Highlights
-
•
Periprosthetic fracture non-unions are a medical challenge that requires a multi-level treatment.
-
•
Aggressive revision surgery and bone healing therapy are the best solutions for those cases.
-
•
The association of mechanical stability and the support to osteogenic processes can lead to fracture healing in non-union cases. Our method follows the Giannoudis’ “Diamond concept” about fracture healing.
Keywords: Non-union, Bone-healing, Peri-prosthetic fracture
Abstract
Introduction
The worldwide incidence of traumatic fractures has been growing over the last years due to the progressive aging of the population. Today, the increase of arthroplasty procedures in orthopaedic surgery is related to a high rate of peri-prosthetic fractures. Healing of the fracture is a multifactorial metabolic process; if these factors are impaired, healing process could be interrupted resulting in non-union.
Presentation of case
We report our experience about a case of a humeral diaphysis non-union secondary to peri-prosthetic fracture (reverse shoulder arthroplasty) treated by conservative approach.
Discussion
We treated this patient using a multilevel approach, consisting of revision surgery and drug therapy.
Conclusion
We assume that an aggressive revision surgery done with bone autograft implant and a bone healing therapy administering teriparatide off-label can reduce the convalescence in non-unions and can improve prognosis.
1. Introduction
The progressive increase of shoulder arthroplasty implants is correlated to a major incidence of peri-prosthetic fractures. The frequency of these traumatic events on shoulder is 0.6-3% and 40% of these cases are represented by low-energy post-operative fractures [1]. Treatment varies from conservative to implant revision and depends on the type of fracture and the stability of prosthesis [2], [3]. If not completely treated, peri-prosthetic fractures may lead to non-union.
2. Presentation of case
We report a case of a 64-years-old woman with a complete right upper limb dysfunction (DASH 32) [8] due to non-union (type B2 according to Worland classification) [4] occurred on a peri-prosthetic fracture at the distal end of the humeral stem of RSA (reverse shoulder arthroplasty), positioned 3 years before.
Immobilization with an arm brace was used as first conservative treatment.
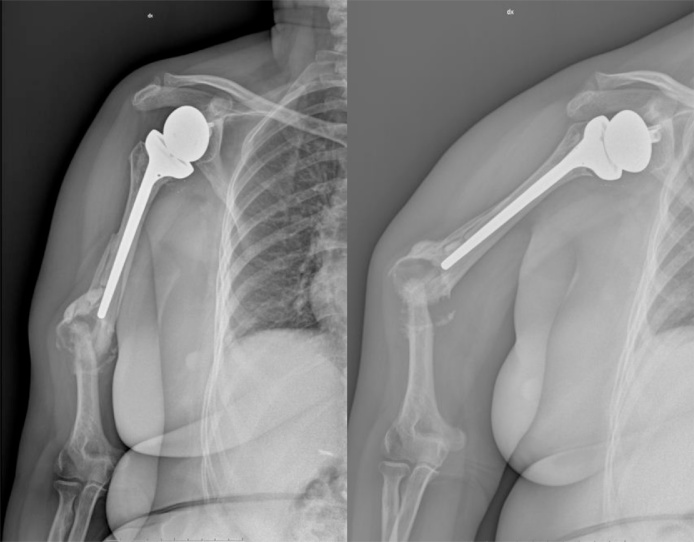
The following x-ray evaluations showed a progression from fracture to non-union and a varus angle deformity (Fig. 1).
Fig. 1.
Pre-operative x-ray view (left); varus angle deformity in shoulder abduction (right).
In order to definitively correct such deformity we chose surgical treatment. We removed fibrous tissue around the locus, reduced the fracture and performed osteo-synthesis with plate, screws and wires in addition to a massive bone autograft. At first a 15 cm autologous bone from peroneal diaphysis and a 8 cm piece of cortical bone from iliac crest were harvested. Then the fracture line was exposed and the surface was regularized, scratched and freshened (Fig. 2). Finally, we corrected the skeletal deformity and defect performing an osteo-synthesis of the fracture line using the autologous bone and a straight plate that was fixed distally with 3 screws, proximally with 4 screws and with 3 looping wires [5], [6] (Fig. 3).
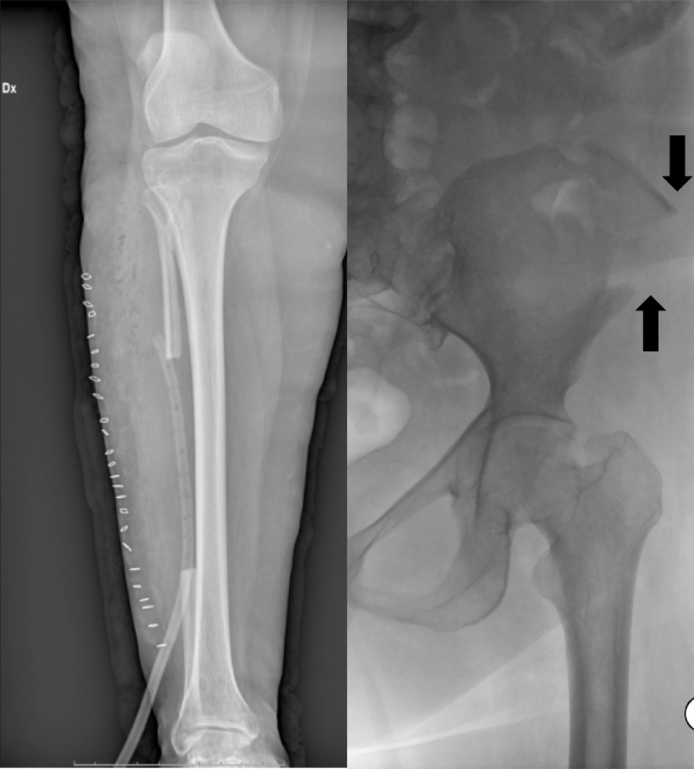
Fig. 2.
Autograft bone from peroneal diaphysis (left); cortical bone from iliac crest (right).
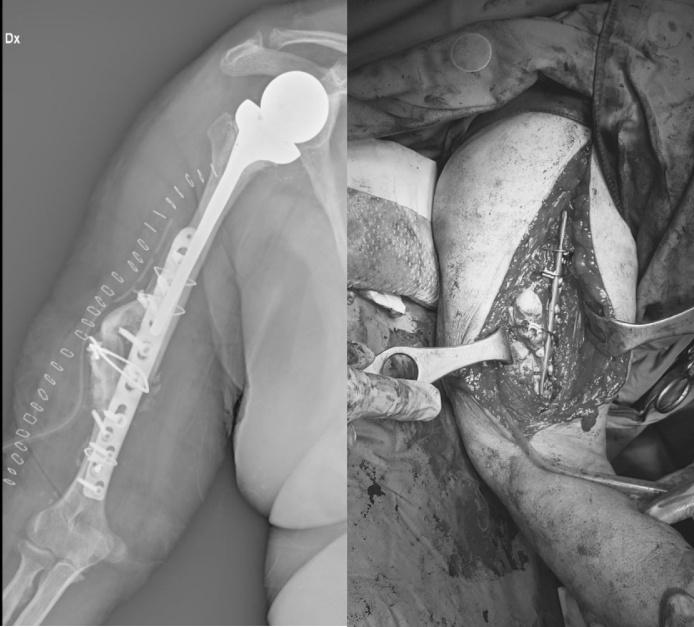
Fig. 3.
Post-operative x-ray (left); intraoperative view (right).
Postoperatively, the patient followed a therapy with Teriparatide (20 μg/die for 3 months) [7], [8]. X-ray control was performed at 3 months. Teriparatide is the foreshortened amino terminal peptide of PTH and has a osteoanabolic effect when administered once daily in low doses for the treatment of osteoporosis. There is evidence that Teriparatide also accelerates the fracture healing process by improving the biomechanical properties of the fracture callus, increasing endochondral ossification and bone remodelling in animal models [9].
The control X ray at 1 year postoperatively showed a complete fracture healing (Fig. 4). Clinical control was good (DASH Score 76) [10].
Fig. 4.
1 year post-operative x.ray.
3. Discussion
Multiple factors can contribute to fracture non-union. Humeral diaphysial fracture is always unstable and requires surgical approach. Non-union may occur after surgical treatment when a good reduction of the fracture or a stable fixation is not achieved. Systemic environment can be another cause of bone healing failure and non-union, but it is essential to respect biomechanical principles to reduce failure percentage.
The application of bone autografts offers an additional guarantee to “revitalize” non-union locus. Actually bone substitutes [11], scaffolds, bone marrow, platelet rich plasma [12] and mesenchymal stem cells represent a supplementary resource for efficacious treatment. In this case, we tried to achieve the best solution in mechanical stability (plate, screws and wires) and we combined a supportive treatment to osteogenic processes (autologous bone grafts and therapy with Teriparatide) [13]. Our method follows the Giannoudis’ “Diamond concept” about fracture healing [14].
4. Conclusions
Both biology and mechanics are essential for a successfully fracture healing process. These two factors have to blend together in order to lead to proliferative and differentiative cell processes. In the examined case, the correct reduction and osteo-synthesis of the fracture combined with Teriparatide therapy showed good clinical result.
This case report has been reported in line with the SCARE criteria [15].
Conflict of interest
Nothing to declare.
Author contributions
E.C. and L.P. data analysis and interpretation, writing the paper.
G.C and M.A. image preparation and study design.
C.D. overall responsibility, data analysis and interpretation, writing the paper.
Funding
The authors have no extra or intra-institutional funding to declare.
Ethical approval
This research did not receive any specific grant from funding agencies in the public, commercial or non-profit sectors.
Consent
Written informed consent for publication of their clinical details and/or clinical images was obtained from the parent of the patient.
Guarantor
Professor Carlo Doria.
Acknowledgements
Nil.
Contributor Information
Ciurlia Emanuele, Email: ciurlia81@gmail.com.
Puddu Leonardo, Email: l.puddu86@gmail.com.
Caggiari Gianfilippo, Email: gianfilippocaggiari@gmail.com.
Andreozzi Matteo, Email: matteo.andreozzi88@gmail.com.
Carlo Doria, Email: cdoria@uniss.it.
References
- 1.Della Rocca Gregory J., Leung K. Hans-Christoph Pape. Periprosthetic fractures: epidemiology and future projections. J. Orthop. Trauma. 2011;25:S66–S70. doi: 10.1097/BOT.0b013e31821b8c28. [DOI] [PubMed] [Google Scholar]
- 2.García-Fernández Carlos. Periprosthetic humeral fractures associated with reverse total shoulder arthroplasty: incidence and management. Int. Orthop. 2015;39(10):1965–1969. doi: 10.1007/s00264-015-2972-7. [DOI] [PubMed] [Google Scholar]
- 3.Mineo G.V. Management of shoulder periprosthetic fractures: our institutional experience and review of the literature. Injury. 2013;44:S82–S85. doi: 10.1016/S0020-1383(13)70018-4. [DOI] [PubMed] [Google Scholar]
- 4.Worland Richard L., Arredondo Jorge. Periprosthetic humeral fractures: management and classification. J. Shoulder Elbow Surg. 1999;8(6):590–594. doi: 10.1016/s1058-2746(99)90095-2. [DOI] [PubMed] [Google Scholar]
- 5.Trompeter Alex J., Gupta Rohit R. The management of complex periprosthetic humeral fractures: a case series of strut allograft augmentation, and a review of the literature. Strat. Trauma Limb. Reconstruct. 2013;8(1):43–51. doi: 10.1007/s11751-013-0155-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Finkemeier Christopher G. Bone-grafting and bone-graft substitutes. J. Bone Joint Surg. Am. 2002;84(3):454–464. doi: 10.2106/00004623-200203000-00020. [DOI] [PubMed] [Google Scholar]
- 7.Oteo-Álvaro Ángel, Moreno Enrique. Atrophyc humeral shaft nonunion treated with teriparatide (rh PTH 1-34): a case report. J. Shoulder Elbow Surg. 2010;19(7):e22–e28. doi: 10.1016/j.jse.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 8.Zhang Dafang. The role of recombinant PTH in human fracture healing: a systematic review. J. Orthop. Trauma. 2014;28(1):57–62. doi: 10.1097/BOT.0b013e31828e13fe. [DOI] [PubMed] [Google Scholar]
- 9.Ciurlia E., Tranquilli Leali P., Doria C. Use of Teriparatide off-label: our experience and review of literature. Clin. Cases Miner. Bone Metab. 2017;14(1):28–34. doi: 10.11138/ccmbm/2017.14.1.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gummesson Christina, Ward Michael M., Atroshi Isam. The shortened disabilities of the arm, shoulder and hand questionnaire (Quick DASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord. 2006;7(1) doi: 10.1186/1471-2474-7-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Emara Khaled M., Diab Ramy Ahmed, Emara Ahmed Khaled. Recent biological trends in management of fracture non-union’. World J. Orthop. 2015;6(September (8)):623–628. doi: 10.5312/wjo.v6.i8.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Caggiari G., Mosele G.R., Puddu L., Ciurlia E., Doria C. Efficacy of platelet-rich plasma in experimental instrumented interbody spinal fusion. Euro Mediterr. Biomed. J. 2016;11(10):141–147. [Google Scholar]
- 13.Doria C., De Santis V., Falcone G., Proietti L., De Santis E. Osseointegration in hip prostheses: experimental study in sheep. Int. Orthop. 2003;27(5):272–277. doi: 10.1007/s00264-003-0474-5. Epub 2003 Jun. 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Giannoudis P.V., Einhorn T.A., Marsh D. Fracture healing:the diamond concept. Injury. 2007;38:S3–S6. doi: 10.1016/s0020-1383(08)70003-2. [DOI] [PubMed] [Google Scholar]
- 15.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., The SCARE group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]