Abstract
Objective
To assess whether foot and/or ankle symptoms are associated with an increased risk of worsening of knee pain and radiographic change in people with knee osteoarthritis (OA).
Methods
The presence and laterality of foot/ankle symptoms were recorded at baseline in 1368 participants from the Osteoarthritis Initiative with symptomatic radiographic knee OA. Knee pain severity (measured using the Western Ontario and McMaster Universities Osteoarthritis Index pain subscale) and minimum medial tibiofemoral joint space (minJSW) width measured on x-ray were assessed yearly over the subsequent four years. Associations between foot/ankle symptoms and worsening of (i) knee pain, and (ii) both knee pain and minJSW (i.e. symptomatic radiographic knee OA) were assessed using logistic regression.
Results
Foot/ankle symptoms in either foot/ankle significantly increased the odds of knee pain worsening (adjusted OR 1.54, 95% CI 1.25 to 1.91). Laterality analysis showed ipsilateral (adjusted OR 1.50, 95% CI 1.07 to 2.10), contralateral (adjusted OR 1.44, 95% CI 1.02 to 2.06) and bilateral foot/ankle symptoms (adjusted OR 1.61, 95% CI 1.22 to 2.13) were all associated with knee pain worsening in the follow up period. There was no association between foot/ankle symptoms and worsening of symptomatic radiographic knee OA.
Conclusion
The presence of foot/ankle symptoms in people with symptomatic radiographic knee OA was associated with increased risk of knee pain worsening, but not worsening of symptomatic radiographic knee OA, over the subsequent four years. Future studies should investigate whether treatment of foot/ankle symptoms reduces the risk of knee pain worsening in people with knee OA.
Keywords: Knee Osteoarthritis, Arthritis, Epidemiology, Foot, Ankle, Pain
Knee osteoarthritis (OA) is a major public health problem that causes substantial pain, physical dysfunction and impaired quality-of-life. There is no cure for knee OA and the disease often progresses to advanced stages. Although there is a discordance between knee pain and joint deterioration1, both are drivers of costly joint replacement surgery2. Therefore, it is important to identify risk factors that are associated with the worsening of knee symptoms, with and without concurrent structural deterioration, in an attempt to prevent disease progression.
Researchers have identified a number of risk factors for the worsening of knee OA symptoms and structure, such as age, ethnicity and malalignment3, 4, however modifiable risk factors are required to prevent progression to advanced disease and/or surgery. To date, the strongest known modifiable risk factors for worsening of knee pain in people with knee OA are a higher body mass index (BMI) and infrapatellar fat pad or intercondylar synovitis4, whilst a recent meta-analysis identified greater knee pain at baseline as the only modifiable risk factor associated with structural progression3. Although these risk factors are potentially modifiable, weight loss interventions have poor compliance and limited long-term success5 and the remaining risk factors are likely to be symptoms or sequelae of OA and thus it is unclear whether targeted treatment would slow disease progression.
A potential risk factor for worsening knee OA that has not been investigated is foot/ankle symptoms. Concurrent symptoms at the foot, ankle and knee occur more often than any other multi-joint pain presentation, and their co-occurrence substantially increases the risk of problems with walking, standing and rising from sitting compared to single- and other multi-joint symptoms6. In people with knee OA, cross-sectional studies have shown that the presence of foot/ankle symptoms is also associated with worse knee symptoms, health-related quality-of-life, depressive symptoms and functional abilities7. More recently, our longitudinal study showed that foot/ankle symptoms are an independent risk factor for developing knee OA in people free of the disease but at risk 8. Potential mechanisms linking foot/ankle symptoms and incident knee OA, such as foot pronation, inappropriate footwear or widespread pain8, may also increase the risk for worsening in those with OA. However, as incident disease is a different phenomenon to worsening OA and risk factors may not be consistent across both, it is necessary to separately establish the association of foot/ankle symptoms with worsening OA. This is important as worse knee pain and greater radiographic severity are predictors of progression to arthroplasty2. Knowledge of risk factors in those with knee OA can provide insight into why the disease progresses in some individuals but not others and help identify potential new treatment targets for future clinical trials10. Therefore, the aim of this study was to investigate whether the presence of foot/ankle symptoms at baseline is associated with an increased risk of worsening of (i) knee pain, and (ii) both knee pain and radiographic change, in people with symptomatic radiographic knee OA.
Methods
Study population
Data were obtained from the Osteoarthritis Initiative (OAI), an online and publically available database (http://www.oai.ecsf.edu/). The OAI is a prospective multi-centre cohort study of 4796 participants aged between 45-79 years who have existing knee OA, or who are considered at-risk of the disease. The participants were recruited from four sites throughout the United States including Baltimore, Maryland; Columbus, Ohio; Pittsburgh, Pennsylvania; and Pawtucket, Rhode Island. The institutional review board at each site approved all protocols and procedures and all participants provided informed consent. Further details regarding the wider OAI study protocols can be found online11. Our study included OAI participants with established symptomatic radiographic knee OA (n=1368), defined as both knee symptoms (pain, aching or stiffness in and around the knee on most days of the month for at least one month in the previous year12) and radiographic evidence of knee OA (Kellgren and Lawrence [KL] grade ≥2) in at least one knee. If knee OA was present in both knees then both were included in the analyses.
Demographic characteristics and covariates
Demographic characteristics collected included age, sex and race (White, Black/African American or Asian/other non-white). Covariates included BMI, baseline Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain, depression measured using the Centre for Epidemiological Studies Depression Scale (CES-D)13, worst baseline KL grade, baseline minimum medial tibiofemoral joint space width (minJSW), baseline tibial rim distance (defined as the distance between the anterior or posterior margin of the tibia, and the tibial margin of the joint space), and comorbidities assessed using the questionnaire version of the Charlson comorbidity index (CCI)14. The CCI derives a weighted score based on the presence or absence of 14 different comorbidities such as stroke, diabetes, asthma, and kidney failure, amongst others, and we dichotomised the cohort into those with ‘no comorbidities’ (CCI=0) and those with ‘one or more comorbidities’ (CCI≥1) based on the total CCI score. Data on individual comorbidities is provided in supplementary Table 1. For descriptive purposes, we also classified participants as obese (>30 kg/m2), overweight (≥25 and ≤30 kg/m2) or healthy weight (<25 kg/m2), Scores on the CES-D were summed and a score of ≥ 16 was used to indicate significant depressive symptoms13.
Foot/ankle symptoms
Self-reported foot/ankle symptoms were recorded for each of the left and right feet at baseline. Foot/ankle symptoms were defined as pain, aching or stiffness in the foot and/or ankle on more than half of the days during the past 30 days, consistent with previously published definitions6, 15. We classified participants as having or not having foot/ankle symptoms, as well as classifying foot/ankle symptoms as ipsilateral, contralateral or bilateral relative to the affected knee.
Outcomes
We investigated worsening of (i) knee pain and; (ii) both knee pain and radiographic knee OA. Knee pain severity was determined using the WOMAC pain subscale at baseline and the 12, 24, 36 and 48 month follow-up visits16. The WOMAC pain subscale is comprised of five items and responses are recorded on a 5-point Likert scale. Scores were summed (range of 0-20) and converted to a 0-100 normalised scale, with higher scores indicating worse pain. We defined knee pain worsening as an increase of at least 9 points on the 0-100 WOMAC pain scale from baseline at any of the subsequent follow up visits, based on previously published smallest detectable difference values17, 18, and consistent with recent definitions used by others investigating risk factors for symptomatic progression in knee OA19. People with a baseline WOMAC pain score >91 (and thus unable to worsen according to this definition) were excluded from these analyses.
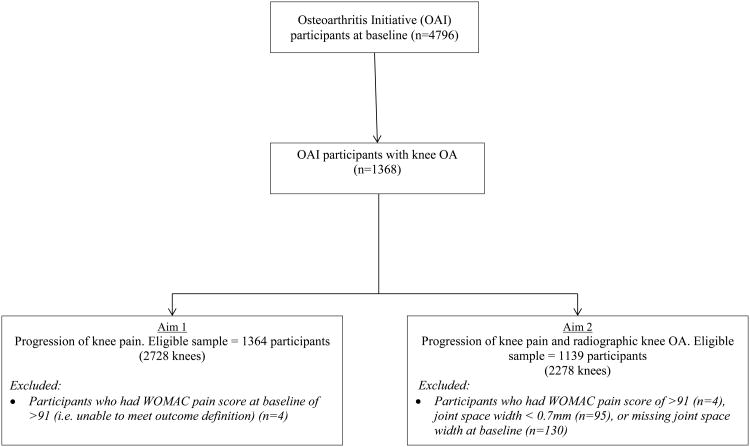
To assess worsening of radiographic knee OA, weightbearing fixed-flexion posteroanterior radiographs of each knee were taken at baseline and at the 12, 24, 36 and 48 month visits. Radiographs were read centrally and automated software was used to identify the tibial and femoral margins of the knee joint from digitised copies of the radiographs20. To determine the minJSW, the software measured the smallest distance between the tibia and the femur in the medial knee joint compartment in millimeters. Worsening of radiographic knee OA was defined as a medial tibiofemoral minJSW decrease of ≥0.7mm from baseline, based on the Osteoarthritis Research Society International and Outcome Measures in Rheumatology minimal detectable difference cut-off value21. People with a baseline minJSW score of <0.7mm (and thus unable to worsen according to this definition) were also excluded from this analysis. A detailed outline of participant inclusion for each of the two aims is presented in Figure 1.
Figure 1.
Flowchart for participant inclusion and exclusion.
Statistical analysis
Descriptive characteristics of all variables at baseline were calculated according to the presence or absence of foot/ankle symptoms. Between-group differences were assessed using χ-squared tests, analysis of variance, Wilcoxon rank-sum or Kruskal-Wallis rank tests as appropriate.
To investigate whether foot/ankle symptoms were associated with worsening of knee pain (aim 1) and worsening of symptomatic radiographic knee OA (aim 2) over the subsequent four years, we used logistic regression models with the presence of foot/ankle symptoms (yes/no) as a binary explanatory variable. Models were fitted using generalized estimating equations to account for the correlation between left and right knees within participants. Models were performed unadjusted, as well as adjusted for baseline covariates determined a priori. The covariates included in the adjusted model for aim 1 were age, sex, BMI, WOMAC pain at baseline, race, depression, worst baseline KL grade, and Charlson Comorbidity index (dichotomised), as these factors are known to be associated with both foot/ankle symptoms and knee OA. Models for aim 2 were also adjusted for the covariates included in the model for aim 1, with baseline minJSW and baseline tibial rim distance also included.
Unadjusted and adjusted analyses were then repeated to investigate the association between ipsilateral, contralateral and bilateral foot/ankle symptoms at baseline and the worsening of knee pain and worsening of symptomatic radiographic knee OA. Logistic regression models were again fitted using generalized estimating equations to adjust for clustering of knees within participants. Significance was set at p-value ≤ 0.05 and Stata v12 (Stata Corporation, College Station, TX, USA) was used for all statistical analyses.
Results
Sample characteristics
Four participants were excluded due to having a baseline WOMAC pain score of >91 in at least one knee, leaving data from 1364 participants. For aim 2, an additional 95 participants with minJSW < 0.7mm were excluded, as were 130 participants with missing minJSW, leaving 1139 participants for aim 2 analyses. People with foot/ankle symptoms were more likely to be female (p<0.001), younger (p=0.038), have a higher BMI (p=0.001) and to report more comorbidities (p=0.016), worse WOMAC knee pain score (p<0.001) and more depressive symptoms (p<0.001) at baseline than those without foot/ankle symptoms. There were no differences in race, worst KL grade, or minJSW at baseline between those with and without foot/ankle symptoms. Data are presented in Table 1.
Table 1.
Baseline characteristics of participants according to the presence of foot/ankle symptoms. One participant had missing foot/ankle symptoms status at baseline. Values are N (%) unless otherwise indicated.
| Characteristic | Missing (n) | No foot/ankle symptoms (n=1013) | Any foot/ankle symptoms (n=351) | P value† |
|---|---|---|---|---|
| Sex | 0 | <0.001 | ||
| Male | 477 (47.1) | 113 (32.2) | ||
| Female | 536 (52.9) | 238 (67.8) | ||
| Mean (SD) age (years) | 0 | 61.6 (9.1) | 60.6 (8.6) | 0.038 |
| Race: | 1 | 0.106 | ||
| Asian and other non-white | 33 (3.3) | 8 (2.3) | ||
| White/Caucasian | 723 (71.4) | 234 (66.9) | ||
| Black/African American | 257 (25.4) | 108 (30.9) | ||
| Comorbidities: | 0 | 0.016 | ||
| 0 | 711 (70.2) | 222 (63.2) | ||
| ≥1 | 302 (29.8) | 129 (36.8) | ||
| Median (IQR) BMI kg/m2 | 3 | 29.4 (26.4, 33.0) | 31 (27.3, 34.5) | <0.001 |
| BMI categories: | 3 | 0.001 | ||
| Healthy weight (BMI <25 kg/m2) | 151 (15.0) | 29 (8.3) | ||
| Overweight (BMI 25-30 kg/m2) | 393 (38.9) | 126 (35.9) | ||
| Obese (BMI >30 kg/m2) | 466 (46.1) | 196 (55.8) | ||
| Worst KL grade* | 0 | 0.080 | ||
| 0 | 0 (0) | 0 (0) | ||
| 1 | 0 (0) | 0 (0) | ||
| 2 | 441 (43.5) | 173 (49.3) | ||
| 3 | 402 (39.7) | 134 (38.2) | ||
| 4 | 170 (16.8) | 44 (12.5) | ||
| Median (IQR) highest WOMAC pain score* | 0 | 25 (10, 40) | 35 (20, 50) | <0.001 |
| Mean (SD) minimum JSW (mm)* | 1 | 3.3 (1.6) | 3.4 (1.4) | 0.278 |
| Depression | 22 | <0.001 | ||
| No | 889 (89.1) | 271 (78.8) | ||
| Yes | 109 (10.9) | 73 (21.2) |
SD, standard deviation; IQR, interquartile range; BMI, body mass index; KL, Kellgren Lawrence; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index; JSW, joint space width.
Baseline values (worst value across knees for each participant)
P-values from chi-squared test for binary and categorical variables, Wilcoxon rank-sum or Kruskal-Wallis rank tests for variables presented as median (IQR), and analysis of variance tests for variables presented as mean (SD).
Worsening of knee pain
Of the 2596 knees from 1319 participants analysed, 1,280 knees from 910 participants worsened (Table 2). See Supplementary Table 2 for the distribution of knees and participants who reported pain worsening at one time point and those who reported sustained pain worsening. The presence of symptoms in any foot/ankle at baseline was significantly associated with knee pain worsening (adjusted OR 1.54, 95% CI 1.25 to 1.91). Analyses of foot/ankle symptom laterality showed that ipsilateral (adjusted OR 1.50, 95% CI 1.07 to 2.10), contralateral (adjusted OR 1.44, 95% CI 1.02 to 2.06) and bilateral foot/ankle symptoms (adjusted OR 1.61, 95% CI 1.22 to 2.13) all significantly increased the odds for knee pain worsening in the follow up period.
Table 2.
Logistic regression analyses for the risk of the worsening of knee pain during the four-year follow up period. Logistic regression models fit using generalised estimating equations to account for the clustering of knees within participants.
| Laterality of foot/ankle symptoms | Total number of knees | No knee pain worsening N (%) | Knee pain worsening N (%) | Risk for knee pain worsening | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Unadjusted OR (95% CI) | P value | Adjusted† OR (95% CI) | P value | ||||
| No symptoms (ref) | 1933 | 1021 (77.6) | 912 (71.3) | 1 | 1 | ||
| Any side | 663 | 295 (22.4) | 368 (28.8) | 1.36 (1.12 to 1.65) | 0.002 | 1.54 (1.25 to 1.91) | <0.001 |
| Ipsilateral | 157 | 71 (5.4) | 86 (6.7) | 1.33 (0.96 to 1.84) | 0.089 | 1.50 (1.07 to 2.10) | 0.017 |
| Contralateral | 154 | 67 (5.1) | 87 (6.8) | 1.44 (1.03 to 1.99) | 0.030 | 1.44 (1.02 to 2.06) | 0.038 |
| Bilateral | 352 | 157 (11.9) | 195 (15.2) | 1.35 (1.05 to 1.73) | 0.019 | 1.61 (1.22 to 2.13) | <0.001 |
OR, odds ratios; CI, confidence intervals.
Adjusted for age, sex, BMI, WOMAC pain at baseline, race, depression, Charlson Comorbidity index (dichotomised), and worst baseline KL grade.
Worsening of symptomatic radiographic knee OA
Of the 2005 knees from 1033 people analysed, 305 knees from 262 participants had worsening of both knee pain and minJSW (Table 3). See Supplementary Table 2 for the distribution of knees and participants who had worsening of both knee pain and minJSW at one time point and those who had sustained pain and minJSW worsening. The presence of symptoms in any foot/ankle at baseline was not significantly associated with worsening of these outcomes. Likewise, analysis based on foot/ankle symptoms laterality also revealed no significant associations between foot/ankle symptoms and worsening of both knee pain and minJSW.
Table 3.
Logistic regression analyses for the risk of the worsening of knee pain and minJSW during the four-year follow up period. Models fit using generalized estimating equations to account for the clustering of knees within participants.
| Laterality of foot/ankle symptoms | Total number of knees | No knee pain or minJSW worsening N (%) | Knee pain and minJSW worsening N (%) | Risk for knee pain and minJSW worsening | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Unadjusted OR (95% CI) | P value | Adjusted† OR (95% CI) | P value | ||||
| No symptoms (ref) | 1513 | 1287 (75.7) | 226 (74.1) | 1 | 1 | ||
| Any side | 492 | 413 (24.3) | 79 (25.9) | 1.06 (0.79 to 1.42) | 0.69 | 1.09 (0.80 to 1.49) | 0.58 |
| Ipsilateral | 106 | 89 (5.2) | 17 (5.6) | 1.11 (0.65 to 1.88) | 0.70 | 1.07 (0.62 to 1.87) | 0.81 |
| Contralateral | 104 | 83 (4.9) | 21 (6.9) | 1.35 (0.82 to 2.23) | 0.23 | 1.43 (0.86 to 2.40) | 0.17 |
| Bilateral | 282 | 241 (14.2) | 41 (13.4) | 0.94 (0.63 to 1.40) | 0.77 | 0.97 (0.64 to 1.48) | 0.90 |
OA, osteoarthritis; minJSW, minimal medial tibiofemoral joint space width; OR, odds ratios; CI, confidence intervals.
Adjusted for age, sex, BMI, WOMAC pain at baseline, race, depression, Charlson Comorbidity index (dichotomised), worst baseline KL grade, baseline minJSW and baseline tibial rim distance.
Discussion
In this study, people with knee OA who also had foot/ankle symptoms were more likely to experience clinically relevant worsening of their knee pain at some time in the subsequent four years than people with knee OA but without foot/ankle symptoms. Risk for knee pain worsening increased regardless of foot/ankle symptom laterality. There were no longitudinal associations between symptoms in any foot/ankle and worsening of symptomatic radiographic knee OA.
The association between knee pain progression and foot/ankle symptoms regardless of laterality may be explained by a number of mechanisms. For example, foot pronation is associated with foot pain22, and people with existing knee OA have been shown to walk with greater foot pronation23, potentially to allow the foot to be plantigrade to compensate for knee varus. Thus, given that foot pronation causes greater internal tibial rotation24, 25, this may increase rotational stress on the tibiofemoral joint and peri-articular structures26, exacerbating existing knee pain in people with knee OA. Ipsilateral and contralateral foot pronation have also been shown to increase the knee adduction moment24, and a higher knee adduction moment is also associated with greater knee pain in people with established knee OA27. Alternatively, associations between multiple pain locations, such as the foot and knee, may be an epiphenomenon due to an unmeasured shared risk factor such as fibromyalgia, pain catastrophizing, a multi-joint pain phenotype or generalised form of OA28. The similar odds ratios for the association between foot/ankle symptoms on the ipsilateral and contralateral limbs, and worsening of knee pain, provide some support for this theory. Finally, certain styles of footwear, such as high heels, are associated with a greater likelihood of foot problems29 and abnormal knee biomechanics30 known to increase the risk of knee pain in older adults31.
Although foot/ankle symptoms were associated with worsening of knee pain, there was no longitudinal association with worsening of both knee pain and minJSW. This may because the participants who experienced this outcome were a smaller subset (n=79) of those who had knee pain worsening, and thus the model may not have had enough power to detect a relationship. Alternatively, it is possible that our measure of radiographic progression (minJSW) recorded using x-ray was not sensitive enough to detect structural deterioration32. The use of MRI measures may be more suitable to detect longitudinal joint changes not evident on x-ray. There is some support for this from a recent study that found having a greater number of painful sites (including at the foot) predicted knee cartilage loss on MRI in people aged between 50 and 80 years33.
Our findings add support to the scant previous literature investigating associations between foot/ankle and knee OA symptoms. Symptoms at these two sites have previously been shown to be the most prevalent multi-joint pain pattern, and to be associated with greater functional limitations, than the co-occurrence of pain at the knee and any other joint6. In a cross-sectional study using OAI data, we showed that knee OA patients with concurrent foot/ankle symptoms reported worse knee pain and other OA symptoms, in addition to worse general health and functional measures, than knee OA patients without foot/ankle symptoms7. Our recent longitudinal study reported that foot/ankle symptoms are a risk factor for developing knee OA symptoms and symptomatic radiographic knee OA over the subsequent four years in people at-risk of the disease34. Interestingly, this previous study found that bilateral and contralateral foot/ankle symptoms, but not ipsilateral foot/ankle symptoms, increased the risk of developing these outcomes. In contrast, we found associations between knee pain worsening and foot/ankle symptoms regardless of laterality in the current study. This might suggest that different mechanisms underpin the associations in incident versus worsening OA.
Some limitations may have influenced the findings of our study. Firstly, foot/ankle symptoms were self-reported and were only required to be present in the previous 30 days. Although this is consistent with the most widely used definitions of foot/ankle pain and/or symptoms15, a clinical foot assessment or more detailed foot pain questionnaire, such as the Manchester Foot Pain and Disability Index35 (which rates a number of different aspects of foot pain and functional limitations), may have yielded different results. Secondly, participants were included based on the presence of knee symptoms, but as there was no minimum WOMAC pain score requirement in our inclusion criteria, it is possible our analyses included people who did not report any measureable knee pain. Further, knee pain worsening was only required to be present at one of the follow up visits, so our analyses included both people whose knee pain worsened temporarily at a single time-point as well as those with sustained pain worsening. Thirdly, potential mechanistic data such as foot/ankle osteoarthritis, foot posture or dynamic foot function were not recorded in the OAI dataset and therefore we were unable to include these variables in our analyses. Finally, dichotomising data such as we did with BMI and Charlson comorbidity index can also leave residual confounding36. However when we repeated the analyses using fractional polynomials to model the continuous scores for these covariates, we found no strong evidence of this (see Table 3 in the supplementary analyses).
In summary, this study found that people with knee OA who report foot/ankle symptoms are at an increased risk of knee pain worsening compared to people without foot/ankle symptoms over the subsequent four years. However, foot/ankle symptoms were not associated with worsening of symptomatic radiographic knee OA. These findings are important given that knee pain worsening has been shown to be an independent predictor of future knee joint replacement surgery37. Furthermore, both general38 and specific39-42 causes of foot pain can be treated using simple conservative interventions, suggesting foot/ankle symptoms may be a modifiable risk factor for knee OA pain worsening. Future research should investigate whether treating foot/ankle symptoms in people with knee OA reduces worsening of knee pain in this population.
Supplementary Material
Acknowledgments
The authors would like to express their thanks to all participants, staff and funders from the Osteoarthritis Initiative for making the data publically available.
Role of the Funding Source: The OAI is a public-private partnership comprised of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation, GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. This manuscript was prepared using an OAI public use data set and does not necessarily reflect the opinions or views of the OAI investigators, the NIH, or the private funding partner. KB and HBM are partly funded by the National Health and Medical Research Council (NHMRC), DH is supported by an NHMRC Practitioner Fellowship and RH is supported by an Australian Research Council Future Fellowship. KP is supported by a NHMRC Program Grant (#1091302). HBM is currently a National Health and Medical Research Council Senior Research Fellow.
Footnotes
Author Contributions: All authors were involved in conception and design of the study, or in acquisition analysis and interpretation of data, and in revising it critically for important intellectual content. All authors approved the final version to be published. Dr. Paterson takes responsibility for the integrity of of the work as a whole, from inception to finished article.
Conception and design. Paterson, Kasza, Hinman, Hunter, Bennell.
Analysis and interpretation of data. Paterson, Kasza, Hunter, Hinman, Menz, Peat, Bennell.
Drafting of the article. Paterson, Bennell.
Critical revision of the article for important intellectual content. Paterson, Kasza, Hunter, Hinman, Menz, Peat, Bennell.
Final approval of the article. Paterson, Kasza, Hunter, Hinman, Menz, Peat, Bennell.
Conflict of Interest: No authors report competing interests.
RSH and KLB, and the University of Melbourne, received royalties from sales of Gel Melbourne OA shoes from 2012-2014. The manufacturer of the shoes played no role in the study design nor had any input into the analysis and interpretation of data from this study.
DH provides consulting services for MerckSerono, Flexion and Tissuegene.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bedson J, Croft PR. The discordance between clinical and radiographic knee osteoarthritis: A systematic search and summary of the literature. BMC Musculoskeletal Disorders. 2008;9:1–11. doi: 10.1186/1471-2474-9-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Conaghan PG, D'Agostino MA, Le Bars M, Baron G, Schmidely N, Wakefield R, et al. Clinical and ultrasonographic predictors of joint replacement for knee osteoarthritis: results from a large, 3-year, prospective EULAR study. Annals of the Rheumatic Diseases. 2010;69:644–647. doi: 10.1136/ard.2008.099564. [DOI] [PubMed] [Google Scholar]
- 3.Bastick AN, Belo JN, Runhaar J, Bierma-Zeinstra SMA. What are the prognostic factors for radiographic progression of knee osteoarthritis? A meta-analysis. Clinical Orthopaedics and Related Research. 2015;473:2969–2989. doi: 10.1007/s11999-015-4349-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bastick AN, Runhaar J, Belo JN, Bierma-Zeinstra SMA. Prognostic factors for progression of clinical osteoarthritis of the knee: a systematic review of observational studies. Arthritis Research & Therapy. 2015;17:1–13. doi: 10.1186/s13075-015-0670-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Elfhag K, Rössner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obesity Reviews. 2005;6:67–85. doi: 10.1111/j.1467-789X.2005.00170.x. [DOI] [PubMed] [Google Scholar]
- 6.Keenan AM, Tennant A, Fear J, Emery P, Conaghan PG. Impact of multiple joint problems on daily living tasks in people in the community over age fifty-five. Arthritis Care & Research. 2006;55:757–764. doi: 10.1002/art.22239. [DOI] [PubMed] [Google Scholar]
- 7.Paterson KL, Hinman RS, Hunter DJ, Wrigley TV, Bennell KL. Impact of concurrent foot pain on health and functional status in people with knee osteoarthritis: data from the osteoarthritis initiative. Arthritis Care Res (Hoboken) 2015;67:989–995. doi: 10.1002/acr.22537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paterson KL, Kasza J, Hunter DJ, Hinman RS, Menz HB, Peat G, et al. The relationship between foot and ankle symptoms and risk of developing knee osteoarthritis: data from the osteoarthritis initiative. Osteoarthritis Cartilage. 2016 doi: 10.1016/j.joca.2016.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Niu J, Zhang YQ, Torner J, Nevitt M, Lewis CE, Aliabadi P, et al. Is obesity a risk factor for progressive radiographic knee osteoarthritis? Arthritis Care & Research. 2009;61:329–335. doi: 10.1002/art.24337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Felson D, Niu J, Sack B, Aliabadi P, McCullough C, Nevitt MC. Progression of osteoarthritis as a state of inertia. Annals of the Rheumatic Diseases. 2013;72:924–929. doi: 10.1136/annrheumdis-2012-201575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Osteoarthritis Initiative. 2013 [Google Scholar]
- 12.Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. Development of criteria for the classification and reporting of osteoarthritis: Classification of osteoarthritis of the knee. Arthritis & Rheumatism. 1986;29:1039–1049. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- 13.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 14.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Medical care. 1996;34:73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Thomas MJ, Roddy E, Zhang W, Menz HB, Hannan MT, Peat GM. The population prevalence of foot and ankle pain in middle and old age: A systematic review. Pain. 2011;152:2870–2880. doi: 10.1016/j.pain.2011.09.019. [DOI] [PubMed] [Google Scholar]
- 16.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. The Journal of rheumatology. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 17.Angst F, Aeschlimann A, Michel BA, Stucki G. Minimal clinically important rehabilitation effects in patients with osteoarthritis of the lower extremities. The Journal of rheumatology. 2002;29:131–138. [PubMed] [Google Scholar]
- 18.Angst F, Aeschlimann A, Stucki G. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Care & Research. 2001;45:384–391. doi: 10.1002/1529-0131(200108)45:4<384::AID-ART352>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 19.Eckstein F, Collins JE, Nevitt MC, Lynch JA, Kraus VB, Katz JN, et al. Brief report: cartilage thickness change as an imaging biomarker of knee osteoarthritis progression: data from the Foundation for the National Institutes of Health Osteoarthritis Biomarkers Consortium. Arthritis & Rheumatology. 2015;67:3184–3189. doi: 10.1002/art.39324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Duryea J, Li J, Peterfy CG, Gordon C, Genant HK. Trainable rule-based algorithm for the measurement of joint space width in digital radiographic images of the knee. Medical Physics. 2000;27:580–591. doi: 10.1118/1.598897. [DOI] [PubMed] [Google Scholar]
- 21.Ornetti P, Brandt K, Hellio-Le Graverand MP, Hochberg M, Hunter DJ, Kloppenburg M, et al. OARSI–OMERACT definition of relevant radiological progression in hip/knee osteoarthritis. Osteoarthritis and Cartilage. 2009;17:856–863. doi: 10.1016/j.joca.2009.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Menz HB, Dufour AB, Riskowski JL, Hillstrom HJ, Hannan MT. Association of planus foot posture and pronated foot function with foot pain: the Framingham Foot Study. Arthritis Care & Research. 2013;65:1991–1999. doi: 10.1002/acr.22079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Levinger P, Menz HB, Morrow AD, Feller JA, Bartlett JR, Bergman NR. Foot kinematics in people with medial compartment knee osteoarthritis. Rheumatology. 2012;51:2191–2198. doi: 10.1093/rheumatology/kes222. [DOI] [PubMed] [Google Scholar]
- 24.Resende RA, Deluzio KJ, Kirkwood RN, Hassan EA, Fonseca ST. Increased unilateral foot pronation affects lower limbs and pelvic biomechanics during walking. Gait & Posture. 2015;41:395–401. doi: 10.1016/j.gaitpost.2014.10.025. [DOI] [PubMed] [Google Scholar]
- 25.Souza TR, Pinto RZ, Trede RG, Kirkwood RN, Fonseca ST. Temporal couplings between rearfoot–shank complex and hip joint during walking. Clinical Biomechanics. 2010;25:745–748. doi: 10.1016/j.clinbiomech.2010.04.012. [DOI] [PubMed] [Google Scholar]
- 26.Andriacchi TP, Briant PL, Bevill SL, Koo S. Rotational changes at the knee after ACL injury cause cartilage thinning. Clinical orthopaedics and related research. 2006;442:39–44. doi: 10.1097/01.blo.0000197079.26600.09. [DOI] [PubMed] [Google Scholar]
- 27.Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Annals of the Rheumatic Diseases. 2002;61:617–622. doi: 10.1136/ard.61.7.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nelson AE, Smith MW, Golightly YM, Jordan JM. “Generalized osteoarthritis”: A systematic review. Seminars in Arthritis and Rheumatism. 2014;43:713–720. doi: 10.1016/j.semarthrit.2013.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Menz HB, Morris ME. Footwear characteristics and foot problems in older people. Gerontology. 2005;51:346–351. doi: 10.1159/000086373. [DOI] [PubMed] [Google Scholar]
- 30.Radzimski AO, Mündermann A, Sole G. Effect of footwear on the external knee adduction moment — A systematic review. The Knee. 2012;19:163–175. doi: 10.1016/j.knee.2011.05.013. [DOI] [PubMed] [Google Scholar]
- 31.Amin S, Luepongsak N, McGibbon CA, LaValley MP, Krebs DE, Felson DT. Knee adduction moment and development of chronic knee pain in elders. Arthritis Care & Research. 2004;51:371–376. doi: 10.1002/art.20396. [DOI] [PubMed] [Google Scholar]
- 32.Wick MC, Kastlunger M, Weiss RJ. Clinical imaging assessments of knee osteoarthritis in the elderly: a mini-review. Gerontology. 2014;60:386–394. doi: 10.1159/000357756. [DOI] [PubMed] [Google Scholar]
- 33.Pan F, Laslett L, Tian J, Cicuttini F, Winzenberg T, Ding C, et al. Pain at sites outside the knee predicts knee cartilage volume loss in elderly people without knee osteoarthritis: A prospective study. Arthritis Care & Research. doi: 10.1002/acr.22964. In press. [DOI] [PubMed] [Google Scholar]
- 34.Paterson KL, Kasza J, Hunter DJ, Hinman RS, Menz HB, Peat G, et al. The relationship between foot and ankle symptoms and risk of developing knee osteoarthritis: data from the osteoarthritis initiative. Osteoarthritis and Cartilage. 2016 doi: 10.1016/j.joca.2016.12.003. Accepted December 1st. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Garrow AP, Silman AJ, Macfarlane GJ. The Cheshire Foot Pain and Disability Survey: a population survey assessing prevalence and associations. Pain. 2004;110:378–384. doi: 10.1016/j.pain.2004.04.019. [DOI] [PubMed] [Google Scholar]
- 36.Brenner H, Blettner M. Controlling for continuous confounders in epidemiologic research. Epidemiology. 1997;8:429–434. [PubMed] [Google Scholar]
- 37.Raynauld JP, Martel-Pelletier J, Dorais M, Haraoui B, Choquette D, Abram F, et al. Total knee replacement as a knee osteoarthritis outcome: predictors derived from a 4-year long-term observation following a randomized clinical trial using chondroitin sulfate. Cartilage. 2013;4:219–226. doi: 10.1177/1947603513483547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Menz HB, Auhl M, Ristevski S, Frescos N, Munteanu SE. Effectiveness of off-the-shelf, extra-depth footwear in reducing foot pain in older people: a randomized controlled trial. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2015;70:511–517. doi: 10.1093/gerona/glu169. [DOI] [PubMed] [Google Scholar]
- 39.Woodburn J, Barker S, Helliwell PS. A randomized controlled trial of foot orthoses in rheumatoid arthritis. The Journal of Rheumatology. 2002;29:1377–1383. [PubMed] [Google Scholar]
- 40.Lee SY, McKeon P, Hertel J. Does the use of orthoses improve self-reported pain and function measures in patients with plantar fasciitis? A meta-analysis. Physical Therapy in Sport. 2009;10:12–18. doi: 10.1016/j.ptsp.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 41.Rome K, Stewart S, Vandal A, Gow P, McNair P, Dalbeth N. The effects of commercially available footwear on foot pain and disability in people with gout: a pilot study. BMC Musculoskeletal Disorders. 2013;14:278. doi: 10.1186/1471-2474-14-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Burns J, Crosbie J, Ouvrier R, Hunt A. Effective orthotic therapy for the painful cavus foot: a randomized controlled trial. Journal of the American Podiatric Medical Association. 2006;96:205–211. doi: 10.7547/0960205. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.