal.org/interactives/global-population-by-income/. Accessed 1 Feb 2017.
- 40.China Internet Network Information Center. The 37th statistical report on Internet development in China. https://cnnic.com.cn/IDR/ReportDownloads/201604/P020160419390562421055.pdf. Accessed 10 May 2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this published article/as supplementary information files.