Abstract
Purpose
The aim of this study was to determine whether having an existing psychiatric disorder is a risk factor for developing post-operative infection following anterior cervical discectomy with fusion (ACDF) and posterior cervical fusion (PCF).
Results
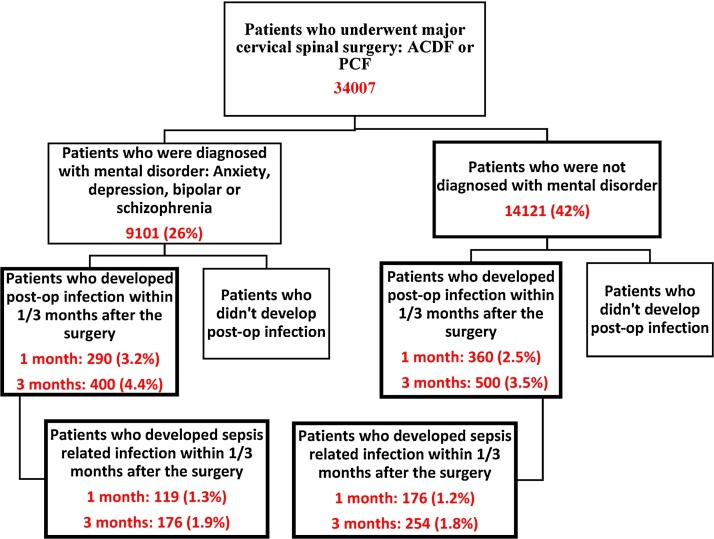
A total of 34,007 patients within Humana database was included in this study. Patients with mental disorders had post-operative infection rates of 3.2% and 4.4% within 1 and 3months, compared to 2.5% and 3.5% in patients without a psychiatric disorder (p < 0.05).
Conclusions
Patients with mental disorders had significantly higher rates of post-operative infection compared to patients who were never diagnosed with a psychiatric disorder.
Keywords: Cervical spine procedures, ACDF, PCF, Mental health, Post-operative infection, Sepsis
1. Introduction
The number of patients who undergo cervical spine procedures is increasing every year.1 Anterior cervical discectomy with fusion (ACDF) and posterior cervical fusion (PCF) are the most commonly performed cervical procedures.1, 2, 3 The increase in the number of surgical procedures performed exposes more patients to the risks of post-operative complications. Post-operative infection is a common and debilitating complication of cervical spine surgery. It has been reported that surgical site infection rates after cervical spine surgery vary between 1% to 6% and non-surgical site infection were reported at 2.8%.4, 5, 6, 7 Post-operative infections can extend the length of stay and increase healthcare expenditures between $3000 to $29,000 per case in the United States.4, 8
Previous studies have shown that risk factors such as diabetes, obesity, chronic steroid use, and length of surgery can contribute to the development of post-operative infections.9, 10, 11 The presence of a psychiatric illness was also demonstrated to be a risk factor in several types of procedures including total knee arthroplasty and coronary artery bypass.12, 13, 14, 15, 16 Menendez et al. reported that patients with depression, schizophrenia, or dementia had a higher rate of adverse events including wound complications, acute renal failure, pulmonary embolism, and an increased need for blood transfusion.21 To our knowledge, there is no research on the effects of psychiatric disorders on post-operative infections following cervical spine procedures. The main objective of this study was to show whether having a pre-existing psychiatric disorder was a risk factor for developing infections following ACDF and PCF procedures.
2. Materials & methods
In this retrospective study, PearlDiver Technologies was used to analyze the Humana database from 2007 to the 3rd quarter of 2015. Patients who underwent primary cervical spine surgery (ACDF or PCF) were included in the study. Patients were followed for 3 months following the surgery to determine if a postoperative infection occurred. Corresponding International Classification of Disease, 9th edition (ICD-9) diagnosis codes for psychiatric disorders (depression, anxiety, bipolar disorder, schizophrenia) and post-operative infections were used. For ACDF and PCF procedures, corresponding ICD-9 procedural codes and Current Procedural Terminology (CPT) codes were used (Appendix A). The main study group was defined as patients who underwent primary ACDF or PCF procedures. This group was subdivided into patients who had a diagnosis of psychiatric disorder on the day of surgery or within 60 days prior to surgery, and patients who were never diagnosed with specific psychiatric disorders. Patients who had a psychiatric disease in the past but did not carry the diagnosis within 60 days prior to surgery were excluded. The psychiatric diseases with the highest incidence in the United States (anxiety, depression, bipolar disorder, and schizophrenia) were included. Each group was further divided based on presence or absence of postoperative infection (Fig. 1). Potential infections included surgical site, urinary tract, catheter related, and sepsis. Since PearlDiver does not allow for classification of infection severity, sepsis was analyzed separately to determine if patients with psychiatric disorders are more prone to severe infections. Due to the large number of patients with multiple psychiatric conditions, the sum of patients with a single psychiatric disorder was lower than the number of patients in the total psychiatric disorder group. Chi-square test was used to calculate p value, odds ratio (OR) and confidence interval (CI) in this study. Since all the information obtained was de-identified, this study was exempt from our institutional review board approval. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Fig. 1.
Study groups.
3. Results
3.1. Demographics
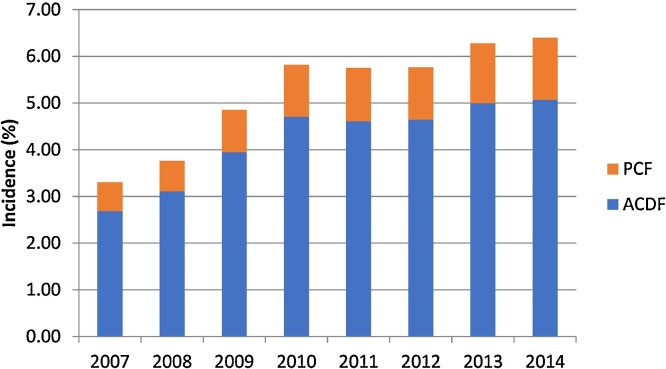
A total of 34,007 patients who underwent primary ACDF or PCF were included in this study. Eighty percent of these patients had ACDF while the remainder had PCF. There were 17,280 female and 16,727 male patients. There were no significant differences in terms of gender. The age group 65 to 69-years of age had the highest prevalence of both ACDF and PCF (18% and 20%, respectively). The incidence of patients undergoing ACDF and PCF demonstrated a rising trend from 2007 to 2015 (Fig. 2).
Fig. 2.
Trend in ACDF and PCF procedures.
3.2. Psychiatric disorders
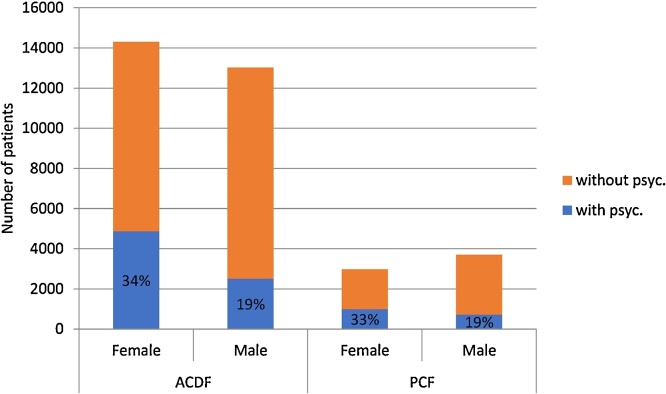
Twenty-six percent of the patients included in this study were diagnosed with at least one of the specified psychiatric disorders within 60 days prior to surgery (Fig. 3). Forty-two percent of the patients were never diagnosed with any of the specific diseases. The remaining patients were either diagnosed with a psychiatric disease in the past but did not have the diagnosis during the 60-day period prior to the surgery, or were diagnosed with a psychiatric disease after the surgery. Thirty-four percent of female patients had a diagnosis of at least one of the psychiatric diseases while only 19% of male patients had a psychiatric diagnosis (p value < 0.0001). There were no significant differences between the ACDF and PCF patients in terms of mental disorder prevalence. When individual psychiatric diseases were analyzed, there were 1446 (4.2%) patients with depression only, 1160 (3.4%) patients with anxiety only, and 75 (0.2%) patients with bipolar only. Due to the PearlDiver privacy policy, numbers <11 were not displayed. Therefore, we were unable to report patients with schizophrenia only. The remaining patients were diagnosed with multiple disorders.
Fig. 3.
Patient demographics.
3.3. Post-operative infections
Post-operative infection rates were 3% and 4.2% at 1 and 3 months after the surgery, respectively (Table 1, Table 2). The highest prevalence of post-operative infection was in 65 to 69-year old patients. When ACDF and PCF patients were reviewed separately, there was a dramatic difference regarding the infection rates. At one-month follow up, the infection rate for ACDF patients was 1.8% compared to 7.7% for PCF patients (p value < 0.001, OR = 0.2259 Table 1). Within 3 months, rates were 2.6% and 10% respectively (p value < 0.001, OR = 0.2317 Table 2). Two-point four percent of female patients developed a post-operative infection within 1 month compared to 3.6% male patients (p value < 0.001, OR = 0.6432 Table 1). At three-month follow-up, infection rates were 3.3% and 5% for female and male patients, respectively (p value < 0.001, OR = 0.6527 Table 2).
Table 1.
Post-op infection and sepsis rates at 1 month.
| Factor | Absent |
Present |
p value |
OR (95% CI) |
|---|---|---|---|---|
| Post-op infection within 1 month | ||||
| Mental Disorder | ||||
| With | 8811 | 290 | 1.2581 | |
| without | 13761 | 360 | 0.004 | (1.0754−1.4719) |
| Surgery type | ||||
| ACDF | 26822 | 505 | 0.2259 | |
| PCF | 6166 | 514 | <0.0001 | (0.1991−0.2562) |
| Gender | ||||
| Female | 16870 | 410 | 0.6432 | |
| Male | 16118 | 609 | <0.0001 | (0.5665−0.7304) |
| Factor | Absent |
Present |
p value |
OR (95% CI) |
|---|---|---|---|---|
| Post-op sepsis within 1 month | ||||
| Mental Disorder | ||||
| With | 8982 | 119 | 1.0497 | |
| without | 13945 | 176 | 0.68 | (0.8306−1.3267) |
| Surgery type | ||||
| ACDF | 27077 | 250 | 0.2625 | |
| PCF | 6453 | 227 | <0.0001 | (0.2189−0.3148) |
| Gender | ||||
| Female | 17103 | 177 | 0.5667 | |
| Male | 16427 | 300 | <0.0001 | (0.47−0.6832) |
Table 2.
post-op infection and sepsis rates at 3 months.
| Factor | Absent | Present | P value | OR (95% CI) |
|---|---|---|---|---|
| Post-op infection within 3 months | ||||
| Mental Disorder | ||||
| With | 8701 | 400 | 1.2524 | |
| Withou | 13621 | 500 | 0.000993 | (1.095−1.4322) |
| Surgery Type | ||||
| ACDF | 26601 | 726 | 0.2317 | |
| PCF | 5976 | 704 | <0.0001 | (0.2081−0.2579) |
| Gender | ||||
| Female | 16698 | 582 | 0.6527 | |
| Male | 15879 | 848 | <0.0001 | (0.586−0.7269) |
| Factor | Absent | Present | P value | OR (95% CI) |
|---|---|---|---|---|
| Post-op sepsis within 3 months | ||||
| Mental Disorder | ||||
| With | 8925 | 176 | 1.0766 | |
| Without | 13867 | 254 | 0.45426 | (0.8867−1.3072) |
| Surgery Type | ||||
| ACDF | 26954 | 373 | 0.2613 | |
| PCF | 6344 | 336 | <0.0001 | (0.2249−0.3035) |
| Gender | ||||
| Female | 17013 | 267 | 0.5782 | |
| Male | 16285 | 442 | <0.0001 | (0.496- 0.6741) |
Data regarding the main objective of this study showed that the post-operative infection rate among patients with a psychiatric disease was 3.2% within a 1-month follow-up period after the surgery, compared to 2.5% among patients who were never diagnosed with a specific psychiatric disorder(p-value = 0.004, OR = 1.2581). Within a 3-months follow-up period, 4.4% of patients with mental health disorders developed a post-operative infection compared to 3.5% of the patients without psychiatric disease (p-value < 0.01, OR = 1.2524). The highest prevalence of post-operative infection was in the 65 to 69-year old group for psychiatric disorder patients, compared to the 70 to 74-year old group for patients without a psychiatric disorder. When ACDF and PCF patients were analyzed separately, the effect of mental health on post-operative infection rates was statistically significant (p value = 0.0003, OR = 1.5025) for ACDF patients but not for PCF patients (Table 3).
Table 3.
Effect of mental health on post-op infection rates among different surgery types.
| Infection 1m | Infection 3m | Sepsis 1m | Sepsis 3m | ||
|---|---|---|---|---|---|
| ACDF | Mental (7380) | 162 | 223 | 73 | 105 |
| Nomental (11415) | 168 | 239 | 86 | 126 | |
| pvalue | 0.000226 | <0.0001 | 0.084822 | 0.052493 | |
| PCF | Mental (1721) | 128 | 177 | 46 | 71 |
| Nomental (2706) | 192 | 261 | 90 | 128 | |
| pvalue | 0.671373 | 0.488422 | 0.219139 | 0.342782 | |
Of patients diagnosed with depression only, 2.6% developed post-operative infection within 1 month and 3.7% within 3 months (Table 4). One and 3-months post-operative infection rates of patients diagnosed with anxiety only were 2% and 2.7%, respectively (Table 4). Pearl Diver privacy policy prevented reporting of infection rates among patients with only bipolar disorder and only schizophrenia.
Table 4.
Effect of different mental health disorders on the infection and sepsis rates at 1 and 3 months post-operatively.
| Infection |
Sepsis |
|||
|---|---|---|---|---|
| 1 month | 3 months | 1 month | 3 months | |
| Only Depression | 38(2.6%) | 54(3.7%) | 20(1.3%) | 29(2%) |
| n = 1446 | ||||
| Only Anxiety | 23(2%) | 31(2.7%) | 13(1.1%) | 16(1.4%) |
| n = 1160 | ||||
| No mental | 360(2.5%) | 500(3.5%) | 176(1.2%) | 254(1.8%) |
| n = 14121 | ||||
| Total mental | 290(3.2%) | 400(4.4%) | 119(1.3%) | 176(2%) |
| n = 9101 | ||||
3.4. Sepsis
Total sepsis rates within 1 month and 3 months after the surgery were 1.4% and 2.1% respectively (Table 1 and 2). The highest prevalence of sepsis was in the 70 to 74- year old group. When ACDF and PCF patients were reviewed separately, there was a dramatic difference regarding the sepsis rates. At 1-month follow-up, the sepsis rate for ACDF patients was 0.9%, compared to 3.5% for PCF patients (p < 0.001, Table 1). With regard to gender, 1% of female and 1.8% of male patients developed sepsis within 1 month after surgery (Table 1). Within 3 months these rates increased to 1.5% and 2.6% respectively (p < 0.0001, Table 2). Mental health did not have a significantly effect on sepsis rates in regard to gender.
Sepsis occurred in 1.3% of patients with psychiatric diseases within 1 month, increasing to 1.9% within 3 months after the surgery (Table 4). Among patients without any specific psychiatric illness, sepsis rates for 1 and 3-months follow-up periods were 1.2% and 1.8%, respectively.
Of those patients who were diagnosed with only depression, 1.4% developed post-operative sepsis within 1 month and 2% within 3 months. 1month and 3-months post-operative sepsis rates of patients diagnosed with only anxiety were 1.1% and 1.4%, respectively (Table 4).
4. Discussion
Post-operative infection can be a debilitating complication of cervical spine surgery, and preoperative risk factors may play an important role. This study demonstrates that patients with pre-existing psychiatric disorders had higher rates of infection following ACDF and PCF procedures compared to patients not diagnosed with specific psychiatric disorders. One-month infection rate was significantly higher in patients with psychiatric disorders compared to patients without a psychiatric diagnosis. At 3 months follow up period the difference between infection rates of patients without a psychiatric diagnosis and patients with psychiatric problems was still significant. Rates of post-operative sepsis were similar between the groups. When analyzing surgery type and gender, we found that, male patients developed significantly higher rates of infection and sepsis compared to female patients. Furthermore, PCF patients had higher post-operative infection and sepsis rates compared to ACDF patients.
There are several studies investigating the effects of psychiatric conditions on post-operative complications following various types of surgeries. Weinberg et al.20 reported that depression increased post-operative complications in orthopedic poly-trauma patients. Klement et al.12 demonstrated that pre-existing psychiatric diseases significantly increased peri-prosthetic infections and wound complications following primary total knee arthroplasty. Similarly, Menendez et al.21 found that patients with mental disorders experienced more adverse events such as wound complications, acute post-operative anemia, and pneumonia following major spinal surgeries, most dramatically for patients with schizophrenia and dementia.
ACDF and PCF are the most commonly performed cervical spine procedures and the incidence of these surgeries is increasing every year.17 Studies have shown that rates of ACDF and PCF rose by 184% and 464% from 1992 to 2005, respectively.2 Similarly, our study found a rising trend in the incidence of ACDF and PCF procedures from 2007 to 2015.
WHO World Mental Health (WMH) surveys on the global burden of mental disorders reported the prevalence of any mental disorder among the U.S population was 47.4%.18 In our study group, 26% of the patients undergoing cervical spine surgery had at least one of the psychiatric disorders. A lower overall rate of psychiatric diseases in the study population is likely explained by the selection bias of surgeons choosing patients without underlying psychiatric illnesses, and the fact that the psychiatric diseases included in this study were limited to anxiety, depression, bipolar disorder, and schizophrenia. In 2014, the NIH reported that psychiatric disorders were more common among female patients. In their report, 21.8% of adult females in the US had some kind of mental disorder compared to 14.1% of males.19 Similarly, in our study group, female patients had significantly higher rates of psychiatric disorder.
Previous studies have reported overall infection rates following spine surgeries between 1 and 6%.4, 5, 6, 7 In our study, 3% of patients developed a post-operative infection following ACDF and PCF. Interestingly, there was a dramatic difference between ACDF and PCF procedures regarding rates of infection and sepsis. Infection and sepsis rates for PCF patients were three to four times higher than ACDF patients. Similarly, Harel et al.22 reported that total infection rates following posterior approach cervical spine surgery were more than two times higher than anterior approach surgery.
Several controversial studies exist in the literature regarding gender as a risk factor for post-operative infection following spinal procedures.23 Rao et al.6 reported that male gender was a significant risk factor for surgical site infection following spinal fusion surgery. Similarly, in our study male patients developed higher rates of post-operative infection and sepsis compared to female patients.
In the current study, each psychiatric disorder was reviewed separately. Patients with depression only developed post-operative infection slightly more than patients without any specific mental disorder. This data suggests that patients with multiple diagnoses were the main group contributing to the higher infection rates among patients with psychiatric disorders compared to patients with no psychiatric illness, 3.2% vs. 2.5% respectively. In 2011 Bozic et al.13 reported that depression increased peri-prosthetic infection rate following TKA. However, in their methodology, diagnosis of depression did not seem to be exclusive. Another possible explanation for the differences in results might be due to our exclusion of patients who potentially had diagnosis of psychiatric disorders in the past but not within 60 days before surgery or on the day of surgery.
There was no significant difference in sepsis rates between patients with and without psychiatric illness. Klement et al.12 found that effect of psychiatric disease on post-operative sepsis was statistically significant. These incongruous findings could be attributed to the fact that their study did not include patients with anxiety. Since our anxiety only group showed lower infection rates, this might have contributed to overall lower sepsis rates among patients with psychiatric disorders.
A possible explanation for higher post-operative infection rates among patients with psychiatric illness can be due to immune modulation. In their literature review, Gnoheim and O’Hara24 stated that psychological stress causes inflammatory response through cytokines IL-1B, IL-6 and TNFα. Similarly, Leonard and co-authors25 reported that depression induces immune dysfunction by acting on pro-inflammatory cytokines. Furthermore, patients with schizophrenia tend to have poor personal hygiene26 which might further contribute to the increase in infection rates. Moreover, adverse behavioral changes, such as poorer self-care and reduced adherence to post-operative instructions are often associated with depression.27
There were several limitations in this study. This study focused on four common psychiatric disorders; depression, anxiety, bipolar disorder, and schizophrenia. It is likely that including all psychiatric diagnoses would potentially increase overall infection rates among patients with mental disorders. Secondly, the data that was collected through billing codes and medical records were not available due to the nature of database. Thirdly, the severity of psychiatric disorders and infections remains unknown. Despite these limitations, this is the first study to elucidate that patients with pre-existing mental health disorders are more prone to develop post-operative infections following cervical spine procedures.
5. Conclusion
Post-operative infection is a very serious complication of cervical spine surgery. Patients with pre-existing psychiatric disorders developed significantly higher infection rates following ACDF and PCF compared to those patients without psychiatric illness. Clinical staff should evaluate the mental health of their patients and counsel them accordingly.
Conflict of interest
There are no conflicts of interest for the current study.
Disclosures outside of submitted work
ZB-Xenco Medical (consultancy), AO Spine (consultancy, past); PCH- Consulting: DePuy Synthes Spine, Medtronic, NuVasive; JCW – Royalties: Aesculap, Biomet, Amedica, Seaspine , Synthes ; Stock Ownership: Fziomed; Private Investments: Promethean Spine, Paradigm spine, Benevenue, NexGen, Vertiflex, electrocore, surgitech, expanding orthopaedics, osprey, bone biologics, curative biosciences, pearldiver; Board of Directors: North American Spine Society (non-financial, reimbursement for travel for board meetings, courses, etc.), North American Spine Foundation (non-financial), Cervical Spine Research Society (non-financial, reimbursement for travel for board meetings), AO Spine/AO Foundation (honorariums for board position); Fellowship Support: AO Foundation (spine fellowship funding paid to institution).
Appendix A. ICD-9 and CPT codes for procedures, psychiatric disorders and infections.
| Description | Codes |
|---|---|
| Procedures | |
| ACDF | CPT-22551, CPT-22554, CPT-22548, ICD-9-P-8102, ICD-9-P-8101 |
| PCF | CPT-22600, CPT-22590, CPT-22595, ICD-9-P-8103 |
| Psychiatricdisorders | |
| Depression | ICD-9-D-29630:ICD-9-D-29636,ICD-9-D-311, ICD-9-D-29620:ICD-9-D-29626 |
| Anxiety | ICD-9-D-30000, ICD-9-D-30001, ICD-9-D-3004, ICD-9-D-30002 |
| Bipolar | ICD-9-D-29600:ICD-9-D-29606, ICD-9-D-29640:ICD-9-D-29646, ICD-9-D-29650: ICD-9-D-29656, ICD-9-D-29660: ICD-9-D-29666, ICD-9-D-2967, ICD-9-D-29680:ICD-9-D-29689 |
| Schizophrenia | ICD-9-D-29500:ICD-9-D-29505, ICD-9-D-29510:ICD-9-D-29515, ICD-9-D-29520:ICD-9-D-29525, ICD-9-D-29530:ICD-9-D-29535, ICD-9-D-29540:ICD-9-D-29545, ICD-9-D-29550:ICD-9-D-29555, ICD-9-D-29560:ICD-9-D-29565, ICD-9-D-29570:ICD-9-D-29575, ICD-9-D-29580:ICD-9-D-29585, ICD-9-D-29590:ICD-9-D-29595 |
| Post-op infection | ICD-9-D-99590:ICD-9-D-99592,ICD-9-D-99660,ICD-9-D-99662:ICD-9-D-99664,ICD-9-D-99666:ICD-9-D-99668,ICD-9-D-9972, ICD-9-D-99802, ICD-9-D-99851, ICD-9-D-99859, ICD-9-D-9986, ICD-9-D-9992, ICD-9-D-99931:ICD-9-D-99934, ICD-9-D-99939 |
| Sepsis | ICD-9-D-99802, ICD-9-D-99590:ICD-9-D-99592 |
References
- 1.Oglesby M., Fineberg S.J., Patel A.A., Pelton M.A., Singh K. Epidemiological trends in cervical spine surgery for degenerative diseases between 2002 and 2009. Spine. 2013;38(14):1226–1232. doi: 10.1097/BRS.0b013e31828be75d. [DOI] [PubMed] [Google Scholar]
- 2.Wang M.C., Kreuter W., Wolfla C.E., Maiman D.J., Deyo R.A. Trends and variations in cervical spine surgery in the United States. Spine. 2009;34(9):955–961. doi: 10.1097/BRS.0b013e31819e2fd5. [DOI] [PubMed] [Google Scholar]
- 3.Marquez-Lara A., Nandyala S.V., Fineberg S.J., Singh K. Current trends in demographics, practice and in-hospital outcomes in cervical spine surgery. Spine. 2014;39(6):476–481. doi: 10.1097/BRS.0000000000000165. [DOI] [PubMed] [Google Scholar]
- 4.Garza-Ramos R.D.L., Abt N.B., Kerezoudis P. Deep-wound and organ-space infection after surgery for degenerative spine disease: an analysis from 2006 to 2012. Neurol Res. 2016;38(2):117–123. doi: 10.1080/01616412.2016.1138669. [DOI] [PubMed] [Google Scholar]
- 5.Tominaga H., Setoguchi T., Ishidou Y., Nagano S., Yamamoto T., Komiya S. Risk factors for surgical site infection and urinary tract infection after spine surgery. Eur Spine J. 2016;25(Dec(12)):3908–3915. doi: 10.1007/s00586-016-4674-2. Epub 2016 Jun 27. [DOI] [PubMed] [Google Scholar]
- 6.Rao S.B., Vasquez G., Harrop J. Risk factors for surgical site infections following spinal fusion procedures: a case-control study. Clin Infect Dis. 2011;53(7):686–692. doi: 10.1093/cid/cir506. [DOI] [PubMed] [Google Scholar]
- 7.Cheung J.P.Y., Luk K.D.-K. Complications of anterior and posterior cervical spine surgery. Asian Spine J. 2016;10(2):385. doi: 10.4184/asj.2016.10.2.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson D.J., Podgorny K., Berríos-Torres S.I. Strategies to prevent surgical site infections in acute care hospitals 2014 update. Infect Control Hosp Epidemiol. 2014;35(6):605–627. doi: 10.1086/676022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Koutsoumbelis S., Hughes A.P., Girardi F.P. Risk factors for postoperative infection following posterior lumbar instrumented arthrodesis. J Bone Joint Surg Am. 2011;93(17) doi: 10.2106/JBJS.J.00039. [DOI] [PubMed] [Google Scholar]
- 10.Imajo Y., Taguchi T., Yone K. Japanese 2011 nationwide survey on complications from spine surgery. J Orthop Sci. 2015;20(1):38–54. doi: 10.1007/s00776-014-0656-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheung J.P.Y., Luk K.D.-K. Complications of anterior and posterior cervical spine surgery. Asian Spine J. 2016;10(2):385. doi: 10.4184/asj.2016.10.2.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klement M.R., Nickel B.T., Penrose C.T. Psychiatric disorders increase complication rate after primary total knee arthroplasty. Knee. 2016;23(5):883–886. doi: 10.1016/j.knee.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 13.Bozic K.J., Lau E., Kurtz S., Ong K., Berry D.J. Patient-related risk factors for postoperative mortality and periprosthetic joint infection in medicare patients undergoing TKA. Clin Orthop Relat Res®. 2011;470(1):130–137. doi: 10.1007/s11999-011-2043-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Browne J.A., Sandberg B.F., D’apuzzo M.R., Novicoff W.M. Depression is associated with early postoperative outcomes following total joint arthroplasty: a nationwide database study. J Arthroplast. 2014;29(3):481–483. doi: 10.1016/j.arth.2013.08.025. [DOI] [PubMed] [Google Scholar]
- 15.Doering L. Relation of depression, natural killer cell function, and infections after coronary artery bypass in women. Eur J Cardiovasc Nurs. 2008;7(1):52–58. doi: 10.1016/j.ejcnurse.2007.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beresnevaitė M., Benetis R., Taylor G.J., Jurėnienė K., Kinduris Š., Barauskienė V. Depression predicts perioperative outcomes following coronary artery bypass graft surgery. Scand Cardiovasc J. 2010;44(5):289–294. doi: 10.3109/14017431.2010.490593. [DOI] [PubMed] [Google Scholar]
- 17.Angevine P.D., Arons R.R., Mccormick P.C. National and regional rates and variation of cervical discectomy with and without anterior fusion, 1990–1999. Spine. 2003;28(9):931–939. doi: 10.1097/01.BRS.0000058880.89444.A9. [DOI] [PubMed] [Google Scholar]
- 18.Kessler R.C., Aguilar-Gaxiola S., Alonso J. The global burden of mental disorders: an update from the WHO world mental health (WMH) surveys. Epidemiologia e PsichiatriaSociale. 2009;18(01):23–33. doi: 10.1017/s1121189x00001421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.NIMH . U.S National Library of Medicine; 2017. Any Mental Illness (AMI) Among U.S. Adults. [ https://www.nimh.nih.gov/health/statistics/prevalence/any-mental-illness-ami-among-us-adults.shtml, Accessed 9 October 2016] [Google Scholar]
- 20.Weinberg D.S., Narayanan A.S., Boden K.A., Breslin M.A., Vallier H.A. Psychiatric illness is common among patients with orthopaedic polytrauma and is linked with poor outcomes. J Bone Joint Surg. 2016;98(5):341–348. doi: 10.2106/JBJS.15.00751. [DOI] [PubMed] [Google Scholar]
- 21.Menendez M.E., Neuhaus V., Bot A.G.J., Ring D., Cha T.D. Psychiatric disorders and major spine surgery. Spine. 2014;39(2) doi: 10.1097/BRS.0000000000000064. [DOI] [PubMed] [Google Scholar]
- 22.Harel R., Stylianou P., Knoller N. Cervical spine surgery: approach-related complications. World Neurosurg. 2016;94:1–5. doi: 10.1016/j.wneu.2016.06.099. [DOI] [PubMed] [Google Scholar]
- 23.Meng F., Cao J., Meng X. Risk factors for surgical site infections following spinal surgery. J Clin Neurosci. 2015;22(12):1862–1866. doi: 10.1016/j.jocn.2015.03.065. [DOI] [PubMed] [Google Scholar]
- 24.Ghoneim M.M., O’Hara M.W. Depression and postoperative complications: an overview. BMC Surg. 2016;16(1) doi: 10.1186/s12893-016-0120-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Leonard B.E. The concept of depression as a dysfunction of the immune system. Mod Trends Pharmacopsychiatry Dep: Psychopathol Pharmacother. 2010:53–71. [Google Scholar]
- 26.Brewer W.J., Edwards J., Anderson V., Robinson T., Pantelis C. Neuropsychological, olfactory, and hygiene deficits in men with negative symptom schizophrenia. Biol Psychiatry. 1996;40(10):1021–1031. doi: 10.1016/0006-3223(95)00594-3. [DOI] [PubMed] [Google Scholar]
- 27.Doering L., Moser D., Lemankiewicz W., Luper C., Khan S. Depression, healing, and recovery from coronary artery bypass surgery. Am J Crit Care. 2005;14(4):316–324. [PubMed] [Google Scholar]