INTRODUCTION
Despite the well-established population burden of chronic obstructive pulmonary disease (COPD), an adequate diagnosis remains a challenge for clinicians and healthcare managers. Recent epidemiological studies are consistently reporting high figures of inadequate diagnosis.
Interestingly, although the term ‘underdiagnosis’ is well accepted and understood, the opposite concept is referred to with a range of terms, for example, overdiagnosis, improper diagnosis, or misdiagnosis. However, they are not synonymous terms, and refer to different situations, with different potential consequences for patients.1 A unified consensus definition is needed for the different clinical scenarios.
The consequences of this underdiagnosis are obvious and directly affect patients not receiving adequate health care for their condition,2 or not controlling a disease that may impact on other comorbidities.3 Additionally, underdiagnosis may impact healthcare resources, because the therapeutic management would not be focused on the right disease. The consequences of this incorrect or wrong diagnosis impact several domains, with many patients receiving pharmacological treatment that is not needed and has a potential for drug-related adverse effects, giving health services to the wrong patients, subjecting them to tests, labelling them as sick or at-risk, telling them to modify their daily living habits, or insisting on monitoring them regularly. Last but not least, it also impacts on the health system, leading to potential extra costs.4,5
The issue of overdiagnosis and overtreatment of COPD was recently highlighted in a large ‘real-world’ study conducted in primary care in the UK, where only two-thirds of diagnoses had been made with spirometry, and of them 29% did not meet the GOLD criteria compatible with COPD. Out of the 1749 (49%) with confirmed COPD by spirometry, 8.6% were undertreated and 38% were overtreated. Overprescription of inhaled steroids was associated with adverse events such as pneumonia, and higher costs.6
In COPD, where treatment is often escalated in the hope of easing the burden of disease, clinicians should confirm the diagnosis before treatment, and then consider both the risks and benefits of treatment, and the costs where the benefits are unproven. Recently, Carter et al7 proposed a theoretical, generic terminology to clearly differentiate within clinical situations regarding inadequate diagnosis. We would like to propose some different concepts relating to misdiagnosis in COPD, and expand previous proposals.
CORRECT DIAGNOSIS OF COPD
COPD is a respiratory condition with chronic airway obstruction resulting from the exposure to different inhaled particles or substances, of which tobacco smoke is the major causal factor.8 The correct diagnosis of COPD should be based on two pillars: the confirmation of a chronic exposure to inhaled substances such as active or passive smoking, and the presence of a non-reversible airway obstruction.8 In order to obtain a precise diagnosis, there are four aspects to consider.
First, although tobacco smoke is the most frequent and principal risk factor for developing COPD, other substances have been described, including biomass-related smoke, occupational exposures, and other forms of indoor or outdoor pollution.9
Second, the physiological parameter to detect a chronic non-reversible airway obstruction is a matter of debate. By consensus, this obstruction is defined with spirometry performed after the administration of a short-acting bronchodilator by a forced volume in the first second (FEV1)/forced vital capacity (FVC) ratio below 0.7.10 However, other authors have proposed other forms of identifying a non-reversible airway obstruction including the lower limit of normal for an FEV1/FVC ratio instead of a fixed ratio.11
Third, although symptoms help the clinician to suspect the disease, the final individual diagnosis relies on a confirmed risk exposure in the medical record, and the presence of a non-reversible airway obstruction.8 Accordingly, the presence of symptoms considered as a diagnostic criterion is also a matter of controversy and current guidelines are not clear-cut whether symptoms should or should not be a diagnostic criterion for COPD.8
Fourth, COPD is known to be a complex, heterogeneous condition with different disease clinical phenotypes. With better understanding of the pathogenesis of COPD and the development of new and better diagnostic techniques, the original pink puffer and blue boater phenotypes have been expanded and different clinical presentations are now acknowledged.12 Also, an evaluation of severity should be part of the diagnostic process, in order to guide treatment selection. Accordingly, diagnosis cannot only rely on the simple detection of bronchial obstruction in an appropriate clinical context but must also consider other aspects, the type of COPD and assessment of its severity, to make a comprehensive, full diagnosis.13
MISDIAGNOSIS DEFINITIONS IN COPD
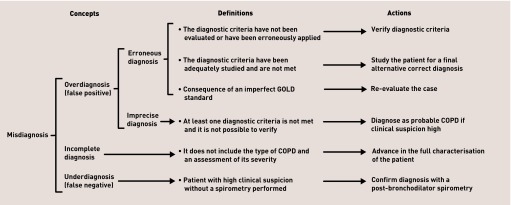
Bearing all these premises in mind, related errors in COPD diagnosis can be systematised and are summarised in Figure 1.
Figure 1.
Concepts, definitions, and actions for misdiagnosis in COPD. COPD = chronic obstructive pulmonary disease.
Misdiagnosis
Contrary to Carter and colleagues proposing ‘too much medicine’ as an umbrella term for overdiagnosis,7 in COPD, however, we believe that the umbrella term should be misdiagnosis itself (Figure 1).
Overdiagnosis or overdetection
According to Carter and colleagues, a real overdiagnosis in the narrow sense occurs whenever an (asymptomatic) patient is diagnosed with a condition, and the diagnosis does not produce a net benefit for that patient.7 In COPD, however, this is controversial. Once established, COPD progresses over time, especially if exposure to inhaled toxins persists. This implies that an earlier diagnosis will surely have an impact on patients in the long term, even if asymptomatic now, as it has been described that the earlier COPD is treated, the better the long-term prognosis.14 Accordingly, overdiagnosis or overdetection in COPD should be left for those cases in which a diagnosis is wrongly established (false positive). Two clinical scenarios reflect this: erroneous diagnosis and imprecise diagnosis.
Erroneous diagnosis
This would be related to the establishment of a diagnosis when the diagnostic criteria are not met; for example, having previous risk factor exposure with no spirometry, or having an obstructive spirometry without risk factor exposure. Additionally, in COPD the use of an imperfect GOLD standard like the post-bronchodilator FEV1:FVC ratio may lead to a false diagnosis. This may happen in several clinical scenarios, for example, using the fixed FEV1:FVC ratio in older patients or those cases with non-reversible airflow obstruction at diagnosis that return to normal with treatment or spontaneously over time.
Imprecise diagnosis
This may include those cases with a compelling clinical context in which it is impossible to perform spirometry, diagnosis based on a pre-bronchodilator spirometry, or those cases where tobacco or other previous exposures are not recorded.
Incomplete diagnosis
As stated before, diagnosis of the disease cannot rely on the simple detection of bronchial obstruction in an appropriate clinical context. Instead, it must include at least the type of COPD and an assessment of its severity.13 Whenever any of these are lacking, an incomplete diagnosis occurs.
Underdiagnosis
This occurs when a patient has an adequate clinical context, based on risk factor exposure, with or without symptoms, but the diagnosis has not been confirmed by spirometry.
STRATEGIES FOR IMPROVEMENT
The definition and differential diagnosis using these alternatives could be the basis for the implementation of initiatives aimed at benchmarking detection and case-finding strategies. The main measures to promote an adequate diagnosis for patients with suspected COPD should start with high-quality spirometry. If persistent airflow limitation is identified, the causes of this airflow limitation should be systematically explored, including all relevant key aspects needed for the correct evaluation of these patients to establish their final diagnosis, type of disease presentation, and eventually the objective staging and severity of COPD patients.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
REFERENCES
- 1.Miller MR, Levy ML. Chronic obstructive pulmonary disease: missed diagnosis versus misdiagnosis. BMJ. 2015;351:h3021. doi: 10.1136/bmj.h3021. [DOI] [PubMed] [Google Scholar]
- 2.Soriano JB, Zielinski J, Price D. Screening for and early detection of chronic obstructive pulmonary disease. Lancet. 2009;374(9691):721–732. doi: 10.1016/S0140-6736(09)61290-3. [DOI] [PubMed] [Google Scholar]
- 3.Putcha N, Drummond MB, Wise RA, Hansel NN. Comorbidities and chronic obstructive pulmonary disease: prevalence, influence on outcomes, and management. Semin Respir Crit Care Med. 2015;36(4):575–591. doi: 10.1055/s-0035-1556063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fernández-Villar A, López-Campos JL, Represas Represas C, et al. Factors associated with inadequate diagnosis of COPD: On-Sint cohort analysis. Int J Chron Obstruct Pulmon Dis. 2015;10:961–967. doi: 10.2147/COPD.S79547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Enright P. Patients are hurt by a false diagnosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2014;189(2):229. doi: 10.1164/rccm.201306-1117LE. [DOI] [PubMed] [Google Scholar]
- 6.White P, Thornton H, Pinnock H, et al. Overtreatment of COPD with inhaled corticosteroids — implications for safety and costs: cross-sectional observational study. PLoS One. 2013;8(10):e75221. doi: 10.1371/journal.pone.0075221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carter SM, Rogers W, Heath I, et al. The challenge of overdiagnosis begins with its definition. BMJ. 2015;350:h869. doi: 10.1136/bmj.h869. [DOI] [PubMed] [Google Scholar]
- 8.Vestbo J, Hurd SS, Agusti AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347–365. doi: 10.1164/rccm.201204-0596PP. [DOI] [PubMed] [Google Scholar]
- 9.Lopez-Campos JL, Marquez-Martin E, Soriano JB. The role of air pollution in COPD and implications for therapy. Expert Rev Respir Med. 2016;10(8):849–859. doi: 10.1080/17476348.2016.1191356. [DOI] [PubMed] [Google Scholar]
- 10.Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 11.van Dijk W, Tan W, Li P, et al. Clinical relevance of fixed ratio vs lower limit of normal of FEV1/ FVC in COPD: patient-reported outcomes from the CanCOLD cohort. Ann Fam Med. 2015;13(1):41–48. doi: 10.1370/afm.1714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pinto LM, Alghamdi M, Benedetti A, et al. Derivation and validation of clinical phenotypes for COPD: a systematic review. Respir Res. 2015;16:50. doi: 10.1186/s12931-015-0208-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miravitlles M. What was the impact of the Spanish COPD guidelines (GesEPOC) and how can they be improved? Arch Bronconeumol. 2016;52(1):1–2. doi: 10.1016/j.arbres.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 14.Decramer M, Miravitlles M, Price D, et al. New horizons in early stage COPD — improving knowledge, detection and treatment. Respir Med. 2011;105(11):1576–1587. doi: 10.1016/j.rmed.2010.12.015. [DOI] [PubMed] [Google Scholar]