Abstract
We describe a female patient who presented with watering followed by swelling in the left infraorbital area of 5 years duration. She had previously been prescribed topical antibiotics on several occasions with no improvement. On pressure over the swelling, there was blood-tinged discharge from the left eye and nostril. Magnetic resonance imaging revealed an enhancing, well-defined mass lesion in the inferomedial aspect of the left orbit, likely of nasolacrimal origin. Computed tomography dacryocystogram with three-dimensional reconstruction showed a well-circumscribed mass with an irregular surface, originating from the lacrimal sac. Gram staining and potassium hydroxide mount from the regurgitant fluid revealed thick-walled cysts with sporangia suggestive of Rhinosporidium seeberi infection. Excision biopsy of the lesion confirmed R. seeberi as the causative agent. The patient has been put on long-term dapsone therapy to prevent a recurrence and has been asked to follow-up 6 months later.
Keywords: Bloody tears, computed tomography-dacryocystography, lacrimal sac, rhinosporidiosis
Bloody tears, though uncommon, is known to occur secondary to trauma, disorders of the adnexa, and systemic bleeding disorders.[1] We describe a case with long-standing blood-tinged epiphora associated with an infraorbital swelling of the left eye.
Case Report
A 13-year-old female from rural Jharkhand, India, presented with complaints of a swelling on the inner aspect of her left lower eyelid with associated watering of eye for 5 years. It started as a painless, pea-sized swelling which gradually increased to its present size. On manual pressure over the swelling, there was regurgitation of blood-tinged fluid in the eye and from the nose. There were no complaints of antecedent trauma, visual disturbances, redness or pain over the swelling, fever, weight loss, or loss of appetite.
On clinical examination, her visual acuity was found to be 20/20 in both eyes. Slit-lamp examination of the anterior segment and fundus examination were normal. Extraocular movements were full in range and painless. There was a soft, nontender, immobile, slightly compressible swelling measuring 3 cm × 3 cm situated 2 cm below the left medial canthus that extended infero-laterally along the inferior orbital margin till the junction of the medial 2/3rd and the lateral 1/3rd [Fig. 1a]. The skin over the swelling was of a greenish-blue hue with signs of mild inflammation. Routine blood investigations were normal with no evidence of bleeding diathesis. Magnetic resonance imaging of the orbit showed a well-defined moderately enhancing lesion (T1-weighted (T1W) hypo-intense, T2W fluid-attenuated inversion recovery hyperintense) measuring approximately 1.4 cm × 1.5 cm × 1.7 cm arising from the region of the left nasolacrimal duct (NLD). Dacryocystography did not yield any filling defect or any delay in contrast disappearance. However, computed tomography (CT) dacryocystography with three dimensional (3D) reconstruction [Fig. 1b] showed a well-circumscribed pear-shaped lesion, with an irregular surface, originating from the left lacrimal sac (LS) and extending onto the medial half of the inferior orbital rim. There was no evidence of bone erosion or thinning.
Figure 1.
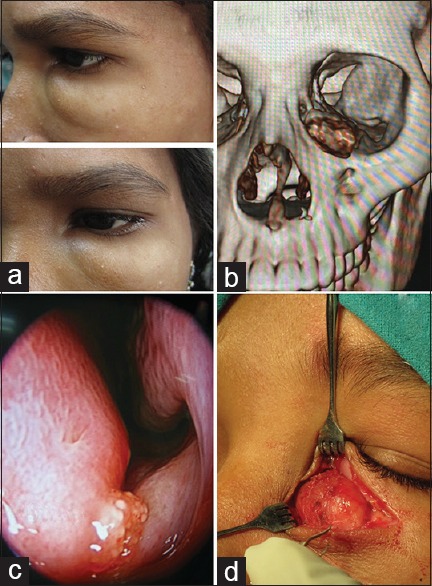
(a) Infraorbital swelling with greenish hue of overlying skin medially. (b) Computed tomography dacryocystography with three-dimensional reconstruction showing a well-circumscribed lesion originating from the lacrimal sac. (c) Diagnostic nasal endoscopy showing lesion with grayish white dots over the lower part of the left nasal septum. (d) On-table appearance of specimen noted to be originating from the region of lacrimal sac. Skin, subcutaneous tissue, and orbicularis incised
Regurgitant fluid was sent for hematoxylin and eosin (H and E) staining, Gram staining, acid–fast bacilli, potassium hydroxide (KOH) mount, bacterial culture and sensitivity, fungal and tuberculosis culture. H and E staining [Figs. 2 and 3] and KOH preparations showed thick-walled cysts which contained spores. Bacterial, fungal, and tubercular culture of the fluid did not yield any growth.
Figure 2.
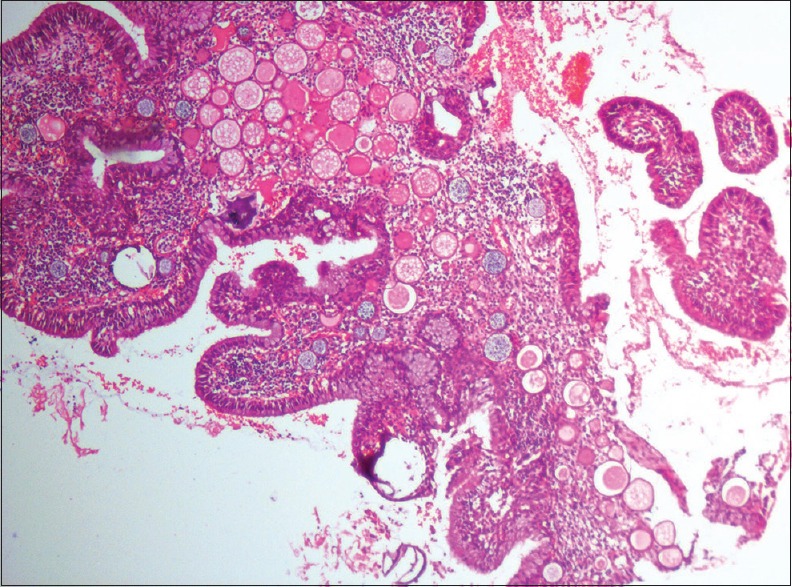
Sporangium containing many sporangiospores (H and E, ×100)
Figure 3.
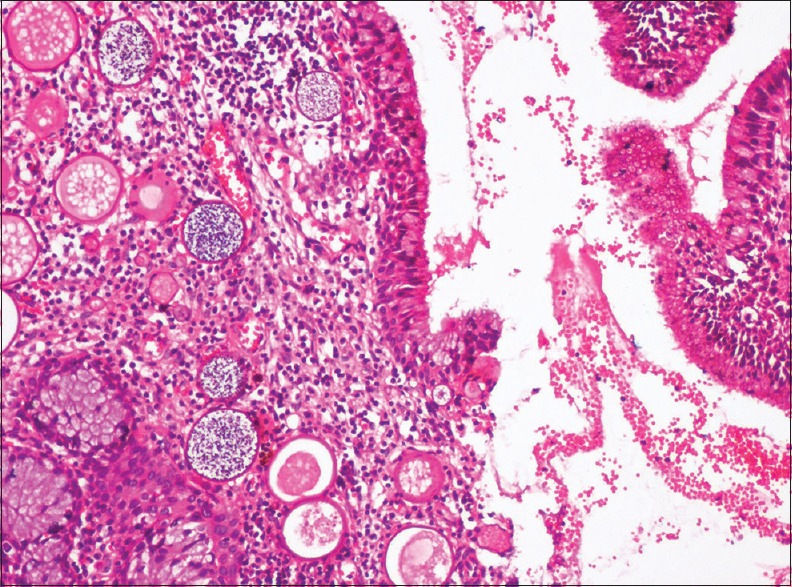
Spores and cysts with chitinous eosinophilic wall (H and E, ×400)
A diagnostic nasal endoscopy [Fig. 1c] reported a lesion with grayish dots seen over the lower septum of the left nasal cavity and a similar lesion over the anterior border of the uncinate process.
An external approach was planned with an incision above the most prominent part and dissection along the plane of the swelling. The anterior lacrimal crest was identified, and the swelling was found to be originating as a continuation of the LS in the lacrimal fossa [Fig. 1d]. Careful dissection enabled an excision in toto along with the LS. The specimen was sent for microbiological and histopathological examination. A diagnosis of rhinosporidiosis of the LS was confirmed.
The patient was put on dapsone therapy 100 mg once a day to be continued for 1 year and was asked to follow-up every 6 months. The patient was lost to follow-up.
Discussion
Common causes for blood-tinged tears include conjunctival lesions, including vascular tumors and malformations, chronic actinomyces canaliculitis, punctual pyogenic granuloma, hereditary hemorrhagic telangiectasis, tumors of the lacrimal apparatus, corneal vascular lesions, severe epistaxis with regurgitation through the lacrimal passage, and systemic bleeding disorders.[1]
NLD mucoceles, encephalocele, hemangioma, dermoid cysts, nasal gliomas, and tumors of the LS are common swellings presenting at the infraorbital and LS region.[2]
Rhinosporoidiosis, a chronic granulomatous disease,[3] is caused by Rhinosporidium seeberi, which has been recently reclassified to a new clade named Mesomycetozoa.[4] The disease is endemic in southern India and Sri Lanka. Ocular rhinosporidiosis accounts for 15% of the cases with the conjunctiva being the most common affected site.[2] Seen most frequently in children between 8 and 10 years, and with a male predilection (2.5:1), the LS is involved in only 7.32%.[5] The natural habitat of the organism is ground water and infection is thought to occur by the transepithelial route.[2] In a study by Shrestha et al., a 95% positive history of affected patients bathing in contaminated water bodies was obtained.[5] Our patient gave a similar history. The mode of inoculation into the sac has been postulated to occur either through the canaliculi or the nose without affecting these structures.[6]
LS rhinosporidiosis has been reported to present with a painless soft fluctuant swelling with epistaxis, partial or complete NLD obstruction, and blood-tinged discharge from the eye.[5] The swelling occurs due to a dilated LS which is found to contain polypoidal growths.[7] Our patient had no evidence of NLD obstruction as seen on dacryocystography. The satellite lesions observed in the nasal cavity could have occurred secondary to autoinoculation by the LS discharge.[2] As the organism has not yet been cultured in vitro, demonstration of the various stages of the organism by histopathology of the biopsied tissue is the mainstay of diagnosis.[2] Complete excision of the mass with removal of the sac has been advocated as the treatment of choice,[5] and the external approach is still preferred as is provides direct visualization of the local anatomy. Medical therapy with dapsone appears to arrest the maturation of the sporangia and promotes fibrosis in the stroma.[8]
Conclusion
Although nasoorbital rhinosporidiosis is common, this lesion manifested with an uncommon clinical presentation. In suspected LS involvement, a CT dacryocystography with 3D reconstruction could be a cost-effective,noninvasive investigation. Since this infection is prone for chronicity and recurrence, it is imperative that we counsel the patient accordingly.
A high index of suspicion with a multidisciplinary approach to treatment including ophthalmology and otorhinolaryngology and community medicine is needed to manage such cases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors wholeheartedly thank Mrs. Kalpaja DA, Director Vydehi Institute of Medical Science and Research Centre (VIMS and RC) and the management of VIMS and RC for providing the necessary support that has made this report possible; Dr Girish, Associate Professor, Department of Microbiology, VIMS and RC for his continued support throughout this case; the HOD's and staff of the Departments of ENT, Microbiology, Pathology, Paediatrics and Radiology, VIMS and RC for their crucial support in clinching the diagnosis of this case; the Professors, Staff and Resident doctors of the Department of Ophthalmology, VIMS and RC; Mr. Tarul Khatun, who, on behalf of his daughter, Ms. Siuli Khatun, has given us permission to report this case.
References
- 1.Karslioglu S, Simsek IB, Akbaba M. A case of recurrent bloody tears. Clin Ophthalmol. 2011;5:1067–9. doi: 10.2147/OPTH.S19779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Britto FC, Rosier VV, Luz TV, Verde RC, Lima CM, Lessa MM. Nasolacrimal duct mucocele: Case report and literature review. Int Arch Otorhinolaryngol. 2015;19:96–8. doi: 10.1055/s-0034-1366978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ashworth JH. On Rhinosporidium seeberi (Wernicke, 1903) with special reference to its sporulation and affinities. Trans R Soc Edinb. 1923;53:301–42. [Google Scholar]
- 4.Herr RA, Ajello L, Taylor JW, Arseculeratne SN, Mendoza L. Phylogenetic analysis of Rhinosporidium seeberi's 18S small-subunit Ribosomal DNA groups this pathogen among members of the protoctistan Mesomycetozoa clade. J Clin Microbiol. 1999;37:2750–4. doi: 10.1128/jcm.37.9.2750-2754.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shrestha SP, Hennig A, Parija SC. Prevalence of rhinosporidiosis of the eye and its adnexa in Nepal. Am J Trop Med Hyg. 1998;59:231–4. doi: 10.4269/ajtmh.1998.59.231. [DOI] [PubMed] [Google Scholar]
- 6.Jain SN. Aetiology and incidence of rhinosporidiosis. Indian J Otolaryngol. 1967;19:1–21. [Google Scholar]
- 7.Pushker N, Kashyap S, Bajaj MS, Meel R, Sood A, Sharma S, et al. Primary lacrimal sac rhinosporidiosis with grossly dilated sac and nasolacrimal duct. Ophthal Plast Reconstr Surg. 2009;25:234–5. doi: 10.1097/IOP.0b013e3181a39495. [DOI] [PubMed] [Google Scholar]
- 8.Job A, Venkateswaran S, Mathan M, Krishnaswami H, Raman R. Medical therapy of rhinosporidiosis with dapsone. J Laryngol Otol. 1993;107:809–12. doi: 10.1017/s002221510012448x. [DOI] [PubMed] [Google Scholar]


