Abstract
In this study, we conducted a path analysis on data from the National Latino and Asian American Study (NLAAS) to investigate the role of religious attendance on mental health among Mexican populations. Using data from 868 Latinos of Mexican origin, we further investigated the extent to which religious attendance mediated the direct path between generation status and lifetime prevalence rates of any substance use disorder, depressive disorder, and anxiety disorder. Results indicate that Mexican immigrants endorsed lower lifetime prevalence rates of depressive disorder, anxiety disorder, and substance use disorder, and endorsed higher levels of religious attendance. Second, results indicate a significant negative relationship between religious attendance and prevalence rates for depressive disorder, anxiety disorder, and substance use disorder. Third, results indicate that religious attendance was a mediator for the relationship between generation status and the lifetime prevalence rates of substance use disorder only. These results provide a contribution toward the discussion of the Immigrant Health Paradox and further highlights the role that religious attendance plays in the relationship between generational status and the lifetime prevalence rates of substance use disorder.
Keywords: Immigrant Health Paradox, Religious Attendance, Substance Use Disorder, Anxiety, Depression
Over one-half of the Latino population consists of immigrants, a term used to describe foreign-born individuals who have immigrated to the United States (U.S. Census Bureau, 2010). These Latino immigrants typically have a number of risk factors that they bring with them from their host countries (e.g., low educational backgrounds, limited English fluency, and limited English reading abilities; Fry, 2010; Larsen, 2004 Pew Research Center, 2007). In addition, they also experience a number of stressors during the immigration process and upon arrival to the mainland United States. Some of these stressors include lower paying jobs and relatively frequent experiences of violence and discrimination (Larsen, 2004; Solis, 2003).
In general, factors associated with poverty like low paying work and lower education have been consistently associated with worse health outcomes and higher mortality rates (e.g., Vick, Jones, & Mitra, 2012). However, when compared to U.S. born Latinos and non-Latino Whites, Latino immigrants experience lower mortality rates (Singh & Miller 2004; Vega & Sribney, 2011), have better overall physical health (Seicean, Neuhauser, Strohl, & Redline, 2011; Zhang, Hayward, & Lu, 2012) as well as behavioral and mental health (e.g., lower prevalence rates of substance use disorders better mental health; Alegría et al., 2008; Alderete et al., 2000; Bacio, Mays, & Lau, 2013; Guarini et al, 2011). This counterintuitive finding of better outcomes among Latino immigrants has been termed the Immigrant Health Paradox (Alegría et al., 2008; Vega et al., 2011).
The recent increase in attention to the paradox has also produced more nuanced research suggesting that it may not extend equally to all Latinos. Alegría and colleagues (2008), using data from both the National Latino and Asian American Studies and the National Comorbidity Study – Replication, found particularly strong evidence for the paradox among Latinos of Mexican origin: Mexican immigrants reported lower lifetime prevalence rates for mood, anxiety, and substance use disorders than U.S.-born Mexican Americans. In contrast, the authors found only some support for the paradox among Latinos of Cuban origin and very little evidence for the paradox among Latinos of Puerto Rican descent. These findings are consistent with other research that has not found support for the paradox among Puerto Ricans (e.g., Rivera & Burgos, 2010).
Despite the growing evidence for the paradox, particularly among Mexican Latinos, researchers have struggled to explain this phenomenon. A few sociological theories have been proffered to explain this paradox, such as the Healthy Migrant Hypothesis, which suggests that the difficulties associated with migration may select for healthier migrants (Franzini, Ribble, & Keddie, 2001; Palloni & Morenoff, 2001), or the Salmon Bias Hypothesis, which speculates that Mexican immigrants are more likely to return to their country of origin to receive medical care (Franzini et al., 2001). Another promising hypothesis has been termed the Barrio Effect, which theorizes that many immigrant Latinos live in Latino enclaves that provide supportive social networks, family, and shared norms (Eschbach, Ostir, Patel, Markides, Goodwin, 2004).
However, the research investigating these ideas has not yielded consistent findings. Moreover, very little is known regarding specific sociocultural explanations or mechanisms for the Barrio Effect. One related sociocultural factor that might play an important role in the paradox and could operate as a possible explanatory mechanism is religious attendance.
Religious Attendance: A Possible Explanatory Mechanism
In general, religiosity refers to individuals’ following of religious practices (e.g., attending a church) through an organized system such as a church (Cervantes & Parham, 2005; Hill & Pargament, 2008). The organized nature of religiosity contrasts it with spirituality, which generally refers to a personal relationship with a transcendent being (e.g., God, Jesus, saints, or spirits; Cervantes & Parham, 2005). Religiosity and spirituality however may have overlapping practices, as many religious individuals also self-identify as spiritual. However, for this study, we are interested in investigating the organized nature of religiosity. Specifically, we seek to understand attending to religious services as a predictor variable acknowledging the potential overlap with spirituality.
To our knowledge, no empirical research has examined how religious attendance may be associated with this paradox, despite the fact that over 90% of Mexicans in the United States report that they are religiously committed (Census, 2010). Recent data also suggest that religious attendance changes by generational status, with Latinos tending to become less likely to endorse religious attitudes and behaviors as they acculturate to the U.S. (Pew Research Center, 2015). For example, Espinosa and colleagues (2003) found that 74% of Mexican immigrants identified as belonging to a particular religion and 52% attended a religious organization while 62% of U.S.-born Latinos identified to belonging to a church and 31% attended a religious organization. Similarly, more than two thirds of Mexican immigrants reported that religion is very important in their lives (69%) in comparison to half (49%) of U.S.-born Mexican Americans.
Moreover, given that Mexican immigrants tend to report higher levels of religious attendance than U.S.-born Mexican American, there is reason to believe that religious attendance might impact health outcomes and provide a possible explanation for the Immigrant Health Paradox. In general, research has documented associations between religious attendance and positive health outcomes, including fewer instances of certain physiological processes such as cardiovascular, neuroendocrine, and immune function disease, lower mortality rates, and better overall mental health (Diaz et al., 2011; Hill et al, 2005; Seeman et al., 2003). With regard to mental health, research has consistently found that higher levels of religious attendance are generally associated with lower rates of depression, substance use disorders, and alcohol abuse (e.g., Ai et al., 2013; Diaz et al., 2011).
This study investigates associations among: generational status and the lifetime prevalence rates of any substance use disorder, depression, and anxiety. We also examined the extent to which religious attendance mediated these associations.
Method
NLAAS Overview
This study1 used data from the NLAAS (Alegría et al., 2004), a nationally representative study whose purpose was to provide a more representative sample of Latinos and Asian Americans than the original National Comorbidity Survey – Replication (Kessler & Merikangas, 2004). The NLAAS is one of the most comprehensive studies of Latinos and Asian Americans ever conducted using up-to-date scientific strategies in the design, sampling procedures, mental health assessments, and analytic techniques. The Internal Review Board Committees of Cambridge Health Alliance, the University of Washington, and the University of Michigan approved this research study.
Participants
Latino participants in this study were 18 years of age or older, living in the noninstitutionalized population of the United States or Hawaii, and were from 1) Puerto Rican, 2) Cuban, 3) Mexican, and 4) other Latino origins. The final NLAAS Latino sample included 2,554 respondents with an overall response rate of 75.5%. Although the NLAAS collected data on 2,554 Latinos respondents, the sample of interest is the 868 Mexican immigrants and Mexican American participants. Respondents were English and Spanish-speaking adults (age 18 or older). The participants’ average age was 36.5 (13.63) and ranged from 18–88. In terms of generation status, 487 (56.1%) participants were Mexican immigrants, while 380 (43.8%) participants were U.S.-born Mexican Americans. In terms of gender, 368 (42.5%) were males and 470 (56.5%) were females. Less than half of participants (45.5%) reported that their English language proficiency was “good/excellent.” In terms of education, 52.71% had less than a high school diploma. 69.7% were married or cohabitating.
Measures
Demographic Variables
Self-reported demographic variables were also used as potential variables to confound the analyses. The information collected on the following demographic variables included age, generation status, gender, education, and SES.
Generation Status
To determine if participants were Mexican immigrants or U.S.-born Mexican American, participants were asked their ethnicity (e.g., Latino/Hispanic) and country of birth (e.g., Mexico or United States). Those participants who indicated that their ethnic background was “Mexican” and reported being born in Mexico were considered Mexican immigrants (coded as 1). Those participants who indicated that their ethnic background was Mexican but reported being born in the United States were considered U.S.-born Mexican Americans (coded as 0).
Religious Attendance
Religious attendance was assessed with a two-item scale. However, only one was used for these analyses. Since the second item was a double-barreled question (i.e., this item has more than one meanings, yet allows only for one answer), the item was dropped. For example, this question asked: “When you have problems or difficulties in your family, work, or personal life, how often do you seek comfort through religious or spiritual means, such as praying, meditating, attending a religious or spiritual service, or talking to a religious or spiritual advisor?” Therefore, participants were only asked their levels of religious attendance (How often do you usually attend religious services?). Participants responded using a Likert scale of 1–5, where 1 indicated “more than once a week” and 5 indicated “never.”
Mental Disorders
Using the World Health Organization’s World Mental Health Version of the Composite International Diagnostic Interview (WHO WMH-CIDI), dichotomized variables were used to determine whether a lifetime prevalence rate existed for these mental disorders. Mental disorders were classified into three composite categories including any depressive disorder (dysthymia or major depressive episode); any anxiety disorder (agoraphobia, social phobia, generalized anxiety disorder, posttraumatic stress disorder, or panic disorder); or any substance use disorder (drug abuse, drug dependence, alcohol abuse, or alcohol dependence). The WHO WMH-CIDI showed consistent reliability with the Structured Clinical Interview for DSM-IV (SCID) diagnoses for depressive disorders (kappa=0.46) as well as substance disorders (kappa=0.49) but not for anxiety disorders. However, this finding is consistent with the general population (First et al, 2002).
Analytic Plan
Path models were tested using Mplus Version 7.3 (Muthen & Muthen, 1998–2012). A weighted least squares means and variance adjusted procedure was employed in estimating the parameters. In all models, the indirect effects model was tested first. If the indirect effects model was an unacceptable fit, we then tested the direct effects model, examining whether the addition of all direct paths from predictors to outcome variables provided a better fit to the data, when added simultaneously (Hu, L. T., & Bentler, P. M., 1999). If the indirect effects model was an acceptable fit to the data, we added direct paths, all at once, and tested whether the addition of each individual path increased the fit of the model (Hu, L. T., & Bentler, P. M., 1999). In all models, SES, gender, age were included as covariates, by allowing paths to all variables.
Results
Preliminary Analyses
Table 1 presents correlations among the variables of interest. Results indicate that gender was correlated with lifetime prevalence of anxiety (r = −19, p < .05), depression (r = .25, p < .05), substance use (r = -.47, p < .05). SES had a significant correlation with generation status (r = −.47, p < .05). It was important to include SES in the analysis in order to evaluate generation status on the outcomes of interest above and beyond SES. Age had small negative correlations with generation status (r = −.06, p = n.s.), and a small and positive correlation with anxiety (r = .12, p < .05). Thus, gender, SES, and age were included as covariates in all path models.
Table 1.
Correlations among variables
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| Religious Attendance | --- | |||||||
| Gen. Status | −.78* | --- | ||||||
| Gender | .05 | −.05 | --- | |||||
| Age | −.11* | −.06 | .06 | --- | ||||
| SES | .56* | −.47* | .03 | −.11 | --- | |||
| Depression | .16* | −.20* | .25* | .00 | .08 | --- | ||
| Anxiety | .17* | −.16 | .19* | .12* | −.02 | .53* | --- | |
| Substance Use | .30* | −.37 | −.47* | .05 | .04 | .31* | .28* | --- |
p < .05
Note: for the gender constructs, males were coded as 1 and females were coded as 2. For generational status, immigrants were coded as 1 and US born we coded as 0
Overall Model Fit
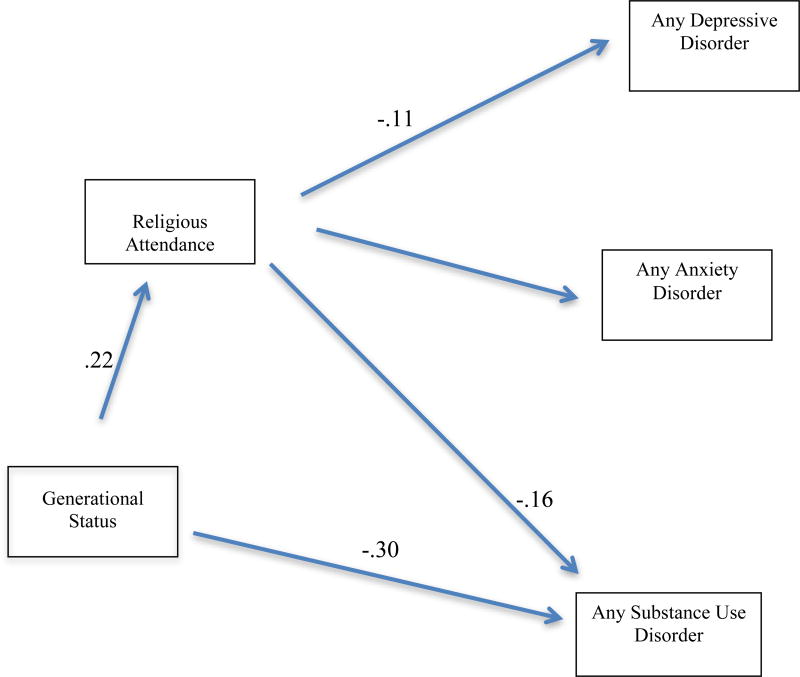
The overall results suggested the indirect effects only model was an unacceptable fit, with a statistically significant, χ2 (3, N = 868) = 48.46, p < .001 and CFI 0.87 (see figure 1). The RMSEA was .13 with a 90% confidence interval of .11 and .15, indicating a poor fit. We then tested the direct effects model, adding direct paths from generational status to depressive disorder, anxiety disorder, and substance use disorder. The addition of these direct effects resulted in a significant improvement in fit. The chi square difference indicated that the model where direct paths were freely estimated had a better fit, Δχ2 (3, N = 868) = 48.942, p < .001. Therefore, the coefficients from those models were reported and interpreted.
Figure 1.
Mediation model of the relations between generational status, religious attendance, and any depressive disorder, any anxiety disorder, and any substance use disorder. Only significant paths (p < .05) are depicted. Model fit, χ2 (3, N= 868) = 48.46, p < .001, CFI = 0.87, RMSEA =.13.
Is there a generational difference in lifetime prevalence rates for depressive disorder, anxiety disorder, or substance use disorder (c paths)?
Results suggest that Mexican immigrants had significantly lower rates of the lifetime prevalence rates of depressive disorder (β = −0.30, p < 0.01), anxiety disorder (β = −0.35, p < 0.01), and substance use disorder (β = −0.97, p < 0.001), as compared to U.S.-born Mexican Americans (controlling for age, gender, and SES).
Is there a generational difference in levels of religious attendance (a path)?
Table 2 presents findings for generational status and the levels of religious attendance. Results indicate that Mexican immigrants had statistically significantly higher levels of religious attendance (M = 2.94, SD= 1.27) when compared to U.S.-born Mexican Americans (M = 2.76, SD= 1.29; β = 0.22, p = 0.02). These results support our second hypothesis that Mexican immigrants have higher levels of religious attendance than U.S.-born Mexican Americans (see Table 2, a path).
Table 2.
Mediation Model of Generational Status on Depression, Anxiety, and Substance use Disorders (N = 867)
| Depression | |
| Direct Effect | B (SE) |
| a path | *0.22 (0.09) |
| b path | * −0.11 (0.04) |
| c’ path | −0.002 (0.01) |
| Total Indirect Effects | |
| ab path | −.05 (.02) |
| Anxiety Disorder | |
| Direct Effects | B (SE) |
| a path | *0.22 (0.09) |
| b path | *−0.09 (0.05) |
| c’ path | −0.002 (0.01) |
| Total Indirect Effects | |
| ab path | −0.04 (0.02) |
| Substance Use Disorder | |
| Direct Effect | B (SE) |
| a path | *0.22 (0.09) |
| b path | ** −0.16 (0.04) |
| c’ path | * −0.006 (0.02) |
| Total Indirect Effects | |
| ab path | −0.09 (0.03) |
Note: Confidence Intervals are biased-estimated intervals; Controlling for gender, age, and SES
p < .05,
p < .01,
p < .001
Is there a relationship between religious attendance and the lifetime prevalence rates of depressive disorder, anxiety disorder, and substance use disorder (b path)?
Table 2 presents findings for religious attendance and the lifetime prevalence rates of depressive disorder, anxiety disorder, and substance use disorder. Results also indicate that religious attendance had a statistically significant negative relation with lifetime prevalence rates of depressive disorder (β = −0.11, p = 0.01), anxiety disorder (β = −0.09, p = 0.04), and substance use disorder (β = −0.16, p < 0.001). These results support our third hypothesis that levels of religious attendance will be negatively associated with the lifetime prevalence rates of these mental disorders (i.e., depressive disorders, anxiety disorder, and substance use disorders).
Does religious attendance mediate the relationships between generational status and the lifetime prevalence of depressive disorder, anxiety disorder, and substance use disorder?
Results then suggested that religious attendance did not mediate the effect of generational status on the lifetime prevalence rates of depressive disorder (β = −0.02 p= 0.08) nor anxiety disorder (β = −0.02, p = 0.12), However, results indicate religious attendance was a statistically significant mediator between generational status and the prevalence rates of substance use disorder (β = −0.03, p = 0.046). These findings partially support the hypothesis that states that religious attendance mediates the relationship between generational status and the lifetime prevalence rates of substance use disorder but not for depression or anxiety.
Discussion
The purpose of this study was to investifate the role of religious attendance on mental health among Mexican populations and investigate if this examination contributes towarsd the discussion of the Immigrant Health Paradox. Our analyses yielded three primary findings. First, in addition to replicating the finding that Mexican immigrants had lower lifetime prevalence rates of depressive disorders, anxiety disorders, and substance use disorders as compared to U.S.-born Mexican Americans, we also found that Mexican immigrants reported higher levels of religious attendance as compared to U.S.-born Mexican Americans. Second, results showed that religious attendance was negatively associated with lifetime prevalence rates of depressive disorders, anxiety disorders, and substance use disorders. Third, religious attendance was a significant mediator of the relationship between generational status and the lifetime prevalence rate of substance use disorders, but not for depressive disorders or anxiety disorders.
Overall, these findings are consistent with the large body of literature that has found higher levels of religious attendance among Latino immigrants (e.g., Espinosa et al, 2003), as well as the protective effect that religious attendance has on mental disorders and substance use disorders (e.g., Ai, Huang, Bjorck, & Appel, 2013; Diaz et al., 2011). However, this study contributes to the literature by highlighting how religious attendance was a significant mediator between generational status and substance use disorder, but not between generational status and depressive or anxiety disorders. This may be the result of religious norms and morals that discourage the use of substances (Hodge, Marsiglia, & Nieri (2011); Krause et al., 2011; Marsiglia, et al., 2005). For example, participants who endorsed higher levels of religious attendance (such Latino immigrants) may have a strong social network that proscribes the use of alcohol and substance use. They may receive these messages through religious channels, including organized church messages and informal support. Krause and colleagues (2011) have also suggested that individuals who are known to deviate from religious norms concerning these issues may receive encouragement to change these types of behaviors. Therefore, these norms and moral codes may promote positive health-related behaviors and lifestyles (e.g., substance free lifestyles) that lowers risk for substance use disorders (Hill & McCullough, 2008; Johnson, 2013). The clear association between religious doctrine and substance use may not be as evident for emotional experiences like depression and anxiety. Since the literature indicates that U.S. Born Mexican Americans endorse less religious involvement when compared to Mexican immigrants (e.g., Pew Research Center 2015), this protective social network may therefore not be as present within the U.S. Born Mexican Americans. Future research would do well to explore what aspects of religious attendance are most salient in this process.
Limitations and Strengths
There are several limitations that are worth noting. First, the NLAAS study measured religious attendance using only one item. Therefore, these results should be interpreted with caution. Future research can also investigate this relationship with a more elaborate examination of religiosity (outside of just attendance). It is also possible that what would be identified as a mental illness (e.g., depression, anxiety) within a secular and therapeutic worldview may have been identified as something else among those participants who endorsed a religious worldview. Future research can investigate the cultural means of assessing anxiety and depression (or related cultural syndromes) in this sample. Moreover, our focus on Latinos of Mexican descent limit our ability to explain the Immigrant Health Paradox among other immigrant groups.
Nevertheless, this study has numerous strengths, including its use of a statistically representative sample, its rigorous assessment of mental disorders, and the relatively large sample size. Given the field’s difficulty in adequately explaining the Immigrant Health Paradox, our findings that religious attendance might play a meaningful role advances our understanding of identifying person-level mechanisms. Understanding the changes in religious attendance across generation correlate with increased risk for substance use disorder raises important questions for future research to explore. In addition, this knowledge could play an important role in adapting mental health interventions for Latinos of Mexican origin. Specifically, these interventions could be tailored in recognition of these generational differences. Given the extensive literature demonstrating that Latinos underutilize mental health services (e.g., Alegría et al., 2002), interventions that are more sensitive to salient cultural issues and client values could help the mental health care disparities that affect this population.
Footnotes
This study was part of a larger study from a doctoral dissertation.
References
- Abraído-Lanza AF, Vásquez E, Echeverría SE. En las manos de Dios [in God's hands]: Religious and other forms of coping Among Latinos with arthritis. Journal of Consulting and Clinical Psychology. 2004;72(1):91–102. doi: 10.1037/0022-006X.72.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ai AL, Huang B, Bjorck J, Appel HB. Religious attendance and major depression among Asian Americans from a national database: The mediation of social support. Psychology of Religion And Spirituality. 2013;5(2):78–89. [Google Scholar]
- Alderete E, Vega W, Kolody B, Aguilar-Gaxiola S. Lifetime prevalence of and risk factors for psychiatric disorders among Mexican migrant farmworkers in California. American Journal of Public Health. 2000;90:608–614. doi: 10.2105/ajph.90.4.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Canino G, Ríos R, Vera M, Calderón J, Rusch D, Ortega AN. Mental health care for Latinos: Inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino Whites. Psychiatric Services. 2002;53:1547–1555. doi: 10.1176/appi.ps.53.12.1547. [DOI] [PubMed] [Google Scholar]
- Alegría M, Takeuchi D, Canino G, Duan N, Shrout P, Meng XL, Vega W, Zane N, Vila D, Woo M, Vera M, Guarnaccia P, Aguilar-Gaxiola S, Sue S, Escobar J, Lin KM, Gong F. Considering context, place and culture: the National Latino and Asian American Study. International Journal of Methods in Psychiatric Research. 2004;13(4):208–2020. doi: 10.1002/mpr.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Canino G, Shrout P, Woo M, Duan N, Vila D, Torres M, Chen C, Meng, Ciao-Li Prevalence of mental illness in immigrant and non-immigrant U.S. Latino groups. American Journal of Psychiatry. 2008;165:359–369. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bacio GA, Mays VM, Lau AS. Drinking initiation and problematic drinking among Latino adolescents: Explanations of the Immigrant Paradox. Psychology of Addictive Behaviors. 2013;27(1):14–22. doi: 10.1037/a0029996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- Collett JL, Lizardo O. A power-control theory of gender and religiosity. Journal for the Scientific Study of Religion. 2009;48(2):213–231. [Google Scholar]
- Comaz-Diaz L. Latino healing: The integration of ethnic psychology into psychotherapy. Psychotherapy: Theory, Research, Practice, Training. 2006;43:436–453. doi: 10.1037/0033-3204.43.4.436. [DOI] [PubMed] [Google Scholar]
- Diaz N, Horton E, McIlveen J, Weiner M, Williams LB. Spirituality, religiosity and depressive symptoms among individuals in substance-abuse treatment. Journal of Religion & Spirituality in Social Work: Social Thought. 2011;30:71–87. [Google Scholar]
- Eschbach K, Ostir GV, Patel KV, Markides KS, Goodwin JS. Neighborhood context and mortality among older Mexican Americans: is there a barrio advantage? American Journal of Public Health. 2004;94:1807–1812. doi: 10.2105/ajph.94.10.1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espinosa G, Elizondo V, Miranda J. Hispanic churches in American public life: Summary of findings. Interim Reports. 2003;2:1–29. [Google Scholar]
- Falicov C. Religion and spiritual traditions in immigrant families: Significance for Latino health and mental health. In: Walsh F, editor. Spiritual resources in family therapy. 2. New York, NY US: Guilford Press; 2009. pp. 156–173. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCIDP) New York: New York State Psychiatric Institute, Biometric Research; 2002. [Google Scholar]
- Franzini L, Ribble JC, Keddie AM. Understanding the Hispanic paradox. Journal of Ethnicity and Disease. 2001;11:496–518. [PubMed] [Google Scholar]
- Fry R. Hispanics, high school dropouts and the GED. Pew Research Hispanic Center. 2010 Retrieved from: http://www.pewhispanic.org/2010/05/13/hispanics-high-school-dropouts-and-the-ged/
- Goodwin RD, Gotlib IH. Gender differences in depression: the role of personality factors. Psychiatry Research. 2004;126(2):135–142. doi: 10.1016/j.psychres.2003.12.024. [DOI] [PubMed] [Google Scholar]
- Guarini T, Marks A, Patton F, Coll C. The Immigrant Paradox in sexual risk behavior among Latino adolescents: Impact of immigrant generation and gender. Applied Developmental Science. 2011;15(4):201–209. [Google Scholar]
- Herrera AP, Lee JW, Nanyonjo RD, Laufman LE, Torres-Vigil I. Religious coping and caregiver well-being in Mexican-American families. Aging & Mental Health. 2009;13:84–91. doi: 10.1080/13607860802154507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill TD, Angel JL, Ellison CG, Angel RJ. Religious attendance and mortality: An 8-year follow up of older Mexican Americans. The Journals of Gerontology: Series B: Psychological Sciences and Social Sciences. 2005;60B(2):S102–SI09. doi: 10.1093/geronb/60.2.s102. [DOI] [PubMed] [Google Scholar]
- Hill TD, McCullough ME. Religious involvement and the intoxication trajectories of low income urban women. Journal of Drug Issues. 2008;43:847–862. [Google Scholar]
- Hodge DR, Marsiglia FF, Nieri T. Religion and Substance Use among Youths of Mexican Heritage: A Social Capital Perspective. Social Work Research, 1. 2011;35(3):137–146. doi: 10.1093/swr/35.3.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling: a multidisciplinary journal. 1999;6(1):1–55. [Google Scholar]
- Johnson TJ. Addiction and the search for the sacred: Religion, spirituality, and the origins and treatment of substance use disorders. In: Pargament KI, Mahoney A, Shafranske EP, Pargament KI, Mahoney A, Shafranske EP, editors. APA handbook of psychology, religion, and spirituality (Vol 2): An applied psychology of religion and spirituality. Washington, DC, US: American Psychological Association; 2013. pp. 297–317. [Google Scholar]
- Jurkowski JM, Kurlanska C, Ramos BM. Latino women's spiritual beliefs related to health. American Journal of Health Promotion. 2010;25:19–25. doi: 10.4278/ajhp.080923-QUAL-211. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Merikangas KR. The national comorbidity survey replication (NCS-R): Background and aims. International Journal of Methods in Psychiatric Research. 2004;13:60–68. doi: 10.1002/mpr.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause N, Shaw B, Liang J. Social relationships in religious institutions and healthy lifestyles. Health Education & Behavior. 2011;38(1):25–38. doi: 10.1177/1090198110370281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen LJ. Current Population Reports, P20-551. Washington, DC: United States Census Bureau; 2004. The foreign-born population in the United States: 2003. [Google Scholar]
- Lev-Ran S, Le Strat Y, Imtiaz S, Rehm J, Le Foll B. Gender differences in prevalence of substance use disorders among individuals with lifetime exposure to substances: Results from a large representative sample. The American Journal on Addictions. 2013;22(1):7–13. doi: 10.1111/j.1521-0391.2013.00321.x. [DOI] [PubMed] [Google Scholar]
- Marsiglia FF, Kulis S, Nieri T, Parsai M. God Forbid! Substance Use Among Religious and Nonreligious Youth. American Journal of Orthopsychiatry. 2005;75(4):585–598. doi: 10.1037/0002-9432.75.4.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markides KS, Coreil J. The health of Hispanics in the southwestern United States: An epidemiologic paradox. Public Health Reports. 1986;101:253–265. [PMC free article] [PubMed] [Google Scholar]
- McLean CP, Asnaani A, Litz BT, Hofmann SG. Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness. Journal of Psychiatric Research. 2011;45(8):1027–1035. doi: 10.1016/j.jpsychires.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AS, Hoffmann JP. Risk and religion: An explanation of gender differences in religiosity. Journal for the Scientific Study of Religion. 1995;34(1):63–75. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. Seventh. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- Palloni A, Morenoff JD. Interpreting the paradoxical in the Hispanic Paradox: Demographic and epidemiological approaches. Annals of the New York Academy of Sciences. 2001;954:140–174. doi: 10.1111/j.1749-6632.2001.tb02751.x. [DOI] [PubMed] [Google Scholar]
- Pew Research Center. English Usage among Hispanics in the United States. 2007 Retrieved from: http://www.pewhispanic.org/files/reports/82.pdf.
- Pew Research Center. 2002 National Survey of Latinos. 2007 Retrieved from: http://www.pewhispanic.org/2002/12/17/2002-national-survey-of-latinos/
- Pew Research Center. U.S. population projections 2005–2050. 2015 Retrieved from http://pewhispanic.org/reports/report-php?RepostID=85.
- Rivera FI, Burgos G. The health status of Puerto Ricans in Florida. Centro Journal. 2010;22(1):199–217. [Google Scholar]
- Seeman TE, Dubin L, Seeman M. Religiosity/spirituality and health: A critical review of the evidence for biological pathways. American Psychologist. 2003;58(1):53–63. doi: 10.1037/0003-066x.58.1.53. [DOI] [PubMed] [Google Scholar]
- Seicean S, Neuhauser D, Strohl K, Redline S. An exploration of differences in sleep characteristics between Mexico-born US immigrants and other Americans to address the Hispanic Paradox. Sleep: Journal of Sleep and Sleep Disorders Research. 2011;34(8):1021–1031. doi: 10.5665/SLEEP.1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh GK, Miller BA. Health, Life Expectancy, and Mortality Patterns Among Immigrant Populations in the United States. Ruvue Canadienne de Santé Publique. 2004;95:14–21. doi: 10.1007/BF03403660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solis J. Re-thinking illegality as a violence against, not by Mexican immigrants, children, and youth. Journal of Social Issues. 2003;59:15–31. [Google Scholar]
- Stark R. Physiology and faith: Addressing the universal gender differences in religious commitment. Journal for the Scientific Study of Religion. 2002;41(3):495–507. [Google Scholar]
- Turra CM, Goldman N. Socioeconomic difference in mortality among U.S. adults: Insights into the Hispanic paradox. The Journals of Gerontology: Series B: Psychological Sciences and Social Sciences. 2007;62B(3):S184–S192. doi: 10.1093/geronb/62.3.s184. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Supporting the 2010 census: A toolkit for reaching Latinos. [Retrieved on February 10, 2012];2010 from: http://2010.census.gov/partners/pdf/toolkit_Latino_Overview.pdf.
- Vega WA, Sribney WM. Understanding the Hispanic health paradox through a multi-generation lens: A focus on behaviour disorders. In: Carlo G, Crockett LJ, Carranza MA, editors. Health disparities in youth and families: Research and applications. New York, NY US: Springer Science + Business Media; 2011. pp. 151–168. [DOI] [PubMed] [Google Scholar]
- Vick B, Jones K, Mitra S. Poverty and severe psychiatric disorder in the U.S.: Evidence from the Medical Expediture Panel Survey. Journal of Mental Health Policy and Economics. 2012;15(2):83–96. [PubMed] [Google Scholar]
- Zhang Z, Hayward MD, Lu C. Is there a Hispanic epidemiologic paradox in later life? A closer look at chronic morbidity. Research on Aging. 2012;34(5):548–571. [Google Scholar]