Abstract
Background
Children who do not attend (DNA) their hospital outpatient appointments are a concern because this potentially compromises the child’s health and incurs financial cost. Little is known about children who DNA or the views of GPs to non-attendance.
Aim
To describe the characteristics of children who DNA hospital paediatric outpatient appointments, and explore how GPs view and respond to DNAs.
Design and setting
A mixed methods study of data from all new referrals to a children’s hospital in the South West of England between 1 September and 31 October 2012.
Method
Data were extracted from patients’ hospital and GP records, and Stata was used to analyse the data quantitatively. Analysis focused on describing the characteristics of children who DNA, and the process of care that followed. Practices that had either the highest or lowest number of DNAs were purposefully sampled for GPs who had referred children to secondary care at the study hospital within the previous year. Interviews were held between May 2014 and July 2015, and were analysed thematically.
Results
Children who DNA are more likely to be from an area of greater deprivation (adjusted odds ratio [AOR] 1.02, 95% confidence interval [CI] = 1.00 to 1.02, P = 0.04), and with a child protection alert in their hospital notes (AOR 2.72, 95% CI = 1.26 to 5.88, P = 0.01). Non-attendance is communicated poorly to GPs, rarely coded in patients’ GP records, and few GP practices have a formal policy regarding paediatric DNAs.
Conclusion
Non-attendance at hospital outpatient appointments may indicate a child’s welfare is at risk. Communication between primary and secondary care needs to be improved, and guidelines developed to encourage GPs to monitor children who DNA.
Keywords: appointments and schedules, attitude of health personnel, child welfare, no-show patients, primary health care
INTRODUCTION
The label ‘did [do] not attend’ (DNA) is given to patients who DNA planned appointments, without giving notice. In 2013–2014, approximately 7.1 million (7.0%) of hospital outpatient appointments in England were missed through non-attendance. Of these, 1.3 million (17.7%) were for children aged 0–19 years.1
Missed appointments are a concern because they may compromise the child’s health,2 incur financial costs to the health service, and increase waiting times for other patients.3 Research suggests that approximately 60% of children who DNA, or perhaps, more accurately, are not brought to their outpatient appointment, need medical attention.4 A recent report identified that 20% of children who missed a paediatric respiratory clinic appointment presented to accident and emergency, or were admitted to hospital, within 90 days of that missed appointment.5
Several reasons have been identified to explain why a child may miss their appointment. These include logistical issues, such as long waiting times for the outpatient appointment,6 administrative errors,7 and social factors, such as lower socioeconomic status,8 family dysfunction,9 parental perception of importance,4 and parental forgetfulness.10 However, despite the pervasive view among healthcare practitioners that children who DNA tend to come from chaotic families,2 potentially raising concerns about their welfare,11 little is known about the characteristics of these children.
The recent Centre for Maternal and Child Enquiries (CMACE) confidential enquiry into child death,12 which looked at all children’s deaths in England, Wales, and Northern Ireland, recommended that there should be proactive follow-up of children who DNA appointments. The National Service Framework for children also states that a local system should be in place to identify those who DNA an appointment following a referral for specialist care, so that the referrer is aware and can take any follow-up action considered appropriate to ensure the child’s needs are being met.13 Despite this, a recent study mapping DNA and associated guidelines across paediatric services in the UK found that only 41% of English NHS organisations had a DNA policy in place, of which only 8% had up-to-date guidelines in the public domain.14 To date, no studies have looked at the implementation of DNA guidelines in primary care practices across the UK, and little is known about the views and response of GPs. GPs are in a good position to prevent and manage children who DNA their outpatient appointment, on the basis that they are able to make sure the parent understands why the child is being referred, to whom, and also who to contact in the event of the health complaint remitting.
How this fits in
Little is known about children who do not attend (DNA) their hospital appointments, or GPs’ views on their non-attendance. The authors’ findings suggest that non-attendance is poorly communicated to GPs, and that children who DNA are more likely than those who attend to be from an area of greater deprivation, and to have a child protection alert in their medical notes. The authors recommend that GPs code any paediatric non-attendance in patients’ GP records and develop formal policies to monitor children who do not attend.
The only qualitative study to explore healthcare professionals’ attitudes to non-attendance suggested that hospital staff tended to consider child protection aspects of paramount concern, with the need to actively follow up missed appointments, whereas GPs, in general, were less judgemental, being reluctant to interfere with parental responsibilities.3
The aim of this study was therefore to describe the characteristics of children who DNA their hospital paediatric outpatient appointments, to understand the process of care that follows non-attendance, and to explore how GPs view, communicate, and respond to DNAs.
METHOD
A mixed methods study was conducted in primary and secondary care settings.
Establishing the sample
The Medway system, a hospital electronic patient database, was used to identify all new referrals from general practices in the Bristol, North Somerset, and South Gloucestershire area to paediatric outpatient departments at a hospital based in the South West of England between 1 September and 31 October 2012. The following specialties were included: endocrinology, haematology, immunology, nephrology, gastroenterology, trauma and orthopaedics, cardiology, dermatology, ENT, oncology, general medicine, metabolic disease, neurology, respiratory medicine, rheumatology, surgery, and urology. All other specialties were excluded, as GPs were unable to make standard referrals to them. Only children up to the age of their 17th birthday were included, as the hospital policy was to only admit or see new patients aged ≤16 years.
Describing the characteristics of non-attenders and the process of care that follows non-attendance
The Medway system was used to characterise all attenders and non-attenders in terms of sex, ethnicity, and postcode (as a proxy for socioeconomic status, according to their Index of Multiple Deprivation15 score as recorded in 2010). Medway, hospital, and GP notes were used to establish the process of care that occurred in the 12 months following non-attendance, what information was given to the patient’s GP, and whether the patient had any safety alerts recorded in their hospital or GP records.
Exploring GPs’ views and response to non-attendance
Interviews were held between May 2014 and July 2015 with GPs working in Bristol, North Somerset, and South Gloucestershire. Practices that had either the highest or lowest number of DNAs were purposefully sampled. Information sheets were sent to these practices with a request for them to be distributed among GPs who had referred children to secondary care at the study hospital within the previous year. The intention was to interview 10 GPs in total: five working in practices with low DNAs, and five working in practices with high DNAs. This number of interviews was viewed as pragmatic, given the time available, and likely to lead to data saturation in the main areas explored. Having conducted 10 interviews, it was felt that data saturation had been reached in relation to these main areas, as no new themes were emerging from the later interviews.
The interviews were held over the telephone. Well-planned telephone interviews can gather the same material as those held face-to-face,16,17 and it was felt that they would be more convenient to the GP, thereby encouraging them to take part. It was also felt that interviews would be easier to organise than focus groups, and would obtain private rather than public accounts of a participant’s experience. Verbal consent was taken prior to each interview. Interviews were audio-recorded and transcribed verbatim. A topic guide was used to ensure key areas were covered with each interviewee, while also allowing GPs to raise issues salient to them (Box 1).
Box 1. Topic areas covered in the interviews with GPs.
The event and process that follow non-attendance.
The perceived significance of non-attendance in relation to the child’s health and safety.
The effectiveness of communication between primary and secondary care in relation to non-attendance.
Individual responsibilities of GPs with regards to non-attendance.
Data analysis
Quantitative data were analysed using Stata version 13 and reported using descriptive statistics. Logistic regression was used to determine the adjusted odds ratio (AORs) and 95% confidence intervals (CIs) for the association between non-attendance and sociodemographic characteristics. Interviews were analysed thematically.18 This approach entailed transcripts being read and re-read by two members of the research team who familiarised themselves with the data independently, identified emerging themes, and drafted coding frames. The two researchers met regularly to discuss and agree the final coding frame. Transcripts were entered into the software package NVivo 10 and electronically coded. Data pertaining to each code were summarised in tables, using an approach based on framework analysis.19 Comparisons were then made within and across the interviews to identify thematic patterns and deviant cases.
RESULTS
Estimate of non-attendance
Between 1 September and 31 October 2012, there were 2488 outpatient appointments booked in 17 specialties at the study hospital. In all, 2346 (94.3%) patients attended their appointment, and 142 (5.7%) were DNAs. The specialties with the highest rates of non-attendance were endocrinology (n = 10 out of 88, 11.4%), dermatology (n = 21 out of 187, 11.2%), and neurology (n = 9 out of 81, 11.1%) (Table 1).
Table 1.
Proportion of children who attended (attenders) and who did not attend (non-attenders) their outpatient appointment at the study hospital between 1 September and 31 October 2012
| Attenders, n | Non-attenders, n | Total, n | DNA rate, % | |
|---|---|---|---|---|
| Total hospital OP appointments | 2346 | 142 | 2488 | 5.7 |
| Endocrinology | 78 | 10 | 88 | 11.4 |
| Haematology | 28 | 1 | 29 | 3.5 |
| Immunology | 38 | 4 | 42 | 9.5 |
| Nephrology | 36 | 1 | 37 | 2.7 |
| Gastroenterology | 65 | 4 | 69 | 5.8 |
| Trauma and orthopaedics | 153 | 16 | 169 | 9.5 |
| Cardiology | 215 | 15 | 230 | 6.5 |
| Dermatology | 166 | 21 | 187 | 11.2 |
| ENT | 58 | 6 | 64 | 9.4 |
| Oncology | 29 | 0 | 29 | 0.0 |
| General medicine | 1043 | 28 | 1071 | 2.6 |
| Metabolic disease | 16 | 1 | 17 | 5.9 |
| Neurology | 72 | 9 | 81 | 11.1 |
| Respiratory medicine | 57 | 5 | 62 | 8.1 |
| Rheumatology | 55 | 2 | 57 | 3.5 |
| Surgery | 169 | 13 | 182 | 7.1 |
| Urology | 68 | 6 | 74 | 8.1 |
DNA = did not attend. ENT = ear, nose, and throat. OP = outpatient.
Characteristics of attenders and non-attenders
According to the hospital records, non-attenders were at greater odds of being from an area of greater deprivation (AOR 1.02, 95% CI = 1.00 to 1.02, P = 0.04) and with a child protection alert recorded in their hospital notes (AOR 2.72, 95% CI = 1.26 to 5.88, P = 0.01) (Table 2). Although children of black ethnicity appeared to have greater odds of non-attendance compared with children of white ethnicity (AOR 2.11, 95% CI = 1.14 to 3.89, P = 0.02) ethnicity did not affect attendance overall.
Table 2.
Characteristics of children who attended (attenders) and who did not attend (non-attenders) their outpatient appointment at the study hospital between 1 September and 31 October 2012
| Attenders, n (%) | Non-attenders, n (%) | AOR (95% CI) P-value | |
|---|---|---|---|
| Average age, year | 5.9 | 6.7 | 1.02 (0.99 to 1.05) 0.27 |
|
| |||
| Sex | |||
| Male | 1182 (50.4) | 75 (52.8) | 1 |
| Female | 942 (40.2) | 67 (47.2) | 0.96 (0.66 to 1.39) 0.81 |
| Unknown | 222 (9.5) | 0 (0.0) | – |
| Total | 2346 (100.0) | 142 (100.0) | |
|
| |||
| Ethnicity | |||
| White | 1607 (68.5) | 80 (56.3) | 1 |
| Mixed | 128 (5.5) | 11 (7.7) | 1.67 (0.77 to 3.62) 0.19 |
| Chinese | 12 (0.5) | 1 (0.7) | 1.93 (0.24 to 15.29) 0.54 |
| Black | 123 (5.2) | 16 (11.3) | 2.11 (1.14 to 3.89) 0.02 |
| Asian | 120 (5.1) | 10 (7.0) | 1.31 (0.58 to 2.97) 0.51 |
| Other | 24 (1.0) | 3 (2.1) | 1.68 (0.92 to 3.07) 0.09 |
| Unknown | 332 (14.1) | 21 (14.8) | – |
| Total | 2346 (100.0) | 142 (100.0) | |
|
| |||
| Socioeconomic scale | |||
| Average IMD deprivation score | 21.05 | 25.28 | 1.01 (1.00 to 1.02) 0.04 |
|
| |||
| Child protection alert | |||
| No | 2281 (97.2) | 131 (92.3) | 1 |
| Yes | 60 (2.6) | 11 (7.7) | 2.72 (1.26 to 5.88) 0.01 |
| Unknown | 5 (0.2) | 0 (0.0) | – |
| Total | 2346 (100) | 142 (100) | |
IMD = Index of Multiple Deprivation.
Process of care that followed non-attendance according to the patient’s hospital records
Information communicated to the GP
According to patients’ hospital records, the majority of GPs (59.9%, n = 85 out of 142) were not informed that their patients had not attended their outpatient appointment. This figure was also confirmed in patients’ GP records.
Repeat appointments
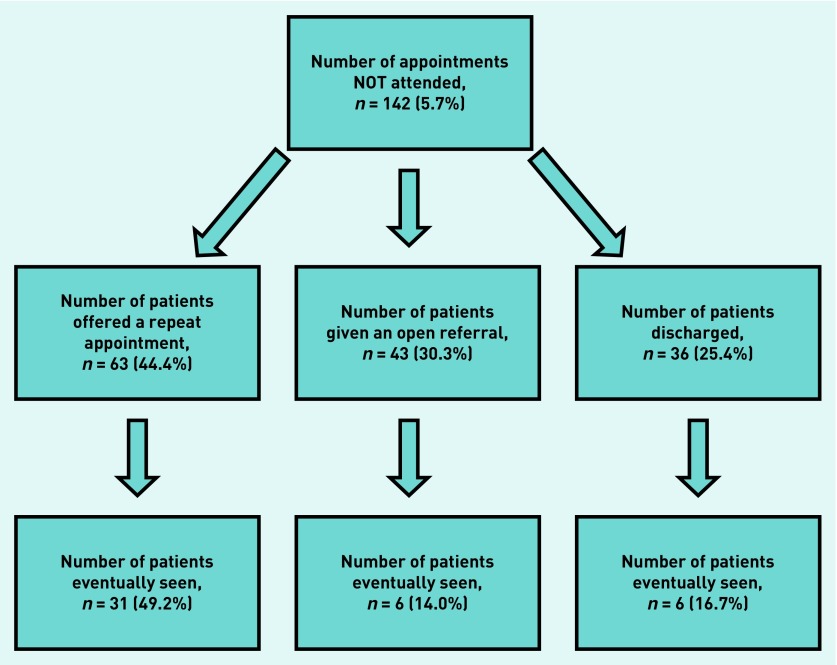
Letters offering repeat appointments were sent to 44.4% (n = 63 out of 142) of non-attenders, of whom 49.2% (n = 31 out of 63) attended the appointment within 12 months of the missed appointment (Figure 1).
Figure 1.
Process of care that followed non-attendance according to the patients’ hospital records.
Open referral
Open referrals were given to 30.3% (n = 43 out of 142) of non-attenders, of whom 14.0% (n = 6 out of 43) were eventually seen by the specialty within 12 months of the missed appointment (Figure 1).
Discharge
In addition, 25.4% (n = 36 out of 142) of non-attenders were discharged, of whom 16.7% (n = 6 out of 36) were eventually seen by the specialty within 12 months of the missed appointment (Figure 1).
Eventually seen
In summary, 30.3% (n = 43 out of 142) of non-attenders were eventually seen by the specialty to which they were originally referred within 12 months of the missed appointment. Hospital records also indicated that 28.2% (n = 40 out of 142) of non-attenders attended A&E within 12 months of their non-attendance. Of these, 10.0% (n = 4 out of 40) attended A&E for the same medical problem (Figure 1).
Child protection alerts
A total of 7.7% (n = 11 out of 142) of non-attenders had a child protection alert recorded in their hospital notes.
Events following non-attendance according to patients’ GP records
Further consultation with GP and re-referral
Since missing their appointment, 23.9% (n = 34 out of 142) of non-attenders had contacted their GP either by telephone or direct consultation for the same medical problem. Out of these, 55.9% (n = 19 out of 34) were re-referred to the same specialty for the same problem.
Evidence of child safety concerns
There were child safety concerns in the GP records of 8.5% (n = 12 out of 142) of non-attenders (Table 2). Practices did not supply this information for 17.6% (n = 25 out of 142) of non-attenders. The remaining 74.0% (n = 105 out of 142) of patients had no safety concerns in their GP notes.
GPs’ views and response to non-attendance
In all, 10 GPs (five males and five females) were interviewed, as data saturation was reached in the main areas. Analysis of the data led to four broad themes being identified. These are detailed below with quotations from GPs.
Views on non-attendance and consequences for health and safeguarding
All GPs felt that one-off non-attendance at hospital outpatient appointments was common and not an indication that they should be concerned for the child’s welfare. They felt it typically resulted from the child’s medical complaint remitting, errors regarding the administration of the appointment, or the parent simply forgetting to take the child. However, all GPs reported patients who DNA multiple times to be a concern. One described them as ‘multiple A&E attenders’, and another felt they were an indicator of inadequate parental care:
‘Yes, we all forget the odd appointment, I understand that. But actually, I think if a parent can’t be bothered to take their child to their eczema appointment, perhaps they can’t be bothered to apply the cream, or bath them. I think it can be the tip of the iceberg as regards the child’s care.’
[GP1]
GPs described three groups of children who were most likely to not attend: children from lower socioeconomic families struggling to arrange time off work, children from ethnic minority groups whose parents may not understand the reason or process of attendance due to language barriers or cultural differences, and children with complex health needs whose parents may receive multiple outpatient appointment letters, poorly stating the reason for the appointment.
GPs’ awareness of patients who DNA once
All GPs believed their practice was informed if a patient DNA an outpatient appointment. They reported being informed by a standard letter sent from the consultant:
‘We assume that the process is foolproof, that there are no missed appointments that aren’t communicated back to us. That’s something we have to go on in trust terms, but gut feeling? Yes, I think we are always told.’
[GP2]
However, many felt they were only informed about their patient’s non-attendance because:
‘All consultants want to do is get rid of the responsibility of the patient [to the GP] and dump the work onto primary care.’
[GP3]
A number of GPs felt consultants did not check their patients’ notes before discharging them. Many GPs felt consultants hid behind a trust policy of ‘discharge on the first DNA’, although they did admit to being unsure if this was a policy. Many GPs also felt the non-attendance letter they received was inadequate. Some said it was not uncommon for the letter to arrive months after the appointment, and others felt the standard format did not adequately convey to them the importance of the appointment.
GPs’ awareness of patients with multiple DNAs
Most GPs reported having long patient lists and described children as ‘one-off, last-minute attenders’ [GP4], who did not see their regular doctor, making it difficult for them to track their medical history. As such, many GPs reported relying on the child’s GP records to see if the child had missed an appointment. However, they felt any non-attendance would not be apparent if it was very recent, unless the GP had read through all of the child’s notes, or every DNA letter for the child was coded into their notes so that an alert could flash up on the front page. Only two GPs reported coding DNA letters, and most GPs reported that they only had time to make a cursory glance at the patient’s notes before a consultation.
GPs’ approach to managing and addressing non-attendance
Only one practice had a formal policy in place for managing patients who DNA their hospital outpatient appointment. The remaining nine GPs described taking a range of actions that were based on their own clinical judgement and knowledge of the patient. Although two GPs professed to not checking the notes at all if they saw that the child had been offered a repeat appointment, most described taking a cursory glance in order to check that the appointment letter had been sent to the correct address. A few GPs described only reading the notes in any great detail if the letter came from an ‘important’ specialty, such as oncology or cardiology, or if the initial referral, as described in the letter, suggested that the referral related to a serious health complaint. Most described being under considerable time pressure at work:
‘If I am honest, most days I barely have time to go to the loo. If I had more time, I would check every letter that arrived in my inbox, but when you have the patient load that we have, then that’s just not realistic. But yes, if I can, I’ll give the letter a cursory glance to check it’s nothing too concerning, you know, and that the letter has gone to right address.’
[GP5]
The majority of GPs described being reluctant to address any non-attendance with the child’s parents, unless they were very concerned for the health and welfare of the child, as they did not want to start a ‘rant’ or had little time to chase patients. If the GP was concerned for the child’s health or welfare, this appeared to escalate the GP’s response to managing the DNA. In this instance, GPs described making contact with the parent, checking the patient’s notes for other DNAs, and writing to the parent or speaking to other team members, such as the health visitor or community paediatrician. A few admitted that the main reason for doing this was to ‘cover their back’ should any concerns arise from the DNA.
DISCUSSION
Summary
According to patients’ hospital records, non-attenders were more likely than children who did attend to come from an area of greater deprivation and to have a child protection alert recorded in their hospital notes. The qualitative findings suggest that GPs are less informed about non-attendance than they think they are, and highlight concerns regarding the lack of any formal policy in primary care to manage DNAs, or code DNAs in patients’ notes. Taken together, it might be argued that GPs should be more concerned about DNA events in children, as these findings suggest they may be associated with a child’s welfare being at risk. This small, mixed methods study also indicated that one-quarter of all non-attenders attended A&E in the 12 months following their DNA, and that approximately one-third of non-attenders are eventually seen by the specialty to which they were originally referred. This suggests that health complaints for a significant proportion of these children do not remit, and confirms GPs’ views that non-attenders at outpatient clinics may be high A&E attenders. Finally, although the General Medical Council do not comment specifically on patients not attending outpatient appointments,20 and their guidance regarding the care of children is mainly geared towards child protection issues, the medical defence organisations suggest there is a protocol for practices to follow when informed of patients who DNA.21 This does, however, require the GP to be informed of the DNA by the hospital.
Strengths and limitations
The main strength of this study is its mixed method approach, which enabled the study to achieve both of its objectives and, in doing so, provide some insight into which children DNA, and how primary care responds to this. However, the fact that data were only from one hospital, and for a 2-month period, will limit generalisability of the findings. Generalisability may also be limited by the fact that GP practices were purposefully sampled and only 10 GPs were interviewed, although data saturation was reached. Nor did the study explore the views of service users to understand possible reasons for non-attendance. Lastly, as the demographic data for the study were generated from hospital notes, 100% accuracy cannot be assumed.
Comparison with existing literature
The only qualitative study to explore GPs’ attitudes to non-attendance suggested that GPs in general were reluctant to address non-attendance with patients, and interfere with parental responsibilities.2 The findings lend some support to this, but also highlight the little time GPs have to address non-attendance, and the reasons why they may not be aware of it. The findings also support previous research that suggests children who DNA may be from lower socioeconomic backgrounds,7 and provides some support to the notion that there may be welfare concerns for these children.11
Implications for research
This was a small, exploratory, mixed methods study and there is clear need for further research in this area to support its findings. However, the findings do suggest that non-attendance at hospital outpatient appointments may highlight a safeguarding concern. They also cast light on potentially poor communication between primary and secondary care, drawing attention to the lack of procedures or policies in primary care to identify and follow up children who DNA. Due to limited time and resources it was not possible to interview the parents or carers of children that DNA. However, future research may consider doing so, as this would allow for a fuller understanding of the reasons for non-attendance. The findings from this study may also usefully inform the development of a larger survey of GPs’ views regarding communication with secondary care, patient responsibility, and non-attendance, in order that procedures and policies across primary and secondary care may be improved. Finally, it may be that a child who DNA is only at greater risk of any welfare issues if this occurs in the context of other risk factors, not all of which could be identified in this study. Further research should therefore include larger samples from a wider geographical area, to allow more in-depth analysis of presenting symptoms and reason for referral.
Acknowledgments
The authors are very grateful to all the GPs who shared their views and experiences of managing DNAs in primary care.
Funding
Hannah Morley was funded as an Academic Foundation Doctor through the Severn Deanery. Julian Hamilton-Shield was funded by the Biomedical Research Unit in the National Institute for Health Research Biomedical Research Centre and Unit scheme. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research, or the Department of Health.
Ethical approval
The University of Bristol’s ethics committee approved the study.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
All other authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Health and Social Care Information Centre . Hospital outpatient activity — April 2012 to March 2013. Provider level analysis. NHS HSCIC; 2013. [Google Scholar]
- 2.Arai L, Stapley S, Roberts H. ‘Did not attends’ in children 0–10: a scoping review. Child Care Health Dev. 2014;40(6):797–805. doi: 10.1111/cch.12111. [DOI] [PubMed] [Google Scholar]
- 3.Cameron E, Heath G, Redwood S, et al. Health care professionals’ views of paediatric outpatient non-attendance: implications for general practice. Fam Pract. 2013;31(1):111–117. doi: 10.1093/fampra/cmt063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andrews R, Morgan JD, Addy DP, McNeish AS. Understanding non-attendance in outpatient paediatric clinics. Arch Dis Child. 1990;65(2):192–195. doi: 10.1136/adc.65.2.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Health and Social Care Information Centre Provisional monthly topic of interest: outpatient did not attend (DNA) appointment. http://www.hscic.gov.uk/catalogue/PUB14316/prov-mont-hes-admi-outp-ae-April%202013%20to%20March%202014-toi-rep.pdf (accessed 17 May 2017)
- 6.Bowman RJ, Bennett HG, Houston CA, et al. Waiting times for and attendance at paediatric ophthalmology outpatient appointments. BMJ. 1996;313(7067):1244. doi: 10.1136/bmj.313.7067.1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barnado’s South West . Consultation to explore non-attendance rates in East Central Bristol Paediatric and Child and Adolescent Mental Health Service. Bristol: Barnardo’s; 2011. [Google Scholar]
- 8.McClure RJ, Newell SJ, Edwards S. Patient characteristics affecting attendance at general outpatient clinics. Arch Dis Child. 1996;74(2):121–125. doi: 10.1136/adc.74.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simkiss DE, Spencer NJ, Stallard N, Thorogood M. Health service use in families where children enter public care: a nested case control study using the General Practice Research Database. BMC Health Serv Res. 2012;12(1):65. doi: 10.1186/1472-6963-12-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gurney K, Pearson V, Gibbs S. Audit of hospital did not attend (DNA) appointments for 0–18-year-olds. NHS Devon; 2012. [Google Scholar]
- 11.Watson M, Forshaw M. Child outpatient non-attendance may indicate welfare concerns. BMJ. 2002;324(7339):739. doi: 10.1136/bmj.324.7339.739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Department for Education Child death reviews: year ending 31 March 2010. 2010. https://www.gov.uk/government/statistics/preventable-child-deaths-in-england-year-ending-31-march-2010 (accessed 24 May 2017)
- 13.Department of Health . National service framework for children, young people and maternity services. London: DH; 2004. [DOI] [PubMed] [Google Scholar]
- 14.Arai L, Stephenson T, Roberts H. The unseen child and safeguarding: ‘did not attend’ guidelines in the NHS. Arch Dis Child. 2015 doi: 10.1136/archdischild-2014-307294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Department of Communities and Local Government English indices of deprivation 2010. https://www.gov.uk/government/statistics/english-indices-of-deprivation-2010 (accessed 8 Jun 2017)
- 16.Sturges JE, Hanrahan KJ. Comparing telephone and face-to-face qualitative interviewing: a research note. Qual Res. 2004;4(1):107–118. [Google Scholar]
- 17.Taylor AW, Wilson DH, Wakefield M. Differences in health estimates using telephone and door-to-door survey methods — a hypothetical exercise. Aust N Z J Public Health. 1998;22(2):223–226. doi: 10.1111/j.1467-842x.1998.tb01177.x. [DOI] [PubMed] [Google Scholar]
- 18.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. [Google Scholar]
- 19.Bryman A, Burgess RG, editors. Analysing qualitative data. London: Routledge; 1994. [Google Scholar]
- 20.General Medical Council Protecting children and young people: doctors’ responsibilities. 2016. http://www.gmc-uk.org/guidance/ethical_guidance/13257.asp (accessed 24 May 2017)
- 21.MDU Who takes responsibility for missed appointments? 2016. https://www.themdu.com/guidance-and-advice/guides/who-takes-responsibility-for-missed-appointments (accessed 22 May 2017)